Abstract
Many patients, particularly those aged above 40, experience knee joint pain, which hampers both sports activities and daily living. Treating isolated chondral and osteochondral defects in the knee poses a significant clinical challenge, particularly in younger patients who are not typically recommended partial or total knee arthroplasty as alternatives. Several surgical approaches have been developed to address focal cartilage defects. The treatment strategies are characterized as palliation (e.g., chondroplasty and debridement), repair (e.g., drilling and microfracture), or restoration (e.g., autologous chondrocyte implantation, osteochondral autograft, and osteochondral allograft). This review offers an overview of the commonly employed clinical methods for treating articular cartilage defects, with a specific focus on the clinical trials conducted in the last decade. Our study reveals that, currently, no single technology fully meets the essential requirements for effective cartilage healing while remaining easily applicable during surgical procedures. Nevertheless, numerous methods are available, and the choice of treatment should consider factors such as the location and size of the cartilage lesion, patient preferences, and whether it is chondral or osteochondral in nature. Promising directions for the future include tissue engineering, stem cell therapies, and the development of pre-formed scaffolds from hyaline cartilage, offering hope for improved outcomes.
1. Introduction
The knee joint, due to its location and complex function, is very susceptible to damage. Many patients, especially those over 40 years of age and sports patients after traumatic injuries, complain of painful symptoms in this joint, most commonly located in the medial compartment and the patellofemoral joint. These symptoms are caused by changes in the structure of the articular cartilage [1]. Articular cartilage is a highly differentiated and specialized connective tissue [2]. The extracellular matrix is mainly composed of water, collagen, and proteoglycans, as well as a small amount of non-collagenous proteins. Type II collagen is the most common form and represents about 90–95% of collagen in the extracellular matrix [3]. Articular cartilage is avascular and aneural, and lacks lymphatic vessels, resulting in a poor potential for healing. Damaged surfaces rubbing against each other accelerate the processes of the softening and cracking of the cartilage [4,5]. With progressive destruction of the cartilage, joint deformity occurs, leading to secondary damage to other structures, such as the menisci. Fragments of damaged menisci accelerate cartilage destruction and worsen pain [6]. The incidence of cartilage injuries is confirmed in over 60% of knee arthroscopies performed [7].
Articular cartilage lesions have poor repair capacity, leading to progressive joint damage, and cannot be predictably restored by conservative treatment, physical therapy, or injectable regimens.
Various methods are used to prevent the progression of cartilage lesions. One of them is orthotic treatment, which can correct existing deformities. Such treatment includes knee joint stabilizers, corrective insoles for shoes, special orthopedic shoes, and elbow crutches [8]. However, such treatment methods are not accepted for a long time, especially by young people. Another treatment method is the use of glycosaminoglycans. These substances are widely used in the treatment of cartilage injuries, but the results of therapy are highly variable [9]. Intra-articular injections of hyaluronic acid and platelet-rich plasma (PRP) can promote the healing of cartilage injuries and improve the lubricating properties of the joint [10]. However, these solutions have their limitations in cases of large cartilage defects and significant angular deformities of the knee joint [11]. In such situations, minimally invasive techniques based on the stimulation of bone marrow cells or the use of osteochondral grafts should be considered. These techniques are demanding, but failure to treat cartilage defects leads to the development of generalized cartilage lesions in the joint and ultimately ends in total joint replacement [12].
The aim of this review was to characterize the most commonly used minimally invasive surgical procedures to treat articular cartilage defects, based on evidence from clinical trials from the last decade.
Scopus, PubMed, Web of Science, and Google Scholar were utilized to identify papers related to the study’s objectives. The following keywords were used to search databases: “articular cartilage” OR “knee” OR “mesenchymal stem cells” OR “autologous chondrocyte implantation” OR “osteochondral defect” OR “microfracture” OR “mosaicplasty” OR “osteochondral autograft transfer” AND “repair techniques” OR “regenerative medicine”. The search period covered the period 2014 to 2023 and included searches in titles, abstracts, and keywords. All retrieved articles were reviewed based on inclusion criteria, which included full-text availability and English language. Excluded from the review were conference papers, reviews, abstract-only articles, books, and animal studies.
2. Surgical Strategies for the Treatment of Cartilage Defects
In clinical practice, various treatment options are available for addressing cartilage defects. However, surgical intervention should be specifically considered for symptomatic cartilage lesions graded as 3 or 4 according to the International Cartilage Repair Society (ICRS) classification [13]. Grade 3 lesions are characterized by defects exceeding 50% of the cartilage depth without extending into the subchondral bone, while grade 4 lesions involve both the cartilage and the underlying subchondral bone. These criteria are outlined in Table 1.

Table 1.
Classification of knee cartilage defects according to ICRS (International Cartilage Repair Society Classification).
Treatment options for chondral lesions involve either marrow-stimulating techniques or cell-regenerating approaches. Osteochondral lesions, on the other hand, can be addressed through bone graft and chondrocyte implantation, mosaicplasty, or allografts. It states that the choice of surgical procedure depends on factors such as the location and size of the cartilage lesion, patient demands, and whether it is chondral or osteochondral in nature. The size of the lesion is typically determined post debridement, and it is measured by area (cm2) (width × length of lesions). The location and size of the defect are preoperatively estimated using MRI and definitively assessed during arthroscopy. Traditionally, defects larger than 8 cm2 are not considered suitable for regenerative surgery. The scheme of approach for the treatment of cartilage defects is shown in Figure 1.
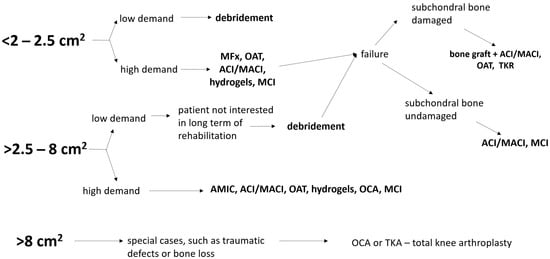
Figure 1.
Approaches for the treatment of cartilage defects. MFx—microfracture, OAT—osteochondral autograft transfer, ACI—autologous chondrocyte implantation, TKA—total knee arthroplasty, OCA—osteochondral allografts, MCI—minced cartilage implantation, MACI—matrix-assisted chondrocyte implantation, AMIC—autologous matrix-induced chondrogenesis.
The knee joint consists of two articulations: the patellofemoral and tibiofemoral joints. They differ from each other in terms of shape, biomechanics, and the pressure generated during movement. The treatment of cartilage defects in these joints is similar, but the postoperative management varies. Rehabilitation after surgery should consider the anatomical differences of both joints, with particular attention to the location and extent of the injury, as well as the surgical technique used.
The cartilage lesions lead to focal degeneration, however, a disturbed joint homeostasis after, for example, trauma, may induce a generalized loss of cartilage, leading to end-stage osteoarthritis, encompassing the entire joint. Interestingly, isolated articular cartilage defects seem to be associated with general knee osteoarthritis severity [14]. In recent years, regenerative medicine has been applied to patients who have clinically evident but not end-stage osteoarthritis. It seems that new regenerative technologies can work better for focal lesions when the overall joint damage is minimal [15].
2.1. Microfracture, Drilling, and Abrasion
Techniques stimulating bone marrow cells are widely used in the arthroscopic treatment of cartilage and osteochondral defects. Among them, microfracture, drilling, or abrasion of the subchondral layer should be mentioned. The aim of these therapies is to induce the extravasation of bone marrow rich in stromal cells and the secondary formation of a fibrin clot, which will be the basis for creating hyaline cartilage in the defect site [16]. However, bone marrow cells may differentiate into fibrochondrocytes, resulting in the formation of fibrous cartilage, sometimes with elements of fibrocartilage. Fibrous cartilage is mainly composed of type I collagen and has weaker biochemical and biomechanical properties than hyaline cartilage [17].
Microfracture (MFx) used in the treatment of cartilage defects is often considered the gold standard of therapy. The first results and description of the microfracture technique were published by Steadman in 1994 [18]. The idea of the method is to support the natural process of healing the cartilage defect by releasing bone marrow stromal cells. Initially, microfracture was performed in patients with full-thickness cartilage defects resulting from knee joint injuries. The indication for the use of this treatment method was also unstable damage to the cartilage covering the subchondral layer, as well as cartilage lesions in the knee joint with preserved anatomical mechanical axis [19]. The microfracture technique is the simplest and cheapest method of treating osteochondral defects and is used as a first-line procedure in the treatment of such injuries [20]. It involves creating 4 mm-deep holes throughout the surface of the cartilage defect, which are 3–4 mm apart from each other [21]. Special tools are used to perform the microfracture, which can be used in both open and arthroscopic techniques. The defect should be cleaned of any remaining damaged cartilage to expose the subchondral layer and obtain a stable environment for the defect through healthy, undamaged cartilage. Such preparation of the defect provides stability for the developing clot, which contains bone marrow cells [22].
Subchondral drilling or abrasion is an alternative method to microfracture and involves drilling the damaged surface with a special drill or thin Kirschner wire [23]. Subchondral abrasion requires the use of a drill bit, which allows for the removal of the damaged cartilage tissue and partially removes the subchondral bone layer. This technique is less commonly used than microfracture because it can cause thermal damage to osteocytes, as well as excessive damage to the subchondral layer, resulting in necrosis, hypertrophy, or the development of intraosseous cysts [21]. However, animal studies have shown that drilling does not destroy more osteocytes than microfracture [24].
Nanofracture is a variation of microfracture that differs from the primary technique in terms of the smaller size of the hole, of up to 1 mm, and deeper penetration, of up to 9 mm. The advantage of this method is the possibility of a denser distribution of microfracture and less damage to the subchondral layer at the site of the defect. Additionally, osteocytes are not thermally damaged during the procedure. Animal studies confirm less destruction of trabecular bone in the case of nanofracture, as well as less crushing and fragmentation of the subchondral layer. Moreover, better healing and anatomical reconstruction of trabecular bone and less frequent formation of subchondral cysts are observed [25].
On the other hand, deeper subchondral penetration results in more effective filling of the defect by the extravasated blood and proportionally more frequent development of fibrocartilage at the site of injury [26].
Over the years, various microfracture techniques have been thoroughly investigated. Many studies have confirmed an improvement in clinical outcomes in early postoperative observations [27]. However, the relatively common development of fibrous cartilage and worsening of results in long-term observations should encourage considerations of alternative surgical techniques, including autologous chondrocyte implantation and osteochondral cylinder transfers. [28].
An alternative to these techniques includes the augmentation of microfractures with biological agents. For example, microfracture augmented with particulated costal allocartilage resulted in superior cartilage repair quality compared with microfracture alone at short-term follow-up [29]. In general, biological augmentation resulted in significant improvements in patient-reported outcome measures [30,31,32]. However, in all the trials, this improvement did not reach the minimally clinically important difference, meaning that it was not perceivable by the patients. Moreover, the overall low evidence and the paucity of high-level studies indicate further research is needed to confirm the potential of PRP augmentation to microfracture for the treatment of cartilage lesions [33].
In summary, many studies have confirmed that microfracture brings better clinical results in the treatment of smaller defects involving an area of 2–4 cm2 and in younger patients [34].
2.2. Autologous Matrix-Induced Chondrogenesis
A fibrous clot formed as a result of microfracture does not have proper mechanical stability and is not able to withstand the shearing forces that occur during joint movements [35]. To prevent damage to the clot formed after microfracture, the autologous matrix-induced chondrogenesis (AMIC) technique is used. This technique combines microfracture with a collagen patch covering the defect, which provides mechanical stability to the clot and allows stromal cells to differentiate into chondrocytes. To seal the defect, the collagen patch is stabilized with cartilage using tissue adhesives or sutures. Randomized clinical trials comparing microfracture with AMIC showed that the tissue produced was quantitatively and qualitatively better in 5-year observations in the AMIC group. However, no clear differences in clinical outcomes were observed [36]. The best results with this method are obtained when it is used in defects of up to 12 cm2.
2.3. Techniques Based on Chodrocyte Implantation
In 1970, Bentley and Greer conducted animal studies in which they implanted chondrocytes into cartilage defects with the aim of restoring hyaline cartilage [37]. This method, known as autologous chondrocyte implantation (ACI), was developed in the 1990s by Brittberg et al. and is divided into two stages [38]. The first stage involves harvesting articular cartilage from an unburdened area of the joint. Chondrocytes are released from the cartilage under enzymatic digestion in laboratory conditions. Then, they are multiplied for a period of 4 to 6 weeks. The second stage involves implanting the multiplied chondrocytes into the cartilage defect. In the original method, chondrocytes were delivered under a periosteal patch, which was sutured to the surrounding cartilage and additionally reinforced with fibrin glue. A characteristic feature of this method was periosteal overgrowth, which resulted in painful popping observed in about 25% of patients [39]. Currently, periosteal patches have been replaced by various types of collagen patches.
MACI—Matrix-Assisted Chondrocyte Implantation is a second-generation technique that uses scaffolds made from a mixture of collagen types I and III. Chondrocytes are grown on these scaffolds, which are then implanted at the site of the defect and stabilized with tissue glue [40]. This technique shortens the surgery time and avoids the complications that were associated with the use of periosteal membrane patches. The next stage in treatment will involve using chondrocyte cultures in the form of small spheres, called chondrospheres [41].
In both ACI and MACI methods, the rebuilt cartilage has a hyaline or hyaline-like structure in histological studies. In 5-year observations, the graft survival rate oscillates around 78%, while in 10-year observations, it is 51%. The improvement in functional results is comparable to mosaicplasty [42,43]. This is confirmed, among others, by studies by Minas and colleagues, who presented a graft survival rate of 71% in 10-year observations and an improvement in function in 75% of cases in patients with defects of an average size of 8.4 cm2. ACI/MACI has been approved and recommended by the National Institute for Health and Care Excellence (NICE) in the UK as a first-line treatment for cartilage defects. ACI/MACI is recommended for large cartilage defects with a surface area of up to 22 cm2 [44]. Despite its many advantages, this method also has some drawbacks, including the need for two surgical procedures, a long rehabilitation time after surgery, and high surgical costs.
The classic ACI technique has been modified in recent years, and three-dimensional matrix-based procedures (e.g., spheroids) have been developed. Spheroids are a type of three-dimensional cell aggregate, self-assembling under conditions that prevent attachment to a flat surface [45]. Once formed into a self-adhesive matrix, the spheroids (marketed under the name Spherox by CO.DON AG) are implanted into the defect, and the chondrocytes migrate and synthesize extracellular matrix components, thus filling the lesion [46]. There are promising mid- to long-term results of this technique [47,48]; the histological and immunohistological outcomes are excellent at 6 to 16 months after the surgery, showing the regeneration of hyaline articular cartilage [49]. However, there still remain questions regarding the optimal cultivation time [50] and dosage [51], and operating surgeons should be aware of the frequent adverse reactions, including joint effusion, arthralgia, and joint swelling [52].
Another approach to cartilage regeneration utilizes rapidly isolated recycled autologous chondrons (chondrocytes with pericellular matrix [53,54]) with allogeneic MSCs in a one-stage surgery. So far, animal test results have been very promising [55]. There was a single, proof-of-concept, first-in-human study by Saris et al. [56]. In the study, no signs of a foreign body response or serious adverse reactions were recorded after 5 years in 35 of the study group patients. The majority of patients showed statistically significant and clinically relevant improvements in the KOOS and all of its subscales from baseline to 60 months. The authors concluded that these data support MSC-augmented chondron transplantation (coined IMPACT) as a safe one-stage surgical intervention. However, one should await the results of the larger-scale human trial, for which a study protocol was published in 2020 [57].
2.4. Hydrogels Treatment
Another method used in the treatment of cartilage defects is hydrogels. It is one of the more modern techniques that can be used in both open and arthroscopic methods. Hydrogels have different characteristics regarding reabsorption time. When this time is fast, the migration of stromal cells may not be sufficient to restore the correct structure of the cartilage defect, while in the case of too slow bioabsorption, chondrocyte overgrowth may cause irregularities on the surface of the joint cartilage. Due to these limitations, the use of gels is currently combined with the microfracture technique, which improves the quality of the resulting cartilage tissue. Hydrogels are characterized by good lubricating properties as well as biomechanical characteristics that allow stromal cells to mature. The efficiency of gels depends on their mechanical strength and modular elasticity. The first gels did not have sufficient compressive strength and load-carrying capacity, which appeared during the normal functioning of the knee joint and did not fulfill their stabilizing role for mesenchymal cells. Currently, improved gel preparations have very good mechanical properties. Shive et al. evaluated the early and 5-year results of gel use compared to microfracture. They obtained significantly better MRI image results in the group using the gel for filling and healing the cartilage defect, while in 5-year observations, the WOMAC scale results were comparable in terms of pain, stiffness, and function [36].
2.5. Osteochondral Autograft Transfer Mosaicplasty
Osteochondral autograft transfer (OAT) mosaicplasty is a surgical technique in which cartilage-bone cylinders are taken from non-weight-bearing zones of the joint and are simultaneously transplanted and implanted in the area of the cartilage defect after its preparation. The bone portion of the autograft provides an excellent foundation and stability for the cartilaginous portion above it. In the procedure, one or several cylinders can be used to fully fill the cartilage defect. However, this technique is more time-consuming than microfracture and requires the use of special tools. The bone fragment of the graft usually fully fuses with the surrounding bone, while the cartilage fragment does not always undergo biointegration with the surrounding cartilage. Gaps appear between the cartilage-bone cylinders, which are filled with fibrous tissue that transforms into fibrocartilaginous tissue. This also does not achieve homogenous uniformity in the filled defect. The disadvantage of mosaicplasty is the potential mismatch of the size and shape of the graft compared to the filled defect [58]. Despite its drawbacks, this technique has significantly better long-term outcomes than microfracture. Opinion papers that used mosaicplasty showed very good results, with a survival rate of 72% in observations over 10 years [59]. However, the older age of patients, previous surgeries, and larger cartilage defects ultimately affect worse long-term outcomes [60]. These findings are confirmed by Bentley’s studies, which found mosaicplasty to be less effective than ACI in large cartilage defects. However, mosaicplasty has significantly better outcomes in smaller defects compared to ACI [61].
2.6. Fresh Osteochondral Allografts
Fresh osteochondral allografts (OCA) are an alternative to OATS. They can be used in cases where the primary treatment of cartilage defects with other methods has failed [62]. The advantage of this method is that it avoids harvesting material from non-weight-bearing areas and allows for coverage of large surface areas that would not be possible with autologous grafts under normal conditions. The value of this method has been confirmed in numerous studies for the treatment of both local and extensive injuries in demanding patients [63,64]. The survival rate of grafts in this method has been reported to be up to 82% in 10-year follow-up observations and 74% in 15-year follow-up observations [65]. The correct storage of fresh osteochondral allografts at physiological body temperature is crucial for the ultimate treatment outcome, as it significantly affects the survival of chondrocytes [20]. The main problem with this technique is the possible rejection reaction of the graft by the recipient. Additionally, thin grafts of less than 1 cm or smaller may not heal, and the cartilage may not consolidate with the graft. Another problem with the use of fresh osteochondral allografts may be their availability [66].
2.7. Stromal Cells
Mesenchymal stromal cells (MSCs) are unspecialized, primary cells with a high potential for proliferation and transformation into specialized cells. Depending on their origin, stromal cells can be divided into embryonic stromal cells and adult stromal cells. Until now, stromal cells have been administered through intra-articular injections to slow down the degenerative process of the joint. Currently, stromal cells are being explored to be combined with other types of therapies for the potential development of hyaline cartilage regeneration. The administration of stromal cells is used either during the filling of a cartilage defect at the site of the lesion or delivered into the joint as a means to enhance tissue healing. The use of bone marrow stromal cells to repair cartilage defects can be performed as a one-step procedure, which makes it significantly cheaper than ACI/MACI techniques [67]. The injection of stromal cells into the joint for the treatment of cartilage defects has not been fully confirmed, but reports appear in the literature indicating the beneficial effects of such therapy in cartilage lesions and aseptic necrosis of the bone.
A review of the literature confirms that intra-articular injections of stromal cells derived from adipose tissue improve clinical scores, magnetic resonance imaging, arthroscopic evaluation, and histological evaluation of cartilage material obtained after stem cell treatment [68]. Additionally, better results have been obtained in studies comparing the effectiveness of stromal cells to hyaluronic acid [69]. Sekiya et al. combined stromal cells taken from the synovial membrane with patient serum and administered them under arthroscopic control to the sites of cartilage defects, observing improvements in clinical outcomes and MRI images [70]. So far, few studies have been published on the combination of stromal cells with scaffolds as a simultaneous procedure. Most published studies so far have been patient series. Buda et al. transplanted stromal cells in combination with a hyaluronic acid membrane in cartilage defects of the medial and lateral femoral condyles in 20 patients. Researchers observed a significant improvement in clinical symptoms in 2-year observations [71].
Nejadnik et al. compared a group of patients who underwent ACI with a group of patients treated with stromal cells. Overall, the treatment outcomes in both groups were comparable and indicated an improvement in the quality of life of patients, as well as significantly improving the physical activity of the subjects [72]. However, the use of stromal cells in combination with collagen membranes still requires randomized, multicenter clinical trials to be conducted.
2.8. Autologous Cartilage Repair Technique
Minced cartilage implantation (MCI) is another promising cartilage reconstruction technique. It consists of transplanting autologous cartilage fragments in a single-step procedure. First, cartilage from the lesion, less weight-bearing areas, or both are harvested, optimally preserving the uniform fragment size without crushing the fragments. Simultaneously, autologous thrombin and platelet-rich plasma (PRP) solutions are prepared. After the defect is cleaned and dried, cartilage fragments and PRP are introduced and stabilized in situ with autologous fibrin glue, membrane, or staples [73]. Since adult human cartilage cells are postmitotic, they cannot fill the cartilage defects [74]. However, the fragmentation of healthy cartilage is meant to activate mitogenic activity, and following implantation, an outgrowth of autologous chondrocytes is initiated. The outgrowth of chondrocytes from minced pieces results in proliferation, which is hoped to promote the extracellular matrix (ECM) production of naive articular cartilage tissue [75].
In animal models, minced cartilage has shown results superior to membranes and microfracture, similar to ACI [76]. In addition, chondrocyte outgrowth from chondral fragments has been proven feasible in vivo, further suggesting the viability of this technique [77].
There is only limited clinical evidence on autologous minced cartilage procedures in humans [78,79]. While the published studies have shown satisfying clinical outcomes and safety, with failure and revision rates comparable to other available cartilage repair techniques, more comparative trials are necessary to allow comparison with alternative cartilage repair techniques. Autologous minced cartilage repair does not require manipulating the specimen in the laboratory or using allografts. It is, therefore, economically attractive and should not require significant regulations. In summary, minced cartilage has a strong biologic potential since autologous, activated, non-dedifferentiated chondrocytes are utilized. Thus, one avoids the problems of the dedifferentiation of chondrocytes, which produces weak type I collagen, not primarily associated with healthy cartilage, while maintaining adequate cellularity required for matrix generation. Preliminary data show that it can be used for small and large cartilage and osteochondral lesions. However, comparative study and long-term outcomes data are required to the determine minced cartilage construct’s effectiveness and durability.
2.9. Scaffold-Based Therapies
Scaffold-based therapies emerged as another potential solution for chondral and osteochondral lesions. Primarily, scaffolds were implanted with autologous chondrocytes, replacing the periosteal patch to contain the cell culture, and later as matrix-assisted ACI, serving as a culturing medium [80,81,82]. However, cell-based therapies involved regulatory restrictions, higher costs, and required an additional surgical procedure for cell harvest and time for cell expansion; cell-free scaffolds were thus introduced. The cell-free approach was meant to allow native cells to populate the scaffold over time [83]. Along with increasing the body of evidence, two approaches have recently dominated clinical practice—a trend for a single-step procedure with various cell sources and the use of biomaterials as a stand-alone, cell-free therapy [81,84]. The latter approach also marks clinicians’ increasing understanding that scaffolds could not only serve as a matrix for transplanted cells, but can also display intrinsic properties supporting tissue regeneration, promoting chondral and osteochondral regrowth [84].
A variety of scaffolds have been introduced to clinical practice and there are human studies showing good mid- to long-term results, regardless of the scaffold form (fibers, gels, meshes) and cell content (cell-free or including autologous chondrocytes) [85,86]. Importantly, both clinical outcomes and the return to sports rates for scaffold-based techniques are similar to other repair techniques; for example, ‘kissing lesions’ are connected with inferior results for this technique too [82,87,88]. This finding, present in many studies on cartilage repair, signifies the influence of both biomechanics as well as the overall joint status (arthritic vs. non-arthritic) on the outcomes of different cartilage restoration procedures.
3. Novel Techniques
Novel techniques are being introduced into clinical trials to improve the clinical outcomes of cartilage lesion treatment. Articular chondrocyte-based autologous chondrocyte implantations have been shown to restore articular cartilage defects. However, there is a significant donor-site morbidity associated with this technique, which increases the likelihood of developing osteoarthritis [89,90], and the available volume of chondral tissue is limited. Therefore, alternative cell sources for cartilage repair have been introduced, including nasal, auricular, and costal cartilage [91,92]. The trials performed in humans suggest that these innovative techniques can become an established therapeutic option, while overcoming the limitations of classical ACI procedures. Short- to mid-term results have been promising, with good clinical outcomes and confirmed structural regeneration [92,93]. The evolution of these techniques could also involve 3D bioprinting in the future [94].
In the last decade, numerous scientific reports have been dedicated to describing the clinical observation of the effects of therapy using different approaches (Table 2). Furthermore, some papers have compared the effectiveness of various treatments for knee cartilage defects. Some examples of the observed effects of therapy are presented in Table 3.

Table 2.
Examples of the application of different surgical strategies in the treatment of knee cartilage defects.

Table 3.
Comparison of clinical outcomes for different surgical approaches in the treatment of knee cartilage defects.
4. Conclusions
In summary, this article outlines the current treatment options for articular cartilage injuries, as well as their indications, advantages, and limitations. Furthermore, it explores future prospects in cartilage regeneration techniques. The dynamic advancements in science and biotechnology provide the groundwork for creating superior materials for knee joint cartilage defect treatments. Tissue engineering takes the lead, aiming to develop tissues that mimic the biological, structural, and functional characteristics of hyaline cartilage, with better integration into the surrounding tissue. Consequently, this could enhance the longevity of implants in the mechanically demanding knee joint environment.
Stem cell therapies hold great promise as readily available and biologically compatible materials. Promising advances in gene therapies and the development of pre-formed scaffolds from hyaline cartilage offer hope for the future. Overall, there is currently no technology that fully meets the essential requirements for effective cartilage healing, which include proper extracellular matrix organization and bioactivity, and can be easily applied by surgeons during surgical procedures. However, the latest techniques, although not yet widely available in clinical practice, provide hope for the future.
Author Contributions
Conceptualization, J.J.; methodology, J.J. and T.B.; investigation, J.J., M.K.W., W.W., A.T.-W., M.W. and I.S.; writing—original draft preparation, J.J., M.K.W., W.W., A.T.-W., M.W. and I.S.; writing—review and editing, J.J., M.W., I.S. and T.B.; supervision, J.J.; project administration, J.J.; funding acquisition, T.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Farrokhi, S.; Chen, Y.-F.; Piva, S.R.; Fitzgerald, G.K.; Jeong, J.-H.; Kwoh, C.K. The Influence of Knee Pain Location on Symptoms, Functional Status, and Knee-Related Quality of Life in Older Adults with Chronic Knee Pain: Data from the Osteoarthritis Initiative. Clin. J. Pain 2016, 32, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Sophia Fox, A.J.; Bedi, A.; Rodeo, S.A. The Basic Science of Articular Cartilage: Structure, Composition, and Function. Sports Health Multidiscip. Approach 2009, 1, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Alford, J.W.; Cole, B.J. Cartilage Restoration, Part 1: Basic Science, Historical Perspective, Patient Evaluation, and Treatment Options. Am. J. Sports Med. 2005, 33, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Oldershaw, R.A. Cell Sources for the Regeneration of Articular Cartilage: The Past, the Horizon and the Future. Int. J. Exp. Pathol. 2012, 93, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Moyad, T.F. Cartilage Injuries in the Adult Knee: Evaluation and Management. Cartilage 2011, 2, 226–236. [Google Scholar] [CrossRef]
- McCann, L.; Ingham, E.; Jin, Z.; Fisher, J. Influence of the Meniscus on Friction and Degradation of Cartilage in the Natural Knee Joint. Osteoarthr. Cartil. 2009, 17, 995–1000. [Google Scholar] [CrossRef]
- Hjelle, K.; Solheim, E.; Strand, T.; Muri, R.; Brittberg, M. Articular Cartilage Defects in 1000 Knee Arthroscopies. Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 730–734. [Google Scholar] [CrossRef]
- Rosneck, J.; Higuera, C.A.; Tadross, N.; Krebs, V.; Barsoum, W.K. Managing Knee Osteoarthritis before and after Arthroplasty. Cleve. Clin. J. Med. 2007, 74, 663–671. [Google Scholar] [CrossRef]
- Jerosch, J. Effects of Glucosamine and Chondroitin Sulfate on Cartilage Metabolism in OA: Outlook on Other Nutrient Partners Especially Omega-3 Fatty Acids. Int. J. Rheumatol. 2011, 2011, 969012. [Google Scholar] [CrossRef]
- Lubowitz, J.H. Editorial Commentary: Knee Hyaluronic Acid Viscosupplementation Reduces Osteoarthritis Pain. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 2046. [Google Scholar] [CrossRef]
- Kon, E.; Mandelbaum, B.; Buda, R.; Filardo, G.; Delcogliano, M.; Timoncini, A.; Fornasari, P.M.; Giannini, S.; Marcacci, M. Platelet-Rich Plasma Intra-Articular Injection Versus Hyaluronic Acid Viscosupplementation as Treatments for Cartilage Pathology: From Early Degeneration to Osteoarthritis. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1490–1501. [Google Scholar] [CrossRef]
- Strauss, E.J.; Fonseca, L.E.; Shah, M.R.; Yorum, T. Management of Focal Cartilage Defects in the Knee—Is ACI the Answer? Bull. NYU Hosp. Jt. Dis. 2011, 69, 63–72. [Google Scholar] [PubMed]
- Van Den Borne, M.P.J.; Raijmakers, N.J.H.; Vanlauwe, J.; Victor, J.; De Jong, S.N.; Bellemans, J.; Saris, D.B.F. International Cartilage Repair Society (ICRS) and Oswestry Macroscopic Cartilage Evaluation Scores Validated for Use in Autologous Chondrocyte Implantation (ACI) and Microfracture. Osteoarthr. Cartil. 2007, 15, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Wluka, A.E.; Ding, C.; Jones, G.; Cicuttini, F.M. The Clinical Correlates of Articular Cartilage Defects in Symptomatic Knee Osteoarthritis: A Prospective Study. Rheumatology 2005, 44, 1311–1316. [Google Scholar] [CrossRef]
- Im, G.-I. The Concept of Early Osteoarthritis and Its Significance in Regenerative Medicine. Tissue Eng. Regen. Med. 2022, 19, 431–436. [Google Scholar] [CrossRef]
- Chawla, A.; Twycross-Lewis, R.; Maffulli, N. Microfracture Produces Inferior Outcomes to Other Cartilage Repair Techniques in Chondral Injuries in the Paediatric Knee. Br. Med. Bull. 2015, 116, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.J.; Asnis, P.D.; Berkson, E.M. The Treatment of Articular Cartilage Defects Using the Microfracture Technique. J. Orthop. Sports Phys. Ther. 2006, 36, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, J.J.; Steadman, J.R.; Silliman, J.H.A. Improvement of Full Thickness Chondral Defect Healing in the Human Knee after Debridement and Microfracture Using Continuous Passive Motion. Am. J. Knee Surg. 1994, 7, 109–116. [Google Scholar]
- Steadman, J.R.; Rodkey, W.G.; Briggs, K.K. Microfracture to Treat Full-Thickness Chondral Defects: Surgical Technique, Rehabilitation, and Outcomes. J. Knee Surg. 2002, 15, 170–176. [Google Scholar]
- Richter, D.L.; Schenck, R.C.; Wascher, D.C.; Treme, G. Knee Articular Cartilage Repair and Restoration Techniques: A Review of the Literature. Sports Health Multidiscip. Approach 2016, 8, 153–160. [Google Scholar] [CrossRef]
- Özmeriç, A. Treatment for Cartilage Injuries of the Knee with a New Treatment Algorithm. World J. Orthop. 2014, 5, 677. [Google Scholar] [CrossRef] [PubMed]
- Frisbie, D.D.; Trotter, G.W.; Powers, B.E.; Rodkey, W.G.; Steadman, J.R.; Howard, R.D.; Park, R.D.; McIlwraith, C.W. Arthroscopic Subchondral Bone Plate Microfracture Technique Augments Healing of Large Chondral Defects in the Radial Carpal Bone and Medial Femoral Condyle of Horses. Vet. Surg. 1999, 28, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Goebel, L.K.H.; Orth, P.; Cucchiarini, M.; Madry, H. Subchondral Drilling for Articular Cartilage Repair: A Systematic Review of Translational Research. Dis. Model. Mech. 2018, 11, dmm.034280. [Google Scholar] [CrossRef]
- Chen, H.; Sun, J.; Hoemann, C.D.; Lascau-Coman, V.; Ouyang, W.; McKee, M.D.; Shive, M.S.; Buschmann, M.D. Drilling and Microfracture Lead to Different Bone Structure and Necrosis during Bone-Marrow Stimulation for Cartilage Repair. J. Orthop. Res. 2009, 27, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Zedde, P.; Cudoni, S.; Giachetti, G.; Manunta, M.; Masala, G.; Brunetti, A.; Manunta, A. Subchondral Bone Remodeling: Comparing Nanofracture with Microfracture. An Ovine in Vivo Study. Joints 2016, 4, 087–093. [Google Scholar] [CrossRef]
- Chen, H.; Hoemann, C.D.; Sun, J.; Chevrier, A.; McKee, M.D.; Shive, M.S.; Hurtig, M.; Buschmann, M.D. Depth of Subchondral Perforation Influences the Outcome of Bone Marrow Stimulation Cartilage Repair: Surgical Parameters in Bone Marrow Stimulation. J. Orthop. Res. 2011, 29, 1178–1184. [Google Scholar] [CrossRef]
- Mithoefer, K.; Williams, R.J.; Warren, R.F.; Potter, H.G.; Spock, C.R.; Jones, E.C.; Wickiewicz, T.L.; Marx, R.G. Chondral Resurfacing of Articular Cartilage Defects in the Knee with the Microfracture Technique: Surgical Technique. J. Bone Jt. Surg. 2006, 88, 294–304. [Google Scholar] [CrossRef]
- Goyal, D.; Keyhani, S.; Lee, E.H.; Hui, J.H.P. Evidence-Based Status of Microfracture Technique: A Systematic Review of Level I and II Studies. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 1579–1588. [Google Scholar] [CrossRef]
- Chung, K.; Jung, M.; Jang, K.-M.; Park, S.-H.; Nam, B.J.; Kim, H.; Kim, S.-H. Particulated Costal Allocartilage with Microfracture Versus Microfracture Alone for Knee Cartilage Defects: A Multicenter, Prospective, Randomized, Participant- and Rater-Blinded Study. Orthop. J. Sports Med. 2023, 11, 23259671231185570. [Google Scholar] [CrossRef]
- Fortier, L.M.; Knapik, D.M.; Dasari, S.P.; Polce, E.M.; Familiari, F.; Gursoy, S.; Chahla, J. Clinical and Magnetic Resonance Imaging Outcomes after Microfracture Treatment with and without Augmentation for Focal Chondral Lesions in the Knee: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2023, 51, 2193–2206. [Google Scholar] [CrossRef]
- Görmeli, G.; Karakaplan, M.; Görmeli, C.A.; Sarıkaya, B.; Elmalı, N.; Ersoy, Y. Clinical Effects of Platelet-Rich Plasma and Hyaluronic Acid as an Additional Therapy for Talar Osteochondral Lesions Treated with Microfracture Surgery: A Prospective Randomized Clinical Trial. Foot Ankle Int. 2015, 36, 891–900. [Google Scholar] [CrossRef]
- Papalia, R.; Diaz Balzani, L.; Torre, G.; Tirindelli, M.C.; Nobile, C.; Maffulli, N.; Denaro, V. Intraoperative Application Platelet Rich Fibrin, Postoperative Injections OF PRP or Microfracture Only for Osteochondral Lesions of the Knee: A Five-Year Retrospective Evaluation. J. Biol. Regul. Homeost. Agents 2016, 30 (4 Suppl. 1), 41–49. [Google Scholar]
- Boffa, A.; Previtali, D.; Altamura, S.A.; Zaffagnini, S.; Candrian, C.; Filardo, G. Platelet-Rich Plasma Augmentation to Microfracture Provides a Limited Benefit for the Treatment of Cartilage Lesions: A Meta-Analysis. Orthop. J. Sports Med. 2020, 8, 232596712091050. [Google Scholar] [CrossRef]
- Miller, B.S.; Briggs, K.K.; Downie, B.; Steadman, J.R. Clinical Outcomes Following the Microfracture Procedure for Chondral Defects of the Knee: A Longitudinal Data Analysis. Cartilage 2010, 1, 108–112. [Google Scholar] [CrossRef]
- Gille, J.; Behrens, P.; Volpi, P.; De Girolamo, L.; Reiss, E.; Zoch, W.; Anders, S. Outcome of Autologous Matrix Induced Chondrogenesis (AMIC) in Cartilage Knee Surgery: Data of the AMIC Registry. Arch. Orthop. Trauma Surg. 2013, 133, 87–93. [Google Scholar] [CrossRef]
- Shive, M.S.; Stanish, W.D.; McCormack, R.; Forriol, F.; Mohtadi, N.; Pelet, S.; Desnoyers, J.; Méthot, S.; Vehik, K.; Restrepo, A. BST-CarGel® Treatment Maintains Cartilage Repair Superiority over Microfracture at 5 Years in a Multicenter Randomized Controlled Trial. Cartilage 2015, 6, 62–72. [Google Scholar] [CrossRef]
- Bentley, G.; Greer, R.B. Homotransplantation of Isolated Epiphyseal and Articular Cartilage Chondrocytes into Joint Surfaces of Rabbits. Nature 1971, 230, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Brittberg, M.; Lindahl, A.; Nilsson, A.; Ohlsson, C.; Isaksson, O.; Peterson, L. Treatment of Deep Cartilage Defects in the Knee with Autologous Chondrocyte Transplantation. N. Engl. J. Med. 1994, 331, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Gikas, P.D.; Bayliss, L.; Bentley, G.; Briggs, T.W.R. An Overview of Autologous Chondrocyte Implantation. J. Bone Jt. Surg. Br. 2009, 91, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Nawaz, S.Z.; Bentley, G.; Briggs, T.W.R.; Carrington, R.W.J.; Skinner, J.A.; Gallagher, K.R.; Dhinsa, B.S. Autologous Chondrocyte Implantation in the Knee: Mid-Term to Long-Term Results. J. Bone Jt. Surg. Am. 2014, 96, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Becher, C.; Laute, V.; Fickert, S.; Zinser, W.; Niemeyer, P.; John, T.; Diehl, P.; Kolombe, T.; Siebold, R.; Fay, J. Safety of Three Different Product Doses in Autologous Chondrocyte Implantation: Results of a Prospective, Randomised, Controlled Trial. J. Orthop. Surg. 2017, 12, 71. [Google Scholar] [CrossRef]
- Bentley, G.; Biant, L.C.; Vijayan, S.; Macmull, S.; Skinner, J.A.; Carrington, R.W.J. Minimum Ten-Year Results of a Prospective Randomised Study of Autologous Chondrocyte Implantation versus Mosaicplasty for Symptomatic Articular Cartilage Lesions of the Knee. J. Bone Jt. Surg. Br. 2012, 94-B, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Minas, T.; Von Keudell, A.; Bryant, T.; Gomoll, A.H. The John Insall Award: A Minimum 10-Year Outcome Study of Autologous Chondrocyte Implantation. Clin. Orthop. 2014, 472, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, W.; Skinner, J.A.; Gooding, C.R.; Carrington, R.W.J.; Flanagan, A.M.; Briggs, T.W.R.; Bentley, G. Autologous Chondrocyte Implantation versus Matrix-Induced Autologous Chondrocyte Implantation for Osteochondral Defects of the Knee: A Prospective, Randomised Study. J. Bone Jt. Surg. Br. 2005, 87-B, 640–645. [Google Scholar] [CrossRef] [PubMed]
- Białkowska, K.; Komorowski, P.; Bryszewska, M.; Miłowska, K. Spheroids as a Type of Three-Dimensional Cell Cultures—Examples of Methods of Preparation and the Most Important Application. Int. J. Mol. Sci. 2020, 21, 6225. [Google Scholar] [CrossRef]
- Anderer, U.; Libera, J. In Vitro Engineering of Human Autogenous Cartilage. J. Bone Miner. Res. 2002, 17, 1420–1429. [Google Scholar] [CrossRef]
- Hoburg, A.; Niemeyer, P.; Laute, V.; Zinser, W.; Becher, C.; Kolombe, T.; Fay, J.; Pietsch, S.; Kuźma, T.; Widuchowski, W.; et al. Sustained Superiority in KOOS Subscores after Matrix-Associated Chondrocyte Implantation Using Spheroids Compared to Microfracture. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2482–2493. [Google Scholar] [CrossRef]
- Vonk, L.A.; Roël, G.; Hernigou, J.; Kaps, C.; Hernigou, P. Role of Matrix-Associated Autologous Chondrocyte Implantation with Spheroids in the Treatment of Large Chondral Defects in the Knee: A Systematic Review. Int. J. Mol. Sci. 2021, 22, 7149. [Google Scholar] [CrossRef]
- Grevenstein, D.; Mamilos, A.; Schmitt, V.H.; Niedermair, T.; Wagner, W.; Kirkpatrick, C.J.; Brochhausen, C. Excellent Histological Results in Terms of Articular Cartilage Regeneration after Spheroid-Based Autologous Chondrocyte Implantation (ACI). Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 417–421. [Google Scholar] [CrossRef]
- Eschen, C.; Kaps, C.; Widuchowski, W.; Fickert, S.; Zinser, W.; Niemeyer, P.; Roël, G. Clinical Outcome Is Significantly Better with Spheroid-Based Autologous Chondrocyte Implantation Manufactured with More Stringent Cell Culture Criteria. Osteoarthr. Cartil. Open 2020, 2, 100033. [Google Scholar] [CrossRef]
- Hoburg, A.; Niemeyer, P.; Laute, V.; Zinser, W.; John, T.; Becher, C.; Izadpanah, K.; Diehl, P.; Kolombe, T.; Fay, J.; et al. Safety and Efficacy of Matrix-Associated Autologous Chondrocyte Implantation with Spheroids for Patellofemoral or Tibiofemoral Defects: A 5-Year Follow-up of a Phase 2, Dose-Confirmation Trial. Orthop. J. Sports Med. 2022, 10, 232596712110533. [Google Scholar] [CrossRef] [PubMed]
- Hoburg, A.; Löer, I.; Körsmeier, K.; Siebold, R.; Niemeyer, P.; Fickert, S.; Ruhnau, K. Matrix-Associated Autologous Chondrocyte Implantation Is an Effective Treatment at Midterm Follow-up in Adolescents and Young Adults. Orthop. J. Sports Med. 2019, 7, 232596711984107. [Google Scholar] [CrossRef] [PubMed]
- Pettenuzzo, S.; Arduino, A.; Belluzzi, E.; Pozzuoli, A.; Fontanella, C.G.; Ruggieri, P.; Salomoni, V.; Majorana, C.; Berardo, A. Biomechanics of Chondrocytes and Chondrons in Healthy Conditions and Osteoarthritis: A Review of the Mechanical Characterisations at the Microscale. Biomedicines 2023, 11, 1942. [Google Scholar] [CrossRef] [PubMed]
- Guilak, F. The Pericellular Matrix as a Transducer of Biomechanical and Biochemical Signals in Articular Cartilage. Ann. N. Y. Acad. Sci. 2006, 1068, 498–512. [Google Scholar] [CrossRef]
- Duan, W.; Zhao, Y.; Ren, X.; Zhao, R.; Li, Q.; Sun, Z.; Song, W.; Yang, Y.; Li, P.; Wei, X. Combination of Chondrocytes and Chondrons Improves Extracellular Matrix Production to Promote the Repairs of Defective Knee Cartilage in Rabbits. J. Orthop. Transl. 2021, 28, 47–54. [Google Scholar] [CrossRef]
- Saris, T.F.F.; De Windt, T.S.; Kester, E.C.; Vonk, L.A.; Custers, R.J.H.; Saris, D.B.F. Five-Year Outcome of 1-Stage Cell-Based Cartilage Repair Using Recycled Autologous Chondrons and Allogenic Mesenchymal Stromal Cells: A First-in-Human Clinical Trial. Am. J. Sports Med. 2021, 49, 941–947. [Google Scholar] [CrossRef]
- Korpershoek, J.V.; Vonk, L.A.; Kester, E.C.; Creemers, L.B.; De Windt, T.S.; Kip, M.M.A.; Saris, D.B.F.; Custers, R.J.H. Efficacy of One-Stage Cartilage Repair Using Allogeneic Mesenchymal Stromal Cells and Autologous Chondron Transplantation (IMPACT) Compared to Nonsurgical Treatment for Focal Articular Cartilage Lesions of the Knee: Study Protocol for a Crossover Randomized Controlled Trial. Trials 2020, 21, 842. [Google Scholar] [CrossRef]
- Patil, S.; Tapasvi, S.R. Osteochondral Autografts. Curr. Rev. Musculoskelet. Med. 2015, 8, 423–428. [Google Scholar] [CrossRef]
- Solheim, E.; Hegna, J.; Strand, T.; Harlem, T.; Inderhaug, E. Randomized Study of Long-Term (15–17 Years) Outcome after Microfracture versus Mosaicplasty in Knee Articular Cartilage Defects. Am. J. Sports Med. 2018, 46, 826–831. [Google Scholar] [CrossRef]
- Pareek, A.; Reardon, P.J.; Maak, T.G.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Long-Term Outcomes after Osteochondral Autograft Transfer: A Systematic Review at Mean Follow-up of 10.2 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 1174–1184. [Google Scholar] [CrossRef]
- Bentley, G.; Biant, L.C.; Carrington, R.W.J.; Akmal, M.; Goldberg, A.; Williams, A.M.; Skinner, J.A.; Pringle, J. A Prospective, Randomised Comparison of Autologous Chondrocyte Implantation versus Mosaicplasty for Osteochondral Defects in the Knee. J. Bone Joint Surg. Br. 2003, 85, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Shaw, K.A.; Waterman, B.R. Outcomes After Fresh Osteochondral Allograft Transplantation for Medium to Large Chondral Defects of the Knee. Orthop. J. Sports Med. 2019, 7, 232596711983229. [Google Scholar] [CrossRef] [PubMed]
- Briggs, D.T.; Sadr, K.N.; Pulido, P.A.; Bugbee, W.D. The Use of Osteochondral Allograft Transplantation for Primary Treatment of Cartilage Lesions in the Knee. Cartilage 2015, 6, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Chahal, J.; Gross, A.E.; Gross, C.; Mall, N.; Dwyer, T.; Chahal, A.; Whelan, D.B.; Cole, B.J. Outcomes of Osteochondral Allograft Transplantation in the Knee. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Levy, Y.D.; Görtz, S.; Pulido, P.A.; McCauley, J.C.; Bugbee, W.D. Do Fresh Osteochondral Allografts Successfully Treat Femoral Condyle Lesions? Clin. Orthop. 2013, 471, 231–237. [Google Scholar] [CrossRef]
- Cook, J.L.; Stoker, A.M.; Stannard, J.P.; Kuroki, K.; Cook, C.R.; Pfeiffer, F.M.; Bozynski, C.; Hung, C.T. A Novel System Improves Preservation of Osteochondral Allografts. Clin. Orthop. 2014, 472, 3404–3414. [Google Scholar] [CrossRef]
- Koh, Y.-G.; Jo, S.-B.; Kwon, O.-R.; Suh, D.-S.; Lee, S.-W.; Park, S.-H.; Choi, Y.-J. Mesenchymal Stem Cell Injections Improve Symptoms of Knee Osteoarthritis. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 748–755. [Google Scholar] [CrossRef]
- Jo, C.H.; Lee, Y.G.; Shin, W.H.; Kim, H.; Chai, J.W.; Jeong, E.C.; Kim, J.E.; Shim, H.; Shin, J.S.; Shin, I.S.; et al. Intra-Articular Injection of Mesenchymal Stem Cells for the Treatment of Osteoarthritis of the Knee: A Proof-of-Concept Clinical Trial. Stem Cells 2014, 32, 1254–1266. [Google Scholar] [CrossRef]
- Vega, A.; Martín-Ferrero, M.A.; Del Canto, F.; Alberca, M.; García, V.; Munar, A.; Orozco, L.; Soler, R.; Fuertes, J.J.; Huguet, M.; et al. Treatment of Knee Osteoarthritis with Allogeneic Bone Marrow Mesenchymal Stem Cells: A Randomized Controlled Trial. Transplantation 2015, 99, 1681–1690. [Google Scholar] [CrossRef]
- Sekiya, I.; Muneta, T.; Horie, M.; Koga, H. Arthroscopic Transplantation of Synovial Stem Cells Improves Clinical Outcomes in Knees with Cartilage Defects. Clin. Orthop. 2015, 473, 2316–2326. [Google Scholar] [CrossRef]
- Buda, R.; Vannini, F.; Cavallo, M.; Grigolo, B.; Cenacchi, A.; Giannini, S. Osteochondral Lesions of the Knee: A New One-Step Repair Technique with Bone-Marrow-Derived Cells. J. Bone Jt. Surg. 2010, 92 (Suppl. S2), 2–11. [Google Scholar] [CrossRef]
- Nejadnik, H.; Hui, J.H.; Feng Choong, E.P.; Tai, B.-C.; Lee, E.H. Autologous Bone Marrow–Derived Mesenchymal Stem Cells Versus Autologous Chondrocyte Implantation: An Observational Cohort Study. Am. J. Sports Med. 2010, 38, 1110–1116. [Google Scholar] [CrossRef] [PubMed]
- Salzmann, G.M.; Ossendorff, R.; Gilat, R.; Cole, B.J. Autologous Minced Cartilage Implantation for Treatment of Chondral and Osteochondral Lesions in the Knee Joint: An Overview. Cartilage 2021, 13 (Suppl. S1), 1124S–1136S. [Google Scholar] [CrossRef] [PubMed]
- Lotz, M.; Loeser, R.F. Effects of Aging on Articular Cartilage Homeostasis. Bone 2012, 51, 241–248. [Google Scholar] [CrossRef]
- Evuarherhe, A.; Condron, N.B.; Knapik, D.M.; Haunschild, E.D.; Gilat, R.; Huddleston, H.P.; Kaiser, J.T.; Parvaresh, K.C.; Wagner, K.R.; Chubinskaya, S.; et al. Effect of Mechanical Mincing on Minimally Manipulated Articular Cartilage for Surgical Transplantation. Am. J. Sports Med. 2022, 50, 2515–2525. [Google Scholar] [CrossRef] [PubMed]
- McCormick, F.; Yanke, A.; Provencher, M.T.; Cole, B.J. Minced Articular Cartilage—Basic Science, Surgical Technique, and Clinical Application. Sports Med. Arthrosc. Rev. 2008, 16, 217–220. [Google Scholar] [CrossRef]
- Salzmann, G.M.; Calek, A.-K.; Preiss, S. Second-Generation Autologous Minced Cartilage Repair Technique. Arthrosc. Tech. 2017, 6, e127–e131. [Google Scholar] [CrossRef]
- Massen, F.K.; Inauen, C.R.; Harder, L.P.; Runer, A.; Preiss, S.; Salzmann, G.M. One-Step Autologous Minced Cartilage Procedure for the Treatment of Knee Joint Chondral and Osteochondral Lesions: A Series of 27 Patients with 2-Year Follow-Up. Orthop. J. Sports Med. 2019, 7, 232596711985377. [Google Scholar] [CrossRef]
- Wodzig, M.H.H.; Peters, M.J.M.; Emanuel, K.S.; Van Hugten, P.P.W.; Wijnen, W.; Jutten, L.M.; Boymans, T.A.; Loeffen, D.V.; Emans, P.J. Minced Autologous Chondral Fragments with Fibrin Glue as a Simple Promising One-Step Cartilage Repair Procedure: A Clinical and MRI Study at 12-Month Follow-Up. Cartilage 2022, 13, 19–31. [Google Scholar] [CrossRef]
- Kon, E.; Roffi, A.; Filardo, G.; Tesei, G.; Marcacci, M. Scaffold-Based Cartilage Treatments: With or without Cells? A Systematic Review of Preclinical and Clinical Evidence. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 767–775. [Google Scholar] [CrossRef]
- Gobbi, A.; Scotti, C.; Karnatzikos, G.; Mudhigere, A.; Castro, M.; Peretti, G.M. One-Step Surgery with Multipotent Stem Cells and Hyaluronan-Based Scaffold for the Treatment of Full-Thickness Chondral Defects of the Knee in Patients Older than 45 Years. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2494–2501. [Google Scholar] [CrossRef] [PubMed]
- Aldrian, S.; Zak, L.; Wondrasch, B.; Albrecht, C.; Stelzeneder, B.; Binder, H.; Kovar, F.; Trattnig, S.; Marlovits, S. Clinical and Radiological Long-Term Outcomes after Matrix-Induced Autologous Chondrocyte Transplantation: A Prospective Follow-up at a Minimum of 10 Years. Am. J. Sports Med. 2014, 42, 2680–2688. [Google Scholar] [CrossRef] [PubMed]
- Berruto, M.; Delcogliano, M.; De Caro, F.; Carimati, G.; Uboldi, F.; Ferrua, P.; Ziveri, G.; De Biase, C.F. Treatment of Large Knee Osteochondral Lesions with a Biomimetic Scaffold: Results of a Multicenter Study of 49 Patients at 2-Year Follow-Up. Am. J. Sports Med. 2014, 42, 1607–1617. [Google Scholar] [CrossRef]
- Andriolo, L.; Reale, D.; Di Martino, A.; Boffa, A.; Zaffagnini, S.; Filardo, G. Cell-Free Scaffolds in Cartilage Knee Surgery: A Systematic Review and Meta-Analysis of Clinical Evidence. Cartilage 2021, 12, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Kon, E.; Filardo, G.; Di Matteo, B.; Perdisa, F.; Marcacci, M. Matrix Assisted Autologous Chondrocyte Transplantation for Cartilage Treatment: A Systematic Review. Bone Jt. Res. 2013, 2, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Shimomura, K.; Moriguchi, Y.; Murawski, C.D.; Yoshikawa, H.; Nakamura, N. Osteochondral Tissue Engineering with Biphasic Scaffold: Current Strategies and Techniques. Tissue Eng. Part B Rev. 2014, 20, 468–476. [Google Scholar] [CrossRef]
- Filardo, G.; Kon, E.; Andriolo, L.; Di Matteo, B.; Balboni, F.; Marcacci, M. Clinical Profiling in Cartilage Regeneration: Prognostic Factors for Midterm Results of Matrix-Assisted Autologous Chondrocyte Transplantation. Am. J. Sports Med. 2014, 42, 898–905. [Google Scholar] [CrossRef]
- Kon, E.; Filardo, G.; Brittberg, M.; Busacca, M.; Condello, V.; Engebretsen, L.; Marlovits, S.; Niemeyer, P.; Platzer, P.; Posthumus, M.; et al. A Multilayer Biomaterial for Osteochondral Regeneration Shows Superiority vs. Microfractures for the Treatment of Osteochondral Lesions in a Multicentre Randomized Trial at 2 Years. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2704–2715. [Google Scholar] [CrossRef]
- Lee, C.R.; Grodzinsky, A.J.; Hsu, H.-P.; Spector, M. Effects of a Cultured Autologous Chondrocyte-Seeded Type II Collagen Scaffold on the Healing of a Chondral Defect in a Canine Model. J. Orthop. Res. 2003, 21, 272–281. [Google Scholar] [CrossRef]
- Wong, C.-C.; Chen, C.-H.; Chiu, L.-H.; Tsuang, Y.-H.; Bai, M.-Y.; Chung, R.-J.; Lin, Y.-H.; Hsieh, F.-J.; Chen, Y.-T.; Yang, T.-L. Facilitating In Vivo Articular Cartilage Repair by Tissue-Engineered Cartilage Grafts Produced from Auricular Chondrocytes. Am. J. Sports Med. 2018, 46, 713–727. [Google Scholar] [CrossRef]
- Sayed, K.E.; Haisch, A.; John, T.; Marzahn, U.; Lohan, A.; Müller, R.D.; Kohl, B.; Ertel, W.; Stoelzel, K.; Schulze-Tanzil, G. Heterotopic Autologous Chondrocyte Transplantation—A Realistic Approach to Support Articular Cartilage Repair? Tissue Eng. Part B Rev. 2010, 16, 603–616. [Google Scholar] [CrossRef] [PubMed]
- Mumme, M.; Barbero, A.; Miot, S.; Wixmerten, A.; Feliciano, S.; Wolf, F.; Asnaghi, A.M.; Baumhoer, D.; Bieri, O.; Kretzschmar, M.; et al. Nasal Chondrocyte-Based Engineered Autologous Cartilage Tissue for Repair of Articular Cartilage Defects: An Observational First-in-Human Trial. Lancet 2016, 388, 1985–1994. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.-H.; Park, J.-Y.; Lee, J.-Y.; Lee, E.; Lee, J.; Kim, S.-G. Costal Chondrocyte–Derived Pellet-Type Autologous Chondrocyte Implantation for Treatment of Articular Cartilage Defect. Am. J. Sports Med. 2020, 48, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Lan, X.; Boluk, Y.; Adesida, A.B. 3D Bioprinting of Hyaline Cartilage Using Nasal Chondrocytes. Ann. Biomed. Eng. 2023. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, A.; Karnatzikos, G.; Kumar, A. Long-Term Results after Microfracture Treatment for Full-Thickness Knee Chondral Lesions in Athletes. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1986–1996. [Google Scholar] [CrossRef]
- Miller, B.; Steadman, J.; Briggs, K.; Rodrigo, J.; Rodkey, W. Patient Satisfaction and Outcome after Microfracture of the Degenerative Knee. J. Knee Surg. 2010, 17, 13–17. [Google Scholar] [CrossRef]
- Kreuz, P.C.; Steinwachs, M.R.; Erggelet, C.; Krause, S.J.; Konrad, G.; Uhl, M.; Südkamp, N. Results after Microfracture of Full-Thickness Chondral Defects in Different Compartments in the Knee. Osteoarthr. Cartil. 2006, 14, 1119–1125. [Google Scholar] [CrossRef]
- Volz, M.; Schaumburger, J.; Frick, H.; Grifka, J.; Anders, S. A Randomized Controlled Trial Demonstrating Sustained Benefit of Autologous Matrix-Induced Chondrogenesis over Microfracture at Five Years. Int. Orthop. 2017, 41, 797–804. [Google Scholar] [CrossRef]
- Niemeyer, P.; Laute, V.; Zinser, W.; John, T.; Becher, C.; Diehl, P.; Kolombe, T.; Fay, J.; Siebold, R.; Fickert, S. Safety and Efficacy of Matrix-Associated Autologous Chondrocyte Implantation with Spheroid Technology Is Independent of Spheroid Dose after 4 Years. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1130–1143. [Google Scholar] [CrossRef]
- Wolf, M.T.; Zhang, H.; Sharma, B.; Marcus, N.A.; Pietzner, U.; Fickert, S.; Lueth, A.; Albers, G.H.R.; Elisseeff, J.H. Two-Year Follow-Up and Remodeling Kinetics of ChonDux Hydrogel for Full-Thickness Cartilage Defect Repair in the Knee. Cartilage 2020, 11, 447–457. [Google Scholar] [CrossRef]
- Werner, B.C.; Cosgrove, C.T.; Gilmore, C.J.; Lyons, M.L.; Miller, M.D.; Brockmeier, S.F.; Diduch, D.R. Accelerated Return to Sport after Osteochondral Autograft Plug Transfer. Orthop. J. Sports Med. 2017, 5, 232596711770241. [Google Scholar] [CrossRef] [PubMed]
- Filardo, G.; Kon, E.; Di Matteo, B.; Di Martino, A.; Marcacci, M. Single-Plug Autologous Osteochondral Transplantation: Results at Minimum 16 Years’ Follow-Up. Orthopedics 2014, 37, e761–e767. [Google Scholar] [CrossRef] [PubMed]
- Filardo, G.; Kon, E.; Perdisa, F.; Tetta, C.; Di Martino, A.; Marcacci, M. Arthroscopic Mosaicplasty: Long-Term Outcome and Joint Degeneration Progression. Knee 2015, 22, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Cognault, J.; Seurat, O.; Chaussard, C.; Ionescu, S.; Saragaglia, D. Return to Sports after Autogenous Osteochondral Mosaicplasty of the Femoral Condyles: 25 Cases at a Mean Follow-up of 9 Years. Orthop. Traumatol. Surg. Res. 2015, 101, 313–317. [Google Scholar] [CrossRef]
- Hamahashi, K.; Toyoda, E.; Ishihara, M.; Mitani, G.; Takagaki, T.; Kaneshiro, N.; Maehara, M.; Takahashi, T.; Okada, E.; Watanabe, A.; et al. Polydactyly-Derived Allogeneic Chondrocyte Cell-Sheet Transplantation with High Tibial Osteotomy as Regenerative Therapy for Knee Osteoarthritis. NPJ Regen. Med. 2022, 7, 71. [Google Scholar] [CrossRef]
- Ossendorff, R.; Franke, K.; Erdle, B.; Uhl, M.; Südkamp, N.P.; Salzmann, G.M. Clinical and Radiographical Ten Years Long-Term Outcome of Microfracture vs. Autologous Chondrocyte Implantation: A Matched-Pair Analysis. Int. Orthop. 2019, 43, 553–559. [Google Scholar] [CrossRef]
- Saris, D.; Price, A.; Widuchowski, W.; Bertrand-Marchand, M.; Caron, J.; Drogset, J.O.; Emans, P.; Podskubka, A.; Tsuchida, A.; Kili, S.; et al. Matrix-Applied Characterized Autologous Cultured Chondrocytes Versus Microfracture: Two-Year Follow-up of a Prospective Randomized Trial. Am. J. Sports Med. 2014, 42, 1384–1394. [Google Scholar] [CrossRef]
- Ulstein, S.; Årøen, A.; Røtterud, J.H.; Løken, S.; Engebretsen, L.; Heir, S. Microfracture Technique versus Osteochondral Autologous Transplantation Mosaicplasty in Patients with Articular Chondral Lesions of the Knee: A Prospective Randomized Trial with Long-Term Follow-Up. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1207–1215. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Choi, Y.J.; Pak, K.H.; In, Y. Collagen Augmentation Improves the Quality of Cartilage Repair after Microfracture in Patients Undergoing High Tibial Osteotomy: A Randomized Controlled Trial. Am. J. Sports Med. 2017, 45, 1845–1855. [Google Scholar] [CrossRef]
- Altschuler, N.; Zaslav, K.R.; Di Matteo, B.; Sherman, S.L.; Gomoll, A.H.; Hacker, S.A.; Verdonk, P.; Dulic, O.; Patrascu, J.M.; Levy, A.S.; et al. Aragonite-Based Scaffold Versus Microfracture and Debridement for the Treatment of Knee Chondral and Osteochondral Lesions: Results of a Multicenter Randomized Controlled Trial. Am. J. Sports Med. 2023, 51, 957–967. [Google Scholar] [CrossRef]
- Venosa, M.; Calafiore, F.; Mazzoleni, M.; Romanini, E.; Cerciello, S.; Calvisi, V. Platelet-Rich Plasma and Adipose-Derived Mesenchymal Stem Cells in Association with Arthroscopic Microfracture of Knee Articular Cartilage Defects: A Pilot Randomized Controlled Trial. Adv. Orthop. 2022, 2022, 6048477. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.-H.; Yoo, J.D.; Choi, C.-H.; Lee, J.; Lee, J.-Y.; Kim, S.-G.; Park, J.-Y. Costal Chondrocyte–Derived Pellet-Type Autologous Chondrocyte Implantation versus Microfracture for Repair of Articular Cartilage Defects: A Prospective Randomized Trial. Cartilage 2021, 13 (Suppl. S1), 1092S–1104S. [Google Scholar] [CrossRef] [PubMed]
- Hoburg, A.; Niemeyer, P.; Laute, V.; Zinser, W.; Becher, C.; Kolombe, T.; Fay, J.; Pietsch, S.; Kuźma, T.; Widuchowski, W.; et al. Matrix-Associated Autologous Chondrocyte Implantation with Spheroid Technology Is Superior to Arthroscopic Microfracture at 36 Months Regarding Activities of Daily Living and Sporting Activities after Treatment. Cartilage 2021, 13 (Suppl. S1), 437S–448S. [Google Scholar] [CrossRef] [PubMed]
- Cole, B.J.; Haunschild, E.D.; Carter, T.; Meyer, J.; Fortier, L.A.; Gilat, R.; Mandelbaum, B.R.; Scopp, J.M.; Mall, N.A.; Cunningham, K.; et al. Clinically Significant Outcomes Following the Treatment of Focal Cartilage Defects of the Knee with Microfracture Augmentation Using Cartilage Allograft Extracellular Matrix: A Multicenter Prospective Study. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 1512–1521. [Google Scholar] [CrossRef]
- Lim, H.-C.; Park, Y.-B.; Ha, C.-W.; Cole, B.J.; Lee, B.-K.; Jeong, H.-J.; Kim, M.-K.; Bin, S.-I.; Choi, C.-H.; Choi, C.H.; et al. Allogeneic Umbilical Cord Blood–Derived Mesenchymal Stem Cell Implantation Versus Microfracture for Large, Full-Thickness Cartilage Defects in Older Patients: A Multicenter Randomized Clinical Trial and Extended 5-Year Clinical Follow-Up. Orthop. J. Sports Med. 2021, 9, 232596712097305. [Google Scholar] [CrossRef]
- Kim, M.S.; Chun, C.H.; Wang, J.H.; Kim, J.G.; Kang, S.-B.; Yoo, J.D.; Chon, J.-G.; Kim, M.K.; Moon, C.W.; Chang, C.B.; et al. Microfractures Versus a Porcine-Derived Collagen-Augmented Chondrogenesis Technique for Treating Knee Cartilage Defects: A Multicenter Randomized Controlled Trial. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 1612–1624. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).