A Modified 90-Degree Distal Chevron Metatarsal Osteotomy for Correcting Moderate Hallux Valgus Deformity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
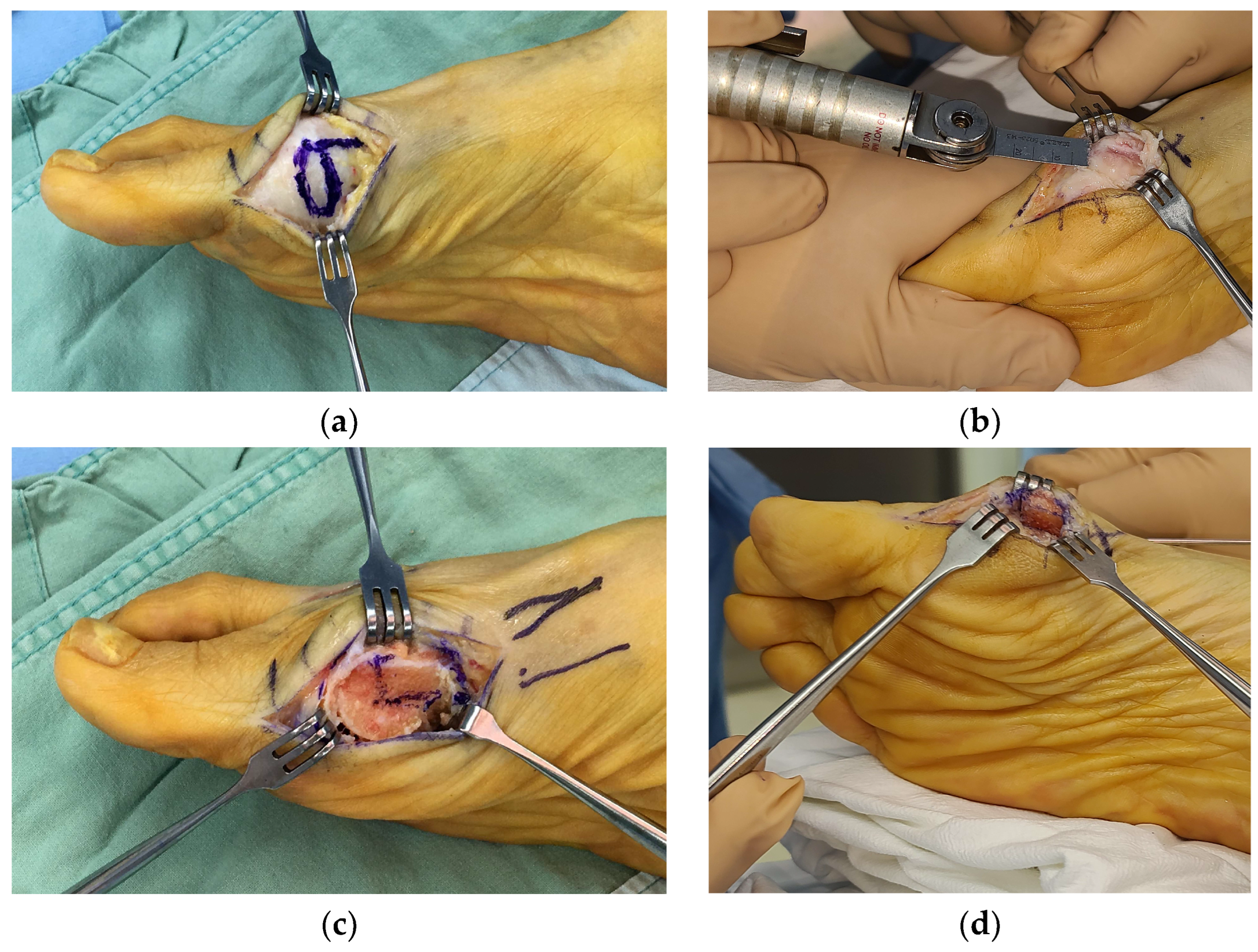
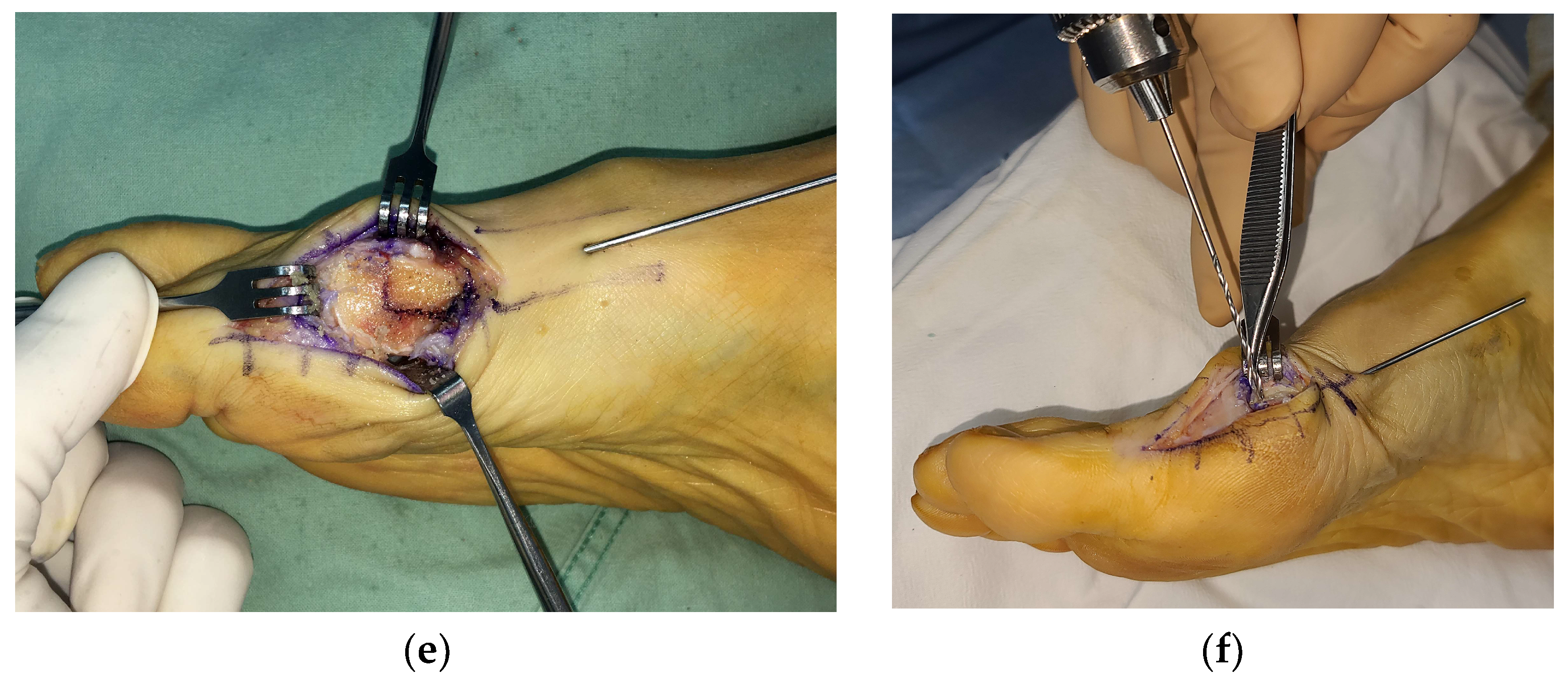
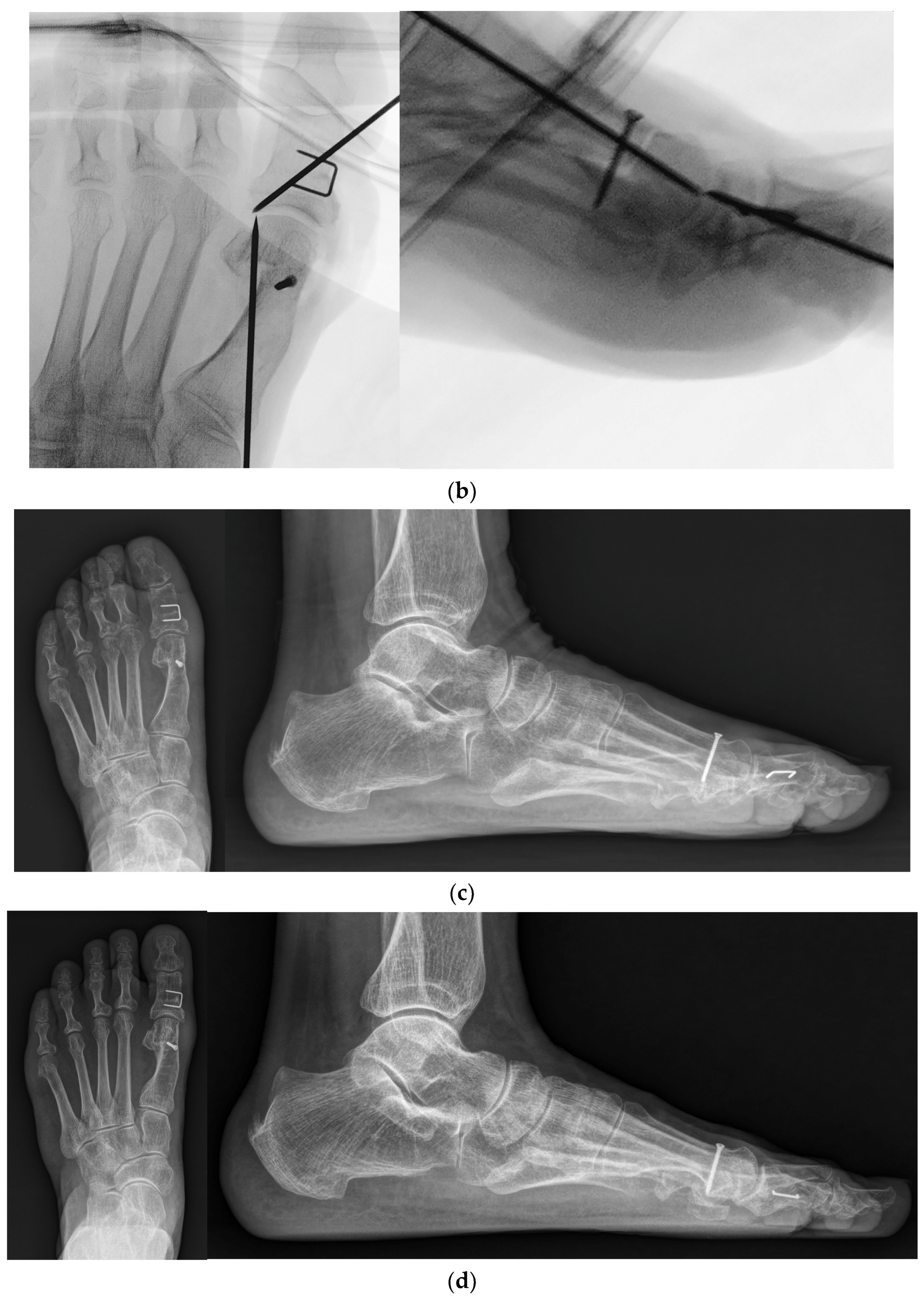
2.2. Surgical Procedures
2.3. Postoperative Management
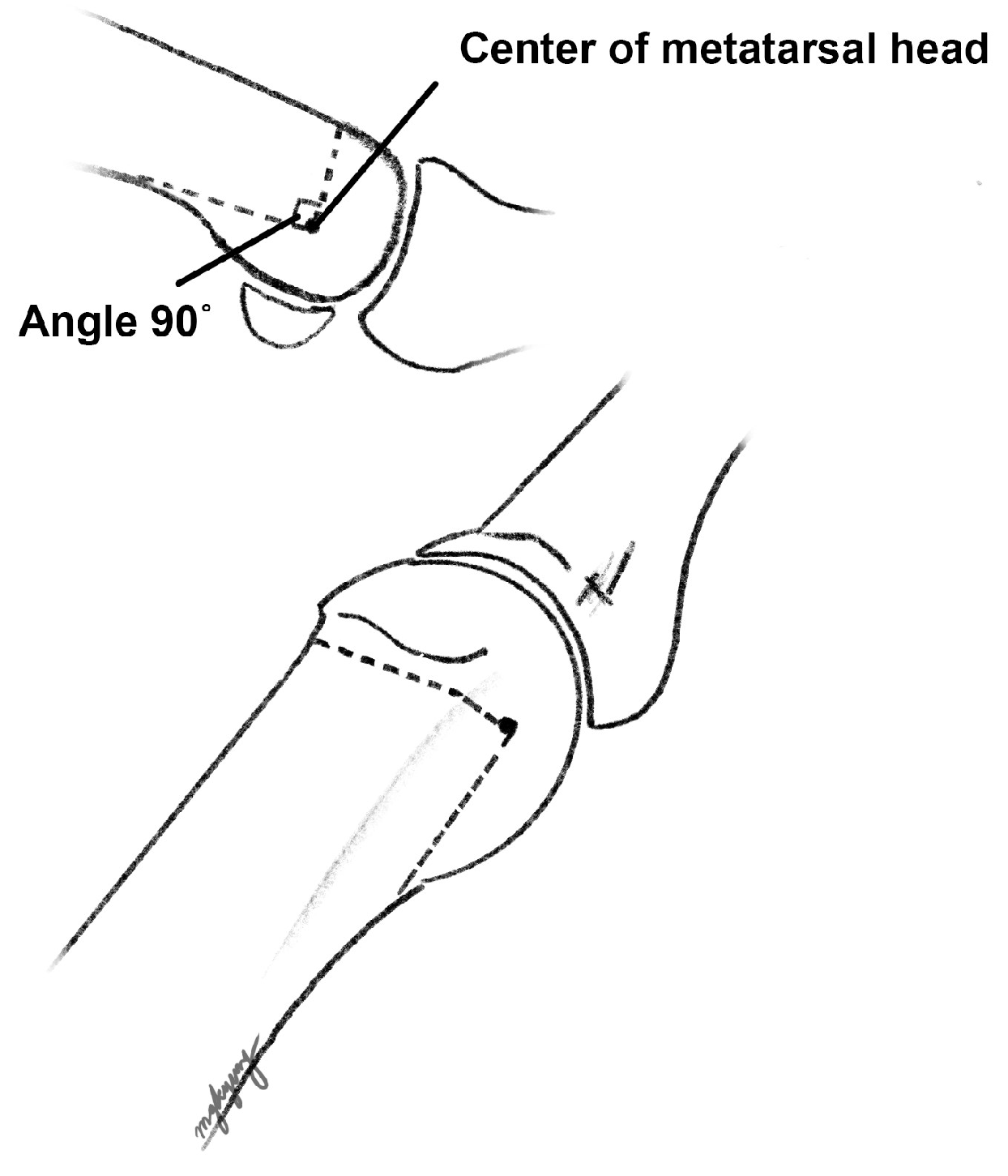
2.4. Radiographic Outcome Assessment
2.5. Statistical Analysis
3. Results
3.1. Radiographic Outcome
3.2. Postoperative Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ray, J.J.; Friedmann, A.J.; Hanselman, A.E.; Vaida, J.; Dayton, P.D.; Hatch, D.J.; Smith, B.; Santrock, R.D. Hallux Valgus. Foot Ankle Orthop. 2019, 4, 2473011419838500. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.H.; Limbers, J.P. Modern concepts in the treatment of hallux valgus. J. Bone Jt. Surg. Br. 2005, 87, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Coull, R.; Stephens, M.M. Operative decision making in hallux valgus. Curr. Orthop. 2002, 16, 180–186. [Google Scholar] [CrossRef]
- Pinney, S.; Song, K.; Chou, L. Surgical treatment of mild hallux valgus deformity: The state of practice among academic foot and ankle surgeons. Foot Ankle Int. 2006, 27, 970–973. [Google Scholar] [CrossRef] [PubMed]
- Trnka, H.J.; Zembsch, A.; Easley, M.E.; Salzer, M.; Ritschl, P.; Myerson, M.S. The chevron osteotomy for correction of hallux valgus. Comparison of findings after two and five years of follow-up. J. Bone Jt. Surg. Am. 2000, 82, 1373–1378. [Google Scholar] [CrossRef]
- Murawski, D.E.; Beskin, J.L. Increased displacement maximizes the utility of the distal chevron osteotomy for hallux valgus deformity correction. Foot Ankle Int. 2008, 29, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Gross, C.E.; Parekh, S.G. Short-Term Radiographic Outcome After Distal Chevron Osteotomy for Hallux Valgus Using Intramedullary Plates With an Amended Algorithm for the Surgical Management of Hallux Valgus. Foot Ankle Spec. 2019, 12, 25–33. [Google Scholar] [CrossRef]
- Choi, Y.R.; Lee, S.J.; Kim, J.H.; Kim, T.H.; Oh, C.H. Effect of metatarsal osteotomy and open lateral soft tissue procedure on sesamoid position: Radiological assessment. J. Orthop. Surg. Res. 2018, 13, 11. [Google Scholar] [CrossRef]
- Coughlin, M.J. Hallux valgus in men: Effect of the distal metatarsal articular angle on hallux valgus correction. Foot Ankle Int. 1997, 18, 463–470. [Google Scholar] [CrossRef]
- Huang, E.H.; Charlton, T.P.; Ajayi, S.; Thordarson, D.B. Effect of various hallux valgus reconstruction on sesamoid location: A radiographic study. Foot Ankle Int. 2013, 34, 99–103. [Google Scholar] [CrossRef]
- Easley, M.E.; Kelly, I.P. Avascular necrosis of the hallux metatarsal head. Foot Ankle Clin. 2000, 5, 591–608. [Google Scholar] [PubMed]
- Williams, W.W.; Barrett, D.S.; Copeland, S.A. Avascular necrosis following chevron distal metatarsal osteotomy: A significant risk? J. Foot Surg. 1989, 28, 414–416. [Google Scholar] [PubMed]
- Espinosa, N.; Meyer, D.C.; Von Campe, A.; Helmy, N.; Vienne, P. A New Modified Distal First Metatarsal Osteotomy for the Treatment of Hallux Valgus Deformity: The Reversed L-shaped Osteotomy. Tech. Foot Ankle Surg. 2006, 5, 190–197. [Google Scholar] [CrossRef]
- Donnelly, R.E.; Saltzman, C.L.; Kile, T.A.; Johnson, K.A. Modified chevron osteotomy for hallux valgus. Foot Ankle Int. 1994, 15, 642–645. [Google Scholar] [CrossRef]
- Iliou, K.; Paraskevas, G.; Kanavaros, P.; Barbouti, A.; Vrettakos, A.; Gekas, C.; Kitsoulis, P. Correlation between Manchester Grading Scale and American Orthopaedic Foot and Ankle Society Score in Patients with Hallux Valgus. Med. Princ. Pract. 2016, 25, 21–24. [Google Scholar] [CrossRef]
- Meier, P.J.; Kenzora, J.E. The risks and benefits of distal first metatarsal osteotomies. Foot Ankle 1985, 6, 7–17. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Saltzman, C.L.; Nunley, J.A., 2nd. Angular measurements in the evaluation of hallux valgus deformities: A report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002, 23, 68–74. [Google Scholar]
- Hardy, R.H.; Clapham, J.C. Observations on hallux valgus; based on a controlled series. J. Bone Jt. Surg. Br. 1951, 33-B, 376–391. [Google Scholar] [CrossRef]
- Park, C.H.; Jang, J.H.; Lee, S.H.; Lee, W.C. A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. Bone Jt. J. 2013, 95-B, 649–656. [Google Scholar] [CrossRef]
- Austin, D.W.; Leventen, E.O. A new osteotomy for hallux valgus: A horizontally directed “V” displacement osteotomy of the metatarsal head for hallux valgus and primus varus. Clin. Orthop. Relat. Res. 1981, 157, 25–30. [Google Scholar] [CrossRef]
- Kalish, S.R.; Spector, J.E. The Kalish osteotomy. A review and retrospective analysis of 265 cases. J. Am. Podiatr. Med. Assoc. 1994, 84, 237–242. [Google Scholar] [PubMed]
- Youngswick, F.D. Modifications of the Austin bunionectomy for treatment of metatarsus primus elevatus associated with hallux limitus. J. Foot Surg. 1982, 21, 114–116. [Google Scholar]
- Jahss, M.H. Disorders of the hallux and the first ray. In Disorders of the Foot and Ankle: Medical and Surgical Management, 2nd ed.; Jahss, M.H., Ed.; WB Saunders Co: Philadelphia, PA, USA, 1991; pp. 943–946. [Google Scholar]
- Matzaroglou, C.; Bougas, P.; Panagiotopoulos, E.; Saridis, A.; Karanikolas, M.; Kouzoudis, D. Ninety-degree chevron osteotomy for correction of hallux valgus deformity: Clinical data and finite element analysis. Open Orthop. J. 2010, 4, 152–156. [Google Scholar] [CrossRef]
- DeOrio, J. Technique tip: Dorsal wedge resection (uniplanar) in the chevron osteotomy for high distal metatarsal articular angle bunions. Foot Ankle Int. 2007, 28, 642–644. [Google Scholar] [CrossRef]
- Hattrup, S.J.; Johnson, K.A. Chevron osteotomy: Analysis of factors in patients’ dissatisfaction. Foot Ankle 1985, 5, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Ezzatvar, Y.; Lopez-Bueno, L.; Fuentes-Aparicio, L.; Duenas, L. Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5753. [Google Scholar] [CrossRef] [PubMed]
- Dufour, A.B.; Casey, V.A.; Golightly, Y.M.; Hannan, M.T. Characteristics associated with hallux valgus in a population-based foot study of older adults. Arthritis Care Res. 2014, 66, 1880–1886. [Google Scholar] [CrossRef]
- Goh, G.S.; Tay, A.Y.W.; Thever, Y.; Koo, K. Effect of Age on Clinical and Radiological Outcomes of Hallux Valgus Surgery. Foot Ankle Int. 2021, 42, 798–804. [Google Scholar] [CrossRef]
- Aiyer, A.; Stewart, S.; Rome, K. The effect of age on muscle characteristics of the abductor hallucis in people with hallux valgus: A cross-sectional observational study. J. Foot Ankle Res. 2015, 8, 19. [Google Scholar] [CrossRef]
- Noyes, F.R.; Grood, E.S. The strength of the anterior cruciate ligament in humans and Rhesus monkeys. J. Bone Jt. Surg. Am. 1976, 58, 1074–1082. [Google Scholar] [CrossRef]
- Alimy, A.R.; Polzer, H.; Ocokoljic, A.; Ray, R.; Lewis, T.L.; Rolvien, T.; Waizy, H. Does Minimally Invasive Surgery Provide Better Clinical or Radiographic Outcomes Than Open Surgery in the Treatment of Hallux Valgus Deformity? A Systematic Review and Meta-analysis. Clin. Orthop. Relat. Res. 2023, 481, 1143–1155. [Google Scholar] [CrossRef] [PubMed]
- Palmanovich, E.; Ohana, N.; Atzmon, R.; Slevin, O.; Brin, Y.; Feldman, V.; Segal, D. MICA: A Learning Curve. J. Foot Ankle Surg. 2020, 59, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Crimi, A.; Fantoni, I.; Tagliapietra, J.; Ruggieri, P. Functional and Radiographic Outcomes of Minimally Invasive Intramedullary Nail Device (MIIND) for Moderate to Severe Hallux Valgus. Foot Ankle Int. 2021, 42, 409–424. [Google Scholar] [CrossRef] [PubMed]

| Modified DCMO Group (n = 68) | Control Group (n = 22) | p Value | |
|---|---|---|---|
| Age, year | 62.7 ± 8.4 | 55.2 ± 12.4 | 0.002 |
| Sex, number | Male 2, Female 66 | Male 2, Female 20 | 0.224 |
| Side, number | Left 35, Right 33 | Left 13, Right 9 | 0.533 |
| Body mass index, kg/m2 | 24.5 ± 3.3 | 23.2 ± 2.5 | 0.099 |
| Modified DCMO Group (n = 68) | Control Group (n = 22) | p Value | |
|---|---|---|---|
| Hallux valgus angle, degrees | 36.1 ± 8.1 | 32.2 ± 5.5 | 0.013 |
| Intermetatarsal angle, degrees | 15.0 ± 3.8 | 14.2 ± 2.3 | 0.351 |
| Distal metatarsal articular angle, degrees | 21.6 ± 8.9 | 25.7 ± 7.6 | 0.058 |
| Sesamoid position, grade | 6.4 ± 0.6 | 6.1 ± 0.8 | 0.068 |
| Preoperative | Postoperative 2 Months | Final Follow-Up | p Value * | p Value ** | p Value *** | |
|---|---|---|---|---|---|---|
| Modified DCMO group (N = 68) | ||||||
| Hallux valgus angle, degrees | 36.1 ± 8.1 | 11.8 ± 5.9 | 15.2 ± 7.3 | <0.001 | <0.001 | <0.001 |
| Intermetatarsal angle, degrees | 15.0 ± 3.8 | 7.0 ± 2.6 | 7.0 ± 2.7 | <0.001 | 0.887 | <0.001 |
| Distal metatarsal articular angle, degrees | 21.6 ± 8.9 | 13.4 ± 5.3 | 14.8 ± 6.9 | <0.001 | 0.022 | <0.001 |
| Sesamoid position, grade | 6.4 ± 0.6 | 4.1 ± 1.0 | 4.4 ± 1.0 | <0.001 | <0.001 | <0.001 |
| Control group (N = 22) | ||||||
| Hallux valgus angle, degrees | 32.2 ± 5.5 | 14.2 ± 410 | 17.1 ± 5.1 | <0.001 | 0.004 | <0.001 |
| Intermetatarsal angle, degrees | 14.2 ± 2.3 | 7.6 ± 2.6 | 8.6 ± 2.9 | <0.001 | 0.089 | <0.001 |
| Distal metatarsal articular angle, degrees | 25.7 ± 7.6 | 12.4 ± 4.6 | 15.9 ± 4.4 | <0.001 | 0.002 | <0.001 |
| Sesamoid position, grade | 6.1 ± 0.8 | 4.5 ± 1.1 | 4.9 ± 1.1 | <0.001 | 0.009 | <0.001 |
| Modified DCMO Group (n = 68) | Control Group (n = 22) | p Value | |
|---|---|---|---|
| *Δ Hallux valgus angle, degrees | −20.9 ± 8.2 | −15.1 ± 7.9 | 0.005 |
| *Δ Intermetatarsal angle, degrees | −7.9 ± 3.2 | −5.5 ± 2.7 | 0.002 |
| *Δ Distal metatarsal articular angle, degrees | −6.8 ± 11.7 | −9.8 ± 7.4 | 0.157 |
| *Δ Sesamoid position, grade | −2.0 ± 0.9 | −1.2 ± 1.1 | 0.002 |
| Dependent Variable | Independent Variable | Beta | 95% CI | p Value |
|---|---|---|---|---|
| *Δ Hallux valgus angle | Constant | 14.436 | −2.950 to 31.822 | 0.102 |
| Age | −0.169 | −0.312 to −0.027 | 0.021 | |
| Sex | 2.765 | −3.978 to 9.508 | 0.417 | |
| Surgical method | −2.249 | −5.684 to 1.186 | 0.196 | |
| Preoperative hallux valgus angle | −0.651 | −0.846 to −0.457 | <0.001 | |
| Preoperative intermetatarsal angle | 0.155 | −0.275 to 0.584 | 0.476 | |
| Preoperative distal metatarsal articular angle | −0.031 | −0.193 to 0.131 | 0.702 | |
| Preoperative sesamoid position | −0.513 | −2.869 to 1.842 | 0.666 | |
| *Δ Intermetatarsal angle | Constant | 3.977 | −2.202 to 10.156 | 0.204 |
| Age | −0.069 | −0.120 to −0.019 | 0.008 | |
| Sex | 1.285 | −1.111 to 3.682 | 0.289 | |
| Surgical method | −1.395 | −2.616 to −0.174 | 0.026 | |
| Preoperative hallux valgus angle | −0.002 | −0.072 to 0.067 | 0.944 | |
| Preoperative intermetatarsal angle | −0.553 | −0.706 to −0.400 | <0.001 | |
| Preoperative distal metatarsal articular angle | 0.032 | −0.026 to 0.089 | 0.273 | |
| Preoperative sesamoid position | 0.041 | −0.796 to 0.879 | 0.922 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyung, M.G.; Park, G.Y.; Yang, H.; Lee, D.Y. A Modified 90-Degree Distal Chevron Metatarsal Osteotomy for Correcting Moderate Hallux Valgus Deformity. J. Clin. Med. 2023, 12, 6902. https://doi.org/10.3390/jcm12216902
Kyung MG, Park GY, Yang H, Lee DY. A Modified 90-Degree Distal Chevron Metatarsal Osteotomy for Correcting Moderate Hallux Valgus Deformity. Journal of Clinical Medicine. 2023; 12(21):6902. https://doi.org/10.3390/jcm12216902
Chicago/Turabian StyleKyung, Min Gyu, Gil Young Park, Hanbual Yang, and Dong Yeon Lee. 2023. "A Modified 90-Degree Distal Chevron Metatarsal Osteotomy for Correcting Moderate Hallux Valgus Deformity" Journal of Clinical Medicine 12, no. 21: 6902. https://doi.org/10.3390/jcm12216902
APA StyleKyung, M. G., Park, G. Y., Yang, H., & Lee, D. Y. (2023). A Modified 90-Degree Distal Chevron Metatarsal Osteotomy for Correcting Moderate Hallux Valgus Deformity. Journal of Clinical Medicine, 12(21), 6902. https://doi.org/10.3390/jcm12216902







