Recurrence and Complication Rates of Surgical Treatment for Blount’s Disease in Children: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
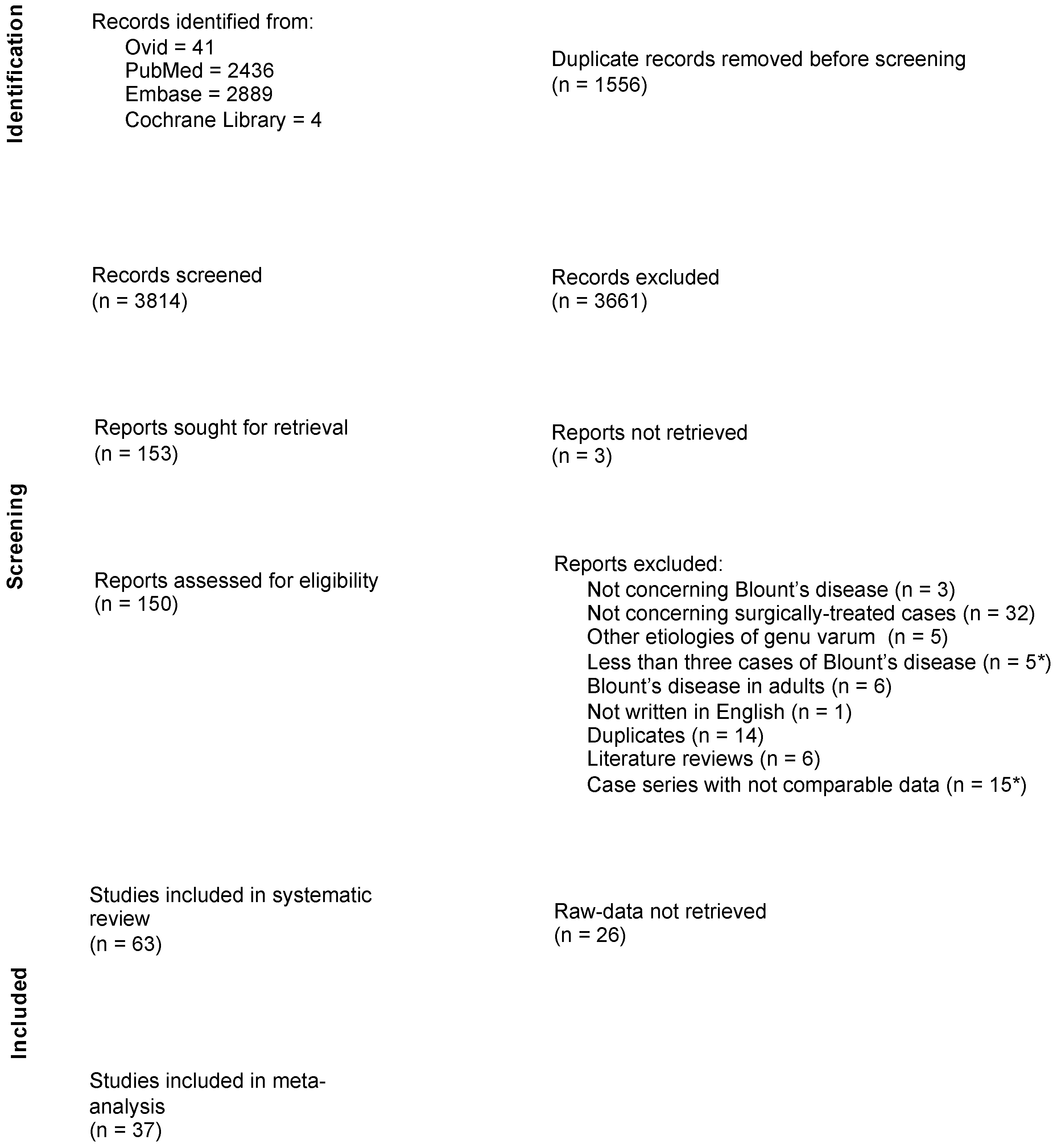
2.1. Bibliographic Research
2.2. Inclusion and Exclusion Criteria
2.3. Selection of Articles
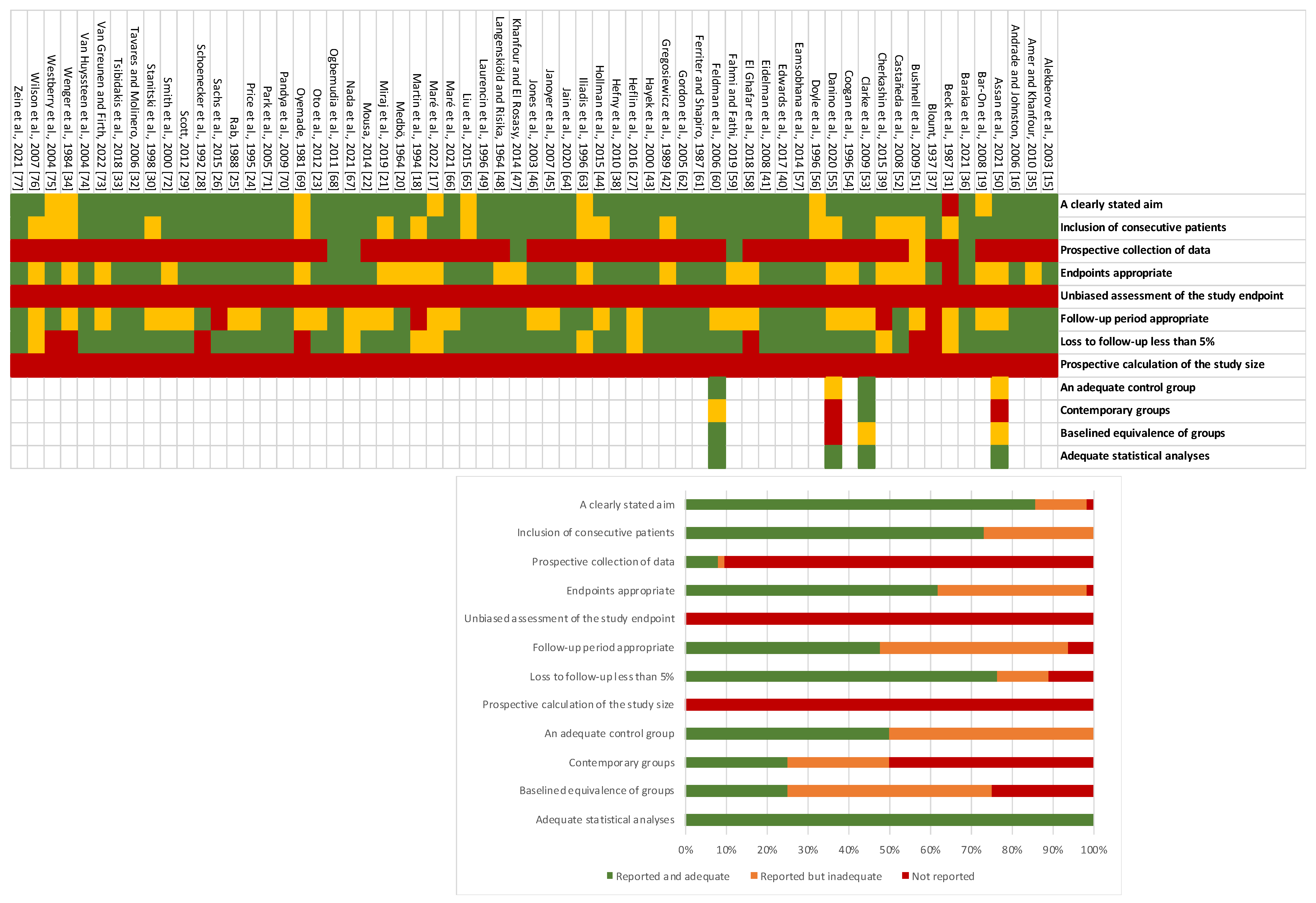
2.4. Methodological Quality and Risk of Bias Assessment
2.5. Data Extraction
- -
- gradual correction of at least one of the deformities (GC);
- -
- gradual correction of at least one of the deformities, combined with hemiepiphysiodesis (GC + hE);
- -
- acute correction of all deformities (AC);
- -
- acute correction of all deformities, combined with hemiepiphysiodesis (AC + hE);
- -
- isolated growth modulation via hemiepiphysiodesis (hE);
- -
- hemichondrodiastasis (hChD).
2.6. Statistical Analysis
3. Results
3.1. Characteristics and Methodological Qualities of the Included Studies
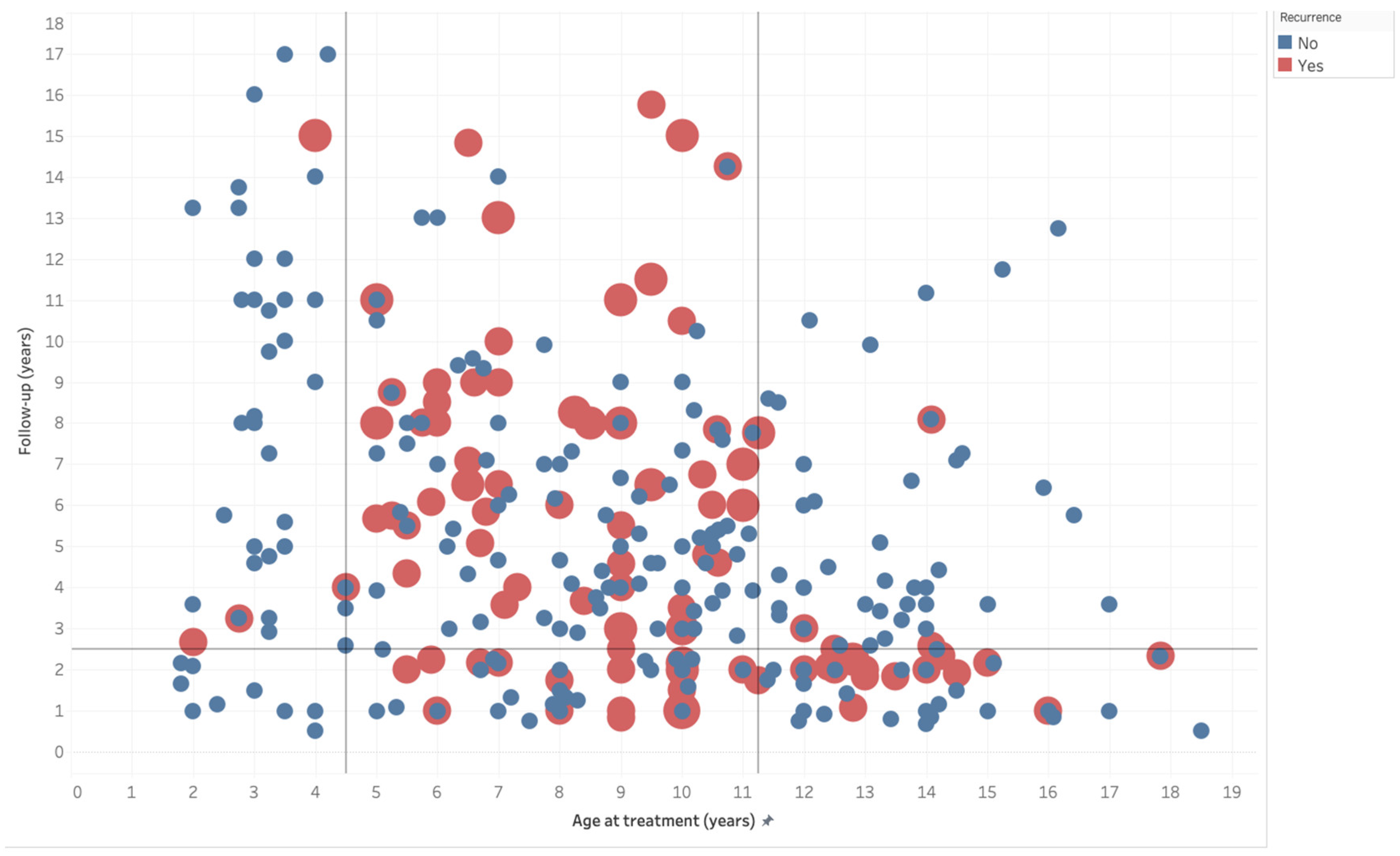
3.2. Demographics, Clinical, and Radiographic Characteristics
3.3. Surgical Outcomes, Recurrence, and Complications
4. Discussion
4.1. Definition of ITV/LOTV Subgroups
4.2. Overall Treatment Prognosis
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rivero, S.M.; Zhao, C.; Sabharwal, S. Are Patient Demographics Different for Early-Onset and Late-Onset Blount Disease? Results Based on Meta-Analysis. J. Pediatr. Orthop. B 2015, 24, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Janoyer, M. Blount Disease. Orthop. Traumatol. Surg. Res. 2019, 105, S111–S121. [Google Scholar] [CrossRef] [PubMed]
- Herring, J. Tachdjian’s Pediatric Orthopaedics: From the Texas Scottish Rite Hospital for Children, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2020; ISBN 9780323567695. [Google Scholar]
- Khanfour, A.A. Blount’s Disease—An up-to-Date Insight with Contemporary Treatment Guidelines Deduced from Critical Analysis of a Large 146 Surgical Case Series. J. Pediatr. Orthop. B 2021, 30, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Flynn, J.M.; Flynn, J.; Flynn, D.J.M. Lovell and Winter’s Pediatric Orthopaedics; Wolters Kluwer Health: Philadelphia, PA, USA, 2014; ISBN 9781469878812. [Google Scholar]
- Sabharwal, S. Blount Disease. J. Bone Jt. Surg. 2009, 91, 1758–1776. [Google Scholar] [CrossRef]
- Funk, S.S.; Mignemi, M.E.; Schoenecker, J.G.; Lovejoy, S.A.; Mencio, G.A.; Martus, J.E. Hemiepiphysiodesis Implants for Late-Onset Tibia Vara: A Comparison of Cost, Surgical Success, and Implant Failure. J. Pediatr. Orthop. 2016, 36, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The Levels of Evidence and Their Role in Evidence-Based Medicine. Plast. Reconstr. Surg. 2011, 128, 305. [Google Scholar] [CrossRef] [PubMed]
- Coleman, B.D.; Khan, K.M.; Maffulli, N.; Cook, J.L.; Wark, J.D. Studies of Surgical Outcome after Patellar Tendinopathy: Clinical Significance of Methodological Deficiencies and Guidelines for Future Studies. Victorian Institute of Sport Tendon Study Group. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (Minors): Development and Validation of a New Instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Dodwell, E.R.; Pathy, R.; Widmann, R.F.; Green, D.W.; Scher, D.M.; Blanco, J.S.; Doyle, S.M.; Daluiski, A.; Sink, E.L. Reliability of the Modified Clavien-Dindo-Sink Complication Classification System in Pediatric Orthopaedic Surgery. JBJS Open Access 2018, 3, E0020. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G.; on behalf of the Cochrane Statistical Methods Group. Analysing Data and Undertaking Meta-Analyses. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 241–284. ISBN 9781119536604. [Google Scholar]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Alekberov, C.; Shevtsov, V.I.; Karatosun, V.; Günal, I.; Alici, E. Treatment of Tibia Vara by the Ilizarov Method. Clin. Orthop. Relat. Res. 2003, 409, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Andrade, N.; Johnston, C.E. Medial Epiphysiolysis in Severe Infantile Tibia Vara. J. Pediatr. Orthop. 2006, 26, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Maré, P.H.; Thompson, D.M.; Marais, L.C. Guided Growth Using a Tension-Band Plate in Blount’s Disease. J. Pediatr. Orthop. B 2022, 31, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.D.; Moran, M.C.; Martin, T.L.; Burke, S.W. Proximal Tibial Osteotomy with Compression Plate Fixation for Tibia Vara. J. Pediatr. Orthop. 1994, 14, 619–622. [Google Scholar] [CrossRef]
- Bar-On, E.; Weigl, D.M.; Becker, T.; Katz, K. Treatment of Severe Early Onset Blount’s Disease by an Intra-Articular and a Metaphyseal Osteotomy Using the Taylor Spatial Frame. J. Child. Orthop. 2008, 2, 457–461. [Google Scholar] [CrossRef]
- Medbö, I. Tibia Vara (Osteochondrosis Deformans Tibiae or Blount’s Disease): Treatment and Follow-up Examination. Acta Orthop. 1964, 34, 323–336. [Google Scholar] [CrossRef]
- Miraj, F.; Ajiantoro; Arya Mahendra Karda, I.W. Step Cut “V” Osteotomy for Acute Correction in Blount’s Disease Treatment: A Case Series. Int. J. Surg. Case Rep. 2019, 58, 57–62. [Google Scholar] [CrossRef]
- Mousa, W.F.A. Proximal Tibial Chevron Osteotomy in Treating Adolescent Tibia Vara. Undefined 2014, 25, 152–157. [Google Scholar] [CrossRef]
- Oto, M.; Yılmaz, G.; Bowen, J.R.; Thacker, M.; Kruse, R. Adolescent Blount Disease in Obese Children Treated by Eight-Plate Hemiepiphysiodesis. Eklem Hastalik. Cerrahisi 2012, 23, 20–24. [Google Scholar]
- Price, C.T.; Scott, D.S.; Greenberg, D.A. Dynamic Axial External Fixation in the Surgical Treatment of Tibia Vara. J. Pediatr. Orthop. 1995, 15, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Rab, G.T. Oblique Tibial Osteotomy for Blount’s Disease (Tibia Vara). J. Pediatr. Orthop. 1988, 8, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Sachs, O.; Katzman, A.; Abu-Johar, E.; Eidelman, M. Treatment of Adolescent Blount Disease Using Taylor Spatial Frame With and Without Fibular Osteotomy: Is There Any Difference? J. Pediatr. Orthop. 2015, 35, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Heflin, J.A.; Ford, S.; Stevens, P. Guided Growth for Tibia Vara (Blount’s Disease). Medicine 2016, 95, e4951. [Google Scholar] [CrossRef]
- Schoenecker, P.L.; Johnston, R.; Rich, M.M.; Capelli, A.M. Elevation of the Medical Plateau of the Tibia in the Treatment of Blount Disease. J. Bone Jt. Surg. Am. 1992, 74, 351–358. [Google Scholar] [CrossRef]
- Scott, A.C. Treatment of Infantile Blount Disease with Lateral Tension Band Plating. J. Pediatr. Orthop. 2012, 32, 29–34. [Google Scholar] [CrossRef]
- Stanitski, D.F.; Srivastava, P.; Stanitski, C.L. Correction of Proximal Tibial Deformities in Adolescents with the T-Garches External Fixator. J. Pediatr. Orthop. 1998, 18, 512–517. [Google Scholar] [CrossRef]
- Beck, C.L.; Burke, S.W.; Roberts, J.M.; Johnston, C.E.I.I. Physeal Bridge Resection in Infantile Blount Disease. J. Pediatr. Orthop. 1987, 7, 161–163. [Google Scholar] [CrossRef]
- Tavares, J.O.; Molinero, K. Elevation of Medial Tibial Condyle for Severe Tibia Vara. J. Pediatr. Orthop. B 2006, 15, 362–369. [Google Scholar] [CrossRef]
- Tsibidakis, H.; Panou, A.; Angoules, A.; Sakellariou, V.I.; Portinaro, N.M.; Krumov, J.; Kanellopoulos, A.D. The Role of Taylor Spatial Frame in the Treatment of Blount Disease. Folia Med. 2018, 60, 208–215. [Google Scholar] [CrossRef]
- Wenger, D.R.; Mickelson, M.; Maynard, J.A. The Evolution and Histopathology of Adolescent Tibia Vara. J. Pediatr. Orthop. 1984, 4, 78–88. [Google Scholar] [CrossRef]
- Amer, A.R.A.L.; Khanfour, A.A. Evaluation of Treatment of Late-Onset Tibia Vara Using Gradual Angulation Translation High Tibial Osteotomy. Acta Orthop. Belg. 2010, 76, 360–366. [Google Scholar]
- Baraka, M.M.; Hefny, H.M.; Mahran, M.A.; Fayyad, T.A.; Abdelazim, H.; Nabil, A. Single-Stage Medial Plateau Elevation and Metaphyseal Osteotomies in Advanced-Stage Blount’s Disease: A New Technique. J. Child. Orthop. 2021, 15, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Blount, W.P. Tibia Vara: Osteochondrosis Deformans Tibiae. JBJS 1937, 19, 1–29. [Google Scholar]
- Hefny, H.; Shalaby, H. A Safer Technique for the Double Elevation Osteotomy in Severe Infantile Tibia Vara. Strateg. Trauma Limb Reconstr. 2010, 5, 79–85. [Google Scholar] [CrossRef]
- Cherkashin, A.M.; Samchukov, M.L.; Birch, J.G.; Da Cunha, A.L.M. Evaluation of Complications of Treatment of Severe Blount’s Disease by Circular External Fixation Using a Novel Classification Scheme. J. Pediatr. Orthop. B 2015, 24, 123–130. [Google Scholar] [CrossRef]
- Edwards, T.A.; Hughes, R.; Monsell, F. The Challenges of a Comprehensive Surgical Approach to Blount’s Disease. J. Child. Orthop. 2017, 11, 479–487. [Google Scholar] [CrossRef]
- Eidelman, M.; Bialik, V.; Katzman, A. The Use of the Taylor Spatial Frame in Adolescent Blount’s Disease: Is Fibular Osteotomy Necessary? J. Child. Orthop. 2008, 2, 199–204. [Google Scholar] [CrossRef]
- Gregosiewicz, A.; Wośko, I.; Kandzierski, G.; Drabik, Z. Double-Elevating Osteotomy of Tibiae in the Treatment of Severe Cases of Blount’s Disease. J. Pediatr. Orthop. 1989, 9, 178–181. [Google Scholar] [CrossRef]
- Hayek, S.; Segev, E.; Ezra, E.; Lokiec, F.; Wientroub, S. Serrated W/M Osteotomy. Results Using a New Technique for the Correction of Infantile Tibia Vara. J. Bone Jt. Surg. Br. 2000, 82, 1026–1029. [Google Scholar] [CrossRef]
- Hollman, F.; Korpisah, J.; Ismail, A.; Rompa, P.; Moh, P.; Van Rhijn, L.W.; Staal, H.M. W/M Serrated Osteotomy for Infantile Blount’s Disease in Ghana: Short-Term Results. Niger. J. Clin. Pract. 2016, 19, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Janoyer, M.; Jabbari, H.; Rouvillain, J.L.; Sommier, J.; Py, G.; Catonné, Y.; Colombani, J.F. Infantile Blount’s Disease Treated by Hemiplateau Elevation and Epiphyseal Distraction Using a Specific External Fixator: Preliminary Report. J. Pediatr. Orthop. B 2007, 16, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Hosalkar, H.S.; Hill, R.A.; Hartley, J. Relapsed Infantile Blount’s Disease Treated by Hemiplateau Elevation Using the Ilizarov Frame. J. Bone Jt. Surg. Br. 2003, 85, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Khanfour, A.A.; El-Rosasy, M. Late Onset Tibia Vara. Acute Correction Strategy: Proper Case Selection and a Simple External Fixation Technique. Acta Orthop. Belg. 2014, 80, 241–250. [Google Scholar]
- Langenskiöld, A.; Risika, E.B. Tibia Vara (Osteochondrosis Deformans Tibiae): A Survey of Seventy-One Cases. J. Bone Jt. Surg. Am. 1964, 46, 1405–1420. [Google Scholar] [CrossRef]
- Laurencin, C.T.; Ferriter, P.J.; Millis, M.B. Oblique Proximal Tibial Osteotomy for the Correction of Tibia Vara in the Young. Clin. Orthop. Relat. Res. 1996, 327, 218–224. [Google Scholar] [CrossRef]
- Assan, B.R.; Simon, A.L.; Adjadohoun, S.; Segbedji, G.G.P.; Souchet, P.; Metchioungbe, C.S.; Fiogbe, M.A.; Ilharreborde, B.; Gbenou, A.S. Guided Growth vs. Tibial Osteotomy at Early Stage of Blount Disease in Squelletically Immature Patients. J. Orthop. 2021, 25, 140–144. [Google Scholar] [CrossRef]
- Bushnell, B.D.; May, R.; Campion, E.R.; Schmale, G.A.; Henderson, R.C. Hemiepiphyseodesis for Late-Onset Tibia Vara. J. Pediatr. Orthop. 2009, 29, 285–289. [Google Scholar] [CrossRef]
- Castañeda, P.; Urquhart, B.; Sullivan, E.; Haynes, R.J. Hemiepiphysiodesis for the Correction of Angular Deformity about the Knee. J. Pediatr. Orthop. 2008, 28, 188–191. [Google Scholar] [CrossRef]
- Clarke, S.E.; McCarthy, J.J.; Davidson, R.S. Treatment of Blount Disease: A Comparison between the Multiaxial Correction System and Other External Fixators. J. Pediatr. Orthop. 2009, 29, 103–109. [Google Scholar] [CrossRef]
- Coogan, P.G.; Fox, J.A.; Fitch, R.D. Treatment of Adolescent Blount Disease with the Circular External Fixation Device and Distraction Osteogenesis. J. Pediatr. Orthop. 1996, 16, 450–454. [Google Scholar] [CrossRef]
- Danino, B.; Rödl, R.; Herzenberg, J.E.; Shabtai, L.; Grill, F.; Narayanan, U.; Gigi, R.; Segev, E.; Wientroub, S. The Efficacy of Guided Growth as an Initial Strategy for Blount Disease Treatment. J. Child. Orthop. 2020, 14, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Doyle, B.S.; Volk, A.G.; Smith, C.F. Infantile Blount Disease: Long-Term Follow-up of Surgically Treated Patients at Skeletal Maturity. J. Pediatr. Orthop. 1996, 16, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Eamsobhana, P.; Kaewpornsawan, K.; Yusuwan, K. Do We Need to Do Overcorrection in Blount’s Disease? Int. Orthop. 2014, 38, 1661–1664. [Google Scholar] [CrossRef] [PubMed]
- El Ghafar, K.A.; Samir, S.; Diab, R.A. Acute Correction of Proximal Tibial Varus Deformity in Adolescent Blount Disease with a Low-Profile Ilizarov Frame. Curr. Orthop. Pract. 2018, 29, 231–236. [Google Scholar] [CrossRef]
- Fahmy, F.S.; Fathi, H. Satisfactory Outcomes after Gradual Deformity Correction of Delayed Onset Blount Disease Using the Ilizarov Device. Curr. Orthop. Pract. 2019, 30, 50–54. [Google Scholar] [CrossRef]
- Feldman, D.S.; Madan, S.S.; Ruchelsman, D.E.; Sala, D.A.; Lehman, W.B. Accuracy of Correction of Tibia Vara: Acute versus Gradual Correction. J. Pediatr. Orthop. 2006, 26, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Ferriter, P.J.; Shapiro, F. Infantile Tibia Vara: Factors Affecting Outcome Following Proximal Tibial Osteotomy. J. Pediatr. Orthop. 1987, 7, 1–7. [Google Scholar] [CrossRef]
- Gordon, J.E.; King, D.J.; Luhmann, S.J.; Dobbs, M.B.; Schoenecker, P.L. Femoral Deformity in Tibia Vara. J. Bone Jt. Surg. Am. 2006, 88, 380–386. [Google Scholar] [CrossRef][Green Version]
- Iliadis, A.; Morakis, A.; Dimitriou, J.K. High Tibial Osteotomy in the Treatment of Infantile Blount’s Disease. Bull. Hosp. Jt. Dis. 1996, 55, 20–24. [Google Scholar]
- Jain, M.J.; Inneh, I.A.; Zhu, H.; Phillips, W.A. Tension Band Plate (TBP)-Guided Hemiepiphysiodesis in Blount Disease: 10-Year Single-Center Experience with a Systematic Review of Literature. J. Pediatr. Orthop. 2020, 40, e138–e143. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Cao, L.; Guo, S.-F.; Xue, W.; Chen, Z.-X.; Tai, H.-P.; He, Z.-R.; Qian, Y.-W. Melt-Metaphyseal and Diphyseal Osteotomy for Correction of Infantile Blount’s Disease: A Long-Term Follow-up Study. Int. J. Clin. Exp. Med. 2015, 8, 2480–2483. [Google Scholar] [PubMed]
- Maré, P.H.; Thompson, D.M.; Marais, L.C. The Medial Elevation Osteotomy for Late-Presenting and Recurrent Infantile Blount Disease. J. Pediatr. Orthop. 2021, 41, 67–76. [Google Scholar] [CrossRef]
- Nada, A.A.; Hammad, M.E.; Eltanahy, A.F.; Gazar, A.A.; Khalifa, A.M.; El-Sayed, M.H. Acute Correction and Plate Fixation for the Management of Severe Infantile Blount’s Disease: Short-Term Results. Strateg. Trauma Limb Reconstr. 2021, 16, 78–85. [Google Scholar] [CrossRef]
- Ogbemudia, A.O.; Bafor, A.; Ogbemudia, P.E. Anterior Posterior Inverted-‘U’ Osteotomy for Tibia Vara: Technique and Early Results. Arch. Orthop. Trauma Surg. 2011, 131, 437–442. [Google Scholar] [CrossRef]
- Oyemade, G.A. Advanced Tibia Vara (Blount Disease) in Adolescent Nigerians. J. Natl. Med. Assoc. 1981, 73, 339–344. [Google Scholar] [PubMed]
- Pandya, N.K.; Clarke, S.E.; McCarthy, J.J.; Horn, B.D.; Hosalkar, H.S. Correction of Blount’s Disease by a Multi-Axial External Fixation System. J. Child. Orthop. 2009, 3, 291–299. [Google Scholar] [CrossRef]
- Park, S.S.; Gordon, J.E.; Luhmann, S.J.; Dobbs, M.B.; Schoenecker, P.L. Outcome of Hemiepiphyseal Stapling for Late-Onset Tibia Vara. J. Bone Jt. Surg. 2005, 87, 2259–2266. [Google Scholar] [CrossRef]
- Smith, S.L.; Beckish, M.L.; Winters, S.C.; Pugh, L.I.; Bray, E.W. Treatment of Late-Onset Tibia Vara Using Afghan Percutaneous Osteotomy and Orthofix External Fixation. J. Pediatr. Orthop. 2000, 20, 606–610. [Google Scholar] [CrossRef]
- van Greunen, E.; Firth, G.B. Recurrence in Infantile Tibia Vara (Blount Disease) after High Tibia and Fibula Osteotomy. J. Pediatr. Orthop. B 2022, 31, 134–138. [Google Scholar] [CrossRef]
- van Huyssteen, A.L.; Hastings, C.J.; Olesak, M.; Hoffman, E.B. Double-Elevating Osteotomy for Late-Presenting Infantile Blount’s Disease: The Importance of Concomitant Lateral Epiphysiodesis. J. Bone Jt. Surg. Br. 2005, 87, 710–715. [Google Scholar] [CrossRef] [PubMed]
- Westberry, D.E.; Davids, J.R.; Pugh, L.I.; Blackhurst, D. Tibia Vara: Results of Hemiepiphyseodesis. J. Pediatr. Orthop. Part B 2004, 13, 374–378. [Google Scholar] [CrossRef]
- Wilson, N.A.; Scherl, S.A.; Cramer, K.E. Complications of High Tibial Osteotomy with External Fixation in Adolescent Blount’s Disease. Orthopedics 2007, 30, 848–852. [Google Scholar] [CrossRef]
- Zein, A.B.; Elhalawany, A.S.; Ali, M.; Cousins, G.R. Acute Correction of Severe Complex Adolescent Late-Onset Tibia Vara by Minimally Invasive Osteotomy and Simple Circular Fixation: A Case Series with 2-Year Minimum Follow-Up. BMC Musculoskelet. Disord. 2021, 22, 681. [Google Scholar] [CrossRef] [PubMed]
- Gilbody, J.; Thomas, G.; Ho, K. Acute versus Gradual Correction of Idiopathic Tibia Vara in Children: A Systematic Review. J. Pediatr. Orthop. 2009, 29, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Phedy, P.; Siregar, P.U. Osteotomy for Deformities in Blount Disease: A Systematic Review. J. Orthop. 2015, 13, 207–209. [Google Scholar] [CrossRef]
- Burghardt, R.D.; Herzenberg, J.E.; Andre, S.; Bernius, P.; Kazim, M.A. Treatment Failures and Complications in Patients with Blount Disease Treated with Temporary Hemiepiphysiodesis: A Critical Systematic Literature Review. J. Pediatr. Orthop. B 2018, 27, 522–529. [Google Scholar] [CrossRef]
- Banwarie, R.R.; Hollman, F.; Meijs, N.; Arts, J.J.; Vroemen, P.; Moh, P.; Staal, H.M. Insight into the Possible Aetiologies of Blount’s Disease: A Systematic Review of the Literature. J. Pediatr. Orthop. B 2020, 29, 323–336. [Google Scholar] [CrossRef]
- Fan, B.; Zhao, C.; Sabharwal, S. Risk Factors for Failure of Temporary Hemiepiphysiodesis in Blount Disease: A Systematic Review. J. Pediatr. Orthop. B 2020, 29, 65–72. [Google Scholar] [CrossRef]
- Sananta, P.; Santoso, J.; Sugiarto, M.A. Osteotomy Treatments and Post-Operative Fixations for Blount Disease: A Systematic Review. Ann. Med. Surg. 2022, 78, 103784. [Google Scholar] [CrossRef]
- Salenius, P.; Vankka, E. The Development of the Tibiofemoral Angle in Children. J. Bone Jt. Surg. Am. 1975, 57, 259–261. [Google Scholar] [CrossRef]
- Birch, J.G. Blount Disease. J. Am. Acad. Orthop. Surg. 2013, 21, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Chotigavanichaya, C.; Salinas, G.; Green, T.; Moseley, C.F.; Otsuka, N.Y. Recurrence of Varus Deformity After Proximal Tibial Osteotomy in Blount Disease: Long-Term Follow-Up. J. Pediatr. Orthop. 2002, 22, 638–641. [Google Scholar] [CrossRef] [PubMed]
- Lascombes, P.; Popkov, D.; Huber, H.; Haumont, T.; Journeau, P. Classification of Complications after Progressive Long Bone Lengthening: Proposal for a New Classification. Orthop. Traumatol. Surg. Res. 2012, 98, 629–637. [Google Scholar] [CrossRef]
| Paper and Year | Design CEBM | Patients * | Details by Number of Knees | Nation | mCMS | MINORS | Mean FU (Range) | Recurrence | Complications |
|---|---|---|---|---|---|---|---|---|---|
| Alekberov et al. 2003 [15] | CS 4 | 45/45 24 bilateral | 49: metaphyseal tibial osteotomy and GC with Ilizarov 9: metaphyseal tibial osteotomy, acute derotation, and GC with Ilizarov 9: metaphyseal tibial osteotomy and GC with Ilizarov + femoral osteotomy and GC with Ilizarov 2: metaphyseal tibial osteotomy, acute derotation, and GC with Ilizarov + femoral osteotomy and GC with Ilizarov | Russia Turkey | 49 | 10/16 | 6.5 (2.3–14.8) | 9% | 16% |
| Amer and Khanfour 2010 [42] | CS 4 | 20/20 2 bilateral | 22: metaphyseal tibial osteotomy, acute derotation, and GC with Ilizarov | Egypt | 26 | 9/16 | 2.9 (2.0–4.0) | 45% | 0% |
| Andrade and Johnston 2006 [16] | CS 4 | 24/24 3 bilateral | 27: physeal bar resection, metaphyseal tibial osteotomy, and K-wires | USA | 63 | 10/16 | 3.9 (0.8–7.1) | 41% | 4% |
| Assan et al. 2021 [50] | RCS 3b | 17/17 7 bilateral | 14: proximal tibial lateral epiphysiodesis with plate 10: Rab osteotomy and screws | Benin France | 33 | 12/24 | hE 2.0 AC 1.9 | hE 0% AC 60% | 14% |
| Bar-On et al. 2008 [27] | CS 4 | 4/4 | 4: medial plate acute elevation + metaphyseal osteotomy and GC with TSF | Israel | 38 | 7/16 | 2.4 (2.0–3.2) | 0% | 50% |
| Baraka et al. 2021 [43] | CS 4 | 19/19 2 bilateral | 21: medial plate elevation, metaphyseal tibial dome osteotomy, and K-wires + lateral percutaneous epiphysiodesis | Egypt | 62 | 12/16 | 5.1 (3.2–8.3) | 0% | 24% |
| Beck et al. 1987 [38] | CS 4 | 3/3 | 3: physeal bar resection, metaphyseal tibial osteotomy, and pins | USA | 19 | 3/16 | 1.9 (1.1–2.3) | 0% | 0% |
| Blount 1937 [44] | CS 4 | 6/13 1 bilateral | 6: metaphyseal osteotomy and cast 1: medial plate elevation + lateral percutaneous epiphysiodesis and cast | USA | 22 | 6/16 | n.d. | AC 33% AC + hE 0% | n.d. |
| Bushnell et al. 2009 [51] | CS 4 | 53/53 14 bilateral | 45: proximal tibial lateral epiphysiodesis with staples 20: proximal tibial lateral epiphysiodesis with staples + distal femoral lateral epiphysiodesis with staples 2: metaphyseal tibial osteotomy + distal femoral lateral epiphysiodesis with staples | USA | 39 | 6/16 | n.d. | 40% | 4% |
| Castañeda et al. 2008 [52] | CS 4 | 21/48 14 bilateral | 35: lateral proximal tibial epiphysiodesis | USA | 33 | 8/16 | 3.0 | n.d. | 0% |
| Cherkashin et al. 2015 [45] | CS 4 | 31/31 2 bilateral | 33: metaphyseal tibial osteotomy and GC with TSF or Ilizarov, with or without lengthening | USA | 10 | 5/16 | n.d. | 21% | 100% |
| Clarke et al. 2009 [53] | RCS 3b | 38/38 16 bilateral 4 treated twice | 20: metaphyseal tibial osteotomy (and medial plateau elevation if MPDA > 15°) and GC with MAC system + proximal tibial lateral epiphysiodesis 38: metaphyseal tibial osteotomy (and medial plateau elevation if MPDA > 15°) and GC with other external fixators + proximal tibial lateral epiphysiodesis | USA | 50 | 16/24 | 1.9 | 24% | 100% |
| Coogan et al. 1996 [54] | CS 4 | 8/8 4 bilateral | 12: metaphyseal tibial osteotomy and GC with Ilizarov (distal AC of valgus of tibia in some cases) | USA | 54 | 8/16 | 1.9 | 8% | 58% |
| Danino et al. 2020 [55] | RCS 3b | 45/71 10 bilateral | 55: proximal tibial lateral epiphysiodesis | Israel Germany USA Austria Canada | 38 | 10/16 | 2.0 (1.0–4.4) | 27% | 11% |
| Doyle et al. 1996 [56] | CS 4 | 17/17 11 bilateral | 13: single proximal tibial osteotomy 13: two or more surgical procedures for proximal tibial osteotomy 2: proximal tibial lateral epiphysiodesis | USA | 47 | 8/16 | 14.8 (3.2–27.2) | AC 27% hE 50% | AC 12% hE 0% |
| Eamsobhana et al. 2014 [57] | CS 4 | 38/38 27 bilateral | 65: metaphyseal tibial osteotomy | Thailand | 33 | 10/16 | 3.0 | 15% | n.d. |
| Edwards et al. 2017 [46] | CS 4 | 7/7 1 bilateral | 8: medial plate acute elevation + metaphyseal osteotomy and GC with TSF | UK | 42 | 10/16 | 4.6 (2.2–9.0) | 38% | 88% |
| Eidelman et al. 2008 [47] | CS 4 | 8/8 2 bilateral | 10: metaphyseal osteotomy and GC with TSF (no fibular osteotomy) | Israel | 54 | 10/16 | 3.6 | 0% | 100% |
| El Ghafar et al. 2018 [58] | CS 4 | 13/13 7 bilateral | 20: metaphyseal osteotomy, AC, and fixation with Ilizarov | Egypt | 26 | 6/16 | 1.5 | 10% | 40% |
| Fahmy and Fathi 2019 [59] | CS 4 | 13/13 3 bilateral | 16: metaphyseal tibial osteotomy and GC with Ilizarov | Egypt | 51 | 10/16 | 2.0 (1.0–3.0) | 0% | 63% |
| Feldman et al. 2006 [60] | RCS 3b | 32/32 | 14: metaphyseal tibial osteotomy, AC and fixation with external fixator 18: metaphyseal tibial osteotomy and GC with TSF (associated lateral tibial epiphysiodesis in 1 case, not separable) | USA | 65 | 16/24 | 2.0 | AC 43% GC 0% | AC 17% GC 21% |
| Ferriter and Shapiro 1987 [61] | CS 4 | 25/25 12 bilateral | 37: metaphyseal proximal tibial osteotomy (closing wedge, dome, opening wedge), variable types of fixations | USA | 25 | 10/16 | 4.0 (2.0–9.0) | 57% | n.d. |
| Gordon et al. 2005 [62] | CS 4 | 15/15 4 bilateral | 19: metaphyseal tibial osteotomy and GC with Ilizarov | USA | 59 | 10/16 | 5.0 | 0% | 100% |
| Gregosiewicz et al. 1989 [48] | CS 4 | 10/10 3 bilateral | 10: double elevation osteotomy | Poland | 50 | 8/16 | 8.1 (4.0–14.0) | 23% | 38% |
| Hayek et al. 2000 [49] | CS 4 | 9/9 4 bilateral | 13: metaphyseal W osteotomy and AC with K-wires and/or cast | Israel | 77 | 10/16 | 9.0 (2.5–17.0) | 0% | 0% |
| Heflin et al. 2016 [17] | CS 4 | 17/17 10 bilateral | 27: proximal tibial lateral epiphysiodesis | USA | 29 | 8/16 | 2.5 (0.7–5.8) | 15% | 22% |
| Hefny et al. 2010 [18] | CS 4 | 8/8 4 bilateral | 12: double elevation osteotomy combined with GC using Ilizarov frame | Egypt | 35 | 10/16 | 5.0 (3.0–7.0) | 0% | 33% |
| Hollman et al. 2015 [19] | CS 4 | 17/17 8 bilateral | 25: metaphyseal W osteotomy and AC with K-wires and/or cast | Ghana | 37 | 8/16 | Short-term | 0% | 4% |
| Iliadis et al. 1996 [63] | CS 4 | 17/17 6 bilateral | 23: metaphyseal tibial osteotomy proximal to the tibial tubercle and K-wires | Greece | 32 | 6/16 | 4.5 | 17% | 9% |
| Jain et al. 2020 [64] | CS 4 | 40/40 19 bilateral | 61: proximal tibial lateral epiphysiodesis with TBP | USA | 51 | 10/16 | 3.2 (0.7–9.9) | 41% | 8% |
| Janoyer et al. 2007 [20] | CS 4 | 8/8 1 bilateral | 9: medial plate osteotomy and GC with external fixator | France | 59 | 9/16 | 2.0 (1.2–3.8) | 11% | 100% |
| Jones et al. 2003 [21] | CS 4 | 7/7 | 7: (step I) medial plate osteotomy, GC (step II) tibial osteotomy, and GC of residual deformity, rotation and LLD | UK | 59 | 9/16 | 2.4 (1.3–3.7) | 50% | 100% |
| Khanfour and El Rosasy 2014 [22] | CS 4 | 20/20 11 bilateral | 30: metaphyseal osteotomy, AC and fixation with mini-Ilizarov 1: metaphyseal osteotomy and GC with Ilizarov | Egypt | 47 | 11/16 | AC 5.9 (5.0–7.0) GC 7.0 | AC 13% GC 0% | 100% |
| Langenskiöld and Risika 1964 [23] | CS 4 | 59/65 26 bilateral | 85: proximal metaphyseal curved osteotomy and cast | Finland | 44 | 9/16 | 7.3 (0.5–15.8) | 41% | n.d. |
| Laurencin et al. 1996 [24] | CS 4 | 8/11 | 8: lateral closing-wedge metaphyseal osteotomy and plate | USA | 45 | 10/16 | 8.5 (4.0–13.0) | 0% | 13% |
| Liu et al. 2015 [65] | CS 4 | 12/12 5 bilateral | 12: metaphyseal proximal tibia dome osteotomy and AC with K-wires, always with valgizing femoral osteotomy and AC with plate | China | 50 | 8/16 | 9.0 (3.0–16.0) | 8% | 0% |
| Maré et al. 2021 [66] | CS 4 | 48/48 16 bilateral | 50: medial plate elevation, proximal tibial osteotomy, screw fixation, and lateral tibial epiphysiodesis 14: medial plate elevation osteotomy, screw fixation, and lateral tibial epiphysiodesis | South Africa | 40 | 9/16 | 3.2 (1.0–6.2) | 19% | 13% |
| Maré et al. 2022 [25] | CS 4 | 14/14 4 bilateral | 18: proximal tibial lateral epiphysiodesis with TBP | South Africa | 34 | 6/16 | 2.7 (1.4–5.2) | 22% | 33% |
| Martin et al. 1994 [26] | CS 4 | 7/9 4 bilateral | 9: metaphyseal proximal tibial osteotomy and plate fixation 2: metaphyseal proximal tibial osteotomy, proximal lateral tibial epiphysiodesis, and plate fixation | USA | 40 | 5/16 | n.d. | AC 11% AC + hE 100% | AC 0% AC + hE 100% |
| Medbö 1964 [28] | CS 4 | 17/17 12 bilateral | 29: proximal tibial osteotomy, Blount staple fixation, and cast | Norway | 29 | 9/16 | 9.8 (1.0–17.0) | 59% | 24% |
| Miraj et al. 2019 [29] | CS 4 | 17/17 10 bilateral | 27: metaphyseal proximal tibial step-cut V osteotomy and LCP plate fixation | Indonesia | 39 | 7/16 | 1.0 | 15% | 0% |
| Mousa 2014 [30] | CS 4 | 9/9 5 bilateral | 14: metaphyseal proximal tibial Chevron osteotomy, wedge transfer, and plate | Egypt | 54 | 9/16 | 1.0 | 7% | 7% |
| Nada et al. 2021 [67] | CS 4 | 11/11 | 11: medial plate elevation, closing-wedge osteotomy and plate fixation | Egypt | 70 | 10/16 | 2.2 (1.5–3.0) | n.d. | 18% |
| Ogbemudia et al. 2011 [68] | CS 4 | 31/31 16 bilateral | 47: anteroposterior inverted ‘U’ metaphyseal tibial osteotomy and cast | Nigeria | 67 | 12/16 | 3.2 | n.d. | n.d. |
| Oto et al. 2012 [31] | CS 4 | 5/5 1 bilateral | 6: lateral proximal tibial epiphysiodesis with TBP | Turkey | 59 | 12/16 | 2.0 (1.1–2.6) | 100% | 0% |
| Oyemade 1981 [69] | CS 4 | 25/25 15 bilateral | 40: metaphyseal proximal tibial wedge osteotomy and cast | Nigeria | 28 | 4/16 | n.d. | 10% | 15% |
| Pandya et al. 2009 [70] | CS 4 | 17/17 1 bilateral | 18: proximal tibial osteotomy and GC with MAC system | USA | 62 | 10/16 | 1.7 | 17% | 50% |
| Park et al. 2005 [71] | CS 4 | 26/26 7 bilateral | 33: lateral proximal tibial epiphysiodesis with stapling | USA | 51 | 10/16 | 3.7 (2.0–6.8) | 33% | 18% |
| Price et al. 1995 [32] | CS 4 | 25/25 9 bilateral | 26: metaphyseal proximal tibial osteotomy, AC, and fixation with monoaxial fixator 4: metaphyseal proximal tibial osteotomy, AC of varus, and GC of LLD with monoaxial fixator 4: GC with hemichondrodiastasis with external fixator | USA | 33 | 9/16 | n.d. | AC 15% GC 0% hChD 75% | AC 19% GC 25% hChD 100% |
| Rab 1988 [33] | CS 4 | 6/6 1 bilateral | 7: Rab osteotomy of proximal tibia and fixation with screws | USA | 46 | 9/16 | 1.3 (0.8–2.0) | 14% | 29% |
| Sachs et al. 2015 [34] | CS 4 | 22/23 2 bilateral | 24: metaphyseal osteotomy and gradual tibial lengthening with TSF | Israel | 48 | 8/16 | n.d. | 0% | 42% |
| Schoenecker et al. 1992 [35] | CS 4 | 7/7 | 3: (stage A) medial plateau elevation, graft, and fixation with pinning or plate (no fixation in 1 patient) + (stage B) metaphyseal proximal tibial osteotomy 3: stage B and, after 7 to 15 months, stage A 1: stage A and, after 7 months, stage B | USA | 54 | 8/16 | 3.2 (2.0–6.0) | 14% | 14% |
| Scott 2012 [36] | CS 4 | 12/12 6 bilateral | 18: lateral proximal tibial epiphysiodesis with TBP | USA | 44 | 9/16 | 1.6 (0.1–3.1) | 11% | 28% |
| Smith et al. 2000 [72] | CS 4 | 19/19 4 bilateral | 23: metaphyseal proximal tibial osteotomy, AC, and fixation with monoaxial external fixator | USA | 49 | 8/16 | 2.7 (0.5–7.1) | 17% | 35% |
| Stanitski et al. 1998 [37] | CS 4 | 10/14 | 10: metaphyseal proximal tibial osteotomy and GC with T-Garches fixator | USA | 46 | 8/16 | 1.4 (0.8–2.6) | 20% | 40% |
| Tavares and Molinero 2006 [39] | CS 4 | 4/5 | 4: (stage A) medial plate elevation with graft and lateral tibial epiphysiodesis with staples or percutaneous drilling; (stage B) after 3 months, metaphyseal osteotomy and GC with Ilizarov, TSF, or monoaxial fixator | USA | 49 | 10/16 | 3.3 (3.0–4.0) | 0% | 0% |
| Tsibidakis et al. 2018 [40] | CS 4 | 16/16 8 bilateral | 24: metaphyseal proximal tibial osteotomy and GC with TSF | Italy Greece Bulgaria | 42 | 10/16 | 3.8 (3.0–6.0) | 13% | 25% |
| Van Greunen and Firth 2022 [73] | CS 4 | 44/44 16 bilateral | 60: metaphyseal proximal tibial osteotomy and fixation with K-wires | South Africa | 33 | 8/16 | 2.3 (1.0–6.2) | 63% | n.d. |
| van Huyssteen et al. 2004 [74] | CS 4 | 24/24 10 bilateral | 34: elevating osteotomy, and the remaining tibial varus and internal torsion with an osteotomy just below the apophysis and proximal lateral tibial epiphysiodesis (19 concomitant epiphysiodesis, 15 of them 3 and 12 months after the osteotomy) | South Africa | 59 | 10/16 | 2.8 | 3% | 9% |
| Wenger et al. 1984 [41] | CS 4 | 6/7 2 bilateral | 8: corrective osteotomy below growth plate | USA | 26 | 4/16 | 1.0 | 0% | n.d. |
| Westberry et al. 2004 [75] | CS 4 | 23/23 10 bilateral | 21: proximal lateral tibial stapling only 9: proximal lateral drill hemiepiphysiodesis 3: simultaneous proximal lateral tibial stapling and distal lateral femoral stapling | USA | 47 | 6/16 | 3.1 | 27% | 30% |
| Wilson et al. 2007 [76] | CS 4 | 29/29 9 bilateral | 38: high tibial osteotomy, AC, and fixation with Ilizarov | USA | 39 | 6/16 | 2.0 | 18% | 100% |
| Zein et al. 2021 [77] | CS 4 | 30/30 2 bilateral | 32: AC with minimally invasive osteotomy and simple circular fixation | Egypt | 43 | 10/16 | 2.1 (2.8–3.8) | 0% | 34% |
| Group | Knees (N) | Recurrence (Mean % and C.I. 95%) | I2 | Minor Complications (Mean % and C.I. 95%) | I2 | Major Complications (Mean % and C.I. 95%) | I2 |
|---|---|---|---|---|---|---|---|
| GC | 306 (18%) | 7% (1–15%) | 0.27 | 49% (34–64%) | 0.57 | 2% (0–9%) | 0.33 |
| GC + hE | 76 (5%) | 15% (0–40%) | 1 | 74% (37–99%) | 0.55 | 16% (1–41%) | 1 |
| AC | 788 (47%) | 22% (15–29%) | 0.34 | 14% (7–22%) | 0.54 | 6% (2–12%) | 0.01 |
| AC + hE | 129 (8%) | 5% (2–20%) | 0.22 | 0% (0–8%) | 0.12 | 4% (2–17%) | 1 |
| hE | 369 (22%) | 29% (19–40%) | 0.11 | 1% (1–6%) | 0.42 | 4% (0–10%) | 0.01 |
| hChD | 4 (0.2%) | 75% (-) | - | 100% (-) | - | 0% (-) | - |
| Total | 1672 | 18% (14–22%) * | 0.22 * | 18% (12–24%) ** | 0.60 ** | 5% (2–8%) ** | 0.01 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramella, M.; Depaoli, A.; Menozzi, G.C.; Gallone, G.; Cerasoli, T.; Rocca, G.; Trisolino, G. Recurrence and Complication Rates of Surgical Treatment for Blount’s Disease in Children: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 6495. https://doi.org/10.3390/jcm12206495
Ramella M, Depaoli A, Menozzi GC, Gallone G, Cerasoli T, Rocca G, Trisolino G. Recurrence and Complication Rates of Surgical Treatment for Blount’s Disease in Children: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(20):6495. https://doi.org/10.3390/jcm12206495
Chicago/Turabian StyleRamella, Marco, Alessandro Depaoli, Grazia Chiara Menozzi, Giovanni Gallone, Tosca Cerasoli, Gino Rocca, and Giovanni Trisolino. 2023. "Recurrence and Complication Rates of Surgical Treatment for Blount’s Disease in Children: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 20: 6495. https://doi.org/10.3390/jcm12206495
APA StyleRamella, M., Depaoli, A., Menozzi, G. C., Gallone, G., Cerasoli, T., Rocca, G., & Trisolino, G. (2023). Recurrence and Complication Rates of Surgical Treatment for Blount’s Disease in Children: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(20), 6495. https://doi.org/10.3390/jcm12206495






