Oral Health-Related Quality of Life in Adult Patients with Depression or Attention Deficit Hyperactivity Disorder (ADHD)
Abstract
:1. Introduction
2. Methods
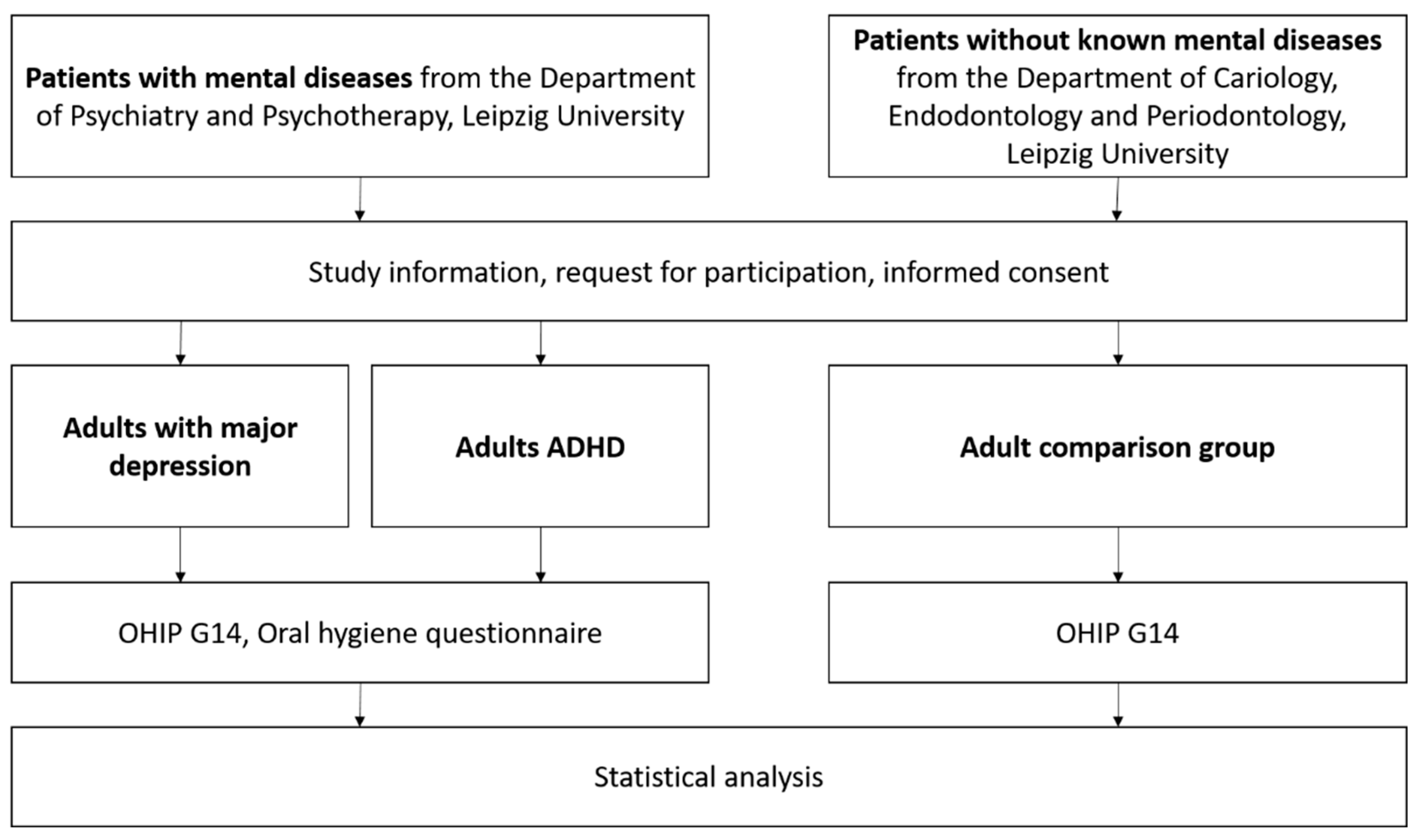
2.1. Study Design
2.2. Study Participants
2.3. Oral Health Impact Profile (OHIP G14)
2.4. Periodontitis and Oral Health Behaviour
2.5. Statistical Analysis
3. Results
3.1. Patients
3.2. OHIP G14
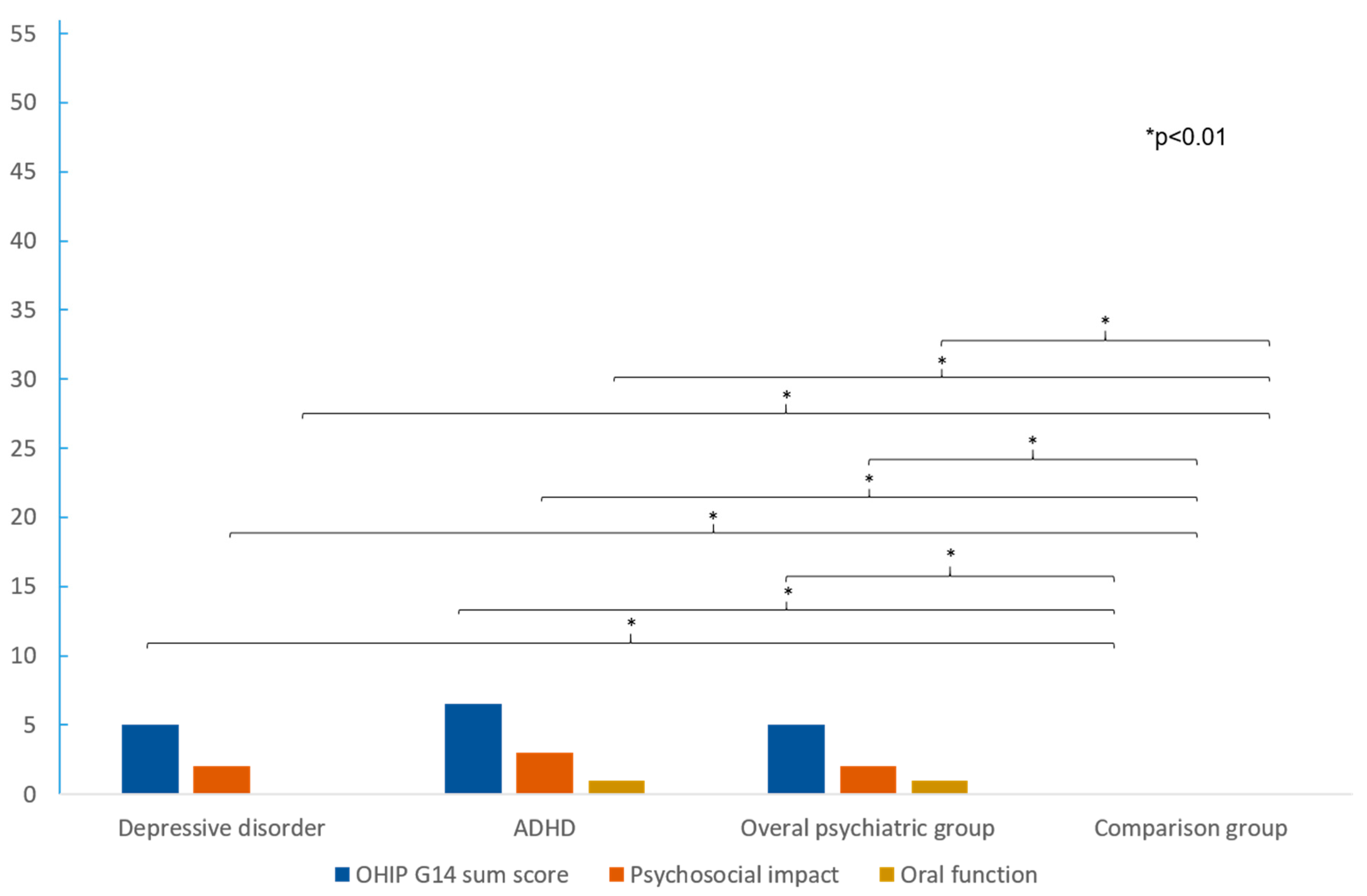
3.3. Oral Health Behaviour and Sensation
3.4. Associations between OHIP and Oral Health Behaviour and Sensation
4. Discussion
4.1. Summary of the Main Results
4.2. OHRQoL Disparities in Patients with Depressive Disorders and ADHD
4.3. Factors Influencing OHRQoL and Mentally Diseased Patients
4.4. Implications for Dental Care
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kisely, S. No Mental Health without Oral Health. Can. J. Psychiatry 2016, 61, 277–282. [Google Scholar] [CrossRef]
- Ball, J.; Darby, I. Mental health and periodontal and peri-implant diseases. Periodontology 2022, 90, 106–124. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Sawyer, E.; Siskind, D.; Lalloo, R. The oral health of people with anxiety and depressive disorders—A systematic review and meta-analysis. J. Affect. Disord. 2016, 200, 119–132. [Google Scholar] [CrossRef]
- Baiju, R.M.; Peter, E.; Varghese, N.O.; Sivaram, R. Oral Health and Quality of Life: Current Concepts. J. Clin. Diagn. Res. 2017, 11, ZE21–ZE26. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Rener-Sitar, K.; Baba, K.; Čelebić, A.; Larsson, P.; Szabo, G.; Norton, W.E.; Reissmann, D.R. Patterns of impaired oral health-related quality of life dimensions. J. Oral Rehabil. 2016, 43, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Reissmann, D.R. Dental Patient-Reported Outcome Measures Are Essential for Evidence-Based Prosthetic Dentistry. J. Evid. Based Dent. Pract. 2019, 19, 1–6. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.H. Oral health-related quality of life, probable depression and probable anxiety: Evidence from a representative survey in Germany. BMC Oral Health 2022, 22, 9. [Google Scholar] [CrossRef]
- Persson, K.; Axtelius, B.; Söderfeldt, B.; Ostman, M. Oral health-related quality of life and dental status in an outpatient psychiatric population: A multivariate approach. Int. J. Ment. Health Nurs. 2010, 19, 62–70. [Google Scholar] [CrossRef]
- Nerobkova, N.; Park, E.C.; Jang, S.I. Depression and oral health-related quality of life: A longitudinal study. Front. Public Health 2023, 11, 1072115. [Google Scholar] [CrossRef]
- Goh, V.; Hassan, F.W.; Baharin, B.; Rosli, T.I. Impact of psychological states on periodontitis severity and oral health-related quality of life. J. Oral Sci. 2022, 64, 1–5. [Google Scholar] [CrossRef]
- Noguchi, S.; Makino, M.; Haresaku, S.; Shimada, K.; Naito, T. Insomnia and depression impair oral health-related quality of life in the old-old. Geriatr. Gerontol. Int. 2017, 17, 893–897. [Google Scholar] [CrossRef]
- Ohi, T.; Murakami, T.; Komiyama, T.; Miyoshi, Y.; Endo, K.; Hiratsuka, T.; Satoh, M.; Asayama, K.; Inoue, R.; Kikuya, M.; et al. Oral health-related quality of life is associated with the prevalence and development of depressive symptoms in older Japanese individuals: The Ohasama Study. Gerodontology 2022, 39, 204–212. [Google Scholar] [CrossRef]
- Abdelsalam, S.; Van Den Boom, W.; Higgs, P.; Dietze, P.; Erbas, B. The association between depression and oral health related quality of life in people who inject drugs. Drug Alcohol. Depend. 2021, 229 Pt B, 109121. [Google Scholar] [CrossRef]
- Oancea, R.; Timar, B.; Papava, I.; Cristina, B.A.; Ilie, A.C.; Dehelean, L. Influence of depression and self-esteem on oral health-related quality of life in students. J. Intern. Med. Res. 2020, 48, 300060520902615. [Google Scholar] [CrossRef]
- Drechsler, R.; Brem, S.; Brandeis, D.; Grünblatt, E.; Berger, G.; Walitza, S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics 2020, 51, 315–335. [Google Scholar] [CrossRef]
- Reddy, E.R.; Kiranmayi, M.; Mudusu, S.P.; Raju, S.S.; Jannapureddy, R.; Kumar, A. Oral Health Status and Caries Experience in Children Diagnosed with Attention-deficit Hyperactive Disorder. Int. J. Clin. Pediatr. Dent. 2022, 15, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Ludovichetti, F.S.; Zuccon, A.; Cantatore, D.; Zambon, G.; Girotto, L.; Lucchi, P.; Stellini, E.; Mazzoleni, S. Early Childhood Caries and Oral Health-Related Quality of Life: Evaluation of the Effectiveness of Single-Session Therapy Under General Anesthesia. Eur. J. Dent. 2023, 17, 834–839. [Google Scholar] [CrossRef]
- Jamali, Z.; Ghaffari, P.; Aminabadi, N.A.; Norouzi, S.; Shirazi, S. Oral health status and oral health-related quality of life in children with attention-deficit hyperactivity disorder and oppositional defiant disorder. Spec. Care Dent. 2021, 41, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Zalsman, G.; Shilton, T. Adult ADHD: A new disease? Int. J. Psychiatry Clin. Pract. 2016, 20, 70–76. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epi-demiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the oral health impact profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- John, M.T.; Patrick, D.L.; Slade, G.D. The German version of the Oral Health Impact Profile—Translation and psychometric properties. Eur. J. Oral Sci. 2002, 110, 425–433. [Google Scholar] [CrossRef]
- Reissmann, D.R.; Krautz, M.; Schierz, O.; John, M.T.; Rudolph, M.; Szentpétery, A. Assessment of clinically significant changes in oral health. Ger. Dent. J. 2008, 63, 668–680. [Google Scholar]
- Schmalz, G.; Hübscher, A.E.; Angermann, H.; Schmidt, J.; Schmickler, J.; Legler, T.J.; Ziebolz, D. High prevalence of periodontitis in blood donors and the possibility of questionnaire-based screening—Results of a cross-sectional study. Transfus. Med. 2019, 29, 394–400. [Google Scholar] [CrossRef]
- Buset, S.L.; Walter, C.; Friedmann, A.; Weiger, R.; Borgnakke, W.S.; Zitzmann, N.U. Are periodontal diseases really silent? A systematic review of their effect on quality of life. J. Clin. Periodontol. 2016, 43, 333–344. [Google Scholar] [CrossRef]
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H.J. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Relat. Qual. Life Outcomes 2010, 8, 126. [Google Scholar] [CrossRef] [PubMed]
- Haag, D.G.; Peres, K.G.; Balasubramanian, M.; Brennan, D.S. Oral Conditions and Health-Related Quality of Life: A Systematic Review. J. Dent. Res. 2017, 96, 864–874. [Google Scholar] [CrossRef]
- Qamar, Z.; Alghamdi, A.M.S.; Haydarah, N.K.B.; Balateef, A.A.; Alamoudi, A.A.; Abumismar, M.A.; Shivakumar, S.; Cicciù, M.; Minervini, G. Impact of temporomandibular disorders on oral health-related quality of life: A systematic review and meta-analysis. J. Oral Rehabil. 2023, 50, 706–714. [Google Scholar] [CrossRef]
- Drumond, V.Z.; Souza, G.L.N.; Pereira, M.J.C.; Mesquita, R.A.; Amin, M.; Abreu, L.G. Dental Caries in Children with Attention Deficit/Hyperactivity Disorder: A Meta-Analysis. Caries Res. 2022, 56, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, A.H.; Yagiela, J.A.; Mahler, M.E.; Rubin, R. The pathophysiology, medical management and dental implications of adult attention-deficit/hyperactivity disorder. J. Am. Dent. Assoc. 2007, 138, 475–482, quiz 535, 537. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, V.; Hakeberg, M.; Blomkvist, K.; Wide Boman, U. Attention deficit hyperactivity disorder and dental anxiety in adults: Relationship with oral health. Eur. J. Oral Sci. 2013, 121, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, M.A.; Schwartz, C.E. Integrating response shift into health-related quality of life research: A theoretical model. Soc. Sci. Med. 1999, 48, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.E. Applications of response shift theory and methods to participation measurement: A brief history of a young field. Arch. Phys. Med. Rehabil. 2010, 91 (Suppl. S9), S38–S43. [Google Scholar] [CrossRef]
- Schmalz, G.; Garbade, J.; Kollmar, O.; Ziebolz, D. Does oral health-related quality of life of patients after solid organ transplantation indicate a response shift? Results of a systematic review. BMC Oral Health 2020, 20, 356. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Dietl, M.; Vasko, R.; Müller, G.A.; Rothermund, L.; Keller, F.; Ziebolz, D.; Rasche, F.M. Dialysis vintage time has the strongest correlation to psychosocial pattern of oral health-related quality of life—A multicentre cross-sectional study. Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e698–e706. [Google Scholar] [CrossRef]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral-Health-Related Quality of Life in Adult Patients with Rheumatic Diseases-A Systematic Review. J. Clin. Med. 2020, 9, 1172. [Google Scholar] [CrossRef]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral health-related quality of life in adult patients with end-stage kidney diseases undergoing renal replacement therapy—A systematic review. BMC Nephrol. 2020, 21, 154. [Google Scholar] [CrossRef]
- John, M.T.; Micheelis, W.; Biffar, R. Reference values in oral health-related quality of life for the abbreviated version of the Oral Health Impact Profile. Swiss Dent. J. 2004, 114, 784–791. [Google Scholar]
- Cockburn, N.; Pradhan, A.; Taing, M.W.; Kisely, S.; Ford, P.J. Oral health impacts of medications used to treat mental illness. J. Affect. Disord. 2017, 223, 184–193. [Google Scholar] [CrossRef]
- John, M.T.; Omara, M.; Su, N.; List, T.; Sekulic, S.; Häggman-Henrikson, B.; Visscher, C.M.; Bekes, K.; Reissmann, D.R.; Baba, K.; et al. Recommendations for use and scoring of oral health impact profile versions. J. Evid. Based Dent. Pract. 2022, 22, 101619. [Google Scholar] [CrossRef] [PubMed]
| Psychiatric Group n = 141 | Depressive Disorder n = 94 | ADHD n = 47 | Comparison Group N = 145 | p-Value | |
|---|---|---|---|---|---|
| Age mv ± SD | 39.0 ± 13.1 | 40.9 ± 13.9 | 36.0 ± 11.3 | 38.9 ± 13.9 | 0.354 |
| Age Range | 21–67 | 21–67 | 21–65 | 21–67 | 0.653 |
| Gender | |||||
| Male (%) | 47 | 51 | 40 | 37 | 0.176 |
| Female (%) | 53 | 49 | 60 | 63 | 0.143 |
| OHIP Items Mean (Range) | Psychiatric Group (n = 141) | Depressive Disorder (n = 94) | ADHD (n = 47) | Comparison Group (N = 145) | PG vs. CG p-Value | DD vs. CG p-Value | ADHD vs. CG p-Value | ADHD vs. DD p-Value |
|---|---|---|---|---|---|---|---|---|
| Trouble pronouncing | 0 (0–4) | 0 (0–4) | 0 (0–2) | 0 (0–2) | 0.007 | 0.003 | 0.196 | 0.346 |
| Taste worsened | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0 (0–2) | 0.001 | 0.051 | <0.001 | 0.034 |
| Life less satisfactory | 0 (0–4) | 0 (0–4) | 0 (0–4) | 0 (0–3) | <0.001 | <0.001 | <0.001 | 0.561 |
| Difficult to relax | 0 (0–4) | 0 (0–4) | 0.50 (0–4) | 0 (0–4) | <0.001 | <0.001 | 0.004 | 0.884 |
| Feeling of tension | 1.00 (0–4) | 0.5 (0–4) | 1.00 (0–4) | 0 (0–4) | <0.001 | <0.001 | <0.001 | 0.836 |
| Interrupting meals | 0 (0–4) | 0 (0–4) | 0 (0–2) | 0 (0–2) | 0.001 | 0.035 | <0.001 | 0.077 |
| Uncomfortable eating | 0 (0–4) | 0 (0–4) | 0 (0–3) | 0 (0–4) | <0.001 | <0.001 | <0.001 | 0.197 |
| Short tempered | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0.003 | 0.015 | 0.008 | 0.555 |
| Difficult to perform daily jobs | 0 (0–4) | 0 (0–4) | 0 (0–3) | 0 (0–4) | 0.010 | 0.017 | 0.033 | 0.919 |
| Unable to function | 0 (0–3) | 0 (0–3) | 0 (0–2) | 0 (0–3) | 0.007 | 0.026 | 0.007 | 0.460 |
| Embarrassed | 0 (0–4) | 0 (0–4) | 0 (0–4) | 0 (0–2) | <0.001 | <0.001 | <0.001 | 0.292 |
| Diet unsatisfactory | 0 (0–4) | 0 (0–4) | 0 (0–4) | 0 (0–2) | 0.004 | 0.006 | 0.021 | 0.994 |
| Oral pain | 1.00 (0–4) | 0 (0–4) | 1.00 (0–4) | 0 (0–3) | <0.001 | <0.001 | <0.001 | 0.088 |
| Sense of uncertainty with teeth | 0 (0–4) | 0 (0–4) | 1.00 (0–3) | 0 (0–2) | <0.001 | <0.001 | <0.001 | 0.396 |
| Sum oral function | 1.00 (0–16) | 0 (0–16) | 1.00 (0–13) | 0 (0–9) | <0.001 | <0.001 | <0.001 | 0.090 |
| Sum psychosocial impact | 2.00 (0–25) | 2.00 (0–25) | 3.00 (0–19) | 0 (0–16) | <0.001 | <0.001 | <0.001 | 0.666 |
| Sum score | 5.00 (0–46) | 5.00 (0–46) | 6.50 (0–38) | 0 (0–31) | <0.001 | <0.001 | <0.001 | 0.302 |
| Oral Health Behaviour and Sensation | Psychiatric Group (N = 141) | Depressive Disorder (n = 94) | ADHD (n = 47) |
|---|---|---|---|
| Gum Bleeding | 54 (38.3) | 35 (37.2) | 19 (40.4) |
| Worse Taste | 84 (60.4) | 52 (55.9) | 32 (69.6) |
| Periodontitis Treatment | 26 (19.4) | 17 (18.1) | 9 (19.1) |
| Smoking | 89 (63.6) | 58 (62.4) | 31 (66.0) |
| Regular Dental Visits | 66 (47.5) | 53 (57.6) | 13 (27.7) |
| Professional Tooth Cleaning | 65 (46.4) | 48 (51.6) | 17 (36.2) |
| Informed Dentist | 39 (28.1) | 26 (28.0) | 13 (28.3) |
| Educated about Oral Hygiene | 125 (89.3) | 85 (91.4) | 40 (85.1) |
| Interdental Cleaning | 85 (60.3) | 59 (62.8) | 26 (55.3) |
| Mouth Rinse | 54 (38.3) | 33 (35.1) | 21 (44.7) |
| Items | OHIP Score High (n = 67) | OHIP Score Low (n = 72) | p-Value |
|---|---|---|---|
| Gum Bleeding | 23 (31.9) | 30 (44.8) | <0.001 |
| Smoking | 44 (61.1) | 43 (65.2) | <0.001 |
| Professional Tooth Cleaning | 37 (51.4) | 29 (43.9) | <0.001 |
| Educated about Oral Hygiene | 66 (91.7) | 58 (86.6) | <0.001 |
| Interdental Cleaning | 46 (63.9) | 38 (56.7) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gemp, S.; Ziebolz, D.; Haak, R.; Mauche, N.; Prase, M.; Dogan-Sander, E.; Görges, F.; Strauß, M.; Schmalz, G. Oral Health-Related Quality of Life in Adult Patients with Depression or Attention Deficit Hyperactivity Disorder (ADHD). J. Clin. Med. 2023, 12, 7192. https://doi.org/10.3390/jcm12227192
Gemp S, Ziebolz D, Haak R, Mauche N, Prase M, Dogan-Sander E, Görges F, Strauß M, Schmalz G. Oral Health-Related Quality of Life in Adult Patients with Depression or Attention Deficit Hyperactivity Disorder (ADHD). Journal of Clinical Medicine. 2023; 12(22):7192. https://doi.org/10.3390/jcm12227192
Chicago/Turabian StyleGemp, Stephan, Dirk Ziebolz, Rainer Haak, Nicole Mauche, Madlen Prase, Ezgi Dogan-Sander, Frauke Görges, Maria Strauß, and Gerhard Schmalz. 2023. "Oral Health-Related Quality of Life in Adult Patients with Depression or Attention Deficit Hyperactivity Disorder (ADHD)" Journal of Clinical Medicine 12, no. 22: 7192. https://doi.org/10.3390/jcm12227192
APA StyleGemp, S., Ziebolz, D., Haak, R., Mauche, N., Prase, M., Dogan-Sander, E., Görges, F., Strauß, M., & Schmalz, G. (2023). Oral Health-Related Quality of Life in Adult Patients with Depression or Attention Deficit Hyperactivity Disorder (ADHD). Journal of Clinical Medicine, 12(22), 7192. https://doi.org/10.3390/jcm12227192







