The Feasibility and Safety of Endoscopic Submucosal Dissection for Circumferential Superficial Esophageal Squamous Cell Neoplasms
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Evaluation Parameter
2.3. Operation Procedure
2.4. Postoperative Management and Follow-Up
2.5. Statistical Analysis
3. Results
3.1. Patients and Clinicopathological Features
3.2. Preoperative Endoscopic Ultrasonography (EUS) Findings
3.3. The Relationship between Clinicopathological Data and Depth of Invasion/Angiolymphatic Invasion
3.4. Comparison of Clinicopathological Characteristics between the ESD and Surgery Groups
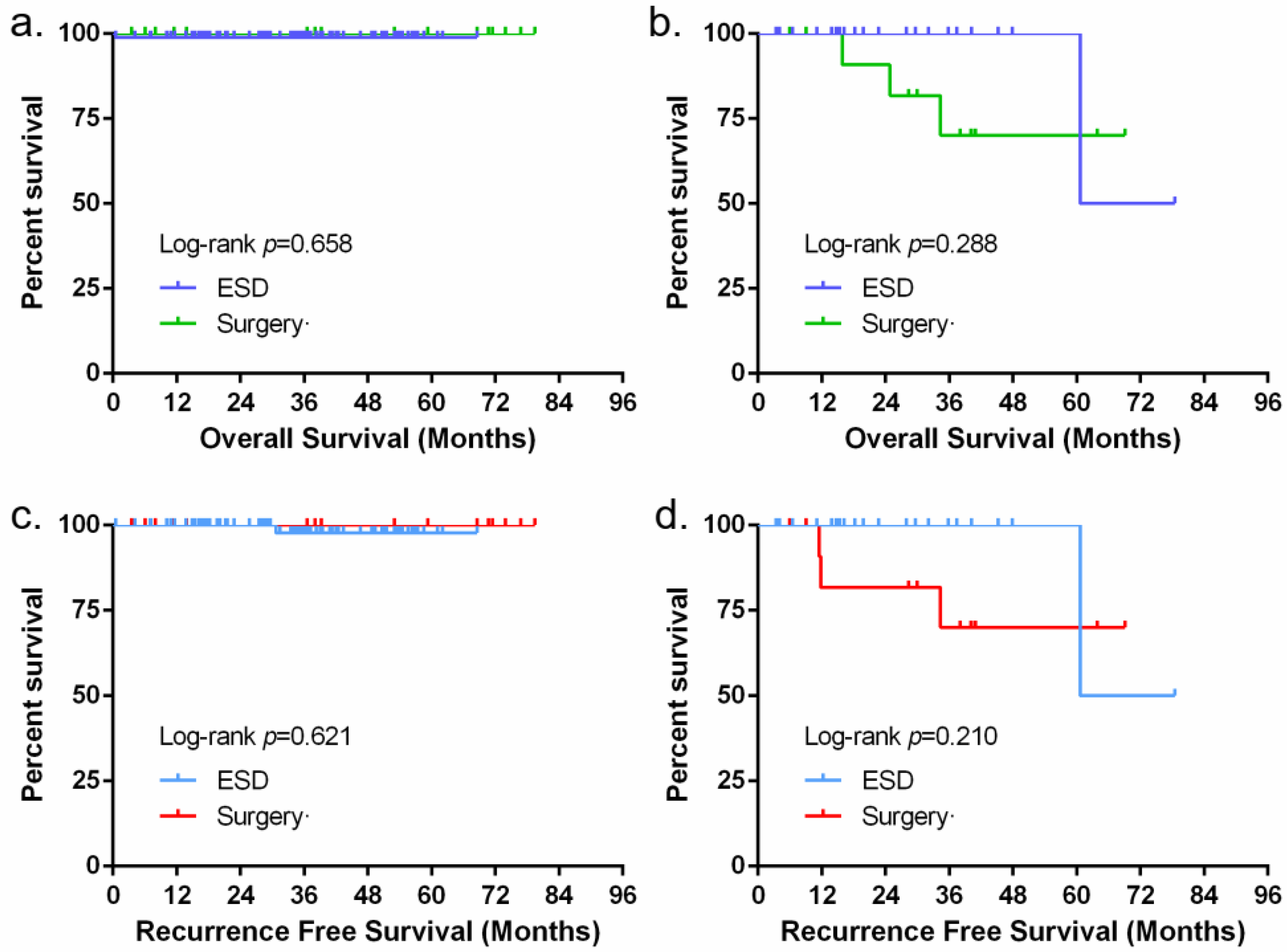
3.5. The Short-Term Outcomes and Long-Term Outcomes of ESD and Surgery
3.6. Comparison of the QOL Scores between ESD and Surgery
3.7. The Effect of Different Methods to Prevent Esophageal Stenosis after ESD
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zheng, R.; Zhang, S.; Zeng, H.; Wang, S.; Sun, K.; Chen, R.; Li, L.; Wei, W.; He, J. Cancer incidence and mortality in China, 2016. J. Natl. Cancer Cent. 2022, 2, 1–9. [Google Scholar] [CrossRef]
- Li, P.; Wang, Y.J.; Chen, G.Y.; Xu, C.Q. Chinese consensus: Screening, diagnosis and treatment of early esophageal squamous cell carcinoma and precancerous lesions. Chin. J. Intern. Med. 2016, 55, 73–85. [Google Scholar] [CrossRef]
- Nagami, Y.; Ominami, M.; Shiba, M.; Minamino, H.; Fukunaga, S.; Kameda, N.; Sugimori, S.; Machida, H.; Tanigawa, T.; Yamagami, H.; et al. The five-year survival rate after endoscopic submucosal dissection for superficial esophageal squamous cell neoplasia. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2017, 49, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, R.; Arima, M.; Iizuka, T.; Oyama, T.; Katada, C.; Kato, M.; Goda, K.; Goto, O.; Tanaka, K.; Yano, T.; et al. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2020, 32, 452–493. [Google Scholar] [CrossRef]
- Ishihara, R. Prevention of esophageal stricture after endoscopic resection. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2019, 31, 134–145. [Google Scholar] [CrossRef]
- Sakaguchi, Y.; Tsuji, Y.; Fujishiro, M.; Kataoka, Y.; Takeuchi, C.; Yakabi, S.; Saito, I.; Shichijo, S.; Minatsuki, C.; Asada-Hirayama, I.; et al. Triamcinolone injection and shielding with polyglycolic acid sheets and fibrin glue for postoperative stricture prevention after esophageal endoscopic resection: A pilot study. Am. J. Gastroenterol. 2016, 111, 581–583. [Google Scholar] [CrossRef]
- Shi, K.D.; Ji, F. Prophylactic stenting for esophageal stricture prevention after endoscopic submucosal dissection. World J. Gastroenterol. 2017, 23, 931–934. [Google Scholar] [CrossRef]
- Chai, N.; Zou, J.; Linghu, E.; Chai, M.; Li, L.; Wang, X.; Zhang, W.; Xiang, J.; Li, Z. Autologous skin-grafting surgery to prevent esophageal stenosis after complete circular endoscopic submucosal tunnel dissection for superficial esophageal neoplasms. Am. J. Gastroenterol. 2019, 114, 822–825. [Google Scholar] [CrossRef]
- Yu, J.P.; Liu, Y.J.; Tao, Y.L.; Ruan, R.W.; Cui, Z.; Zhu, S.W.; Shi, W. Prevention of esophageal stricture after endoscopic submucosal dissection: A systematic review. World J. Surg. 2015, 39, 2955–2964. [Google Scholar] [CrossRef]
- Iizuka, H.; Kakizaki, S.; Sohara, N.; Onozato, Y.; Ishihara, H.; Okamura, S.; Itoh, H.; Mori, M. Stricture after endoscopic submucosal dissection for early gastric cancers and adenomas. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2010, 22, 282–288. [Google Scholar] [CrossRef]
- Toyokawa, T.; Inaba, T.; Omote, S.; Okamoto, A.; Miyasaka, R.; Watanabe, K.; Izumikawa, K.; Horii, J.; Fujita, I.; Ishikawa, S.; et al. Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: Analysis of 1123 lesions. J. Gastroenterol. Hepatol. 2012, 27, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Jia, R.; Luan, Q.; Wang, J.; Hou, D.; Zhao, S. Analysis of predictors for lymph node metastasis in patients with superficial esophageal carcinoma. Gastroenterol. Res. Pract. 2016, 2016, 3797615. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, T.; Hiyama, T.; Oka, S.; Yorita, N.; Kuroki, K.; Kurihara, M.; Yoshifuku, Y.; Sanomura, Y.; Urabe, Y.; Murakami, Y.; et al. Curative criteria after endoscopic resection for superficial esophageal squamous cell carcinomas. Dig. Dis. Sci. 2018, 63, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Axon, A.; Diebold, M.D.; Fujino, M.; Fujita, R.; Genta, R.M.; Gonvers, J.J.; Guelrud, M.; Inoue, H.; Jung, M.; Kashida, H.; et al. Update on the paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy 2005, 37, 570–578. [Google Scholar] [CrossRef]
- Inoue, H.; Kaga, M.; Ikeda, H.; Sato, C.; Sato, H.; Minam, H.; Santi, E.G.; Hayee, B.H.; Eleftheriadis, N. Magnification endoscopy in esophageal squamous cell carcinoma: A review of the intrapapillary capillary loop classification. Ann. Gastroenterol. 2015, 28, 41–48. [Google Scholar]
- Oyama, T.; Ishihara, R.; Takeuchi, M.; Hirasawa, D.; Arima, M.; Inoue, H.; Goda, K.; Tomori, A.; Momma, K. Usefulness of Japan esophageal society classification of magnified endoscopy for the diagnosis of superficial esophageal squamous cell carcinoma. Gastrointest. Endosc. 2012, 75, AB456. [Google Scholar] [CrossRef]
- Hisano, O.; Nonoshita, T.; Hirata, H.; Sasaki, T.; Watanabe, H.; Wakiyama, H.; Ono, M.; Ohga, S.; Honda, H. Additional radiotherapy following endoscopic submucosal dissection for T1a-MM/T1b-SM esophageal squamous cell carcinoma improves locoregional control. Radiat. Oncol. 2018, 13, 1–7. [Google Scholar] [CrossRef]
- Yoshii, T.; Ohkawa, S.; Tamai, S.; Kameda, Y. Clinical outcome of endoscopic mucosal resection for esophageal squamous cell cancer invading muscularis mucosa and submucosal layer. Dis. Esophagus Off. J. Int. Soc. Dis. Esophagus 2013, 26, 496–502. [Google Scholar] [CrossRef]
- Saeki, H.; Watanabe, M.; Mine, S.; Shigaki, H.; Oya, S.; Ishiyama, A.; Tsuchida, T.; Fujisaki, J.; Baba, H.; Maehara, Y.; et al. Esophagectomy for superficial esophageal cancer after non-curative endoscopic resection. J. Gastroenterol. 2015, 50, 406–413. [Google Scholar] [CrossRef]
- Yamashina, T.; Ishihara, R.; Nagai, K.; Matsuura, N.; Matsui, F.; Ito, T.; Fujii, M.; Yamamoto, S.; Hanaoka, N.; Takeuchi, Y.; et al. Long-term outcome and metastatic risk after endoscopic resection of superficial esophageal squamous cell carcinoma. Am. J. Gastroenterol. 2013, 108, 544–551. [Google Scholar] [CrossRef]
- Takahashi, K.; Hashimoto, S.; Mizuno, K.I.; Kobayashi, T.; Tominaga, K.; Sato, H.; Kohisa, J.; Ikarashi, S.; Hayashi, K.; Takeuchi, M.; et al. Management decision based on lymphovascular involvement leads to favorable outcomes after endoscopic treatment of esophageal squamous cell carcinoma. Endoscopy 2018, 50, 662–670. [Google Scholar] [CrossRef]
- Jung, J.I. Clinicopathologic factors influencing the accuracy of EUS for superficial esophageal carcinoma. World J. Gastroenterol. 2014, 20, 6322. [Google Scholar] [CrossRef]
- Rice, T.W.; Boyce, G.A.; Sivak, M.V.; Loop, F.D. Esophageal ultrasound and the preoperative staging of carcinoma of the esophagus. J. Thorac. Cardiovasc. Surg. 1991, 101, 536–543. [Google Scholar] [CrossRef]
- Kadota, T.; Minashi, K.; Wakabayashi, M.; Yano, T.; Ezoe, Y.; Tsuchida, T.; Ono, H.; Iizuka, T.; Matsuura, N.; Oda, I.; et al. Diagnostic yield of conventional endoscopy with endoscopic ultrasonography for submucosal invasion of superficial esophageal squamous cell carcinoma: A post hoc analysis of multicenter prospective confirmatory study (JCOG0508). Esophagus Off. J. Jpn. Esophageal Soc. 2021, 18, 604–611. [Google Scholar] [CrossRef]
- Ishihara, R.; Matsuura, N.; Hanaoka, N.; Yamamoto, S.; Akasaka, T.; Takeuchi, Y.; Higashino, K.; Uedo, N.; Iishi, H. Endoscopic imaging modalities for diagnosing invasion depth of superficial esophageal squamous cell carcinoma: A systematic review and meta-analysis. BMC Gastroenterol. 2017, 17, 24. [Google Scholar] [CrossRef]
- Santi, E.; Inoue, H.; Ikeda, H.; Yoshida, A.; Onimaru, M.; Sato, H.; Maselli, R.; Hayee, B.; Kudo, S. Microvascular caliber changes in intramucosal and submucosally invasive esophageal cancer. Endoscopy 2013, 45, 585–588. [Google Scholar] [CrossRef]
- Oyama, T.; Inoue, H.; Arima, M.; Momma, K.; Omori, T.; Ishihara, R.; Hirasawa, D.; Takeuchi, M.; Tomori, A.; Goda, K. Prediction of the invasion depth of superficial squamous cell carcinoma based on microvessel morphology: Magnifying endoscopic classification of the Japan Esophageal Society. Esophagus Off. J. Jpn. Esophageal Soc. 2017, 14, 105–112. [Google Scholar] [CrossRef]
- Huh, C.W.; Jung, D.H.; Kim, J.H.; Ma, D.W.; Youn, Y.H.; Park, H. Clinical implication of endoscopic gross appearance in superficial esophageal squamous carcinoma: Revisited. Surg. Endosc. 2018, 32, 367–375. [Google Scholar] [CrossRef]
- Ebi, M.; Shimura, T.; Yamada, T.; Mizushima, T.; Itoh, K.; Tsukamoto, H.; Tsuchida, K.; Hirata, Y.; Murakami, K.; Kanie, H.; et al. Multicenter, prospective trial of white-light imaging alone versus white-light imaging followed by magnifying endoscopy with narrow-band imaging for the real-time imaging and diagnosis of invasion depth in superficial esophageal squamous cell carcinoma. Gastrointest. Endosc. 2015, 81, 1355–1361.e2. [Google Scholar] [CrossRef]
- Ma, D.W.; Jung, D.H.; Kim, J.H.; Park, J.J.; Youn, Y.H.; Park, H. Predicting lymph node metastasis for endoscopic resection of superficial esophageal squamous cell carcinoma. J. Thorac. Cardiovasc. Surg. 2019, 157, 397–402.e1. [Google Scholar] [CrossRef]
- Min, B.H.; Yang, J.W.; Min, Y.W.; Baek, S.Y.; Kim, S.; Kim, H.K.; Choi, Y.S.; Shim, Y.M.; Choi, Y.L.; Zo, J.I. Nomogram for prediction of lymph node metastasis in patients with superficial esophageal squamous cell carcinoma. J. Gastroenterol. Hepatol. 2020, 35, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Liu, X.B.; Li, S.B.; Yang, Z.H.; Tong, Q. Prediction of lymph node metastasis in superficial esophageal squamous cell carcinoma in Asia: A systematic review and meta-analysis. Dis. Esophagus Off. J. Int. Soc. Dis. Esophagus 2020, 33, doaa032. [Google Scholar] [CrossRef] [PubMed]
- Ruan, R.; Chen, S.; Tao, Y.; Yu, J.; Zhou, D.; Cui, Z.; Shen, Q.; Wang, S. Retrospective analysis of predictive factors for lymph node metastasis in superficial esophageal squamous cell carcinoma. Sci. Rep. 2021, 11, 16544. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Luo, J.H.; Chen, L. An analysis of vascular tumor embolus: A risk factor for the esophageal carcinoma. Acta Univ. Med. Nanjing Nat. Sci. 2016, 36, 470–472, 494. [Google Scholar] [CrossRef]
- Aadam, A.A.; Abe, S. Endoscopic submucosal dissection for superficial esophageal cancer. Dis. Esophagus Off. J. Int. Soc. Dis. Esophagus 2018, 31, doy021. [Google Scholar] [CrossRef]
- Fujishiro, M. Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J. Gastroenterol. 2008, 14, 4289–4295. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Ding, X. Progress on the prevention of esophageal stricture after endoscopic submucosal dissection. Gastroenterol. Res. Pract. 2018, 2018, 1696849. [Google Scholar] [CrossRef]


| Clinical and Histopathologic Characteristics | Depth of Invasion | Univariate Logistic Regression | Multivariate Logistic Regression | |||
|---|---|---|---|---|---|---|
| EP/LPM/MM/SM (<200 μm) | SM (≥200 μm) | OR (95% CI) | p | OR (95% CI) | p | |
| Age, mean ± SD, years | 63.4 ± 7.73 | 60.9 ± 6.79 | 0.957 (0.909–1.008) | 0.099 | ||
| Sex | ||||||
| Female | 38 | 7 | 1 | |||
| Male | 66 | 29 | 2.385 (0.954–5.966) | 0.063 | ||
| Smoking history | 40 | 24 | 3.200 (1.441–7.105) | 0.004 | ||
| Drinking history | 42 | 25 | 3.355 (1.492–7.543) | 0.003 | 3.142 (1.161–8.503) | 0.024 |
| Family history of cancer | 22 | 15 | 2.372 (1.046–5.379) | 0.039 | 3.029 (1.086–8.446) | 0.034 |
| Complicated with early laryngeal tumour | 6 | 4 | 2.552 (0.730–8.926) | 0.142 | ||
| Lesion location | ||||||
| Upper | 9 | 2 | 0.323 (0.064–1.642) | 0.173 | ||
| Upper-Middle | 18 | 6 | 0.485 (0.166–1.416) | 0.185 | ||
| Middle | 38 | 3 | 0.115 (0.031–0.419) | 0.001 | ||
| Middle-Lower | 32 | 22 | 1 | |||
| Lower | 7 | 3 | 0.623 (0.145–2.677) | 0.525 | ||
| Longitudinal diameter, mm | ||||||
| ≤50 | 32 | 8 | 1.556 (0.639–3.785) | 0.330 | ||
| >50 | 72 | 28 | ||||
| Macroscopic type | ||||||
| 0-IIa | 23 | 20 | 4.348 (1.945–9.720) | <0.001 | ||
| 0-IIb | 80 | 16 | 1 | |||
| 0-IIc | 1 | 0 | 0 (0–∞) | 1.000 | ||
| WLE | ||||||
| Hyperkeratosis present | 34 | 16 | 1.647 (0.759–3.574) | 0.207 | ||
| Red mucosa | 84 | 34 | 4.048 (0.897–18.270) | 0.069 | ||
| Slightly elevated/depressed | 24 | 20 | 4.167 (1.872–9.274) | <0.001 | 3.164 (1.201–8.337) | 0.020 |
| ME-NBI | ||||||
| IPCL (JES classification) | ||||||
| B1 | 74 | 7 | 1 | 1 | ||
| B2/B3 | 30 | 29 | 10.219 (4.040–25.849) | <0.001 | 10.667 (3.867–29.429) | <0.001 |
| Avascular (AVA) present | 30 | 14 | 1.570 (0.710–3.469) | 0.265 | ||
| Degree of differentiation | ||||||
| Well differentiated | 1 | 1 | 2.952 (0.177–49.316) | 0.451 | ||
| Moderately differentiated | 62 | 21 | 1 | |||
| Poorly differentiated | 16 | 12 | 2.214 (0.903–5.431) | 0.082 | ||
| Basaloid | 3 | 2 | 1.968 (0.308–12.598) | 0.475 | ||
| Clinical and Histopathologic Characteristics | Angiolymphatic Invasion | Univariate Logistic Regression | Multivariate Logistic Regression | |||
|---|---|---|---|---|---|---|
| Absent (−) | Present (+) | OR (95% CI) | p | OR (95% CI) | p | |
| Age, mean ± SD, years | 62.9 ± 7.59 | 62.1 ± 7.46 | 0.987 (0.930–1.048) | 0.670 | ||
| Sex | ||||||
| Female | 41 | 4 | 1 | |||
| Male | 76 | 19 | 2.562 (0.817–8.038) | 0.107 | ||
| Smoking history | 47 | 17 | 4.220 (1.550–11.487) | 0.005 | 3.385 (1.197–9.571) | 0.021 |
| Drinking history | 50 | 17 | 3.797 (1.396–10.322) | 0.009 | ||
| Family history of cancer | 32 | 4 | 0.559 (0.177–1.770) | 0.323 | ||
| Complicated with early laryngeal tumour | 5 | 5 | 6.222 (1.636–23.663) | 0.007 | ||
| Lesion location | ||||||
| Upper | 10 | 1 | 0.440 (0.050–3.843) | 0.458 | ||
| Upper-Middle | 19 | 5 | 0.811 (0.348–3.847) | 0.811 | ||
| Middle | 36 | 5 | 0.611 (0.192–1.950) | 0.406 | ||
| Middle-Lower | 44 | 10 | 1 | |||
| Lower | 8 | 2 | 1.100 (0.202–5.990) | 0.912 | ||
| Longitudinal diameter, mm | ||||||
| ≤50 | 31 | 9 | 0.561 (0.221–1.425) | 0.224 | ||
| >50 | 86 | 14 | ||||
| Macroscopic type | ||||||
| 0-IIa | 31 | 12 | 2.991 (1.197–7.473) | 0.019 | ||
| 0-IIb | 85 | 11 | 1 | |||
| 0-IIc | 1 | 0 | 0 (0–∞) | 1.000 | ||
| WLE | ||||||
| Hyperkeratosis present | 43 | 7 | 0.753 (0.287–1.975) | 0.564 | ||
| Red mucosa | 97 | 21 | 2.165 (0.470–9.980) | 0.322 | ||
| Slightly elevated/depressed | 32 | 12 | 2.898 (1.162–7.225) | 0.022 | ||
| ME-NBI | ||||||
| IPCL (JES classification) | ||||||
| B1 | 74 | 7 | 1 | 1 | ||
| B2/B3 | 43 | 16 | 3.934 (1.499–10.319) | 0.005 | 2.864 (1.035–7.923) | 0.043 |
| Avascular (AVA) present | 37 | 7 | 0.946 (0.359–2.495) | 0.911 | ||
| Degree of differentiation | ||||||
| Well differentiated | 2 | 0 | 0 (0–∞) | 0.999 | ||
| Moderately differentiated | 68 | 15 | 1 | |||
| Poorly differentiated | 21 | 7 | 1.511 (0.544–4.199) | 0.428 | ||
| Basaloid | 4 | 1 | 1.133 (0.118–10.877) | 0.914 | ||
| Depth of invasion | ||||||
| EP/LPM/MM/SM(<200 μm) | 96 | 8 | 1 | |||
| SM(≥200 μm) | 21 | 15 | 8.571 (3.219–22.824) | <0.001 | ||
| Clinicopathological Characteristics | Treatment | χ2 | p | |
|---|---|---|---|---|
| ESD | Surgery | |||
| Age, mean ± SD, years | 63.1 ± 7.75 | 61.7 ± 6.79 | 0.361 | |
| Sex | 1.669 | 0.196 | ||
| Male | 71 | 24 | ||
| Female | 38 | 7 | ||
| BMI, mean ± SD, kg/m2 | 22.9 ± 3.39 | 23.2 ± 3.21 | 0.655 | |
| Lesion location | - | 0.179 | ||
| Upper | 10 | 1 | ||
| Upper-Middle | 22 | 2 | ||
| Middle | 32 | 9 | ||
| Middle-Lower | 37 | 17 | ||
| Lower | 8 | 2 | ||
| Longitudinal diameter, mm | ||||
| Median (P25, P75) | 70 (50, 90) | 70 (50, 90) | 0.520 | |
| Macroscopic type | - | 0.362 | ||
| 0-IIa | 30 | 13 | ||
| 0-IIb | 78 | 18 | ||
| 0-IIc | 1 | 0 | ||
| Degree of differentiation | - | 0.814 | ||
| Well differentiated | 2 | 0 | ||
| Moderately differentiated | 63 | 20 | ||
| Poorly differentiated | 19 | 9 | ||
| Basaloid | 4 | 1 | ||
| Depth of invasion | 7.883 | 0.005 | ||
| EP/LPM/MM/SM(<200 μm) | 87 | 17 | ||
| SM(≥200 μm) | 22 | 14 | ||
| Angiolymphatic invasion present | 17 | 5 | - | 1.000 |
| Treatment | p | ||
|---|---|---|---|
| ESD | Surgery | ||
| Total | 109 | 31 | |
| En bloc resection | 109 (100.0%) | - | |
| Complete resection | 108 (99.1%) | - | |
| Operative time | |||
| mean ± SD, minutes | 174.5 ± 51.16 | 255.9 ± 88.18 | <0.001 |
| Perioperative complications | 6 (5.5%) | 6 (19.4%) | 0.015 |
| Delayed bleeding | 3 | 0 | |
| Immediate/Delayed Perforation | 3 | - | |
| Anastomotic fistula | - | 1 | |
| Wound infection | - | 5 | |
| Esophageal scar stenosis | 84 (77.1%) | - | |
| Anastomotic stricture | - | 4 (12.9%) | |
| Duration of follow-up (months) | |||
| Median | 29.7 | 39.3 | |
| Range | 3.38–78.52 | 3.75–79.51 | |
| Further treatment | |||
| Radiotherapy | 8 | - | |
| Surgery | 3 | - | |
| Recurrence | 2 | 3 | |
| Mortality | 2 | 3 | |
| ESD (n = 107) | Surgery (n = 28) | p | |
|---|---|---|---|
| EORTC-QLQ-C30 Functional scales | |||
| Physical functioning | 99.8 ± 1.11 | 99.5 ± 1.75 | 0.283 |
| Role functioning | 100.0 ± 0.00 | 100.0 ± 0.00 | - |
| Emotional functioning | 99.8 ± 1.13 | 94.6 ± 10.46 | 0.014 |
| Cognitive functioning | 99.7 ± 2.27 | 96.4 ± 6.96 | 0.021 |
| Social functioning | 100.00 ± 0.00 | 100.00 ± 0.00 | - |
| Global health status | 85.3 ± 1.92 | 78.1 ± 9.10 | <0.001 |
| EORTC-QLQ-C30 Symptom scales | |||
| Fatigue | 0.0 ± 0.00 | 0.4 ± 2.10 | 0.326 |
| Nausea and vomiting | 0.2 ± 1.61 | 0.0 ± 0.00 | 0.611 |
| Pain | 0.0 ± 0.00 | 14.3 ± 18.54 | <0.001 |
| Dyspnoea | 0.3 ± 3.22 | 13.1 ± 18.90 | 0.001 |
| Insomnia | 0.0 ± 0.00 | 20.2 ± 24.58 | <0.001 |
| Appetite loss | 0.0 ± 0.00 | 11.9 ± 20.72 | 0.005 |
| Constipation | 0.6 ± 4.55 | 3.6 ± 13.88 | 0.277 |
| Diarrhoea | 0.3 ± 3.22 | 17.9 ± 24.82 | 0.001 |
| Financial difficulties | 0.0 ± 0.00 | 0.0 ± 0.00 | - |
| EORTC-QLQ-OES18 Symptom scales | |||
| Dysphagia | 96.3 ± 6.09 | 95.6 ± 9.72 | 0.673 |
| Eating difficulties | 1.7 ± 4.24 | 0.9 ± 4.72 | 0.375 |
| Reflux | 3.1 ± 8.30 | 17.9 ± 22.19 | 0.002 |
| Esophageal pain | 0.4 ± 2.12 | 6.7 ± 8.73 | 0.001 |
| Trouble swallowing saliva | 0.0 ± 0.00 | 0.0 ± 0.00 | - |
| Choking when swallowing | 8.1 ± 15.08 | 3.6 ± 10.50 | 0.071 |
| Dry mouth | 0.0 ± 0.00 | 0.0 ± 0.00 | - |
| Trouble with taste | 2.2 ± 8.28 | 26.2 ± 31.89 | <0.001 |
| Trouble with coughing | 0.0 ± 0.00 | 0.0 ± 0.00 | - |
| Speech difficulties | 0.3 ± 3.22 | 0.0 ± 0.00 | 0.611 |
| Repeated EBD | PGA with AEM | PGA with TSI | PGA with AEM and TSI | PGA with AEM and SSWB | |
|---|---|---|---|---|---|
| Stenosis | |||||
| No | 0 | 0 | 1 | 20 | 4 |
| Yes | 50 (100.0%) | 2 (100.0%) | 4 (80.0%) | 23 (53.5%) | 5 (55.6%) |
| Balloon dilatation | |||||
| mean ± SD | 10.8 ± 8.28 | 14.5 ± 3.54 | 4.6 ± 4.16 | 2.9 ± 4.05 | 3.1 ± 3.52 |
| p | 0.539 | 0.104 | <0.001 | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Dou, L.; Rao, W.; Liu, Y.; Zhang, Y.; He, S.; Xue, L.; Wang, G. The Feasibility and Safety of Endoscopic Submucosal Dissection for Circumferential Superficial Esophageal Squamous Cell Neoplasms. J. Clin. Med. 2023, 12, 471. https://doi.org/10.3390/jcm12020471
Liu Y, Dou L, Rao W, Liu Y, Zhang Y, He S, Xue L, Wang G. The Feasibility and Safety of Endoscopic Submucosal Dissection for Circumferential Superficial Esophageal Squamous Cell Neoplasms. Journal of Clinical Medicine. 2023; 12(2):471. https://doi.org/10.3390/jcm12020471
Chicago/Turabian StyleLiu, Yi, Lizhou Dou, Wei Rao, Yong Liu, Yueming Zhang, Shun He, Liyan Xue, and Guiqi Wang. 2023. "The Feasibility and Safety of Endoscopic Submucosal Dissection for Circumferential Superficial Esophageal Squamous Cell Neoplasms" Journal of Clinical Medicine 12, no. 2: 471. https://doi.org/10.3390/jcm12020471
APA StyleLiu, Y., Dou, L., Rao, W., Liu, Y., Zhang, Y., He, S., Xue, L., & Wang, G. (2023). The Feasibility and Safety of Endoscopic Submucosal Dissection for Circumferential Superficial Esophageal Squamous Cell Neoplasms. Journal of Clinical Medicine, 12(2), 471. https://doi.org/10.3390/jcm12020471






