A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study
Abstract
1. Introduction
2. Materials and Methods
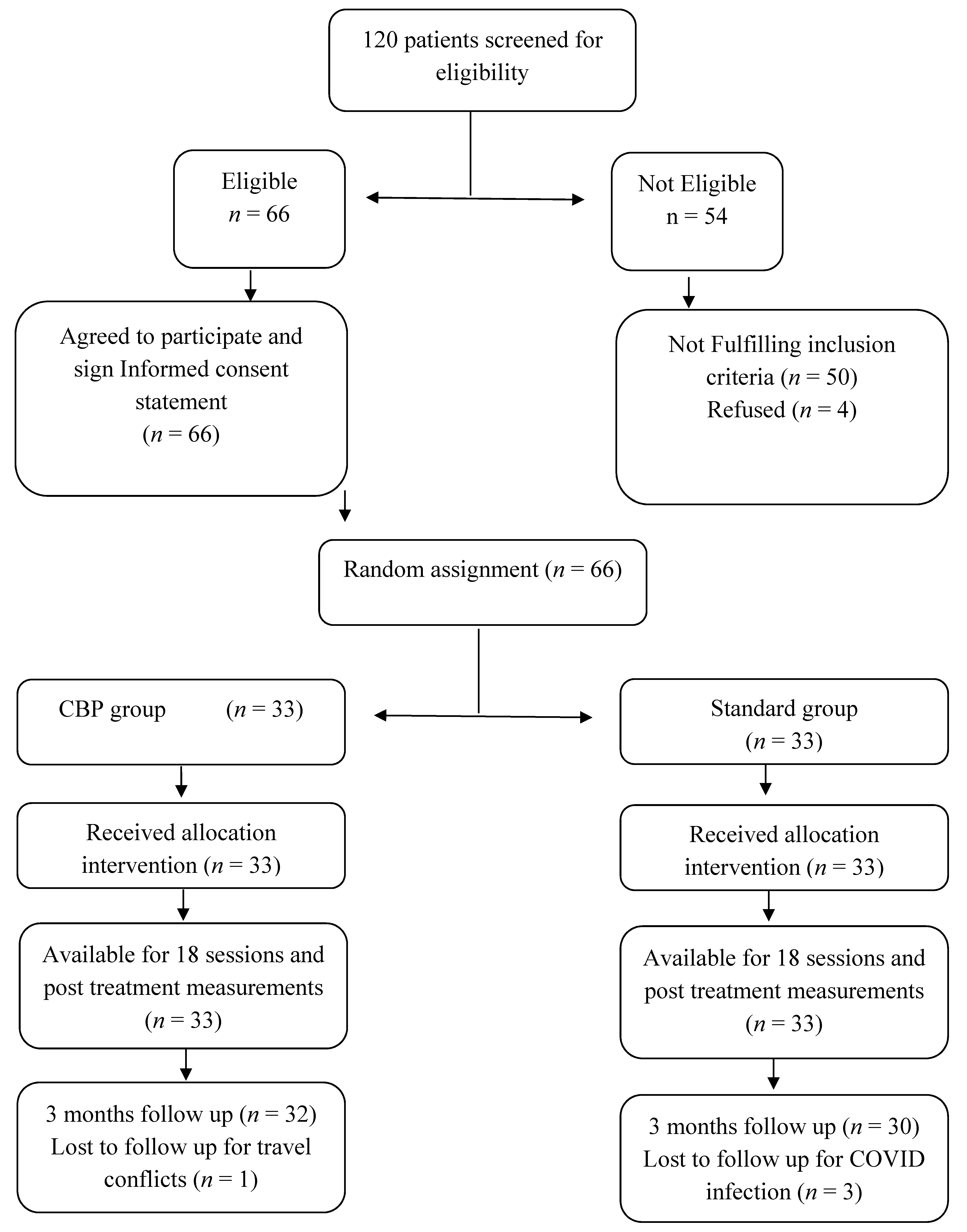
2.1. Participants
2.2. Randomization
2.3. Interventions
Denneroll™ Cervical Traction Orthotic (DCTO)
- (1)
- In the upper cervical area (C2-C4). This position allows for upper cervical segment extension bending while providing minor anterior head translation (AHT). This placement site was assigned to two participants.
- (2)
- In the mid-cervical area (C4-C6). This position allows for mid-upper cervical extension bending while causing a significant posterior head translation. This placement location was assigned to 8 participants.
- (3)
- Upper thoracic/lower cervical (C6-T1) area. This position allows for lower to intermediate cervical segment extension bending while causing substantial posterior head translation. This placement location was assigned to 23 participants.
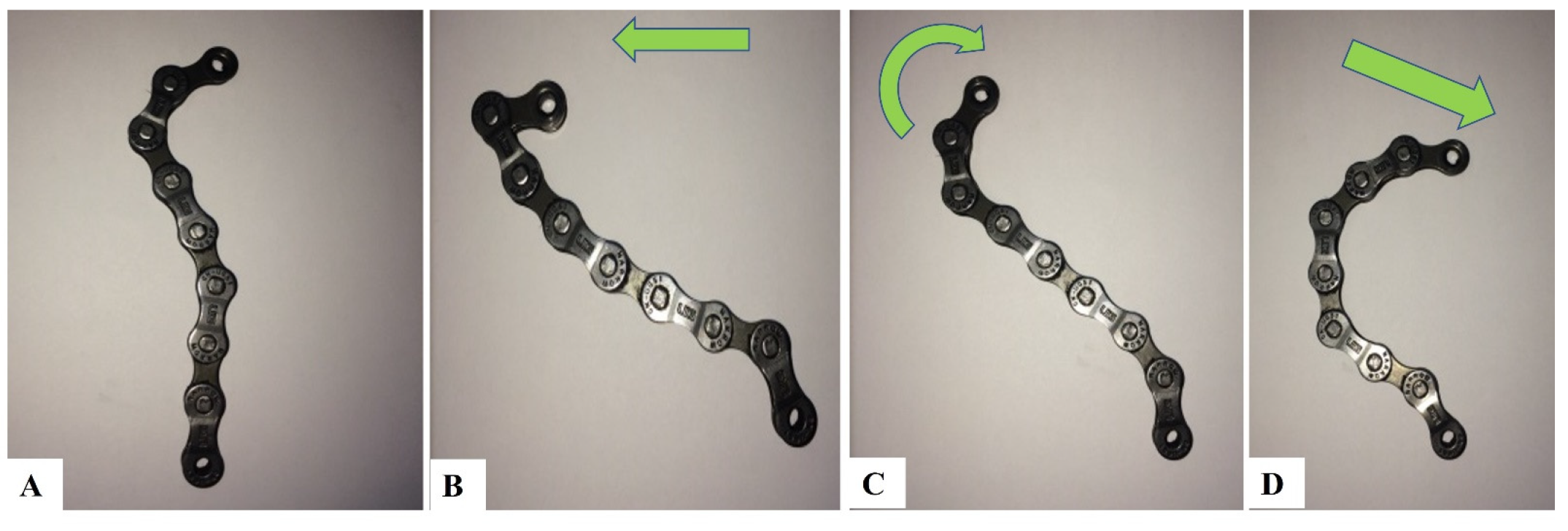
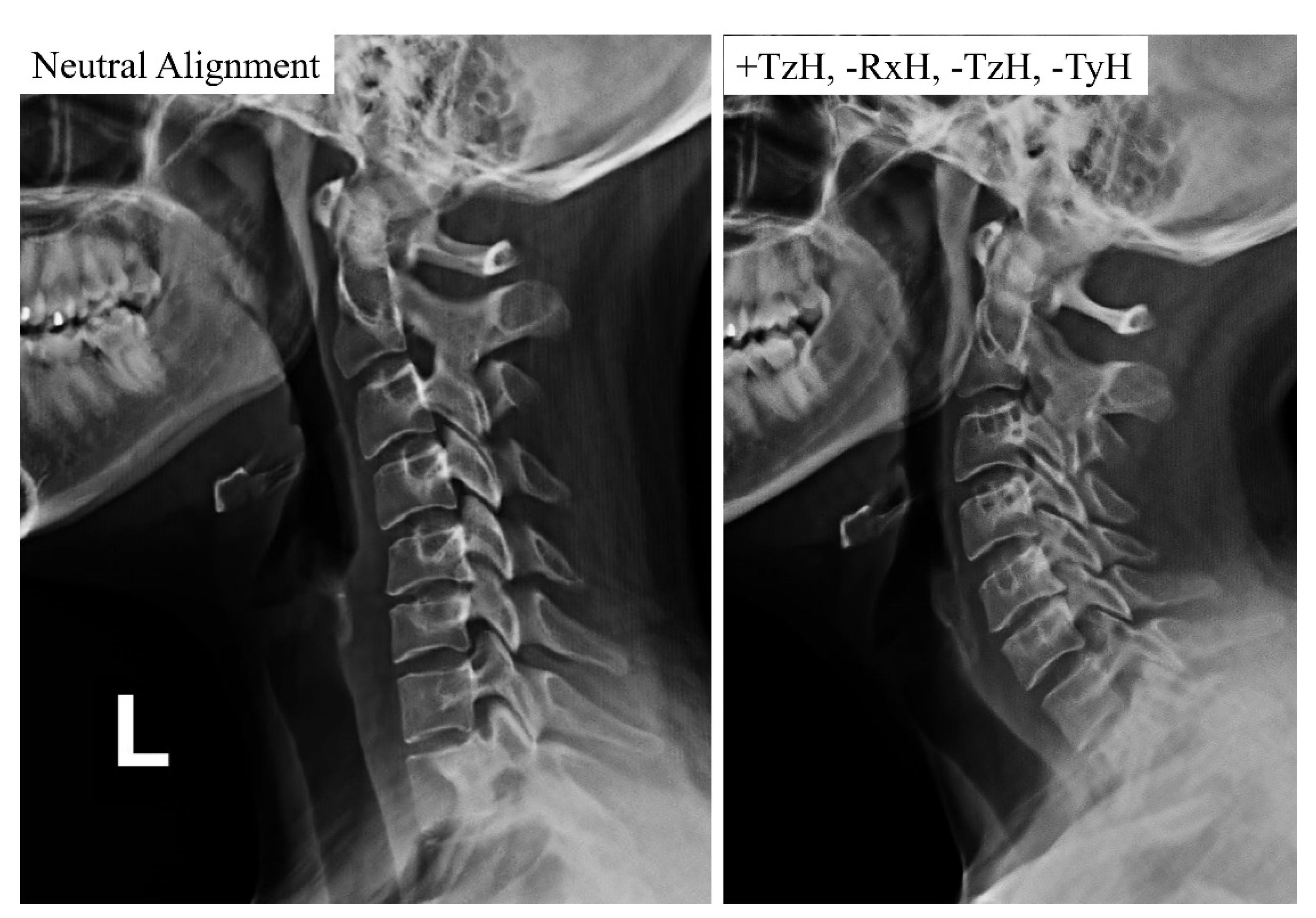
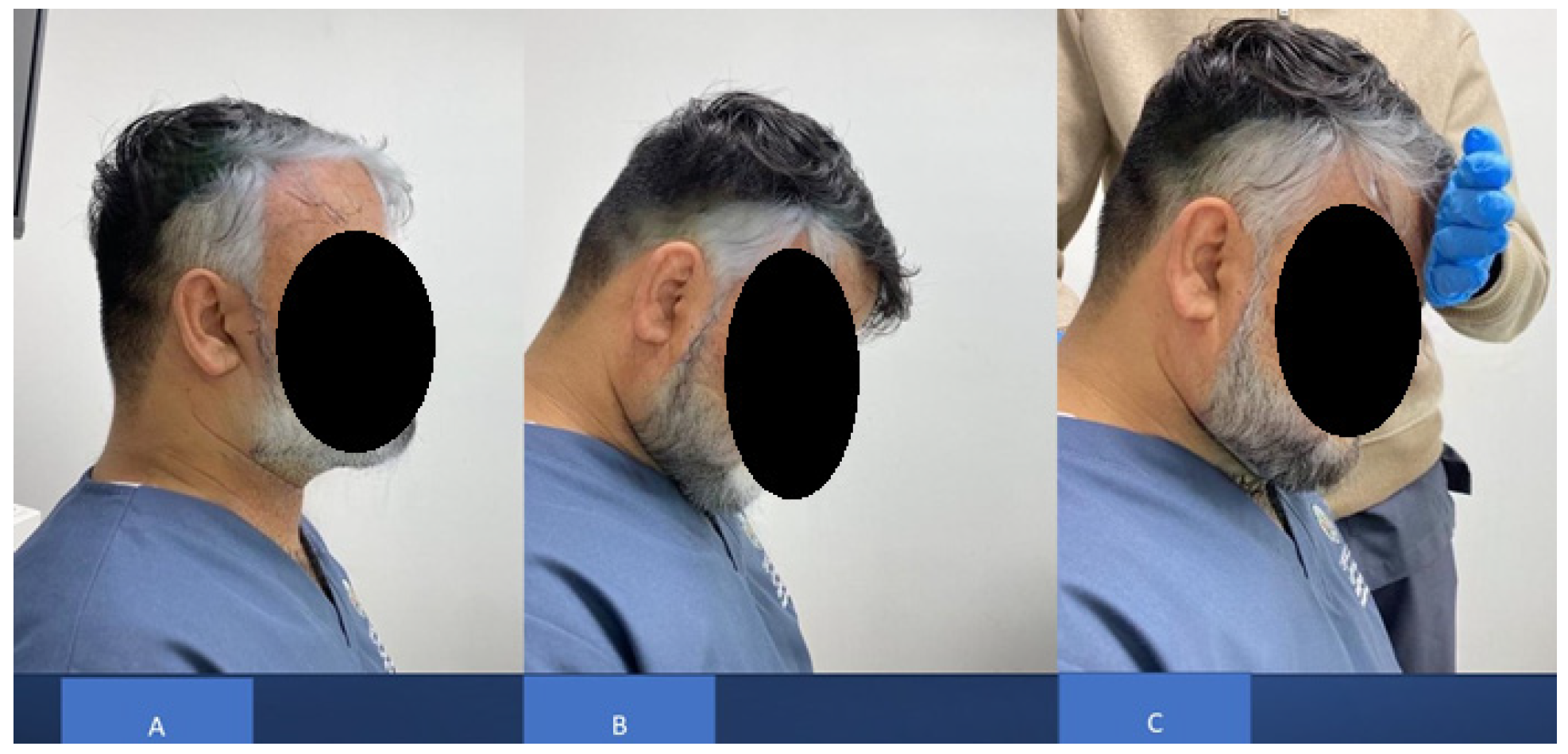
2.4. Mirror Image Exercises
- (1)
- Maximum anterior head translation (+TzH) Anterior head translation generates a cervical spine coupling pattern that results in lordosis of the upper cervical spine and kyphosis (curve reversal) of the lower cervical spine.
- (2)
- While maintaining +TzH, maximum head extension (−RxH). Maintaining anterior head translation permits the upper cervical spine to keep its lordosis, while maximal head extension allows the lower cervical spine to progress toward a healthy lordotic curvature.
- (3)
- While maintaining the −RxH, a posterior head translation (−TzH) with a slight inferior compression down the long axis of the spine (−TyH) is initiated. The posterior head translation with compression from this position allows for the head to return to a normal postural position while maintaining the induced cervical lordosis from the previous movements.
2.5. The Standardized Exercise Based FHP Correction Group (Standard Group)
- Chin tucks were performed while lying supine with the head in touch with the floor, which progressed to lifting the head off the floor in a tucked posture and holding it for varied periods of time (this was to progress by two-second holds starting at two seconds, i.e., 2, 4, 6, and 8 s. During the session, patients completed five chin tuck repetitions and five to seven sets of five chin tucks with a 1-min rest between each set. Figure 4 presents this exercise.
- Chin drop while sitting to stretch cervical extensors (the progression of this exercise was to drop the chin with hand assistance). The patients were instructed to flex the neck until a good stretch was felt at the base of the head and top of the neck. The patient held the final position for 5 s. This chin drop exercise was repeated a total of 10 times, or as tolerated. A modification of the chin tuck that further emphasizes strengthening of the deep neck flexor muscles is to apply resistance with a hand placed under the tucked chin and apply light downward pressure into the hand, or by adding manual resistance to the forehead using the 5-s hold time approach. Figure 5 demonstrates this exercise maneuver.
- Pulling the shoulders back using a theraband while standing to strengthen the shoulder retractors. The patient was instructed to squeeze their scapulae together tightly for at least 6 s without elevating or extending their shoulder. The initial progression step was to use weights to do shoulder retraction from a prone posture. The second stage involved the use of elastic resistance and weights. Each progression was carried out by the participants for two weeks. At the consultation, they were moved to the second progression if they could complete three sets of 12 repetitions, with 2 min of rest in between, accurately for appropriate strengthening. Figure 6 demonstrates this exercise maneuver.
- Every two weeks, participants alternated between unilateral and bilateral pectoralis stretches. The patient was seated comfortably with their hand behind their head for bilateral pectoralis stretching. From this posture, the patient’s elbow was pushed up and out to the limit of its possible range. The arm at the affected location was shifted into abduction and external rotation for unilateral stretching. The end position was maintained for 20–30 s and repeated 3–5 times. For unilateral stretching, the patients were directed to bring their hands up such that their forearms and elbows rested on the side of the doorway. The elbow and shoulder should be at a 90-degree angle. The patient was encouraged to move his or her body toward the opposite side away from the doorway until a stretch was felt anteriorly between the chest and shoulder. Each stretch was performed with slow, steady movements without any bouncing. The same process was repeated on the opposite side. This posture was maintained for 20–30 s and repeated 3–5 times. Two sets of 3–5 repetitions of unilateral self-stretching with a 1-min rest were performed for each patient. Figure 7 shows this exercise maneuver.
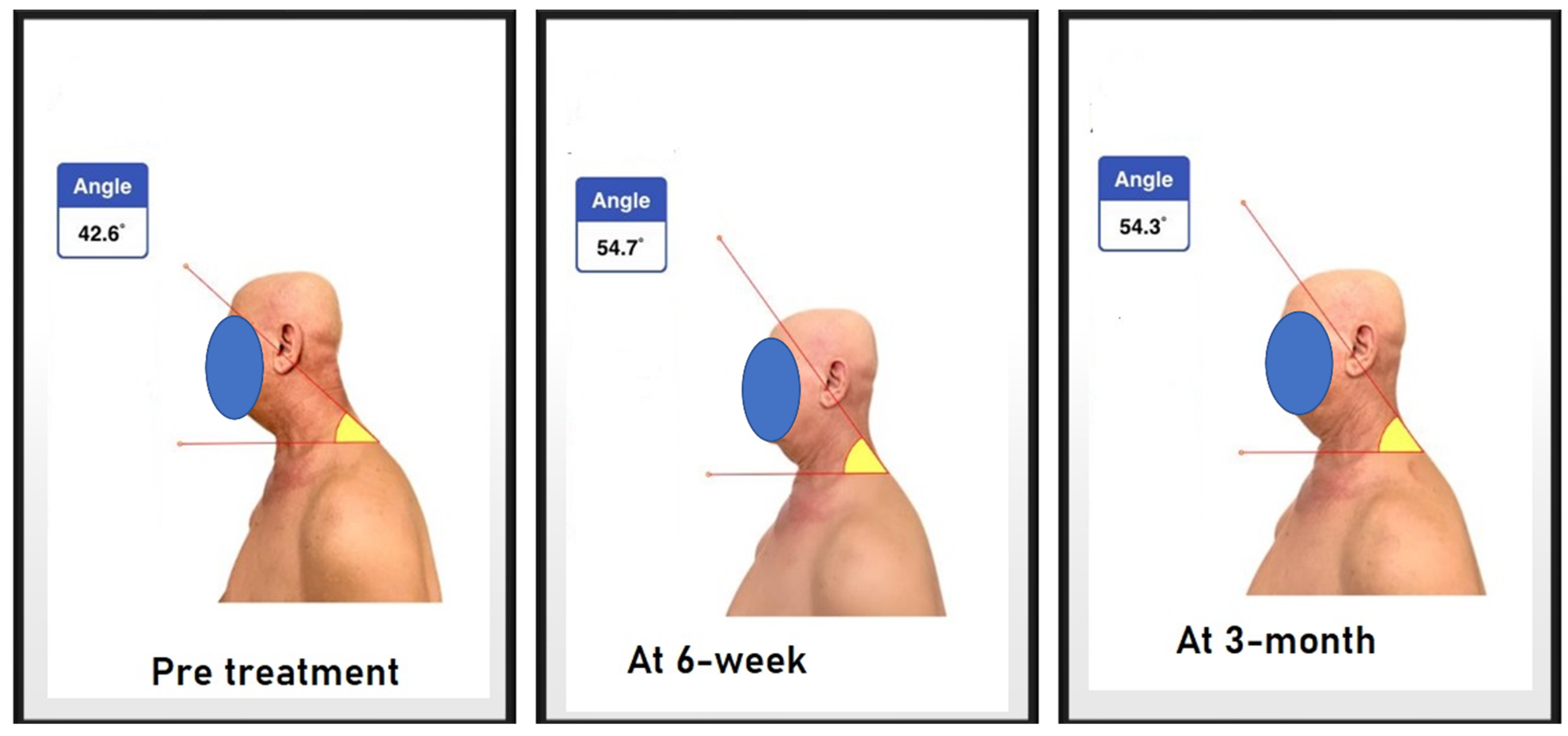
2.6. Outcome Measures
2.6.1. Craniovertebral Angle
2.6.2. Berg Balance Scale
2.6.3. Numeric Pain Rating Scale
2.6.4. Cervicocephalic Kinesthetic Sensibility
2.7. Sample Size Determination
2.8. Data Analysis
3. Results
Group Outcomes
4. Discussion
4.1. Sagittal Cervical Alignment
4.2. Balance, Pain, Cervicocephalic Kinesthetic Sensibility and ROM
4.3. Limitations
4.4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an Exercise Program to Improve Forward Head Posture in Normal Adults: A Randomized, Controlled 10-Week Trial. J. Man. Manip. Ther. 2005, 13, 163–176. [Google Scholar] [CrossRef]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.I.; Romani, W.A. Muscles: Testing and Function, with Posture and Pain; LWW: Baltimore, MD, USA, 2014. [Google Scholar]
- Griegel-Morris, P.; Larson, K.; Mueller-Klaus, K.; Oatis, C.A. Incidence of Common Postural Abnormalities in the Cervical, Shoulder, and Thoracic Regions and Their Association with Pain in Two Age Groups of Healthy Subjects. Phys. Ther. 1992, 72, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef]
- Quek, J.; Pua, Y.H.; Clark, R.A.; Bryant, A.L. Effects of Thoracic Kyphosis and Forward Head Posture on Cervical Range of Motion in Older Adults. Man. Ther. 2013, 18, 65–71. [Google Scholar] [CrossRef]
- Lee, J.H. Effects of Forward Head Posture on Static and Dynamic Balance Control. J. Phys. Ther. Sci. 2016, 28, 274–277. [Google Scholar] [CrossRef]
- Koseki, T.; Kakizaki, F.; Hayashi, S.; Nishida, N.; Itoh, M. Effect of Forward Head Posture on Thoracic Shape and Respiratory Function. J. Phys. Ther. Sci. 2019, 31, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Diab, A.A.; Moustafa, I.M. The Efficacy of Forward Head Correction on Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial. Clin. Rehabil. 2012, 26, 351–361. [Google Scholar] [CrossRef]
- Ling, F.P.; Chevillotte, T.; Leglise, A.; Thompson, W.; Bouthors, C.; Le Huec, J.C. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur. Spine J. 2018, 27 (Suppl. S1), 8–15. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Effects of a Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Posture in Adolescents. J. Manip. Physiol. Ther. 2017, 40, 1–10. [Google Scholar] [CrossRef]
- Oakley, P.A.; Moustafa, I.M.; Harrison, D.E. Restoration of Cervical and Lumbar Lordosis: CBP® Methods Overview. In Spinal Deformities in Adolescents, Adults and Older Adults; IntechOpen: London, UK, 2021. [Google Scholar]
- Harrison, D.D.; Janik, T.J.; Harrison, G.R.; Troyanovich, S.; Harrison, D.E.; Harrison, S.O. Chiropractic biophysics technique: A linear algebra approach to posture in chiropractic. J. Manip. Physiol. Ther. 1996, 19, 525–535. [Google Scholar]
- Oakley, P.A.; Harrison, D.D.; Harrison, D.E.; Haas, J.W. Evidence-Based Protocol for Structural Rehabilitation of the Spine and Posture: Review of Clinical Biomechanics of Posture (CBP) Publications. J. Can. Chiropr. Assoc. 2005, 49, 270–296. [Google Scholar] [PubMed]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring Cervical Lordosis by Cervical Extension Traction Methods in the Treatment of Cervical Spine Disorders: A Systematic Review of Controlled Trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. J. Clin. Med. 2022, 11, 6515. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A.M.; Harrison, D.E. Does Improvement towards a Normal Cervical Sagittal Configuration Aid in the Management of Lumbosacral Radiculopathy: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 5768. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Carita, A.I.; Pezarat-Correia, P. The Effects of Training and Detraining after an 8 Month Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Postures in Adolescents: Randomised Controlled Study. Man. Ther. 2016, 21, 76–82. [Google Scholar] [CrossRef]
- Diab, A.A. The Role of Forward Head Correction in Management of Adolescent Idiopathic Scoliotic Patients: A Randomized Controlled Trial. Clin. Rehabil. 2012, 26, 1123–1132. [Google Scholar] [CrossRef]
- Mulet, M.; Decker, K.L.; Look, J.O.; Lenton, P.A.; Schiffman, E.L. A Randomized Clinical Trial Assessing the Efficacy of Adding 6 x 6 Exercises to Self-Care for the Treatment of Masticatory Myofascial Pain. J. Orofac. Pain 2007, 21, 318–328. [Google Scholar]
- Im, B.; Kim, Y.; Chung, Y.; Hwang, S. Effects of Scapular Stabilization Exercise on Neck Posture and Muscle Activation in Individuals with Neck Pain and Forward Head Posture. J. Physical. Ther. Sci. 2015, 28, 951–955. [Google Scholar] [CrossRef]
- Jang, H.J.; Kim, M.J.; Kim, S.Y. Effect of Thorax Correction Exercises on Flexed Posture and Chest Function in Older Women with Age-Related Hyperkyphosis. J. Phys. Ther. Sci. 2015, 27, 1161–1164. [Google Scholar] [CrossRef]
- Kang, D.Y. Deep Cervical Flexor Training with a Pressure Biofeedback Unit Is an Effective Method for Maintaining Neck Mobility and Muscular Endurance in College Students with Forward Head Posture. J. Phys. Ther. Sci. 2015, 27, 3207–3210. [Google Scholar] [CrossRef]
- Kang, J.-I.; Jeong, D.-K.; Choi, H. The Effect of Feedback Respiratory Exercise on Muscle Activity, Craniovertebral Angle, and Neck Disability Index of the Neck Flexors of Patients with Forward Head Posture. J. Phys. Ther. Sci. 2016, 28, 2477–2481. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, C.H.; O’Sullivan, D.; Jung, J.H.; Park, J.J. Clinical Effectiveness of a Pilates Treatment for Forward Head Posture. J. Phys. Ther. Sci. 2016, 28, 2009–2013. [Google Scholar] [CrossRef] [PubMed]
- Seidi, F.; Rajabi, R.; Ebrahimi, I.; Alizadeh, M.H.; Minoonejad, H. The Efficiency of Corrective Exercise Interventions on Thoracic Hyper-Kyphosis Angle. J. Back Musculoskelet. Rehabil. 2014, 27, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, S.; Uehara, M.; Tokida, R.; Nishimura, H.; Sakai, N.; Horiuchi, H.; Kato, H.; Takahashi, J. Cervical Spinal Alignment Change Accompanying Spondylosis Exposes Harmonization Failure with Total Spinal Balance: A Japanese Cohort Survey Randomly Sampled from a Basic Resident Registry. J. Clin. Med. 2021, 10, 5737. [Google Scholar] [CrossRef]
- Yip, C.H.T.; Chiu, T.T.W.; Poon, A.T.K. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef]
- Fedorchuk, C. Cervical Coupling Patterns following head retraction with compression to neutral: A Prospective Study. In Proceedings of the 39th CBP Annual Convention, Scottsdale, AZ, USA, 13–15 October 2017. [Google Scholar]
- Fedorchuk, C.; Lightstone, D.; Comer, R. Radiographic stress analysis to determine the proper coupling patterns of the cervical spine prior to intervention. In Proceedings of the 2nd International Conference on Medical Imaging and Case Reports (MICR) 2019, Newton, Boston, MA, USA, 20–22 November 2019. [Google Scholar]
- SolakoÄa&lu, Ö.; Yalçin, P.; Dinçer, G. The Effects of Forward Head Posture on Expiratory Muscle Strength in Chronic Neck Pain Patients: A Cross-Sectional Study. Turk. J. Phys. Med. Rehabil. 2020, 66, 161–168. [Google Scholar] [CrossRef]
- Subbarayalu, A.V. Measurement of Craniovertebral Angle by the Modified Head Posture Spinal Curvature Instrument: A Reliability and Validity Study. Physiother. Theory Pract. 2016, 32, 144–152. [Google Scholar] [CrossRef]
- Pickenbrock, H.M.; Diel, A.; Zapf, A. A Comparison between the Static Balance Test and the Berg Balance Scale: Validity, Reliability, and Comparative Resource Use. Clin. Rehabil. 2016, 30, 288–293. [Google Scholar] [CrossRef]
- Young, I.A.; Dunning, J.; Butts, R.; Mourad, F.; Cleland, J.A. Reliability, Construct Validity, and Responsiveness of the Neck Disability Index and Numeric Pain Rating Scale in Patients with Mechanical Neck Pain without Upper Extremity Symptoms. Physiother. Theory Pract. 2019, 35, 1328–1335. [Google Scholar] [CrossRef]
- Rix, G.D.; Bagust, J. Cervicocephalic Kinesthetic Sensibility in Patients with Chronic, Nontraumatic Cervical Spine Pain. Arch. Phys. Med. Rehabil. 2001, 82, 911–919. [Google Scholar] [CrossRef]
- Lee, H.Y.; Teng, C.C.; Chai, H.M.; Wang, S.F. Test-Retest Reliability of Cervicocephalic Kinesthetic Sensibility in Three Cardinal Planes. Man. Ther. 2006, 11, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.Y.; Maiya, A.G.; Rao, S.K. Effect of age on cervicocephalic kinesthetic sensibiity. Int. J. Curr. Res. Rev. 2011, 3, 42–48. [Google Scholar]
- Moustafa, I.M.; Diab, A.A.; Hegazy, F.; Harrison, D.E. Does Improvement towards a Normal Cervical Sagittal Configuration Aid in the Management of Cervical Myofascial Pain Syndrome: A 1- Year Randomized Controlled Trial. BMC Musculoskelet. Disord. 2018, 19, 396. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Effect of Normalizing the Sagittal Cervical Configuration on Dizziness, Neck Pain, and Cervicocephalic Kinesthetic Sensibility: A 1-Year Randomized Controlled Study. Eur. J. Phys. Rehabil. Med. 2017, 53, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A.; Taha, S.; Harrison, D.E. Addition of a Sagittal Cervical Posture Corrective Orthotic Device to a Multimodal Rehabilitation Program Improves Short- and Long-Term Outcomes in Patients With Discogenic Cervical Radiculopathy. Arch. Phys. Med. Rehabil. 2016, 97, 2034–2044. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Betz, J.J.; Janik, T.J.; Holland, B.; Colloca, C.J.; Haas, J.W. Increasing the Cervical Lordosis with Chiropractic Biophysics Seated Combined Extension-Compression and Transverse Load Cervical Traction with Cervical Manipulation: Nonrandomized Clinical Control Trial. J. Manip. Physiol. Ther. 2003, 26, 139–151, Erratum in J. Manip. Physiol. Ther. 2005, 28, 214. [Google Scholar] [CrossRef]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Janik, T.J.; Holland, B. A New 3-Point Bending Traction Method for Restoring Cervical Lordosis and Cervical Manipulation: A Nonrandomized Clinical Controlled Trial. Arch. Phys. Med. Rehabil. 2002, 83, 447–453. [Google Scholar] [CrossRef]
- Oliver, M.J.; Twomey, L.T. Extension creep in the lumbar spine. Clin. Biomech. 1995, 10, 363–368. [Google Scholar] [CrossRef]
- Jackson, A.; Gu, W. Transport Properties of Cartilaginous Tissues. Curr. Rheumatol. Rev. 2009, 5, 40–50. [Google Scholar] [CrossRef]
- Zioupos, P.; Currey, J.D.; Hamer, A.J. The Role of Collagen in the Declining Mechanical Properties of Aging Human Cortical Bone. J. Biomed. Mater. Res. 1999, 45, 108–116. [Google Scholar] [CrossRef]
- Wallmann, H.W. Stretching and Flexibility in the Aging Adult. Home Health Care Manag. Pract. 2009, 21, 355–357. [Google Scholar] [CrossRef]
- Harrison, D.E.; Colloca, C.J.; Harrison, D.D.; Janik, T.J.; Haas, J.W.; Keller, T.S. Anterior Thoracic Posture Increases Thoracolumbar Disc Loading. Eur. Spine J. 2005, 14, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Keller, T.S.; Colloca, C.J.; Harrison, D.E.; Harrison, D.D.; Janik, T.J. Influence of Spine Morphology on Intervertebral Disc Loads and Stresses in Asymptomatic Adults: Implications for the Ideal Spine. Spine J. 2005, 5, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Protopsaltis, T.S.; Scheer, J.K.; Terran, J.S.; Smith, J.S.; Hamilton, D.K.; Kim, H.J.; Mundis, G.M.; Hart, R.A.; McCarthy, I.M.; Klineberg, E.; et al. How the Neck Affects the Back: Changes in Regional Cervical Sagittal Alignment Correlate to HRQOL Improvement in Adult Thoracolumbar Deformity Patients at 2-Year Follow-Up. J. Neurosurg. Spine 2015, 23, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.K.; Passias, P.G.; Sorocean, A.M.; Boniello, A.J.; Mundis, G.M.; Klineberg, E.; Kim, H.J.; Protopsaltis, T.S.; Gupta, M.; Bess, S.; et al. Association between Preoperative Cervical Sagittal Deformity and Inferior Outcomes at 2-Year Follow-up in Patients with Adult Thoracolumbar Deformity: Analysis of 182 Patients. J. Neurosurg. Spine 2016, 24, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The Impact of Positive Sagittal Balance in Adult Spinal Deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Troyanovich, S.J.; Harrison, S.O. A Review of Biomechanics of the Central Nervous System—Part II: Spinal Cord Strains from Postural Loads. J. Manip. Physiol. Ther. 1999, 22, 322–332. [Google Scholar] [CrossRef]
- Breig, A.; Marions, O. Biomechanics of the Lumbosacral Nerve Roots. Acta Radiol. 1963, 1, 1141–1160. [Google Scholar] [CrossRef]
- Berland, R.; Marques-Sule, E.; Marín-Mateo, J.L.; Moreno-Segura, N.; López-Ridaura, A.; Sentandreu-Mañó, T. Effects of the Feldenkrais Method as a Physiotherapy Tool: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 13734. [Google Scholar] [CrossRef]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Ferrantelli, J.R.; Haas, J.W.; Holland, B. Modeling of the Sagittal Cervical Spine as a Method to Discriminate Hypolordosis: Results of Elliptical and Circular Modeling in 72 Asymptomatic Subjects, 52 Acute Neck Pain Subjects, and 70 Chronic Neck Pain Subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef]
- McAviney, J.; Schulz, D.; Bock, R.; Harrison, D.E.; Holland, B. Determining the Relationship between Cervical Lordosis and Neck Complaints. J. Manip. Physiol. Ther. 2005, 28, 187–193. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Youssef, A.; Ahbouch, A.; Tamim, M.; Harrison, D.E. Is Forward Head Posture Relevant to Autonomic Nervous System Function and Cervical Sensorimotor Control? Cross Sectional Study. Gait Posture 2020, 77, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Darnell, M.W. A Proposed Chronology of Events for Forward Head Posture. J. Craniomandib. Pract. 1983, 1, 49–54. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Panjabi, A.A. Clinical Biomechanics of the Spine, 2nd ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 1990; Volume 2. [Google Scholar]
- Miyazaki, M.; Hymanson, H.J.; Morishita, Y.; He, W.; Zhang, H.; Wu, G.; Kong, M.H.; Tsumura, H.; Wang, J.C. Kinematic Analysis of the Relationship between Sagittal Alignment and Disc Degeneration in the Cervical Spine. Spine 2008, 33, E870–E876. [Google Scholar] [CrossRef] [PubMed]




| Demographic Information | CBP Group (n = 33) | Standard Group (n = 33) | p Value |
|---|---|---|---|
| Age (y) | 63.5 ± 3 | 65 ± 4.2 | 0.09 |
| Weight (kg) | 66 ± 10 | 60 ± 19 | 0.1 |
| Sex, Marital status | |||
| Male | 22 (67%) | 20 (60%) | 0.3 |
| Female | 11 (33%) | 13 (40%) | |
| Single | 1 (3%) | 2 (7%) | |
| Married | 22 (67%) | 20 (60%) | |
| Separated, divorced, or widowed | 10 (30%) | 11 (33%) | |
| Pain duration (%) [Mean ± SD] | |||
| < 1 y | 1 (3%) | 3 (10%) | 0.1 |
| 1–2 y | 21 (67%) | 20 (60%) | |
| >2 y | 10 (30%) | 10 (30%) | |
| Smoking history | |||
| Light smoker | 8 (24%) | 7 (21%) | 0.2 |
| Heavy smoker | 0 | 1 | |
| Non-Smoker | 25 (76%) | 26 (79%) | |
| Baseline | 6-Weeks | 3-Month Follow-Up | p-Value | ||||
|---|---|---|---|---|---|---|---|
| G | T | G vs. T | |||||
| CVA | CBP G | 41.4 ± 2.6 | 54.9 ± 3.2 | 54 ± 2.6 | <0.001 * F = 76 Partial Eta squared = 0.5 | <0.001 * F = 248 Partial Eta squared= 0.8 | <0.001 * F = 131 Partial Eta squared = 0.7 |
| Standard G | 42.7 ± 3.2 | 45 ± 2.4 | 45.6 ± 5.9 | ||||
| p-Value 95% C.I. | 0.08 [−2.7, 0.2] | <0.001 * [8.7, 11.1] | <0.001 * [6.1, 10.7] | ||||
| Pain intensity | CBP G | 4.7 ± 0.8 | 1.1 ± 0.7 | 0.5 ± 0.8 | <0.001 * F = 209 Partial Eta squared = 0.7 | <0.001 * F = 244 Partial Eta squared = 0.8 | <0.001 * F = 54 Partial Eta squared = 0.6 |
| Standard G | 5.3 ± 1.5 | 2.9 ± 1.2 | 4.3 ± 1 | ||||
| p-Value 95% C.I. | 0.08 [−1.19, 0.008] | <0.001 * [−2.2, −1.2] | <0.001 * [−4.2, −3.2] | ||||
| Baseline | 6-Weeks | 3-Month Follow-Up | p-Value | ||||
|---|---|---|---|---|---|---|---|
| G | T | G vs. T | |||||
| Berg Balance Score | CBP G | 43 ± 2.1 | 48.1 ± 3 | 48.2 ± 3.2 | <0.001 * F = 28.3 Partial Eta squared =0.3 | <0.001 * F = 91.3 Partial Eta squared = 0.6 | <0.001 * F = 29.2 Partial Eta squared = 0.7 |
| Standard G | 42.3± 2.2 | 44.6 ± 1.7 | 43.8 ± 2.1 | ||||
| p-Value C.I. | 0.2 [−0.49, 1.7] | 0.48 [2.2, 4.7] | <0.001 * [2.9, 5.5] | ||||
| HRA Right | CBP G | 3.4 ± 0.6 | 2.1 ± 0.9 | 0.3 ± 0.5 | <0.001 * F = 43 Partial Eta squared = 0.5 | <0.001 * F = 193 Partial Eta squared = 0.8 | <0.001 * F = 183 Partial Eta squared = 0.8 |
| Standard G | 3 ± 0.9 | 2.2 ± 1.1 | 2.7 ± 1 | ||||
| p-Value C.I. | 0.06 [0.023, −0.77] | 0.6 [−0.3, 0.2] | <0.001 * [−2.5, −2.1] | ||||
| HRA Left | CBP G | 3.8 ± 1.4 | 2.2 ± 1.4 | .4 ± 1.1 | <0.001* F = 20.3 Partial Eta squared = 0.2 | <0.001* F = 184 Partial Eta squared = 0.8 | <0.001* F = 208 Partial Eta squared = 0.8 |
| Standard G | 3.2 ± 0.9 | 2.5 ± 1.6 | 2.9 ± 1.2 | ||||
| p-Value C.I. | 0.07 [0.02, −1.1] | 0.3 [−0.6, 0.07] | <0.001 * [−2.8, −2.1] | ||||
| Baseline | 6-Weeks | 3-Month Follow-Up | p-Value | ||||
|---|---|---|---|---|---|---|---|
| G | T | G vs. T | |||||
| CROM lateral flexion right | CBP G | 36.9 ± 2.8 | 42.4 ± 2 | 42.1 ± 2.2 | <0.001 * F = 44.2 Partial Eta squared = 0.5 | <0.001 * F = 132 Partial Eta squared = 0.6 | <0.001 * F = 44.9 Partial Eta squared = 0.5 |
| Standard G | 37.2 ± 2 | 40.6 ± 3 | 37.4 ± 3.8 | ||||
| p-Value C.I. | 0.5 [−0.9, 1.3] | <0.008 * [0.5, 3.1] | <0.001 * [3.6, 5.7] | ||||
| CROM lateral flexion left | CBP G | 37.5 ± 2.3 | 42.6 ± 1.8 | 42.2 ± 2.6 | <0.001 * F = 23 Partial Eta squared = 0.3 | <0.001 * F = 104 Partial ETA squared = 0.7 | <0.001 * F = 40 Partial Eta squared = 0.5 |
| Standard G | 37.1 ± 2.7 | 40.1 ± 2.6 | 37.8 ± 2.5 | ||||
| p-Value C.I. | 0.4 [−0.6, 1.4] | <0.001 * [0.8, 3.1] | <0.001 * [3.3, 5.4] | ||||
| CROM rotation right | CBP G | 61.1 ± 5.3 | 71.40 ± 2.3 | 70.8 ± 4 | <0.001 * F = 24 Partial Eta squared = 0.2 | <0.001 * F = 150 Partial Eta squared = 0.8 | <0.001 * F = 72 Partial Eta squared = 0.7 |
| Standard G | 62.3 ± 5.6 | 63.6 ± 4.8 | 62 ± 6.1 | ||||
| p-Value C.I. | 0.1 [−2.8, 2.5] | <0.001 * [5.8, 9.6] | <0.001 * [6.4, 11.2] | ||||
| CROM rotation left | CBP G | 62.15 ± 4.5 | 70.7 ± 3.9 | 70 ± 5.7 | <0.001 * F = 24.6 Partial Eta squared = 0.3 | F = 73 Partial Eta squared = 0.7 | F = 46 Partial Eta squared = 0.6 |
| Standard G | 60.9 ± 6.4 | 63.4 ± 4.5 | 61.2 ± 6.7 | ||||
| p-Value C.I. | 0.3 [−1.4, 4.2] | <0.001 * [5.2, 9.1] | <0.001 * [6, 11.4] | ||||
| Correlation between Variables | ∆ CVA CBP Group r (p Value) n = 33 | ∆ CVA Standard Group r (p Value) n = 33 |
|---|---|---|
| ∆Pain intensity | −0.7 (<0.001) | −0.67 (<0.001) |
| ∆Berg Balance Score | 0.64 (<0.001) | 0.49 (<0.001) |
| ∆ Head repositioning accuracy (Right) | −0.69 (<0.001) | −0.71 (<0.001) |
| ∆ Head repositioning accuracy (Left) | −0.72 (<0.001) | −0.72 (<0.001) |
| ∆ CROM lateral flexion Right | 0.49 (<0.001) | 0.61 (<0.001) |
| ∆ CROM lateral flexion Left | 0.57 (<0.001) | 0.52 (<0.001) |
| ∆ CROM rotation right | 0.49 (<0.001) | 0.61 (<0.001) |
| ∆ CROM rotation left | 0.57 (<0.001) | 0.52 (<0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suwaidi, A.S.A.; Moustafa, I.M.; Kim, M.; Oakley, P.A.; Harrison, D.E. A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. J. Clin. Med. 2023, 12, 542. https://doi.org/10.3390/jcm12020542
Suwaidi ASA, Moustafa IM, Kim M, Oakley PA, Harrison DE. A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. Journal of Clinical Medicine. 2023; 12(2):542. https://doi.org/10.3390/jcm12020542
Chicago/Turabian StyleSuwaidi, Aisha Salim Al, Ibrahim M. Moustafa, Meeyoung Kim, Paul A. Oakley, and Deed E. Harrison. 2023. "A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study" Journal of Clinical Medicine 12, no. 2: 542. https://doi.org/10.3390/jcm12020542
APA StyleSuwaidi, A. S. A., Moustafa, I. M., Kim, M., Oakley, P. A., & Harrison, D. E. (2023). A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. Journal of Clinical Medicine, 12(2), 542. https://doi.org/10.3390/jcm12020542








