Body Composition of Master Swimmers before and after the COVID-19 Pandemic: A Longitudinal Study
Abstract
1. Introduction
2. Material and Methods
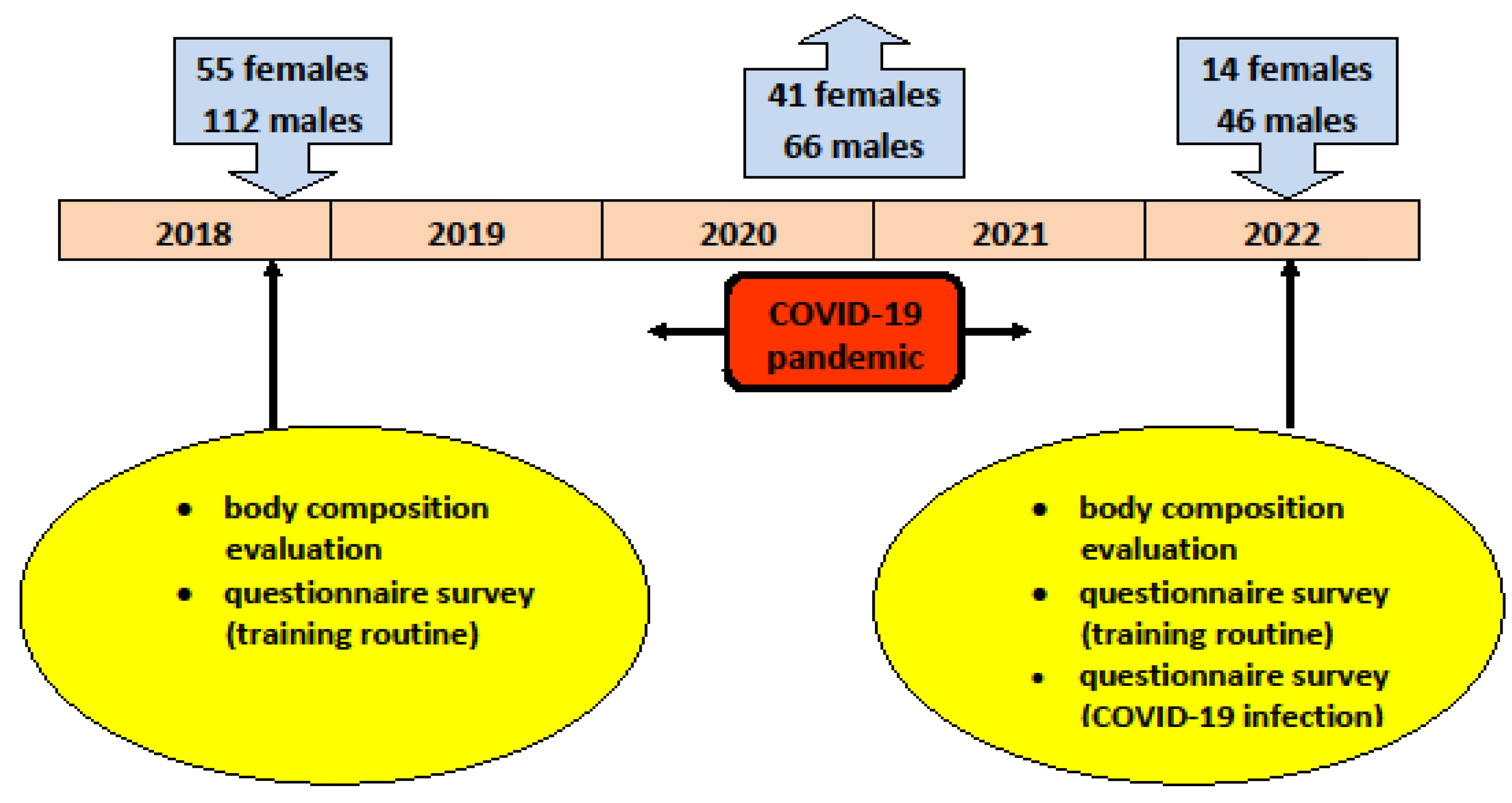
2.1. Study Design and Participants
2.2. Data Collection
2.3. Indicators
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Langhammer, B.; Bergland, A.; Rydwik, E. The importance of physical activity exercise among older people. BioMed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef] [PubMed]
- Ferencz, B.; Laukka, E.J.; Welmer, A.-K.; Kalpouzos, G.; Angleman, S.; Keller, L.; Graff, C.; Lovden, M.; Backman, L. The benefits of staying active in old age: Physical activity counteracts the negative influence of PICALM, BIN1, and CLU risk alleles on episodic memory functioning. Psychol. Aging 2014, 29, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Musich, S.; Wang, S.S.; Hawkins, K.; Greame, C. The frequency and health benefits of physical activity for older adults. Popul. Health Manag. 2017, 20, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Hupin, D.; Roche, F.; Gremeaux, V.; Chatard, J.-C.; Oriol, M.; Gaspoz, J.-M.; Barthelemy, J.-C.; Edouard, P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged > 60 years: A systematic review and meta-analysis. Brit. J. Sports Med. 2015, 49, 1262–1267. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.-Z.; No, M.-H.; Heo, J.-W.; Park, D.-H.; Kang, J.-H.; Kim, S.H.; Kwak, H.-B. Role of exercise in age-related sarcopenia. J. Exerc. Rehab. 2018, 14, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Fien, S.; Climstein, M.; Clodagh, Q.; Buckley, G.; Henwood, T.; Grigg, J.; Keogh, J.W.L. Anthropometric, physical function and general health markers of Master athletes: A cross-sectional study. Peer J. 2017, 5, e3768. [Google Scholar] [CrossRef] [PubMed]
- World Master Athletics. Competition and Technical Rules 2019–2020. Available online: https://world-masters-athletics.org/wp-content/uploads/2019/12/2019-2020-WMA-RULES-OF-COMPETITION-1-Dec-211246.pdf (accessed on 10 October 2023).
- International Masters Games Association. Canoeing at IMGA Master Games. Available online: https://imga.ch/masters-sports/sports-and-disciplines/canoe-kayak/ (accessed on 10 October 2023).
- Deck, S.; Doherty, A.; Hall, C.; Schneider, A.; Patil, S.; Belfry, G. Perceived time, frequency, and intensity of engagement and older Master athletes subjective experiences. Front. Sports Act. Living 2021, 3, 653590. [Google Scholar] [CrossRef] [PubMed]
- Gries, K.J.; Trappe, S.W. The aging athlete: Paradigm of healthy aging. Int. J. Sports Med. 2022, 43, 661–678. [Google Scholar] [CrossRef]
- Zhao, E.; Tranovich, M.J.; De Angelo, R.; Kontos, A.P.; Wright, V.J. Chronic exercise preserves brain function in master athletes when compared to sedentary counterparts. Phys. Sportsmed. 2015, 44, 8–13. [Google Scholar] [CrossRef]
- Sallinen, J.; Ojanen, T.; Karavirta, L.; Ahtiainen, J.P.; Hakkinen, K. Muscle mass and strength, body composition and dietary intake in master strength athletes vs untrained men of different ages. J. Sports Med. Phys. Fitness 2008, 48, 190–196. [Google Scholar]
- Herbert, P.; Hayes, L.D.; Sculthorpe, N.; Grace, F.M. High intensity interval training (HIIT) increases insulin-like growth factor-I (IGF-I) in sedentary aging men but not masters’ athletes: An observational study. Aging Male 2017, 20, 54–59. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Washif, J.A.; Farooq, A.; Krug, I.; Pyne, D.B.; Verhagen, E.; Taylor, L.; Wong, D.P.; Mujika, I.; Cortis, C.; Haddad, M.; et al. Training during the COVID-19 lockdown: Knowledge, beliefs, and practices of 12,526 athletes from 142 countries and six continents. Sports Med. 2022, 52, 933–948. [Google Scholar] [CrossRef] [PubMed]
- Breidenbach, P.; Mitze, T. Large-scale sport events and COVID-19 infection effects: Evidence from the German professional football ‘experiment’. Econom. J. 2022, 25, 15–45. [Google Scholar] [CrossRef]
- Washif, J.A.; Mujika, I.; DeLang, M.D.; Brito, J.; Dellal, A.; Haugen, T.; Hassanmirzaei, B.; Wong, D.P.; Farooq, A.; Donmez, G.; et al. Training practices of football players during the early COVID-19 lockdown worldwide. Int. J. Sports Physiol. Perform. 2022, 18, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Ambrozy, T.; Rydzik, L.; Obminski, Z.; Klimek, A.T.; Serafin, N.; Litwiniuk, A.; Czaja, R.; Czarny, W. The impact of reduced training activity of elite kickboxers on physical fitness, body build, and performance during competitions. Int. J. Environ. Res. Public Health 2021, 18, 4342. [Google Scholar] [CrossRef] [PubMed]
- Andre, M.J.G.; Georges, M.V.; Prosper, L.; Dorel, M.K.; Didace, M.M.; Robert, M.B.J.; Alphonse, M. Effect of COVID-19 lockdown on body composition and fitness performance among football players in Negro African environment. Health 2022, 14, 456–475. [Google Scholar] [CrossRef]
- Shaw, K.A.; Bertrand, L.; Deprez, D.; Ko, J.; Zello, G.A.; Chilibeck, P.D. The impact of the COVID-19 pandemic on the diet, training habits and fitness of Master cyclists. Nutr. Health 2022, 28, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Minuzzi, L.G.; Teixeira, A.M.; Thomatieli-Santos, R.V.; Rosa-Neto, J.C.; Lira, F.S. Immunometabolism and COVID-19: Could lifelong exercise training have a protective effect? Immunometabolism 2021, 3, e210001. [Google Scholar] [CrossRef]
- Campa, F.; Bongiovanni, T.; Trecroci, A.; Rossi, A.; Greco, G.; Pasta, G.; Coratella, G. Effects of COVID-19 lockdown on body composition and bioelectrical phase angle in Serie A soccer players: A comparison of two consecutive seasons. Biology 2021, 10, 1175. [Google Scholar] [CrossRef]
- Yasuda, J.; Kondo, E.; Takai, E.; Eda, N.; Azuma, Y.; Motonaga, K.; Dohi, M.; Kamei, A. The effects of the COVID-19 environments on changes in body composition in Japanese elite fencing athletes. Sports 2021, 9, 95. [Google Scholar] [CrossRef]
- Huebner, M.; Ma, W.; Rieger, T. Weightlifting during the COVID-19 pandemic—A transnational study regarding motivation, barriers, and coping of Master athletes. Int. J. Environ. Res. Public Health 2021, 18, 9343. [Google Scholar] [CrossRef] [PubMed]
- Del Brutto, O.H.; Mera, R.M.; Rumbea, D.A.; Perez, P.; Recalde, B.Y.; Sedler, M.J. Body composition in community-dwelling older adults before and after SARS-CoV-2 infection: A longitudinal prospective study in a rural village struck by the Pandemic. J. Prim. Care Community Health 2021, 12, 21501327211047781. [Google Scholar] [CrossRef] [PubMed]
- Acedo, C.; Roncero-Martin, R.; Sanchez-Fernandez, A.; Mendoza-Holgado, C.; Pedrera-Canal, M.; Lopez-Espuela, F.; Rey-Sanchez, P.; Pedrera-Zamorano, J.D.; Puerto-Pajero, L.M.; Moran, J.M.; et al. Body composition and nutrients dietary intake changes during COVID-19 lockdown in Spanish healthy postmenopausal women. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.-Y.; Li, Y.; Wang, Q. Sarcopenia: An underlying treatment target during the COVID-19 pandemic. Nutrition 2021, 84, 111104. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.P.; Muollo, V.; Dalla Valle, Z.; Urbani, S.; Pellegrini, M.; El Ghoch, M.; Mazzali, G. The role of obesity, body composition, and nutrition in COVID-19 pandemia: A narrative review. Nutrients 2022, 14, 3493. [Google Scholar] [CrossRef] [PubMed]
- Shimokata, H.; Ando, F.; Yuki, A.; Otsuka, R. Age-related changes in skeletal muscle mass among community-dwelling Japanese: A 12-year longitudinal study. Geriatr. Gerontol. Int. 2014, 14 (Suppl. S1), 85–92. [Google Scholar] [CrossRef] [PubMed]
- Goździejewska, A.; Skrzypczak, A.; Wojcik, A. Social, economics, and tourist aspect of master swimming. Folia Pomer. Univ. Technol. Stetinesis 2016, 324, 19–28. [Google Scholar] [CrossRef]
- Tanaka, S.; Jung, H.; Tanaka, R. Identifying target values of body composition for preventing frailty: A descriptive study in older adults. Gerontol. Geriatr. Med. 2022, 8, 1–6. [Google Scholar] [CrossRef]
- Czartoryski, P.; Garcia, J.; Manimaleth, R.; Napolitano, P.; Watters, H.; Weber, C.; Alvarez-Beaton, A.; Nieto, A.C.; Patel, A.; Peacock, C. Body composition assessment: A comparison of DXA, InBody 270, and Omron. J. Exerc. Nutr. 2020, 3, 1–6. [Google Scholar]
- Available online: https://www.wszz.torun.pl/poradnie/szpital-wielospecjalistyczny/regionalne-centrum-kardiologii/poradnia-kardiologiczna-post-covid-19/ (accessed on 20 April 2022).
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Jespers, A.; Brink, M.S.; Probst, S.G.M.; Frencken, W.G.P.; Helsen, W. Relationships between training load indicators and training outcomes in professional soccer. Sports Med. 2017, 47, 533–544. [Google Scholar] [CrossRef]
- Benelli, P.; Ditroilo, M.; Forte, R.; De Vito, G.; Stocchi, V. Assessment of post-competition peak blood lactate in male and female master swimmers aged 40-79 years and its relationship with swimming performance. Eur. J. Appl. Physiol. 2007, 99, 685–693. [Google Scholar] [CrossRef]
- Hopkins, W.G. A New View of Statistics. Internet Society for Sport Science. Available online: http://www.sportsci.org/resource/stats/ (accessed on 19 September 2023).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routlege: New York, NY, USA, 1988; pp. 73–105. [Google Scholar] [CrossRef]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef]
- World Health Organization. Waist Circumference and Waist-to-Hip Ratio: Report of a WHO Expert Consultation; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Alvero-Cruz, J.R.; Garcia Romero, J.C.; Ordonez, F.J.; Mongin, D.; Correas-Gomez, L.; Nikolaidis, P.T.; Knechtle, B. Age and training-related changes on body composition and fitness in male amateur cyclists. Int. J. Environ. Res. Public Health 2022, 19, 93. [Google Scholar] [CrossRef]
- Raguso, C.A.; Kyle, U.; Kossovsky, M.P.; Roynette, C.; Paoloni-Giacombino, A.; Didier, H.; Genton, L.; Pichard, C. A 3-year longitudinal study on body composition changes in elderly: Role of physical exercise. Clin. Nutr. 2006, 25, 573–580. [Google Scholar] [CrossRef]
- Sawczyn, M. The influence of 12 week aerobic training, aerobic-strength training and strength training on body composition of women of different ages. Rocz. Nauk. AWFiS Gdansku 2018, 28, 65–75. [Google Scholar]
- Mohammadi, H.R.; Khoshnam, M.S.; Khoshnam, E. Effects of different modes of exercise training on body composition and risk factors for cardiovascular disease in middle-aged men. Int. J. Prev. Med. 2018, 9, 9. [Google Scholar] [CrossRef]
- Buckinx, F.; Peyrusque, E.; Granet, J.; Aubertin-Leheudre, M. Impact of current and past physical activity level on functional capacities and body composition among elderly people: A cross-sectional analysis from the YMCA study. Arch. Public Health 2021, 79, 50. [Google Scholar] [CrossRef]
- de Mendonca, R.M.S.C.; de Araujo Junior, A.T.; de Sousa, M.S.C.; Fernandes, H.M. The effects of different exercise programmes on female body composition. J. Hum. Kinet. 2014, 43, 67–78. [Google Scholar] [CrossRef][Green Version]
- Kirwan, R.; Mc Cullogh, D.; Butler, T.; de Hereida, F.P.; Davies, I.G.; Stewart, C. Sarcopenia during COVID-19 lockdown restrictions: Long-term health effects of short-term muscle loss. GeroScience 2020, 42, 1547–1578. [Google Scholar] [CrossRef]
- Tsolakis, C.; Cherouveim, E.D.; Viliotis, A.; Simeonidis, T.; Skouras, A.; Koulouvaris, P. Effect of home-based exercise program on anthropometric characteristics and exercise performance during COVID-19 quarantine in young high-level kayak athletes. Sport Sci. Health 2023, 19, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Ghiani, G.; Roberto, S.; Mura, R.; Fois, F.; Scorcu, M.; Crisafulli, A. Body composition changes during the lockdown-restart transition due to SARS-CoV-2 pandemic in a group of professional football players. J. Sports Med. Phys. Fitness 2022, 62, 649–653. [Google Scholar] [CrossRef] [PubMed]
- Spyrou, K.; Alcaraz, P.E.; Marin-Cascales, E.; Herrero-Carrasco, R.; Cohen, D.D.; Calleja-Gonzales, J.; Pereira, L.A.; Lotourco, I.; Freitas, T.T. Effects of the COVID-19 lockdown on neuromuscular performance and body composition in elite futsal payers. J. Strength Cond. Res. 2021, 35, 2309–2315. [Google Scholar] [CrossRef] [PubMed]
- Yoshiji, S.; Tanaka, D.; Minamino, H.; Lu, T.; Butler-Laporte, G.; Murakami, T.; Fujita, Y.; Richards, J.B.; Inagaki, N. Casual associations between body fat accumulation and COVID-19 severity: A Mendelian randomization study. Front. Endocrinol. 2022, 13, 899625. [Google Scholar] [CrossRef] [PubMed]
- Macek, P.; Terek-Derszniak, M.; Biskup, M.; Krol, H.; Smok-Kalwat, J.; Gozdz, S.; Zak, M. Assessment of age-induced changes in body fat percentage, and BMI aided by Bayesian modelling: A cross-sectional cohort study in middle-aged and older adults. Clin. Interv. Aging 2020, 15, 2301–2311. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Gahete, F.J.; Jurado-Fasoli, L.; Ruiz, J.R.; Castillo, M.J. Association of basal metabolic rate and nutrients oxidation with cardiometabolic risk factors and insulin sensitivity in sedentary middle-aged adults. Nutrients 2020, 12, 1186. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Hu, F.; Wang, T.; Zhou, W.; Zhu, L.; Huang, X.; Bao, H.; Cheng, X. Association between basal metabolic rate and all-cause mortality in a prospective cohort of southern Chinese adults. Front. Physiol. 2022, 12, 790347. [Google Scholar] [CrossRef]
- Bosman, A.; Campos-Obando, N.; Medina-Gomez, C.; Voortman, T.; Uitterlinden, A.G.; Zillikens, M.C. Serum phosphate, BMI, and body composition of middle-aged and older adults: A cross-sectional association analysis and bidirectional Mendelian randomization study. J. Nutr. 2022, 152, 276–285. [Google Scholar] [CrossRef]
- Danielewicz, A.; Morze, J.; Obara-Golebiowska, M.; Przybylowicz, M.; Przybylowicz, K.E. Nutrient patterns and skeletal muscle mass index among Polish women: A cross-sectional study. Scient. Rep. 2019, 9, 18930. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, K.W.; Kang, J.; Ki, Y.-J.; Chang, M.; Han, J.-K.; Yang, H.-M.; Kang, H.-J.; Koo, B.-K.; Kim, H.-S. Sarcopenia Index as a predictor of clinical outcomes in older patients with coronary artery disease. J. Clin. Med. 2020, 9, 3121. [Google Scholar] [CrossRef]
- Krzyminska-Siemaszko, R.; Czepulis, N.; Rzepnicka, A.; Dworak, L.B.; Wieczorowska-Tobis, K. Assassment of risk of sarcopenia in older women. Now. Lek. 2013, 82, 19–24. [Google Scholar]
- Wallengren, O.; Bosaeus, I.; Frandin, K.; Lissner, L.; Erhag, H.F.; Wetterberg, H.; Sterner, T.R.; Ryden, L.; Rothenberg, E.; Skoog, I. Comparison of the 2010 and 2019 diagnostic criteria for sarcopenia by the European Working Group on Sarcopenia in Older People (EWGSOP) in two cohorts of Swedish older adults. BMC Geriatr. 2021, 21, 600. [Google Scholar] [CrossRef]
- Bredella, M.A. Sex Differences in Body Composition. In Sex and Gender Factors Affecting Metabolic Homeostasis, Diabetes and Obesity. Advances in Experimental Medicine and Biology; Mauvais-Jarvis, F., Ed.; Springer: Hanover, PA, USA, 2017; Volume 1043, pp. 9–27. ISBN 978-3-319-70177-6. [Google Scholar]
| Sex | Age [Years] | Body Height [cm] | Number of Training Sessions per Week | Distance Covered in Training Session [km] | Training Intensity Index | Sports Experience [Years] |
|---|---|---|---|---|---|---|
| Males (n = 46) | 47.0 ± 11.0 | 180.2 ± 4.8 | 3.2 ± 1.1 | 2.8 ± 0.9 | 9.9 ± 5.3 | 17.0 ± 11.1 |
| Females (n = 14) | 47.2 ± 12.2 | 165.7 ± 8.3 | 3.0 ± 1.2 | 2.7 ± 0.8 | 8.6 ± 4.8 | 15.0 ± 7.5 |
| Males (n = 46) | t-Test p Value/ Cohen’s d | Females (n = 14) | t-Test p-Value/ Cohen’s d | ||
|---|---|---|---|---|---|
| Body mass [kg] | PRE | 83.73 ± 8.48 | p = 0.831 d = 0.010 | 62.49 ± 7.68 | p = 0.593 d = 0.046 |
| POST | 83.82 ± 9.04 | 62.84 ± 7.66 | |||
| Total body water [L] | PRE | 51.08 ± 4.40 | p = 0.632 d = 0.019 | 35.13 ± 4.64 | p = 0.414 d = 0.044 |
| POST | 51.17 ± 4.80 | 34.93 ± 4.36 | |||
| Body fat mass [kg] | PRE | 14.13 ± 4.96 | p = 0.945 d = 0.004 | 14.63 ± 5.32 | p = 0.408 d = 0.115 |
| POST | 14.11 ± 4.93 | 15.22 ± 4.98 | |||
| Fat free mass [kg] | PRE | 69.59 ± 6.01 | p = 0.636 d = 0.019 | 47.86 ± 6.32 | p = 0.447 d = 0.041 |
| POST | 69.71 ± 6.59 | 47.61 ± 5.96 | |||
| Skeletal muscle mass [kg] | PRE | 39.66 ± 3.62 | p = 0.672 d = 0.018 | 26.36 ± 3.81 | p = 0.533 d = 0.032 |
| POST | 39.73 ± 4.02 | 26.24 ± 3.63 | |||
| Body mass index [kg/m2] | PRE | 25.74 ± 2.23 | p = 0.833 d = 0.013 | 22.79 ± 2.50 | p = 0.667 d = 0.041 |
| POST | 25.77 ± 2.36 | 22.89 ± 2.35 | |||
| Percent body fat [%] | PRE | 16.65 ± 4.58 | p = 0.919 d = 0.000 | 23.18 ± 7.30 | p = 0.347 d = 0.121 |
| POST | 16.65 ± 4.54 | 24.01 ± 6.44 | |||
| Basal metabolic rate [kcal] | PRE | 1873.13 ± 129.63 | p = 0.649 d = 0.019 | 1403.36 ± 136.57 | p = 0.503 d = 0.037 |
| POST | 1875.65 ± 142.40 | 1398.43 ± 128.60 | |||
| Waist-to-hip ratio | PRE | 0.870 ± 0.052 | p = 0.075 d = 0.155 | 0.846 ± 0.052 | p = 0.221 d = 0.367 |
| POST | 0.878 ± 0.051 | 0.864 ± 0.046 | |||
| Visceral fat level | PRE | 5.74 ± 2.42 | p = 0.679 d = 0.025 | 5.86 ± 2.66 | p = 0.362 d = 0.171 |
| POST | 5.80 ± 2.34 | 6.29 ± 2.37 | |||
| Muscle Mass Index [kg/m2] | PRE | 12.18 ± 0.75 | p = 0.729 | 9.55 ± 0.69 | p = 0.579 |
| POST | 13.00 ± 0.86 | d = 1.016 | 9.51 ± 0.64 | d = 0.060 | |
| Skeletal Muscle Index [%] | PRE | 47.48 ± 2.66 | p = 0.938 | 42.27 ± 4.30 | p = 0.370 |
| POST | 47.49 ± 2.67 | d = 0.004 | 41.83 ± 3.79 | d = 0.109 |
| Pearson’s Coefficient | p-Value | ||
|---|---|---|---|
| Body mass [kg] | PRE | 0.16 | 0.290 |
| POST | 0.15 | 0.329 | |
| Total body water [L] | PRE | 0.27 | 0.065 |
| POST | 0.31 | 0.037 | |
| Body fat mass [kg] | PRE | −0.06 | 0.678 |
| POST | −0.15 | 0.334 | |
| Fat-free mass [kg] | PRE | 0.27 | 0.064 |
| POST | 0.31 | 0.037 | |
| Skeletal muscle mass [kg] | PRE | 0.28 | 0.057 |
| POST | 0.33 | 0.026 | |
| Body mass index [kg/m2] | PRE | 0.07 | 0.654 |
| POST | 0.06 | 0.689 | |
| Percent body fat [%] | PRE | −0.14 | 0.366 |
| POST | −0.24 | 0.100 | |
| Basal metabolic rate [kcal] | PRE | 0.27 | 0.064 |
| POST | 0.31 | 0.035 | |
| Waist-to-hip ratio | PRE | −0.07 | 0.640 |
| POST | −0.10 | 0.513 | |
| Visceral fat level | PRE | −0.07 | 0.637 |
| POST | −0.14 | 0.340 | |
| Muscle Mass Index [kg/m2] | PRE | 0.26 | 0.083 |
| POST | 0.33 | 0.024 | |
| Skeletal Muscle Index [%] | PRE | 0.17 | 0.258 |
| POST | 0.31 | 0.038 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bielec, G.; Goździejewska, A.; Langhammer, B.; Borysławski, K. Body Composition of Master Swimmers before and after the COVID-19 Pandemic: A Longitudinal Study. J. Clin. Med. 2023, 12, 6992. https://doi.org/10.3390/jcm12226992
Bielec G, Goździejewska A, Langhammer B, Borysławski K. Body Composition of Master Swimmers before and after the COVID-19 Pandemic: A Longitudinal Study. Journal of Clinical Medicine. 2023; 12(22):6992. https://doi.org/10.3390/jcm12226992
Chicago/Turabian StyleBielec, Grzegorz, Anna Goździejewska, Birgitta Langhammer, and Krzysztof Borysławski. 2023. "Body Composition of Master Swimmers before and after the COVID-19 Pandemic: A Longitudinal Study" Journal of Clinical Medicine 12, no. 22: 6992. https://doi.org/10.3390/jcm12226992
APA StyleBielec, G., Goździejewska, A., Langhammer, B., & Borysławski, K. (2023). Body Composition of Master Swimmers before and after the COVID-19 Pandemic: A Longitudinal Study. Journal of Clinical Medicine, 12(22), 6992. https://doi.org/10.3390/jcm12226992






