Association of Cardiovascular Disease and Pancreatitis: What Came First, the Chicken or the Egg?
Abstract
:1. Introduction
2. Methods
3. Results and Discussions
3.1. Acute Pancreatitis
3.1.1. CVD and Risk of Acute Pancreatitis
3.1.2. Risk of Atherosclerosis and Coronary Artery Disease (CAD) in Patients with Acute Pancreatitis
3.1.3. Hypertriglyceridemia and Acute Pancreatitis
3.1.4. Congestive Heart Failure (CHF) and Acute Pancreatitis
3.1.5. Acute Pancreatitis-Associated Cardiac Injury
3.1.6. Acute MI and Acute Pancreatitis
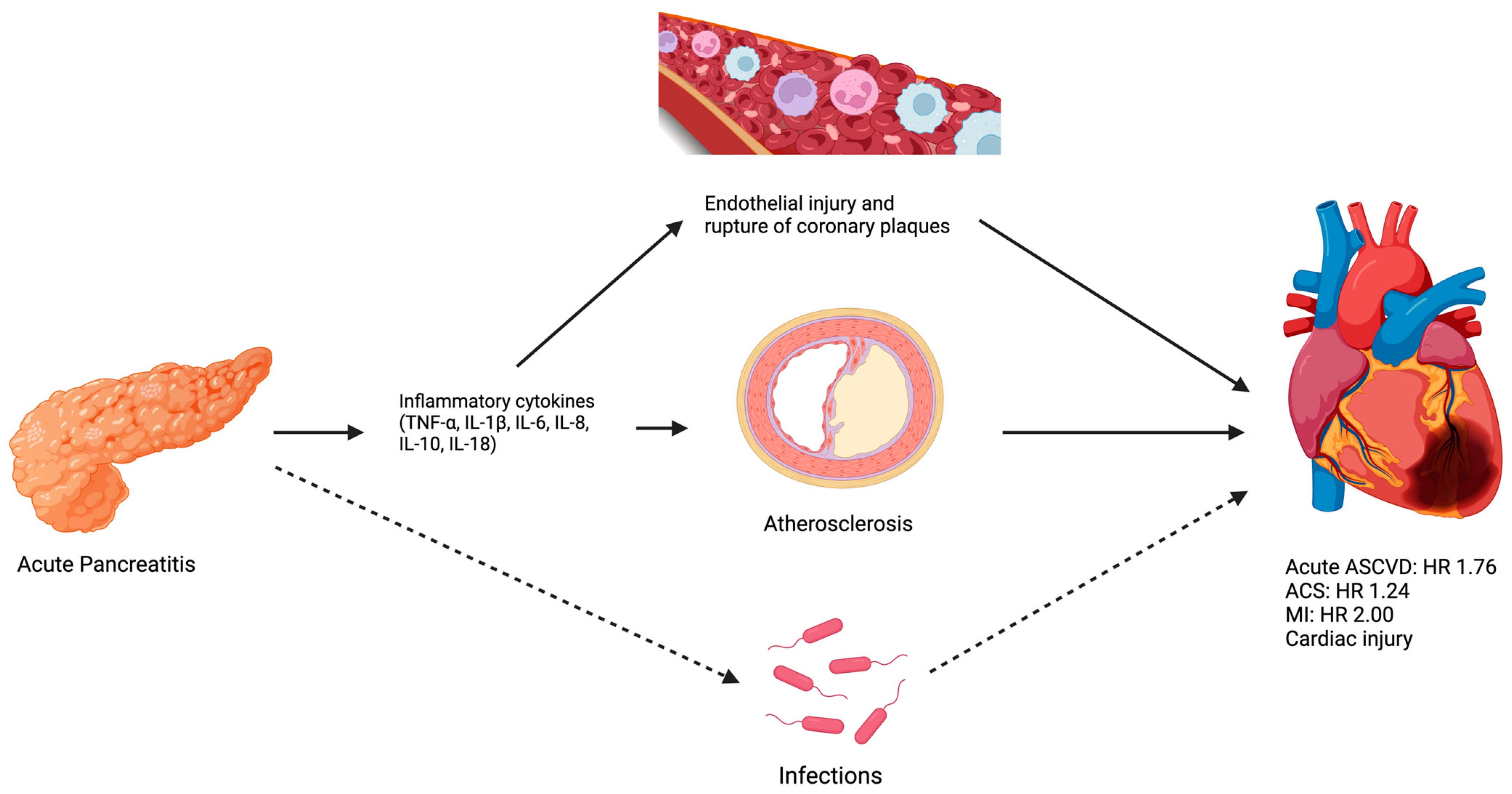
3.1.7. Potential Mechanisms between Acute Pancreatitis and ASCVD
3.2. Chronic Pancreatitis
3.2.1. CVD and Risk of Chronic Pancreatitis
3.2.2. Risk of Atherosclerosis and CAD in Patients with Chronic Pancreatitis
3.2.3. Hypertriglyceridemia and Chronic Pancreatitis
3.2.4. CHF and Chronic Pancreatitis
3.2.5. Chronic Pancreatitis-Associated Cardiac Injury
3.2.6. Acute MI and Chronic Pancreatitis
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mederos, M.A.; Reber, H.A.; Girgis, M.D. Acute Pancreatitis: A Review. JAMA 2021, 325, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Crockett, S.D.; Wani, S.; Gardner, T.B.; Falck-Ytter, Y.; Barkun, A.N.; Feuerstein, J.; Flamm, S.; Gellad, Z.; Gerson, L.; Gupta, S.; et al. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology 2018, 154, 1096–1101. [Google Scholar] [CrossRef]
- Pham, A.; Forsmark, C. Chronic pancreatitis: Review and update of etiology, risk factors, and management. F1000Research 2018, 7, 607. [Google Scholar] [CrossRef] [PubMed]
- Sankaran, S.J.; Xiao, A.Y.; Wu, L.M.; Windsor, J.A.; Forsmark, C.E.; Petrov, M.S. Frequency of progression from acute to chronic pancreatitis and risk factors: A meta-analysis. Gastroenterology 2015, 149, 1490–1500.e1. [Google Scholar] [CrossRef]
- Petrov, M.S.; Yadav, D. Global epidemiology and holistic prevention of pancreatitis. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, G.; Pan, G.; Liu, Q.; Wu, Y.; Liu, Z.; Lu, W.; Li, S.; Zhou, Z.; Wen, Y. The global, regional, and national burden of pancreatitis in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. BMC Med. 2020, 18, 388. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Lond Engl. 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Fairfield, C.J.; Wigmore, S.J.; Harrison, E.M. Gallstone Disease and the Risk of Cardiovascular Disease. Sci. Rep. 2019, 9, 5830. [Google Scholar] [CrossRef]
- Chen, B.; Collen, L.V.; Mowat, C.; Isaacs, K.L.; Singh, S.; Kane, S.V.; Farraye, F.A.; Snapper, S.; Jneid, H.; Lavie, C.J.; et al. Inflammatory Bowel Disease and Cardiovascular Diseases. Am. J. Med. 2022, 135, 1453–1460. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, B.; Ciaccio, E.J.; Jneid, H.; Virani, S.S.; Lavie, C.J.; Lebovits, J.; Green, P.H.R.; Krittanawong, C. Celiac Disease and the Risk of Cardiovascular Diseases. Int. J. Mol. Sci. 2023, 24, 9974. [Google Scholar] [CrossRef] [PubMed]
- Bexelius, T.S.; Ljung, R.; Mattsson, F.; Lagergren, J. Cardiovascular disease and risk of acute pancreatitis in a population-based study. Pancreas 2013, 42, 1011–1015. [Google Scholar] [CrossRef] [PubMed]
- Chacón-Portillo, M.A.; Payró-Ramírez, G.; Pelaez-Luna, M.C.; Uscanga-Domínguez, L.F.; Vasquéz-Ortiz, Z.; Orihuela, C.; Martínez-Vázquez, S.E.; Hernández-Calleros, J. Abnormal Cardiovascular Findings in Acute Pancreatitis: Are They Associated with Disease Severity? Rev. Investig. Clin. Organo. Hosp. Enfermedades Nutr. 2017, 69, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.S.; Lin, C.L. Incidence and risk of acute coronary syndrome in patients with acute pancreatitis: A nationwide cohort study. Pancreatol. Off. J. Int. Assoc. Pancreatol. IAP Al. 2017, 17, 675–680. [Google Scholar] [CrossRef]
- Khan, D.; Abureesh, M.; Alkhayyat, M.; Sadiq, W.; Alshami, M.; Munir, A.B.; Karam, B.; Deeb, L.; Lafferty, J. Prevalence of Myocardial Infarction in Patients With Chronic Pancreatitis. Pancreas 2021, 50, 99–103. [Google Scholar] [CrossRef]
- Bang, U.C.; Benfield, T.; Hyldstrup, L.; Bendtsen, F.; Beck Jensen, J.E. Mortality, cancer, and comorbidities associated with chronic pancreatitis: A Danish nationwide matched-cohort study. Gastroenterology 2014, 146, 989–994. [Google Scholar] [CrossRef]
- Kurkcu, K.; Kara, B.; Koc, A.S.; Keskek, S.O. A practical means of evaluating the prognosis of acute pancreatitis, as measurement of carotid artery intima-media thickness. Acta Gastro-Enterol. Belg. 2021, 84, 437–442. [Google Scholar] [CrossRef]
- Sung, L.-C.; Chang, C.-C.; Lin, C.-S.; Yeh, C.-C.; Cherng, Y.-G.; Chen, T.-L.; Liao, C.-C. Risk of acute atherosclerotic cardiovascular disease in patients with acute and chronic pancreatitis. Sci. Rep. 2021, 11, 20907. [Google Scholar] [CrossRef]
- Adiamah, A.; Psaltis, E.; Crook, M.; Lobo, D.N. A systematic review of the epidemiology, pathophysiology and current management of hyperlipidaemic pancreatitis. Clin Nutr Edinb Scotl. 2018, 37 6PtA, 1810–1822. [Google Scholar] [CrossRef]
- Amblee, A.; Mohananey, D.; Morkos, M.; Basu, S.; Abegunde, A.K.T.; Ganesh, M.; Bhalerao, N.; George, A.M.; Jain, M.; Fogelfeld, L. Acute Pancreatitis in Patients with Severe Hypertriglyceridemia in a Multi-Ethnic Minority Population. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2018, 24, 429–436. [Google Scholar] [CrossRef]
- Copeland, L.A.; Swendsen, C.S.; Sears, D.M.; MacCarthy, A.A.; McNeal, C.J. Association between triglyceride levels and cardiovascular disease in patients with acute pancreatitis. PLoS ONE 2018, 13, e0179998. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Shah, I.; Pahuja, M.; Amin, S.; Bhurwal, A.; Moni, S.; Hawthorne, K. Outcomes of Acute Pancreatitis in Patients with Heart Failure: Insights from the Nationwide Inpatient Sample. J. Card Fail. 2019, 25, S57–S58. [Google Scholar] [CrossRef]
- Thandassery, R.B.; Choudhary, N.; Bahl, A.; Kochhar, R. Characterization of Cardiac Dysfunction by Echocardiography in Early Severe Acute Pancreatitis. Pancreas 2017, 46, 626–630. [Google Scholar] [CrossRef]
- Jang, D.K.; Choi, J.H.; Paik, W.H.; Ryu, J.K.; Kim, Y.-T.; Han, K.-D.; Lee, S.H. Risk of cardiovascular disease and mortality in patients with diabetes and acute pancreatitis history: A nationwide cohort study. Sci. Rep. 2022, 12, 18730. [Google Scholar] [CrossRef] [PubMed]
- Khan, U.; Petrechko, O.; Sagheer, S.; Majeed, H.; Zaidi, S.H.; Wasty, N.; Sheikh, A.B. Acute Pancreatitis and Myocardial Infarction: A Narrative Review. Cardiology 2023, 148, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yegneswaran, B.; Kostis, J.B.; Pitchumoni, C.S. Cardiovascular manifestations of acute pancreatitis. J. Crit. Care. 2011, 26, e11–e18. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.; Orecchioni, M.; Ley, K. How the immune system shapes atherosclerosis: Roles of innate and adaptive immunity. Nat. Rev. Immunol. 2022, 22, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Wolf, D.; Ley, K. Immunity and Inflammation in atherosclerosis. Circ. Res. 2019, 124, 315–327. [Google Scholar] [CrossRef]
- Schaftenaar, F.; Frodermann, V.; Kuiper, J.; Lutgens, E. Atherosclerosis: The interplay between lipids and immune cells. Curr. Opin. Lipidol. 2016, 27, 209–215. [Google Scholar] [CrossRef]
- Mayer, J.; Rau, B.; Gansauge, F.; Beger, H.G. Inflammatory mediators in human acute pancreatitis: Clinical and pathophysiological implications. Gut 2000, 47, 546–552. [Google Scholar] [CrossRef]
- Malmstrøm, M.L.; Hansen, M.B.M.; Andersen, A.M.; Ersbøll, A.K.M.; Nielsen, O.H.M.; Jørgensen, L.N.M.; Novovic, S. Cytokines and organ failure in acute pancreatitis: Inflammatory response in acute pancreatitis. Pancreas 2012, 41, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Ridker, P.M.; Maseri, A. Inflammation and Atherosclerosis. Circulation 2002, 105, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Ramji, D.P.; Davies, T.S. Cytokines in atherosclerosis: Key players in all stages of disease and promising therapeutic targets. Cytokine Growth Factor Rev. 2015, 26, 673–685. [Google Scholar] [CrossRef] [PubMed]
- Tousoulis, D.; Oikonomou, E.; Economou, E.K.; Crea, F.; Kaski, J.C. Inflammatory cytokines in atherosclerosis: Current therapeutic approaches. Eur. Heart J. 2016, 37, 1723–1732. [Google Scholar] [CrossRef] [PubMed]
- Sipilä, P.N.; Lindbohm, J.V.; Batty, G.D.; Heikkilä, N.; Vahtera, J.; Suominen, S.; Väänänen, A.; Koskinen, A.; Nyberg, S.T.; Meri, S.; et al. Severe Infection and Risk of Cardiovascular Disease: A Multicohort Study. Circulation 2023, 147, 1582–1593. [Google Scholar] [CrossRef]
- Ravnskov, U.; McCully, K.S. Review and Hypothesis: Vulnerable plaque formation from obstruction of Vasa vasorum by homocysteinylated and oxidized lipoprotein aggregates complexed with microbial remnants and LDL autoantibodies. Ann. Clin. Lab. Sci. 2009, 39, 3–16. [Google Scholar]
- Ravnskov, U.; McCully, K.S. Infections may be causal in the pathogenesis of atherosclerosis. Am. J. Med. Sci. 2012, 344, 391–394. [Google Scholar] [CrossRef]
- Petrov, M.S.; Shanbhag, S.; Chakraborty, M.; Phillips, A.R.J.; Windsor, J.A. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology 2010, 139, 813–820. [Google Scholar] [CrossRef]
- Ni, T.; Wen, Y.; Zhao, B.; Ning, N.; Chen, E.; Mao, E.; Zhou, W. Characteristics and risk factors for extrapancreatic infection in patients with moderate or severe acute pancreatitis. Heliyon 2023, 9, e13131. [Google Scholar] [CrossRef]
- Brown, L.A.; Hore, T.A.; Phillips, A.R.J.; Windsor, J.A.; Petrov, M.S. A systematic review of the extra-pancreatic infectious complications in acute pancreatitis. Pancreatol. Off. J. Int. Assoc. Pancreatol. IAP Al. 2014, 14, 436–443. [Google Scholar] [CrossRef]
- Lu, J.D.; Cao, F.; Ding, Y.X.; Wu, Y.D.; Guo, Y.L.; Li, F. Timing, distribution, and microbiology of infectious complications after necrotizing pancreatitis. World J. Gastroenterol. 2019, 25, 5162–5173. [Google Scholar] [CrossRef] [PubMed]
- Schmid, S.W.; Uhl, W.; Friess, H.; Malfertheiner, P.; Büchler, M.W. The role of infection in acute pancreatitis. Gut 1999, 45, 311. [Google Scholar] [CrossRef] [PubMed]
- Gullo, L.; Stella, A.; Labriola, E.; Costa, P.L.; Descovich, G.; Labò, G. Cardiovascular lesions in chronic pancreatitis. Dig. Dis. Sci. 1982, 27, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Lee, U.K.; Chang, T.I.; Polanco, J.C.; Pisegna, J.R.; Friedlander, A.H. Prevalence of Panoramically Imaged Carotid Atheromas in Alcoholic Patients With Chronic Pancreatitis and Comorbid Diabetes. J. Oral. Maxillofac. Surg. Off. J. Am. Assoc. Oral. Maxillofac. Surg. 2018, 76, e1–e1929. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.S.; Liao, K.F.; Lin, C.M.; Lin, C.L.; Chen, W.C.; Lai, S.W. Chronic Pancreatitis Correlates With Increased Risk of Cerebrovascular Disease: A Retrospective Population-Based Cohort Study in Taiwan. Medicine 2016, 95, e3266. [Google Scholar] [CrossRef]
- De la Iglesia, D.; Vallejo-Senra, N.; López-López, A.; Iglesias-Garcia, J.; Lariño-Noia, J.; Nieto-García, L.; Domínguez-Muñoz, J.E. Pancreatic exocrine insufficiency and cardiovascular risk in patients with chronic pancreatitis: A prospective, longitudinal cohort study. J. Gastroenterol. Hepatol. 2019, 34, 277–283. [Google Scholar] [CrossRef]
- Xia, T.; Chai, X.; Shen, J. Pancreatic exocrine insufficiency in patients with chronic heart failure and its possible association with appetite loss. PLoS ONE 2017, 12, e0187804. [Google Scholar] [CrossRef]
- Vujasinovic, M.; Tretjak, M.; Tepes, B.; Marolt, A.; Slemenik Pusnik, C.; Kotnik Kerbev, M.; Rudolf, S. Is Pancreatic Exocrine Insufficiency A Result of Decreased Splanchnic Circulation in Patients with Chronic Heart Failure? J. Pancreas. 2016, 17, 201–203. [Google Scholar] [CrossRef]
- Özcan, M.; Öztürk, G.Z.; Köse, M.; Emet, S.; Aydın, Ş.; Arslan, K.; Arman, Y.; Akkaya, V.; Tükek, T. Evaluation of malnutrition with blood ghrelin and fecal elastase levels in acute decompensated heart failure patients. Arch. Turk Soc. Cardiol. 2015, 43, 131–137. [Google Scholar] [CrossRef]
- Hsu, M.T.; Lin, C.L.; Chung, W.S. Increased Risk of Acute Coronary Syndrome in Patients With Chronic Pancreatitis: A Nationwide Cohort Analysis. Medicine 2016, 95, e3451. [Google Scholar] [CrossRef]
- Löhr, J.M.; Dominguez-Munoz, E.; Rosendahl, J.; Besselink, M.; Mayerle, J.; Lerch, M.M.; Haas, S.; Akisik, F.; Kartalis, N.; Iglesias-Garcia, J.; et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United Eur. Gastroenterol. J. 2017, 5, 153–199. [Google Scholar] [CrossRef] [PubMed]
- Dams, O.C.; Vijver, M.A.T.; van Veldhuisen, C.L.; Verdonk, R.C.; Besselink, M.G.; van Veldhuisen, D.J. Heart Failure and Pancreas Exocrine Insufficiency: Pathophysiological Mechanisms and Clinical Point of View. J. Clin. Med. 2022, 11, 4128. [Google Scholar] [CrossRef] [PubMed]

| Reference (First Author, Year of Publication, Country) | Type of Study (Longitudinal vs. Cross-Sectional) | Patients, n | Mean Age (Years) | Outcomes |
|---|---|---|---|---|
| K Kurkcu et al., 2018, Turkey [17] | Cross-sectional | 101 | 50 | Common and internal carotid artery intima-media thickness above > 0.755 were associated with more severe AP. (p = 0.000). |
| Bexelius et al., 2013, Sweden [12] | Cross-sectional | 6161 AP 61,637 controls | N/A | CVD was positively associated with risk of AP (adjusted OR 1.35, 95% CI: 1.25–1.45). |
| Sung et al., 2021, Taiwan [18] | Longitudinal | 2607 | N/A | The adjusted HR of acute ASCVD was 1.76 (95% CI 1.47–2.12) for people with AP. |
| Adiamah et al., 2018, UK [19] | Systematic review with 38 studies | 1979 | NA | The reported proportion of hyperlipidemic pancreatitis ranged between 2.3 and 53% in patients with AP. |
| Amblee et al., 2018, USA [20] | Cross-sectional | 1157 | 49.2 | The prevalence of AP was 9.2% in patients with a serum triglyceride level ≥ 1000 mg/dL. |
| Copeland et al., 2018, USA [21] | Longitudinal | 20,608 | 60.4 | Elevated triglycerides (>2000 mg/dL) levels were positively associated with days to acute pancreatitis admissions from triglyceride assessment (HR 1.38, CI 95: 1.16–1.63). |
| Mehta et al., 2019, USA [22] | Cross-sectional | 1,356,659 AP with 69,657 CHF | 69.7 without CHF vs. 51.1 with CHF | CHF is associated with more respiratory failure, intubation, higher in-hospital mortality, and longer length of stay in patients admitted for AP. |
| Chacon-Portillo et al., 2017, Mexico [13] | Cross-sectional study | 27 | 48 | 67% with increased pro-brain natriuretic peptide levels, 52% had abnormal ECG findings, 48% had abnormal echo findings, and 18% had increased troponin levels in the acute phase of AP. |
| Thandassery et al. 2017, India [23] | Cross-sectional | 72 | 41 (median age) | In patients with severe pancreatitis and hypotension, 60% with diastolic dysfunction, 17% with systolic dysfunction, and 23% with combined dysfunction on ECHO. |
| Chung et al., 2017, Taiwan [14] | Longitudinal | 87,068 with AP, 348,272 controls | 53 | Incidence of ACS in AP vs. control: 5.44 vs. 3.03 per person-years, with adjusted HR of 1.24 (95% CI: 1.19–1.30). |
| Jang et al., 2022, Korea [24] | Longitudinal | 3810 with AP, 2,258,910 control | 55.0 with AP vs. 55.7 in control | AP is associated with increased risk for MI with an adjusted HR of 1.998 (95% CI 1.733–2.303) in patients with diabetes. |
| Reference (First Author, Year of Study, Country) | Type of Study (Longitudinal vs. Cross-Sectional) | Patients, n | Mean Age | Outcomes |
|---|---|---|---|---|
| Gullo et al., 1982, Italy [43] | Cross-sectional | 54 CP, 54 controls | N/A | Arterial involvement in 18 patients vs. 5 controls (33% vs. 9%, p < 0.01); ECG changes indicating CAD in 8 patients vs. 3 controls. |
| Lee et al., 2018, USA [44] | Cross-sectional | 32 | 61.7 | Significant association between a diagnosis of ARCP-DM and presence of atheroma on the panoramic image: 25% vs. 3% (p < 0.05) in patients with alcohol-related chronic pancreatitis vs. general population. |
| Bang et al., 2014, Denmark [16] | Longitudinal | 11,972 CP, 11,972 controls | 54.5 | CP is associated with higher prevalence of cerebrovascular disease with an adjusted HR of 1.3 (95% CI: 1.2–1.4), but not MI with an adjusted HR of 0.9 (95% CI: 0.8–1.0). |
| Wong et al., 2016, Taiwan [45] | Longitudinal | 16,672 CP, 65,877 controls | 47.5 | Incidence of cerebrovascular disease was 14.2 vs. 11.5 per 1000 person-years with an adjusted HR of 1.27 (95% CI: 1.19–1.36). |
| De la Iglesia et al., 2018, Spain [46] | Longitudinal | 430 | 47.8 | PEI was present in 29.3% of patients with chronic pancreatitis |
| Xia et al., 2017, China [47] | Cross-sectional | 104 | 70.4 | The prevalence of PEI (n = 59) is 56.7% in patients with CHF, compared to 0.00% in the control group. |
| Miroslav et al., 2015, Sweden [48] | Cross-sectional | 87 | 74.7 | PEI were diagnosed in 6.9% of patients with CHF: severe PEI 3.45%, and mild PEI 3.45%. |
| Ozcan et al., 2015, Istanbul [49] | Cross-sectional | 52 | 67.5 | In the severe acute decompensated HF group, 20% had mild to moderate PEI, and 50% had severe PEI. In the mild acute decompensated HF group, 9.4% had mild to moderate PEI, and 12.5% had severe PEI. In the control group, 12.9% had mild to moderate PEI, and 19.4% had severe PEI. |
| Hsu et al., 2016, Taiwan [50] | Longitudinal | 17,405 CP, 69,620 controls | 48.3 | ACS incidence 4.89 vs. 2.28 per 10,000 person-years in CP vs. controls with an adjusted hazard ratio of 1.40 (95% CI: 1.20–1.64). |
| Khan et al., 2021, USA [15] | Cross-sectional | 63,230 CP, 28,778,980 controls | N/A | Prevalence of MI 14.22% vs. 3.23% in CP vs. controls (p < 0.0001), with an adjusted OR 1.453 (95% CI: 1.418–1.488). |
| Sung et al., 2021, Taiwan [18] | Longitudinal | 71 CP | N/A | The adjusted HR of acute ASCVD was 3.42 (95% CI: 1.69–6.94) in CP vs. controls. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, B.; Moin, A.; Virk, H.U.H.; Jneid, H.; Virani, S.S.; Krittanawong, C. Association of Cardiovascular Disease and Pancreatitis: What Came First, the Chicken or the Egg? J. Clin. Med. 2023, 12, 7101. https://doi.org/10.3390/jcm12227101
Chen B, Moin A, Virk HUH, Jneid H, Virani SS, Krittanawong C. Association of Cardiovascular Disease and Pancreatitis: What Came First, the Chicken or the Egg? Journal of Clinical Medicine. 2023; 12(22):7101. https://doi.org/10.3390/jcm12227101
Chicago/Turabian StyleChen, Bing, Aleena Moin, Hafeez Ul Hassan Virk, Hani Jneid, Salim S. Virani, and Chayakrit Krittanawong. 2023. "Association of Cardiovascular Disease and Pancreatitis: What Came First, the Chicken or the Egg?" Journal of Clinical Medicine 12, no. 22: 7101. https://doi.org/10.3390/jcm12227101
APA StyleChen, B., Moin, A., Virk, H. U. H., Jneid, H., Virani, S. S., & Krittanawong, C. (2023). Association of Cardiovascular Disease and Pancreatitis: What Came First, the Chicken or the Egg? Journal of Clinical Medicine, 12(22), 7101. https://doi.org/10.3390/jcm12227101







