On-Demand ICS + FABA Combinations in 6–11-Year-Old Children
Abstract
:1. Introduction
1.1. Step 1 Treatment: Use an ICS Every Time You Use a Short-Acting β2-Agonist SABA
- Frequency of treatment failures (the requirement for a second dose of prednisone within any 6-month period) was higher in the placebo group vs. the twice-daily BDP with BDP plus albuterol as rescue (combined group): 23% (95% CI [14–34], n = 17) vs. 8.5% ([2–15], n = 6), p = 0.024.
- Compared with the placebo group, the hazard ratio for asthma exacerbations was lower in the rescue BDP group (0.62 [0.37–1.05], p = 0.073).
- No difference in asthma control days, morning peak expiratory flow (PEF), fractional exhaled nitric oxide (FENO), methacholine bronchial responsiveness, or quality of life in patients using for the relief of their symptoms albuterol vs. the use of SABA + ICS (rescue beclomethasone group).
- There was a significant decrease regarding the prebronchodilator percentage predicted FEV1 in the placebo and rescue BDP group, although the decrease was higher in the group using only albuterol (−6.6%, SD 1.7, p = 0.0001) vs. (−4.1%, SD 1.8, p = 0.024).
1.2. Step 2 Treatment: Continuous ICS vs. ICS + a Fast-Acting Beta-Agonist (FABA) as Needed
- The probability of a first exacerbation by the end of the trial was reduced by 28% [18–40] (n = 20) in the daily BDP group and 35% [24–47] (n = 25) in the rescue BDP group, both compared with the placebo group, although the differences were not significant, and no comparison was made between those two groups [13].
- No difference between continuous ICS therapy vs. ICS + FABA as needed was observed in terms of: asthma control days, morning PEF, methacholine bronchial responsiveness, quality of life, and treatment failures [13].
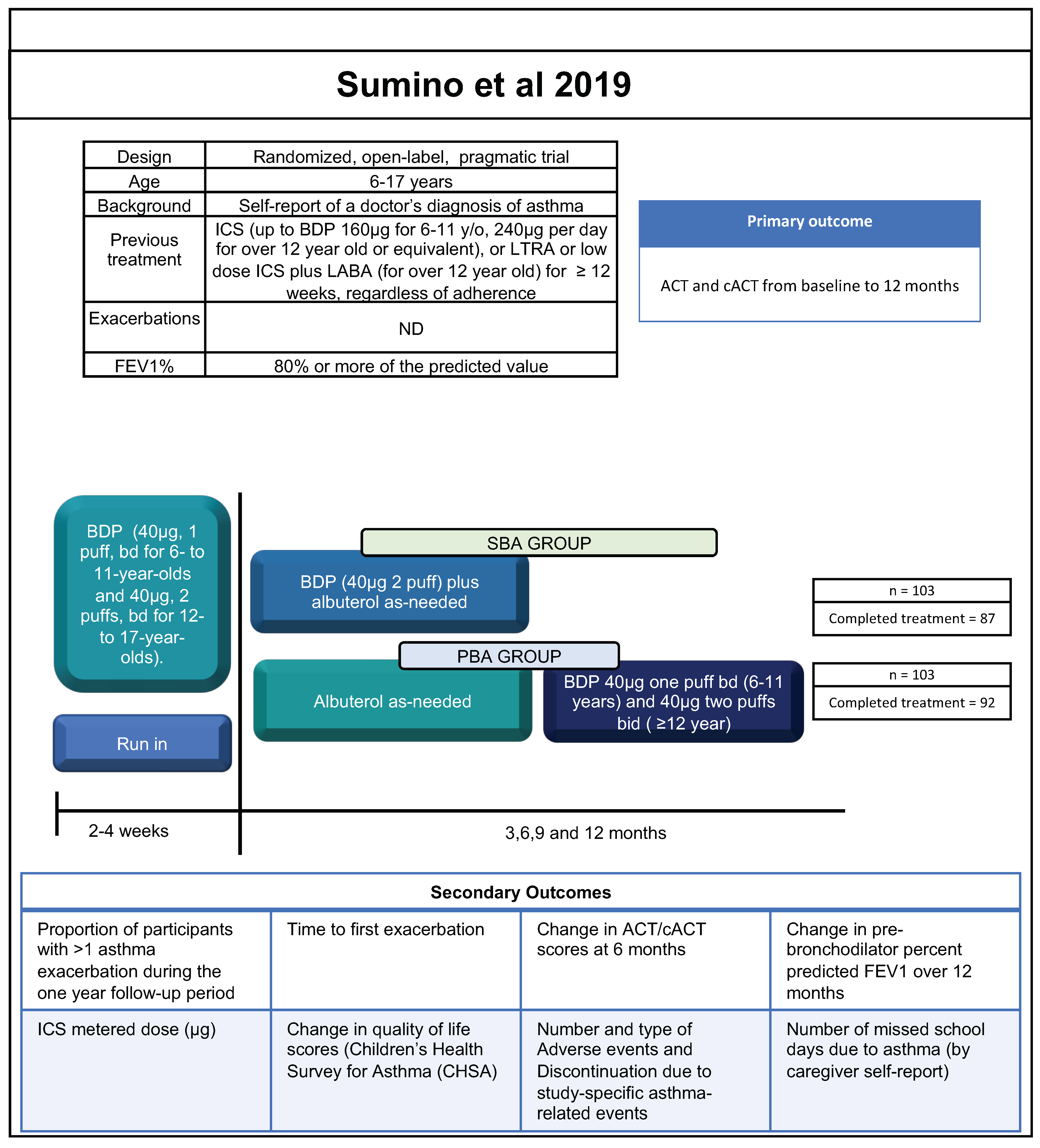
- There was no significant difference between SBA vs. PBA groups in the exacerbations, time to the first exacerbation, asthma control questionnaire (ACQ-5) score, self-reported, missed school days per year, FEV1, and quality of life [14].
- The use of BDP (μg/month) was greater in the PBA group vs. SBA group 1961 μg/month (1681–2241 μg) vs. 526 μg/month (413–639 μg), respectively, p < 0.0001 [14].
- Children in the daily BDP group grew 1·1 cm (SD 0.3) less than the children in the placebo group (p < 0.0001), while the difference between rescue BDP and placebo was not significant [13].
1.3. Step 3 Treatment: Use of MART Therapy
- The risk of experiencing a severe asthma exacerbation was 66% lower when the MART approach was used versus the fixed-combination group (hazard ratio (HR): 0.34, [95% CI 0.19–0.60]), and 51% lower than the fixed-dose budesonide group (HR: 0.49 [0.27–0.90]). Also, there were less exacerbations requiring medical intervention in the MART group 8% vs. 20% (fixed-dose budesonide group) and 31% (fixed-combination group). Morning and evening PEF were significantly better in the MART group vs. the fixed-dose budesonide group, but there was no difference between the utilization of MART vs. the fixed-combination group.
2. Discussion
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- GINA Committee. Global Strategy for Asthma Management and Prevention 2023 Update; Global Initiative for Asthma: Fontana, WI, USA, 2023. [Google Scholar]
- GUÍA ESPAÑOLA PARA EL MANEJO DEL ASMA. Available online: www.gemasma.com (accessed on 1 July 2023).
- Stein, S.W.; Thiel, C.G. The History of Therapeutic Aerosols: A Chronological Review. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 20–41. [Google Scholar] [CrossRef] [PubMed]
- Inman, W.H.; Adelstein, A.M. Rise and fall of asthma mortality in England and Wales in relation to use of pressurised aerosols. Lancet 1969, 2, 7615. [Google Scholar] [CrossRef] [PubMed]
- British Thoracic Society. BTS/SIGN British Guideline on the Management of Asthma. Asthma. 2019. Available online: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/ (accessed on 1 July 2023).
- Plaza, V.; Alobid, I.; Alvarez, C.; Blanco, M.; Ferreira, J.; García, G.; Gómez-Outes, A.; Gómez, F.; Hidalgo, A.; Korta, J.; et al. Guía española para el manejo del asma (GEMA) versión 5.1. Aspectos destacados y controversias. Arch. Bronconeumol. 2022, 58, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.G. Nonadherence to Asthma Treatment: Getting Unstuck. J. Allergy Clin. Immunol. Pract. 2016, 4, 849–851. [Google Scholar] [CrossRef] [PubMed]
- Kuprys-Lipinska, I.; Kolacinska-Flont, M.; Kuna, P. New approach to intermittent and mild asthma therapy: Evolution or revolution in the GINA guidelines? Clin. Transl. Allergy 2020, 10, 19. [Google Scholar] [CrossRef] [PubMed]
- Larenas-Linnemann, D.; Navarrete-Rodríguez, E.M.; Luna-Pech, J.A.; Benítez, R.; Cano-Salas, M.C.; Del Rio-Navarro, B.E.; García-Ramírez, U.N.; Gochicoa, L.; López-Estrada, E.D.C.; Ortega-Martell, J.A.; et al. An independent in-depth analysis proposing adjusted Global Initiative on Asthma Step 1–2 treatment suggestions. Clin. Exp. Allergy 2022, 52, 493–511. [Google Scholar] [CrossRef] [PubMed]
- Ortega, H.; Yancey, S.W.; Keene, O.N.; Gunsoy, N.B.; Albers, F.C.; Howarth, P.H. Asthma Exacerbations Associated with Lung Function Decline in Patients with Severe Eosinophilic Asthma. J. Allergy Clin. Immunol. Pract. 2018, 6, 980–986.e1. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, W.J.; Haselkorn, T.; Miller, D.P.; Omachi, T.A. Asthma exacerbations and lung function in patients with severe or difficult-to-treat asthma. J. Allergy Clin. Immunol. 2015, 136, 1125–1127.e4. [Google Scholar] [CrossRef] [PubMed]
- Gaffin, J.M.; Petty, C.R.; Sorkness, R.L.; Denlinger, L.C.; Phillips, B.R.; Ly, N.P.; Gaston, B.; Ross, K.; Fitzpatrick, A.; Bacharier, L.B.; et al. Determinants of lung function across childhood in the Severe Asthma Research Program (SARP) 3. J. Allergy Clin. Immunol. 2023, 151, 138–146.e9. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.D.; Chinchilli, V.M.; Morgan, W.J.; Boehmer, S.J.; Lemanske, R.F.; Mauger, D.T.; Strunk, R.C.; Szefler, S.J.; Zeiger, R.S.; Bacharier, L.B.; et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): A randomised, double-blind, placebo-controlled trial. Lancet 2011, 377, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Sumino, K.; Bacharier, L.B.; Taylor, J.; Chadwick-Mansker, K.; Curtis, V.; Nash, A.; Jackson-Triggs, S.; Moen, J.; Schechtman, K.B.; Garbutt, J.; et al. A Pragmatic Trial of Symptom-Based Inhaled Corticosteroid Use in African-American Children with Mild Asthma. J. Allergy Clin. Immunol. Pract. 2020, 8, 176–185.e2. [Google Scholar] [CrossRef] [PubMed]
- Bisgaard, H.; Le Roux, P.; Bjåmer, D.; Dymek, A.; Vermeulen, J.H.; Hultquist, C. Budesonide/formoterol maintenance plus reliver therapy: A new strategy in pediatric asthma. Chest 2006, 130, 1733–1743. [Google Scholar] [CrossRef] [PubMed]
- O’Byrne, P.M.; Bisgaard, H.; Godard, P.P.; Pistolesi, M.; Palmqvist, M.; Zhu, Y.; Ekström, T.; Bateman, E.D. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am. J. Respir. Crit. Care Med. 2005, 171, 129–136. [Google Scholar] [CrossRef] [PubMed]
- O’Byrne, P.M.; FitzGerald, J.M.; Bateman, E.D.; Barnes, P.J.; Zhong, N.; Keen, C.; Jorup, C.; Lamarca, R.; Ivanov, S.; Reddel, H.K. Inhaled Combined Budesonide–Formoterol as Needed in Mild Asthma. N. Engl. J. Med. 2018, 378, 1865–1876. [Google Scholar] [CrossRef] [PubMed]
- Bateman, E.D.; Reddel, H.K.; O’Byrne, P.M.; Barnes, P.J.; Zhong, N.; Keen, C.; Jorup, C.; Lamarca, R.; Siwek-Posluszna, A.; FitzGerald, J.M. As-Needed Budesonide–Formoterol versus Maintenance Budesonide in Mild Asthma. N. Engl. J. Med. 2018, 378, 1877–1887. [Google Scholar] [CrossRef] [PubMed]
- Beasley, R.; Holliday, M.; Reddel, H.K.; Braithwaite, I.; Ebmeier, S.; Hancox, R.J.; Harrison, T.; Houghton, C.; Oldfield, K.; Papi, A.; et al. Controlled Trial of Budesonide–Formoterol as Needed for Mild Asthma. N. Engl. J. Med. 2019, 380, 2020–2030. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.; Baggott, C.; Fingleton, J.; Reddel, H.K.; Hancox, R.J.; Harwood, M.; Corin, A.; Sparks, J.; Hall, D.; Sabbagh, D.; et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): A 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet 2019, 394, 919–928. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, M.M.; Baptist, A.P.; Blake, K.V.; Brooks, E.G.; Bryant-Stephens, T.; DiMango, E.; Dixon, A.E.; Elward, K.S.; Hartert, T.; Krishnan, J.A.; et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J. Allergy Clin. Immunol. 2020, 146, 1217–1270. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Prietsch, S.O.; Ducharme, F.M. Inhaled corticosteroids in children with persistent asthma: Effects on growth. Evid.-Based Child Health 2014, 9, 829–930. [Google Scholar] [CrossRef] [PubMed]
- Israel, E.; Cardet, J.C.; Carroll, J.K.; Fuhlbrigge, A.L.; She, L.; Rockhold, F.W.; Maher, N.E.; Fagan, M.; Forth, V.E.; Yawn, B.P.; et al. Reliever-Triggered Inhaled Glucocorticoid in Black and Latinx Adults with Asthma. N. Engl. J. Med. 2022, 386, 1505–1518. [Google Scholar] [CrossRef] [PubMed]


| GINA 6–11 Years [1] | GEMA ≥ 4 Years [2] | BTS/SIGN (Pediatric Treatment) [5] | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | |
| Preferred Controller | Low-dose ICS taken whenever SABA taken | -Daily low-dose ICS | -Low-dose ICS-LABA. -Medium-dose ICS -Very-low-dose ICS + Formoterol maintenance and reliever (MART) | No treatment needed | Daily low-dose ICS | -Medium-dose ICS -Low-dose ICS-LABA | No treatment needed | Very-low- (pediatric) dose ICS | -Very-low- (pediatric) dose ICS + LABA or LTRA (children ≥ 5) -Very-low- (pediatric) dose ICS + LTRA (children < 5) |
| Other controller options | Consider daily low-dose ICS | -Daily leukotriene receptor antagonist. -Low-dose ICS taken whenever SABA taken | Low-dose ICS + LTRA | Daily LTRA | Low-dose ICS + LTRA | ||||
| Reliever | As-needed SABA | As-needed SABA | -As-needed SABA -Low-dose ICS–formoterol reliever for MART | As-needed SABA | As-needed SABA | As-needed SABA | As-needed SABA | As-needed SABA | As-needed SABA |
| TREXA 2011 [13] | SUMINO 2019 [14] | BISGAARD 2006 [15] | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Methods | Design | Multicenter, double-blind, randomized, four-group | Randomized, open-label, pragmatic trial | Prospectively planned analysis of pediatric data from randomized, double-blind, and parallel-group trial. O’Byrne 2005 [16] | ||||||
| Participants | Age | 6–18 years | 6–17 years | 4–11 years | ||||||
| Asthma diagnosis | History of mild persistent asthma during the previous 2 years | Self-report of a doctor’s diagnosis of asthma | Asthma history ≥ 6 months | |||||||
| Treatment step | 2 | 2 (6–11 years), 2–3 (2–17 years) | 3 | |||||||
| Main Inclusion Criteria | Previous treatment | Naive to controller treatment | Treated previous 8 w with monotherapy other than ICS | Controlled 8 weeks on low ICS | ICS (up to BDP 160 mcg for 6–11 y/o, 240 mcg per day for over 12 year old or equivalent), or LTRA or low dose ICS plus LABA (for over 12 year old) for ≥12 weeks, regardless of adherence | ICS (any brand) at a constant dose for ≥3 months (200 to 500 mcg/d) | ||||
| Symptoms | ND | Asthma Evaluation Questionnaire Score (AEQ) 1 up to score 2 in 2 out of 3 questions with total score ≤ 5. | Eight or more inhalations of terbutaline in the last 10 days of run-in and up to seven inhalations on any 1 day | |||||||
| Exacerbations | 1–2 previous year | ND | ND | ND | One clinically important in the last 12 months. | |||||
| FEV1% | 75% or more of the predicted value | ≥80% predicted | 60 to 100% predicted | |||||||
| Run in | 4w run-in period, 40mcg BDP bd, and albuterol for rescue. Placebo rescue inhaler to be used along with albuterol for symptoms. | 2- to 4w. BDP (40 mg, 1 puff, bd for 6–11 year and 40 mg, 2 puffs, bd for 12- to 17-year-olds). Telephone-based education (2–4 sessions). | Previous ICS plus terbutaline as needed | |||||||
| Additional treatment permitted if worsening | Albuterol for the prevention of exercise-induced asthma | In PBA group.- Subsequent dosing adjustments were made by the physician according national guidelines | Not more than 8 inhalations of the medication 1 day. If the patient needed more medication, the investigator had to be contacted. | |||||||
| Adherence to treatment | Electronic measurements review at each visit. | ND | ND | |||||||
| Trial Visits | Four- to eight-week intervals for a total of 44 weeks | 6: 0, randomization, 3,6,9 and 12 months. | 1, 3, 6, 9, and 12 months | |||||||
| Masking | Yes | One unmasked study staff assigned to each provider office for randomization, procedures and deal with assignment related tasks. | Yes | |||||||
| Treatment duration | 44 weeks | 12 Months | 12 months | |||||||
| Groups | 1. Placebo bd with placebo plus albuterol (2 puff 180 μg) as-needed. PLACEBO GROUP (ALB) | n = 74 | ||||||||
| Received treatment = 74 | ||||||||||
| Completed treatment = 50 | ||||||||||
| 2. Placebo bd with BDP plus albuterol as-needed. RESCUE BDP GROUP | n = 71 | 1. BDP 40 mcg two puffs each time they needed to take albuterol. Symptom-based adjustment. SBA GROUP. | n = 103 | |||||||
| Received treatment = 71 | Received treatment 103 | |||||||||
| Completed treatment = 58 | Completed treatment = 87. Analyzed: 103 | |||||||||
| 3. BDP bd (40 mcgs 1 puff) with placebo plus albuterol as-needed (2 puff 180 μg). DAILY BDP GROUP | n = 72 | 2. BDP 40 mcg one puff bd (6–11 years) and 40 mcg two puffs bd (≥12 year) Provider-based guideline-directed adjustment PBA GROUP. | n = 103 | |||||||
| Received treatment = 72 | Received treatment 103 | |||||||||
| Completed treatment = 63 | Completed treatment = 92. Analyzed: 103 | |||||||||
| 4. BDP bd (40 mcgs 1 puff), with BDP (2 puff 40 mcgs each) plus albuterol (2 puff 180 μg) as rescue. COMBINED GROUP | n = 71 | |||||||||
| Received treatment = 71 | ||||||||||
| Completed treatment = 63 | ||||||||||
| BUD/FORM Turbuhaler 80/4.5 μg qd plus additional doses as needed (SMART) | n = 106 | |||||||||
| Received treatment = 106 | ||||||||||
| Completed treatmente = 92 Anallyzed = 106 | ||||||||||
| BUD/FORM 80/4.5 μg qd plus terbutaline 0.4 mg for rescue (FIXED-COMBINATION GROUP) | n = 117 | |||||||||
| Received treatment = 117 | ||||||||||
| Completed treatmente = 107 Anallyzed = 117 | ||||||||||
| Fourfold-higher maintenance dose of BUD 320 μg qd plus terbutaline 0.4 mg for rescue (FIXED-DOSE BUDESONIDE GROUP). | n = 118 | |||||||||
| Received treatment = 118 | ||||||||||
| Completed treatmente = 109 Anallyzed = 18 | ||||||||||
| Primary outcome variable | Time to first exacerbation that required treatment with prednisone. | ACT and cACT from baseline to 12 months. | Time to first exacerbation | |||||||
| SABA Alone vs. ICS + SABA | Regular ICS Treatment vs. ICS + SABA as Needed | SMART vs. Regular ICS Treatment + Terbutaline vs. Forudold-Higer ICS Treatment | |||
|---|---|---|---|---|---|
| TREXA 2011 [13] | TREXA 2011 [13] | SUMINO 2019 [14] | BISGAARD 2006 [15] | ||
| Symptoms | Exacerbations | RESCUE BDP GROUP better than PLACEBO GROUP HR (0.62 0.37–1.05, p = 0.073). | ND | No significant difference SBA GROUP vs. PBA GROUP p = 0.62 | SMART better than FIXED-COMBINATION GROUP (p < 0.001) and FIXED-DOSE BUDESONIDE (p = 0.022) (0.41, 0.76, 0.48) |
| Time to the first exacerbation | No difference between RESCUE BDP GROUP vs. PLACEBO GROUP HR 0.62 (0.37–1.05) p = 0.073 | RESCUE BDP GROUP trend worse than DAILY BDP GROUP (NSR) | No significant difference SBA GROUP vs. PBA GROUP p = 0.49 | SMART betther than FIXED-COMBINATION GROUP (p < 0.001) and FIXED-DOSE BUDESONIDE GROUP (p = 0.02) | |
| ACQ-5 score | ND | ND | No significant difference between SBA GROUP vs. PBA GROUP p = 0.10 | ND | |
| Asthma Control Days | No difference reported between groups. | No difference between RESCUE BDP GROUP vs. DAILY BDP GROUP | ND | FIXED-DOSE BUDESONIDE GROUP trends to be better than SMART (p = 0.14) and FIXED-COMBINATION GROUP (p = 0.6) (50.8 vs. 57.0 vs. 60.6) | |
| Self-reported, missed school days per year | ND | ND | No significant difference between SBA GROUP vs. PBA GROUP p = 0.84 | ND | |
| Pulmonary function test | FEV1 | RESCUE BDP GROUP trends better than PLACEBO GROUP (SNR) | RESCUE BDP GROUP and PLACEBO GROUP worse than DAILY BDP GROUP and COMBINED GROUP p = 0·024 | No significant difference between SBA GROUP vs. PBA GROUP p = 0.14 | FIXED-COMBINATION GROUP trends to be better than FIXED-DOSE BUDESONIDE GROUP (p = 0.43) and SMART (p = 0.094) (1.70 L vs. 1.76 L vs. 1.86 L) |
| Morning PEF | No difference reported between groups. | No difference reported between groups. | ND | SMART better than FIXED-DOSE BUDESONIDE GROUP (p = 0.0019) and trends to be better than FIXED-COMBINATION GROUP (p = 0.22) (255 vs. 238 vs. 242 L/min) | |
| FENO | No difference between RESCUE BDP GROUP vs. PLACEBO GROUP (SNR) | RESCUE BDP GROUP and PLACEBO GROUP worse than DAILY BDP GROUP and COMBINED GROUP | ND | ND | |
| Methacholine bronchial responsiveness | No difference between groups. | No difference between groups. | ND | ND | |
| Rescue medication | Beta-agonist-containing actuations per day | ND | RESCUE BDP GROUP trend worse than DAILY BDP GROUP (SNR) | ND | ND |
| Glucocorticoid treatment | ICS metered dose (μg) | ND | ND | SBA GROUP better than PBA GROUP p < 0.001 | FIXED-COMBINATION GROUP trends to be better than SMART and FIXED-DOSE BUDESONIDE GROUP (80 mcg/dia vs. 126/7.1 mcg/d vs. 320 mcg/d) (SNR) |
| Quality of life | AQLQ score | No difference reported between groups. | No difference reported between groups. | No significant difference SBA GROUP. vs. PBA GROUP | ND |
| Adverse events | Adverse events | ND | ND | No significant difference SBA GROUP vs. PBA GROUP (SNR) | SMART trends to be better than FIXED-DOSE BUDESONIDE GROUP and FIXED-COMBINATION GROUP (2, 5, 16) (SNR) |
| Discontinuation due to study-specific asthma-related events | ND | ND | No significant difference SBA GROUP vs. PBA GROUP | ND | |
| Linear Growth | No difference between RESCUE BDP GROUP vs. PLACEBO GROUP −0.3 cm (0.2) p = 0.26 | RESCUE BDP GROUP trends better than DAILY BDP GROUP (SNR) | ND | SMART better than FIXED-DOSE BUDESONIDE GROUP p < 0.01 5.3 (1.0–14.0) vs. 4.3 (−2.0–15.0) FIXED-COMBINATION GROUP better than FIXED-DOSE BUDESONIDE GROUP p < 0.01 5.4 (−4.0–12.0) vs. 5.3 (1.0–14.0) | |
| Treatment failures | ND | No significance is reported between groups | ND | ND | |
| Adherence | Adherence to the twice-daily, blinded maintenance regimen | ND | ND | ND | ND |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarrete-Rodríguez, E.M.; Del-Rio-Navarro, B.E.; Larenas-Linnemann, D.; Castro-Rodriguez, J.A. On-Demand ICS + FABA Combinations in 6–11-Year-Old Children. J. Clin. Med. 2023, 12, 7270. https://doi.org/10.3390/jcm12237270
Navarrete-Rodríguez EM, Del-Rio-Navarro BE, Larenas-Linnemann D, Castro-Rodriguez JA. On-Demand ICS + FABA Combinations in 6–11-Year-Old Children. Journal of Clinical Medicine. 2023; 12(23):7270. https://doi.org/10.3390/jcm12237270
Chicago/Turabian StyleNavarrete-Rodríguez, Elsy M., Blanca E. Del-Rio-Navarro, Désirée Larenas-Linnemann, and Jose A. Castro-Rodriguez. 2023. "On-Demand ICS + FABA Combinations in 6–11-Year-Old Children" Journal of Clinical Medicine 12, no. 23: 7270. https://doi.org/10.3390/jcm12237270
APA StyleNavarrete-Rodríguez, E. M., Del-Rio-Navarro, B. E., Larenas-Linnemann, D., & Castro-Rodriguez, J. A. (2023). On-Demand ICS + FABA Combinations in 6–11-Year-Old Children. Journal of Clinical Medicine, 12(23), 7270. https://doi.org/10.3390/jcm12237270







