Correlation between Ankle Imaging Findings and Self-Reported Outcomes: A Longitudinal Assessment in Patients with Tibiofibular Diastasis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Inclusion and Exclusion Criteria
2.3. Data Acquisition and Surveys
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Ultrasound and Radiographic Measurements
3.3. Survey Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Medina McKeon, J.M.; Hoch, M.C. The Ankle-Joint Complex: A Kinesiologic Approach to Lateral Ankle Sprains. J. Athl. Train. 2019, 54, 589–602. [Google Scholar] [CrossRef]
- Li, L.; Gollhofer, A.; Lohrer, H.; Dorn-Lange, N.; Bonsignore, G.; Gehring, D. Function of ankle ligaments for subtalar and talocrural joint stability during an inversion movement—An in vitro study. J. Foot Ankle Res. 2019, 12, 16. [Google Scholar] [CrossRef]
- Porter, D.A.; Jaggers, R.R.; Barnes, A.F.; Rund, A.M. Optimal management of ankle syndesmosis injuries. Open Access J. Sports Med. 2014, 5, 173–182. [Google Scholar] [CrossRef]
- Pajaczkowski, J.A. Rehabilitation of distal tibiofibular syndesmosis sprains: A case report. J. Can. Chiropr. Assoc. 2007, 51, 42–49. [Google Scholar]
- Patel, P.; Russell, T.G. Ankle Radiographic Evaluation; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557462/ (accessed on 24 April 2023).
- Pop, D.L.; Nodiţi, G.; Abu-Awwad, A.; Maliţa, D.C.; Zamfir, C.L.; Grigoraş, M.L.; Vermeşan, D.; Prejbeanu, R.; Hărăguş, H.G.; Boşcu, A.L.; et al. Alveolar rhabdomyosarcoma in an adolescent male patient—Case report and current perspectives. Rom. J. Morphol. Embryol. 2018, 59, 1247–1252. [Google Scholar]
- Song, J.H.; Moon, J.J.; Shin, W.J.; Ko, K.P. Use of a comprehensive systemic ultrasound evaluation in the diagnosis and analysis of acute lateral region ankle sprain. BMC Musculoskelet. Disord. 2023, 24, 517. [Google Scholar] [CrossRef]
- Faur, C.I.; Abu-Awwad, A.; Pop, D.L.; Zamfir, C.L.; Gurgus, D.; Hoinoiu, T.; Motoc, A.; Haivas, C.; Grigoraș, M.L.; Folescu, R. Liquid Nitrogen Efficiency in Treatment of Giant Cell Tumor of Bone and Prevention of Recurrence. Appl. Sci. 2020, 10, 6310. [Google Scholar] [CrossRef]
- Siriwanarangsun, P.; Bae, W.C.; Statum, S.; Chung, C.B. Advanced MRI Techniques for the Ankle. AJR Am. J. Roentgenol. 2017, 209, 511–524. [Google Scholar] [CrossRef]
- Gorbachova, T. Magnetic resonance imaging of the ankle and foot. Pol. J. Radiol. 2020, 85, e532–e549. [Google Scholar] [CrossRef]
- Wright, D.J.; Bariteau, J.T.; Hsu, A.R. Advances in the Surgical Management of Ankle Fractures. Foot Ankle Orthop. 2019, 4, 2473011419888505. [Google Scholar] [CrossRef]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef] [PubMed]
- Polzer, H.; Kanz, K.G.; Prall, W.C.; Haasters, F.; Ockert, B.; Mutschler, W.; Grote, S. Diagnosis and treatment of acute ankle injuries: Development of an evidence-based algorithm. Orthop. Rev. 2012, 4, e5. [Google Scholar] [CrossRef]
- Foni, N.O.; Costa, L.A.V.; Velloso, L.M.R.; Pedrotti, C.H.S. Telemedicine: Is It a Tool for Orthopedics? Curr. Rev. Musculoskelet. Med. 2020, 13, 797–801. [Google Scholar] [CrossRef]
- Nguyen, M.Q.; Dalen, I.; Iversen, M.M.; Harboe, K.; Paulsen, A. Ankle fractures: A systematic review of patient-reported outcome measures and their measurement properties. Qual. Life Res. 2023, 32, 27–45. [Google Scholar] [CrossRef]
- Picot, B.; Hardy, A.; Terrier, R.; Tassignon, B.; Lopes, R.; Fourchet, F. Which Functional Tests and Self-Reported Questionnaires Can Help Clinicians Make Valid Return to Sport Decisions in Patients with Chronic Ankle Instability? A Narrative Review and Expert Opinion. Front. Sports Act. Living 2022, 4, 902886. [Google Scholar] [CrossRef]
- Inge, S.Y.; Pull Ter Gunne, A.F.; Aarts, C.A.M.; Bemelman, M. A systematic review on dynamic versus static distal tibiofibular fixation. Injury 2016, 47, 2627–2634. [Google Scholar] [CrossRef]
- Umucu, E.; Reyes, A.; Carrola, P.; Mangadu, T.; Lee, B.; Brooks, J.M.; Fortuna, K.L.; Villegas, D.; Chiu, C.Y.; Valencia, C. Pain intensity and mental health quality of life in veterans with mental illnesses: The intermediary role of physical health and the ability to participate in activities. Qual. Life Res. 2021, 30, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.; Donisi, V.; Battista, S.; Picelli, A.; Valè, N.; Del Piccolo, L.; Smania, N. Health-Related Quality of Life and Psychological Features in Post-Stroke Patients with Chronic Pain: A Cross-Sectional Study in the Neuro-Rehabilitation Context of Care. Int. J. Environ. Res. Public Health 2021, 18, 3089. [Google Scholar] [CrossRef]
- Ferreira, D.C.; Vieira, I.; Pedro, M.I.; Caldas, P.; Varela, M. Patient Satisfaction with Healthcare Services and the Techniques Used for its Assessment: A Systematic Literature Review and a Bibliometric Analysis. Healthcare 2023, 11, 639. [Google Scholar] [CrossRef]
- Houston, M.N.; Van Lunen, B.L.; Hoch, M.C. Health-related quality of life in individuals with chronic ankle instability. J. Athl. Train. 2014, 49, 758–763. [Google Scholar] [CrossRef]
- Houston, M.N.; Hoch, J.M.; Hoch, M.C. Patient-Reported Outcome Measures in Individuals with Chronic Ankle Instability: A Systematic Review. J. Athl. Train. 2015, 50, 1019–1033. [Google Scholar] [CrossRef] [PubMed]
- Steindel, S.J. International classification of diseases, 10th edition, clinical modification and procedure coding system: Descriptive overview of the next generation HIPAA code sets. J. Am. Med. Inform. Assoc. 2010, 17, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef]
- Gimber, L.H.; Daniel Latt, L.; Caruso, C.; Nuncio Zuniga, A.A.; Krupinski, E.A.; Klauser, A.S.; Taljanovic, M.S. Ultrasound shear wave elastography of the anterior talofibular and calcaneofibular ligaments in healthy subjects. J. Ultrason. 2021, 21, e86–e94. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [PubMed]
- Rishi, P.; Rishi, E.; Maitray, A.; Agarwal, A.; Nair, S.; Gopalakrishnan, S. Hospital anxiety and depression scale assessment of 100 patients before and after using low vision care: A prospective study in a tertiary eye-care setting. Indian J. Ophthalmol. 2017, 65, 1203–1208. [Google Scholar] [CrossRef]
- Wong, F.Y.; Yang, L.; Yuen, J.W.M.; Chang, K.K.P.; Wong, F.K.Y. Assessing quality of life using WHOQOL-BREF: A cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. BMC Public Health 2018, 18, 1113. [Google Scholar] [CrossRef]
- Ryu, J.; Jeong, W.K. Current status of musculoskeletal application of shear wave elastography. Ultrasonography 2017, 36, 185–197. [Google Scholar] [CrossRef]
- Lima, K.M.M.E.; Costa Júnior, J.F.S.; Pereira, W.C.A.; Oliveira, L.F. Assessment of the mechanical properties of the muscle-tendon unit by supersonic shear wave imaging elastography: A review. Ultrasonography 2018, 37, 3–15. [Google Scholar] [CrossRef]
- Yang, H.; Su, M.; Chen, Z.; Qu, R.; Yuan, Z.; Yuan, J.; He, S.; Li, Z.; Liu, C.; Xiao, Z.; et al. Anatomic Measurement and Variability Analysis of the Anterior Talofibular Ligament and Calcaneofibular Ligament of the Ankle. Orthop. J. Sports Med. 2021, 9, 23259671211047269. [Google Scholar] [CrossRef]
- Grewal, U.S.; Southgate, C.; Dhinsa, B.S. Sub-Acute Syndesmotic Injury: A Review and Proposed Treatment Algorithm. Cureus 2021, 13, e16670. [Google Scholar] [CrossRef]
- Großterlinden, L.G.; Hartel, M.; Yamamura, J.; Schoennagel, B.; Bürger, N.; Krause, M.; Spiro, A.; Hoffmann, M.; Lehmann, W.; Rueger, J.M.; et al. Isolated syndesmotic injuries in acute ankle sprains: Diagnostic significance of clinical examination and MRI. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2016, 24, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Hermans, J.J.; Wentink, N.; Beumer, A.; Hop, W.C.; Heijboer, M.P.; Moonen, A.F.; Ginai, A.Z. Correlation between radiological assessment of acute ankle fractures and syndesmotic injury on MRI. Skelet. Radiol. 2012, 41, 787–801. [Google Scholar] [CrossRef] [PubMed]
- Schepers, T. To retain or remove the syndesmotic screw: A review of literature. Arch. Orthop. Trauma Surg. 2011, 131, 879–883. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, S.A.; Birnie, M.F.N.; Sanders, F.R.K.; Bekerom, M.P.J.v.D.; Backes, M.; van Beeck, E.; Bloemers, F.W.; van Dijkman, B.; Flikweert, E.; Haverkamp, D.; et al. Routine versus on demand removal of the syndesmotic screw; a protocol for an international randomised controlled trial (RODEO-trial). BMC Musculoskelet. Disord. 2018, 19, 35. [Google Scholar] [CrossRef]
- Hayden, R.; Rucinski, K.; Crecelius, C.R.; Stucky, R.; Stannard, J.P.; Cook, J.L. Outcomes associated with behavioral evaluation and counseling for patients undergoing orthopaedic surgery—A systematic review. J. Orthop. 2020, 21, 178–182. [Google Scholar] [CrossRef]
- Garverich, S.; Prener, C.G.; Guyer, M.E.; Lincoln, A.K. What matters: Factors impacting the recovery process among outpatient mental health service users. Psychiatr. Rehabil. J. 2021, 44, 77–86. [Google Scholar] [CrossRef]
- Tadesse, M.; Ahmed, S.; Regassa, T.; Girma, T.; Hailu, S.; Mohammed, A.; Mohammed, S. Effect of preoperative anxiety on postoperative pain on patients undergoing elective surgery: Prospective cohort study. Ann. Med. Surg. 2021, 73, 103190. [Google Scholar] [CrossRef]
- Takemoto, E.; Wolfe, B.M.; Nagel, C.L.; Boone-Heinonen, J. Physical and Mental Health-Related Quality of Life Changes Among Insurer Subgroups Following Bariatric Surgery. Obesity 2020, 28, 669–675. [Google Scholar] [CrossRef]
- Zhang, Z.; Xing, Q.; Zhong, D.; Pan, Y.; He, T.; Hu, Y.; Wang, L. The Impact of Psychological Health on Patient Recovery After Arthroplasty. Front. Psychiatry 2022, 13, 817716. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Silvestri, C.A.; Manzi, L.; Indino, C.; Maccario, C.; Usuelli, F.G. Post-traumatic ankle osteoarthritis: Quality of life, frequency and associated factors. Muscle Ligaments Tendons J. 2019, 9, 363–371. [Google Scholar] [CrossRef]
- Efrima, B.; Barbero, A.; Ovadia, J.E.; Indino, C.; Maccario, C.; Usuelli, F.G. Reliability of Cone Beam Weightbearing Computed Tomography Analysis of Total Ankle Arthroplasty Positioning and Comparison to Weightbearing X-Ray Measurements. Foot Ankle Int. 2023, 44, 637–644. [Google Scholar] [CrossRef] [PubMed]



| Variables | Screw Removal (n = 85) | Non Screw Removal (n = 44) | p-Value * |
|---|---|---|---|
| Age, years | 34.7 ± 13.3 | 35.4 ± 14.8 | 0.786 |
| Sex (men, %) | 51 (60.0%) | 20 (45.5%) | 0.092 |
| Overweight (>25.0 kg/m2) | 33 (38.8%) | 21 (47.7%) | 0.327 |
| Smoking | 22 (25.9%) | 15 (34.1%) | 0.392 |
| CCI > 2 | 7 (8.2%) | 3 (6.8%) | 0.542 |
| Fracture type | 0.753 | ||
| Unimalleolar | 22 (25.9% | 11 (25.0%) | |
| Bimalleolar | 45 (52.9%) | 20 (45.5%) | |
| Trimalleolar | 18 (21.2%) | 13 (29.5%) | |
| Lauge–Hansen classification | 0.182 | ||
| SER | 38 (44.7%) | 15 (34.1%) | |
| PER | 27 (31.8%) | 12 (27.3%) | |
| SA | 9 (10.6%) | 10 (22.7%) | |
| PA | 11 (12.9%) | 7 (15.9%) |
| Variables | Screw Removal (n = 85) | Non Screw Removal (n = 44) | p-Value * |
|---|---|---|---|
| At 2 months | |||
| Ultrasound (SW velocity **) | |||
| Ankle dorsiflexion | 8.9 ± 1.4 | 10.1 ± 1.8 | <0.001 |
| ATFL | 2.8 ± 0.9 | 3.3 ± 1.3 | 0.012 |
| CFL | 3.0 ± 1.2 | 3.6 ± 1.3 | 0.010 |
| Radiographic changes *** | |||
| TOL | 8.0 ± 2.1 | 8.9 ± 1.6 | 0.014 |
| TCS | 3.4 ± 0.9 | 3.9 ± 1.1 | 0.007 |
| IFD | 4.0 ± 1.2 | 4.3 ± 0.8 | 0.138 |
| At 6 months | |||
| Ultrasound (SW velocity) | |||
| Ankle dorsiflexion | 8.6 ± 1.1 | 9.5 ± 1.3 | <0.001 |
| ATFL | 2.6 ± 0.9 | 2.9 ± 1.0 | 0.086 |
| CFL | 2.8 ± 1.3 | 3.1 ± 0.9 | 0.173 |
| Radiographic changes | |||
| TOL | 8.3 ± 1.6 | 8.8 ± 2.0 | 0.125 |
| TCS | 3.5 ± 1.0 | 4.0 ± 1.1 | 0.010 |
| IFD | 4.1 ± 1.5 | 4.4 ± 1.2 | 0.252 |
| Scores (Mean ± SD) | Screw Removal (n = 85) | Non Screw Removal (n = 44) | p-Value * |
|---|---|---|---|
| At 2 months | |||
| SF-36—Physical | 55.6 ± 6.4 | 52.1 ± 6.8 | 0.005 |
| SF-36—Mental | 54.0 ± 7.5 | 52.2 ± 7.2 | 0.192 |
| SF-36—Total | 56.1 ± 7.2 | 54.0 ± 7.6 | 0.125 |
| At 6 months | |||
| SF-36—Physical | 56.4 ± 6.6 | 53.7 ± 7.0 | 0.032 |
| SF-36—Mental | 54.8 ± 7.0 | 53.2 ± 6.9 | 0.218 |
| SF-36—Total | 56.7 ± 7.4 | 54.3 ± 7.5 | 0.084 |
| WHOQOL-BREF (Mean ± SD) | Screw Removal (n = 85) | Non Screw Removal (n = 44) | p-Value * |
|---|---|---|---|
| At 2 months | |||
| Physical domain | 63.7 ± 11.9 | 59.7 ± 12.4 | 0.077 |
| Mental domain | 61.5 ± 14.1 | 65.0 ± 13.1 | 0.174 |
| Social domain | 59.3 ± 13.0 | 65.8 ± 12.8 | 0.008 |
| Environmental domain | 62.8 ± 12.1 | 60.5 ± 13.4 | 0.326 |
| At 6 months | |||
| Physical domain | 67.2 ± 11.7 | 61.6 ± 10.8 | 0.009 |
| Mental domain | 64.0 ± 13.4 | 66.3 ± 12.2 | 0.342 |
| Social domain | 62.5 ± 12.7 | 67.0 ± 12.9 | 0.060 |
| Environmental domain | 65.3 ± 11.4 | 63.2 ± 12.7 | 0.342 |
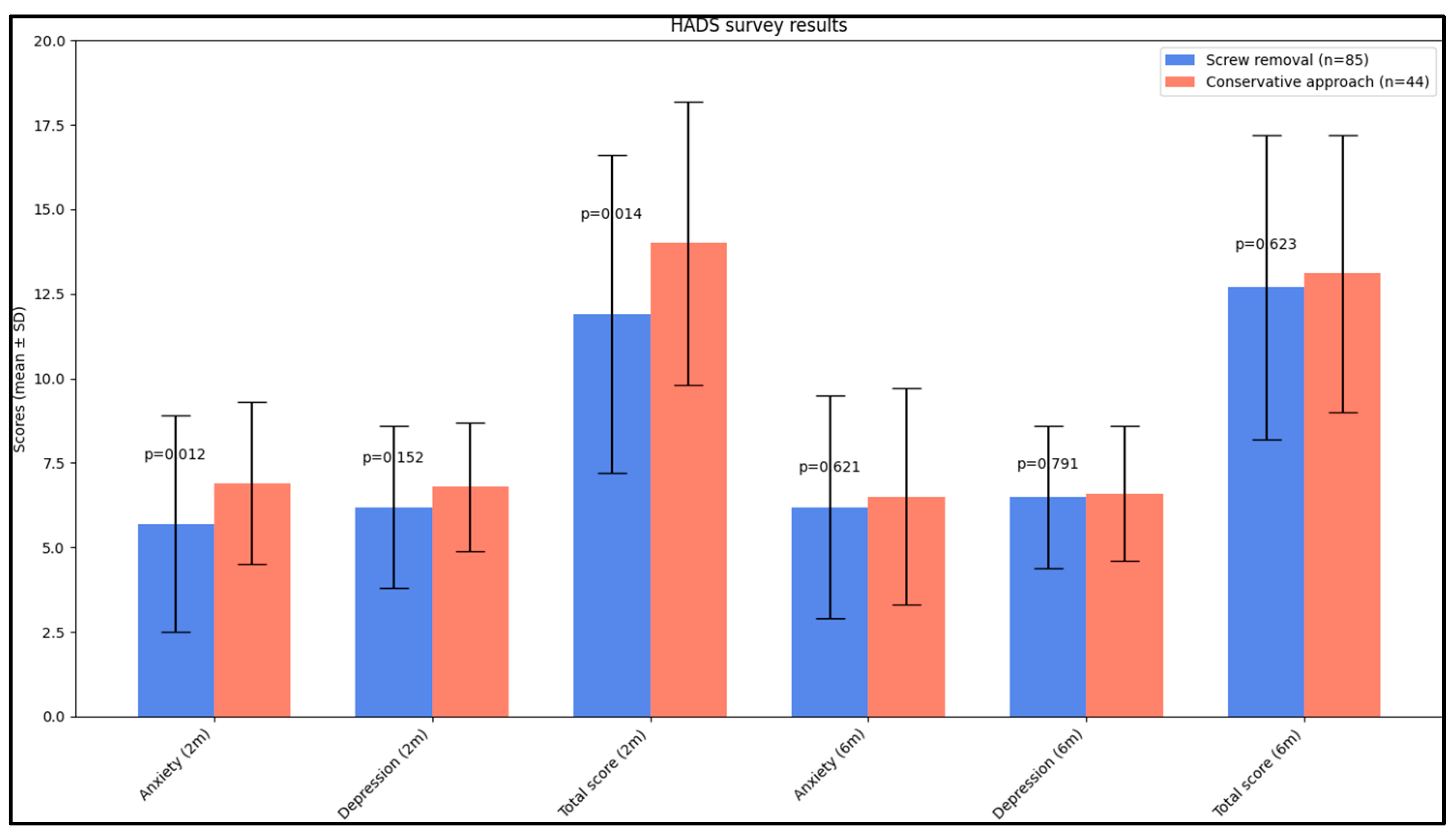
| HADS (Mean ± SD) | Screw Removal (n = 85) | Non Screw Removal (n = 44) | p-Value * |
|---|---|---|---|
| At 2 months | |||
| Anxiety | 5.6 ± 2.9 | 6.9 ± 2.4 | 0.012 |
| Depression | 6.2 ± 2.4 | 6.8 ± 1.9 | 0.152 |
| Total score | 11.9 ± 4.7 | 14.0 ± 4.2 | 0.014 |
| At 6 months | |||
| Anxiety | 6.2 ± 3.3 | 6.5 ± 3.2 | 0.621 |
| Depression | 6.5 ± 2.1 | 6.6 ± 2.0 | 0.791 |
| Total score | 12.7 ± 4.5 | 13.1 ± 4.1 | 0.623 |
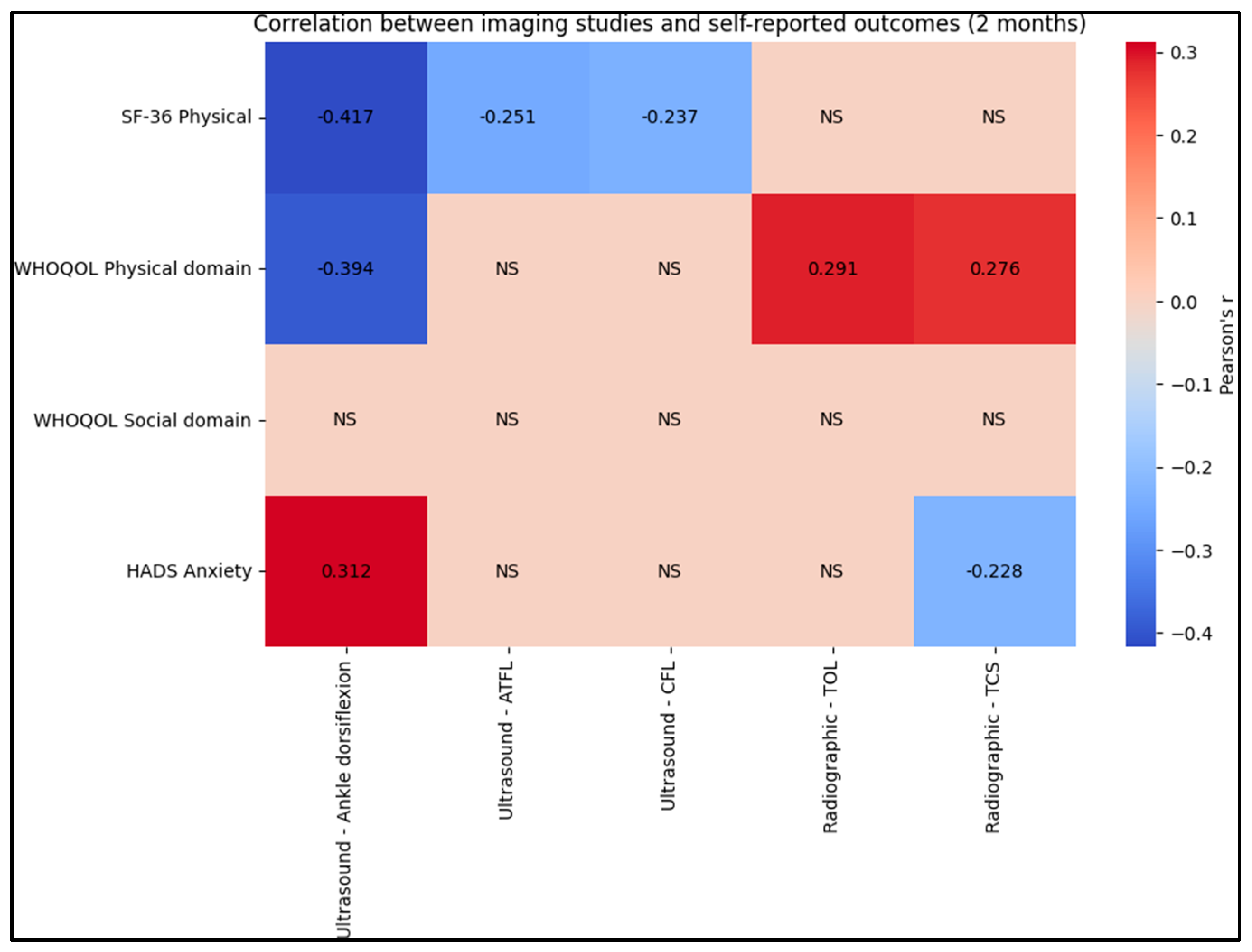
| Variables | Pearson’s r | p-Value |
|---|---|---|
| At 2 months | ||
| Ultrasound—Ankle dorsiflexion vs. SF-36 Physical | −0.417 | <0.001 |
| Ultrasound—Ankle dorsiflexion vs. WHOQOL Physical domain | −0.394 | 0.003 |
| Ultrasound—Ankle dorsiflexion vs. HADS Anxiety | 0.312 | 0.027 |
| Ultrasound—ATFL vs. SF-36 Physical | −0.251 | 0.019 |
| Ultrasound—CFL vs. SF-36 Physical | −0.237 | 0.023 |
| Radiographic—TOL vs. WHOQOL Physical domain | 0.291 | 0.016 |
| Radiographic—TCS vs. WHOQOL Physical domain | 0.276 | 0.021 |
| Radiographic—TCS vs. HADS Anxiety | −0.228 | 0.033 |
| At 6 months | ||
| Ultrasound—Ankle dorsiflexion vs. SF-36 Physical | −0.408 | <0.001 |
| Ultrasound—Ankle dorsiflexion vs. WHOQOL Physical domain | −0.383 | 0.004 |
| Ultrasound—Ankle dorsiflexion vs. HADS Anxiety | 0.295 | 0.038 |
| Ultrasound—ATFL vs. WHOQOL Physical domain | −0.211 | 0.054 |
| Radiographic—TCS vs. SF-36 Physical | 0.244 | 0.026 |
| Radiographic—TCS vs. WHOQOL Physical domain | 0.233 | 0.031 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosin, S.; Vermesan, D.; Deleanu, B.; Pop, D.; Crisan, D.; Al-Qatawneh, M.; Mioc, M.; Faur, C.; Rosca, O.; Prejbeanu, R. Correlation between Ankle Imaging Findings and Self-Reported Outcomes: A Longitudinal Assessment in Patients with Tibiofibular Diastasis. J. Clin. Med. 2023, 12, 7239. https://doi.org/10.3390/jcm12237239
Hosin S, Vermesan D, Deleanu B, Pop D, Crisan D, Al-Qatawneh M, Mioc M, Faur C, Rosca O, Prejbeanu R. Correlation between Ankle Imaging Findings and Self-Reported Outcomes: A Longitudinal Assessment in Patients with Tibiofibular Diastasis. Journal of Clinical Medicine. 2023; 12(23):7239. https://doi.org/10.3390/jcm12237239
Chicago/Turabian StyleHosin, Samer, Dinu Vermesan, Bogdan Deleanu, Daniel Pop, Dan Crisan, Musab Al-Qatawneh, Mihai Mioc, Cosmin Faur, Ovidiu Rosca, and Radu Prejbeanu. 2023. "Correlation between Ankle Imaging Findings and Self-Reported Outcomes: A Longitudinal Assessment in Patients with Tibiofibular Diastasis" Journal of Clinical Medicine 12, no. 23: 7239. https://doi.org/10.3390/jcm12237239
APA StyleHosin, S., Vermesan, D., Deleanu, B., Pop, D., Crisan, D., Al-Qatawneh, M., Mioc, M., Faur, C., Rosca, O., & Prejbeanu, R. (2023). Correlation between Ankle Imaging Findings and Self-Reported Outcomes: A Longitudinal Assessment in Patients with Tibiofibular Diastasis. Journal of Clinical Medicine, 12(23), 7239. https://doi.org/10.3390/jcm12237239







