Horner’s Syndrome and Lymphocele Following Thyroid Surgery
Abstract
1. Introduction
Aim
2. Methods
3. Thyroid Conditions and HS and Lymphocele/Chylous Leakage
3.1. Thyroid Disorders and HS: From Goiter to Iatrogen Elements
3.1.1. Thyroid Aspects Causing HS
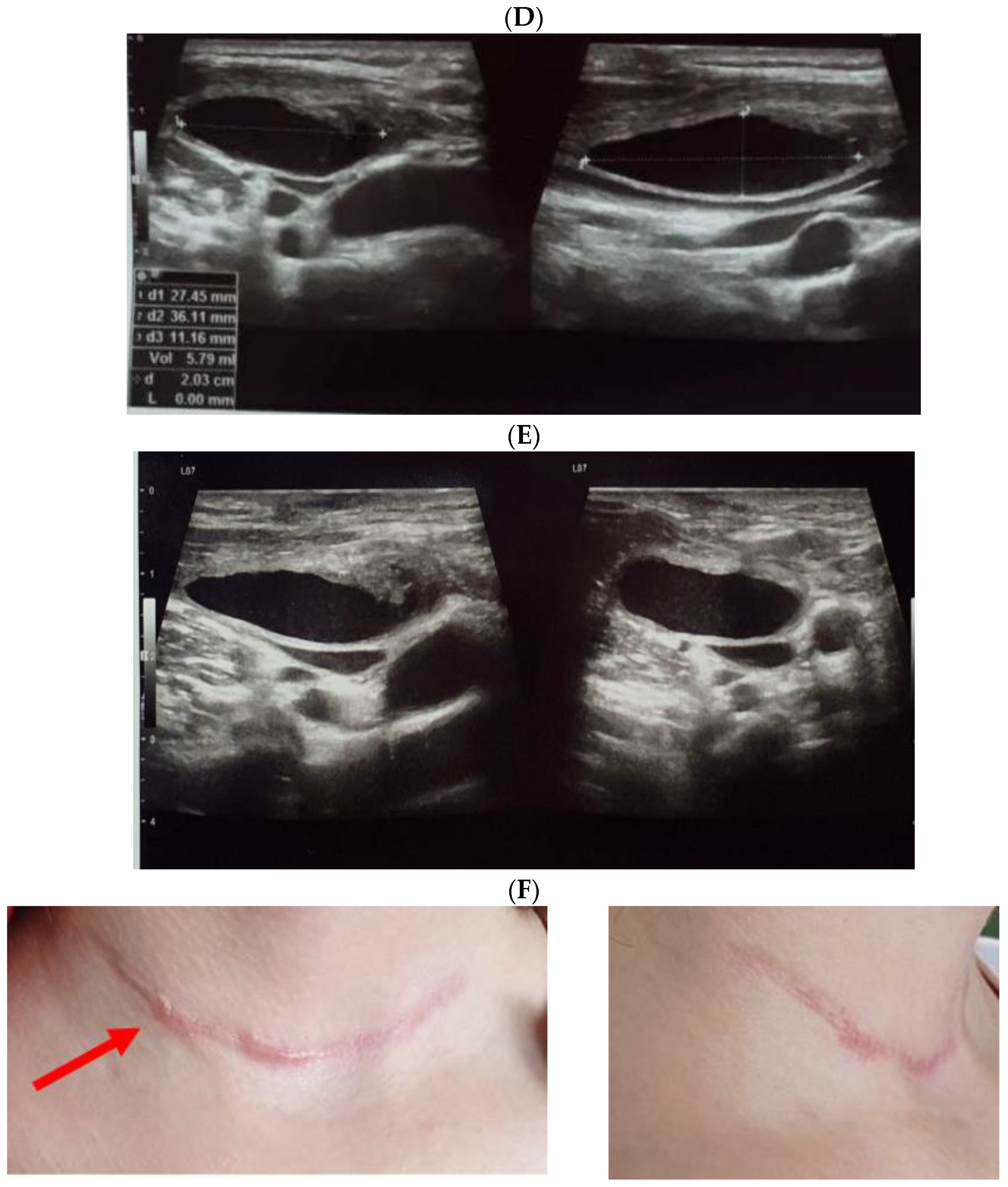
3.1.2. Thyroid Surgery Followed by HS
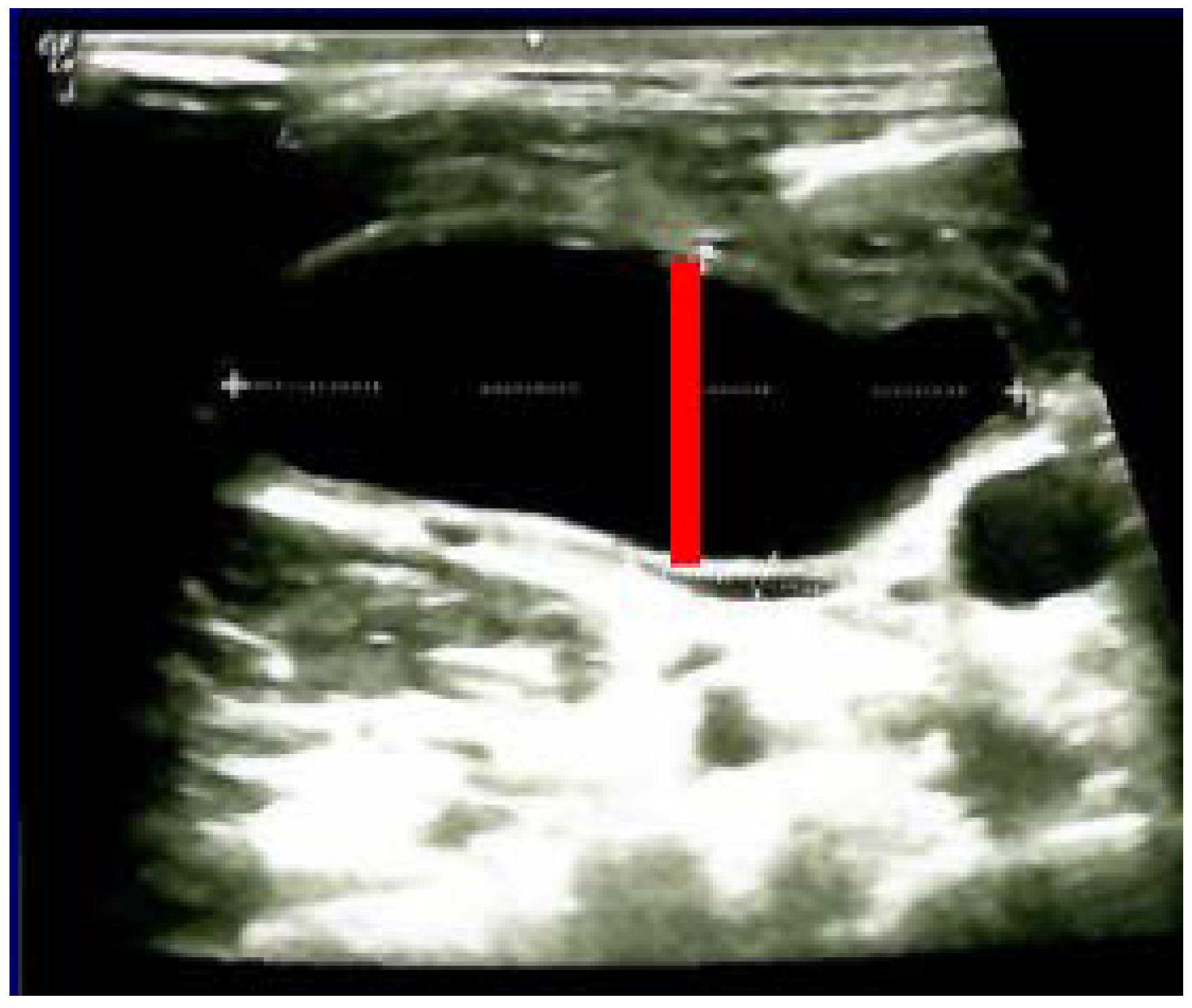
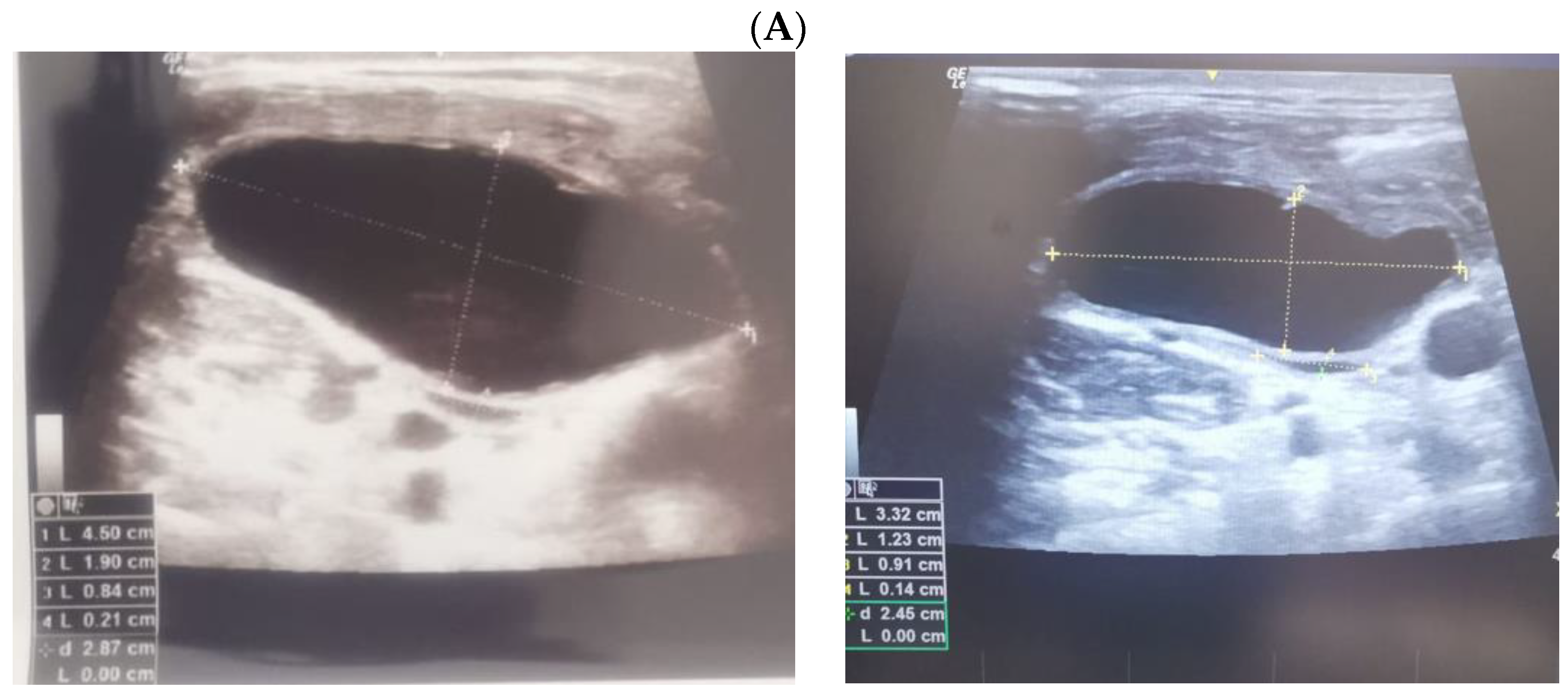
3.2. Thyroidectomy/Lymph Nodes Dissection and Lymphocele/Chylous Leakage
3.3. Post-Thyroidectomy HS and Lymphocele
4. Discussion
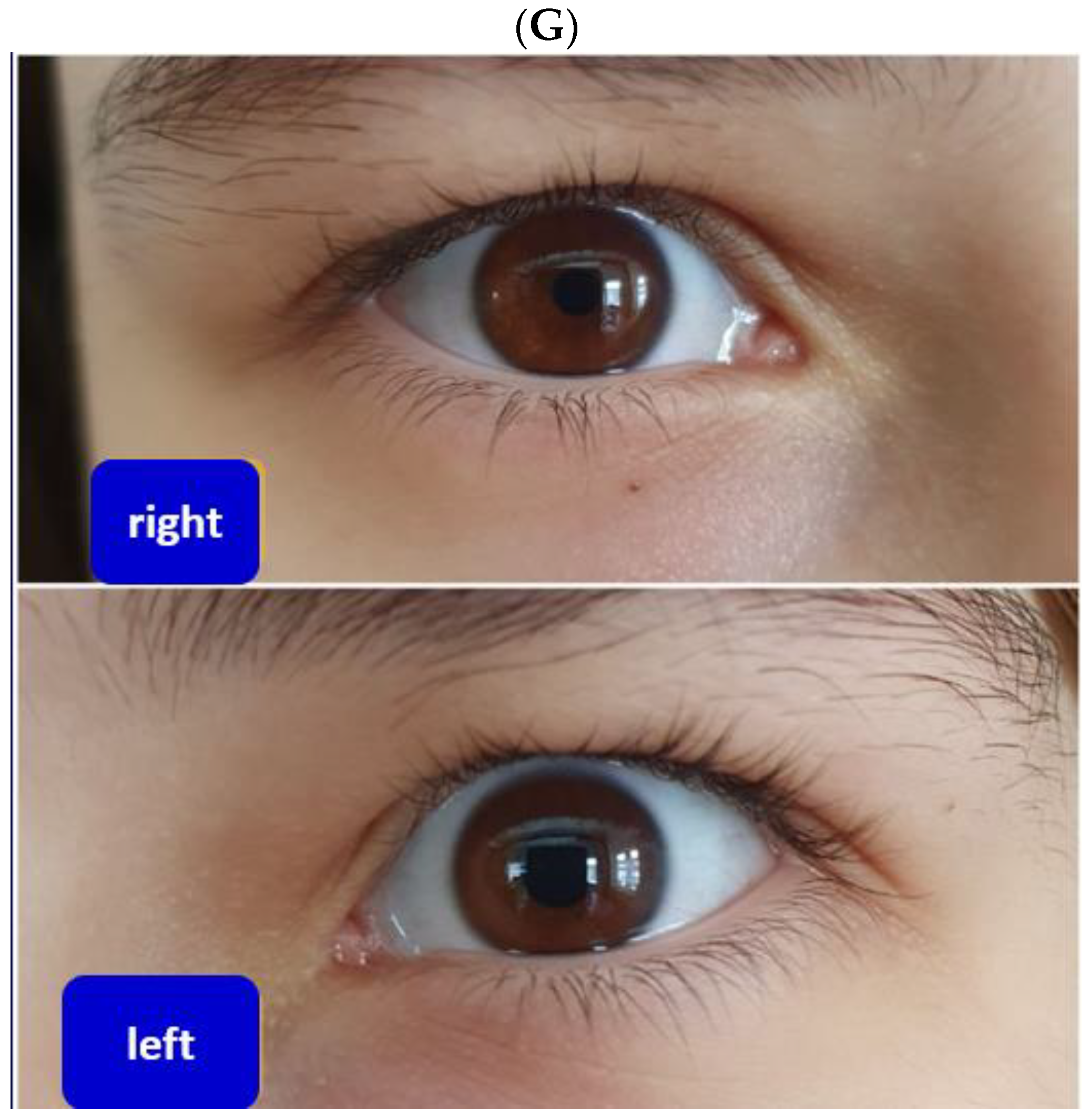
4.1. Integrating HS and Lymphocele to the Panel of Post-Thyroidectomy Complications
4.2. Pediatric HS
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CSC | cervical sympathetic chain |
| CBA | chest-breast approach |
| ETS | Endoscopic thyroid surgery |
| HS | Horner’s syndrome |
| MEN | Multiple Endocrine Neoplasia |
| ONP | oculosympathetic nerve pathway |
References
- Lambert, J.E.; Christiansen, S.P.; Peeler, C.E. Don’t Miss This! Red Flags in the Pediatric Eye Exam: Pupils. J. Binocul. Vis. Ocul. Motil. 2019, 69, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Possley, D.; Luczak, S.B.; Angus, A.; Montgomery, D. T1-T2 Disk Herniation Presenting with Horner Syndrome: A Case Report with Literary Review. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e016. [Google Scholar] [CrossRef]
- Knyazer, B.; Smolar, J.; Lazar, I.; Rosenberg, E.; Tsumi, E.; Lifshitz, T.; Levy, J. Iatrogenic Horner Syndrome: Etiology, Diagnosis and Outcomes. Isr. Med. Assoc. J. 2017, 19, 34–38. [Google Scholar]
- Sadaka, A.; Schockman, S.L.; Golnik, K.C. Evaluation of Horner Syndrome in the MRI Era. J. Neuro-Ophthalmol. 2017, 37, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Da Cruz Escaleira, A.L.R.; Kalogeropoulos, D.; Kalogeropoulos, C.; Ch’Ng, S.W.; Sung, V.C.T.; Asproudis, I.; Papoudou-Bai, A.; Malamos, K.; Mitra, A. Four common diseases causing sudden blindness or death in the eye emergency department. Postgrad. Med. J. 2021, 97, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Udry, M.; Kardon, R.; Sadun, F.; Kawasaki, A. The Tadpole Pupil: Case Series with Review of the Literature and New Considerations. Front. Neurol. 2019, 10, 846. [Google Scholar] [CrossRef]
- Horner, J.F. Über eine Form von Ptosis. Klin. Mon. Augenheilk 1869, 7, 193–198. [Google Scholar]
- Gerste, R.D. Contributions to Progress in Ophthalmology from Switzerland: From the 16th to the 21st Century. Ophthalmologica 2021, 244, 1–17. [Google Scholar] [CrossRef]
- Rootman, M.S.; Dotan, G.; Konen, O. Neuroimaging in Children with Ophthalmological Complaints: A Review. J. Neuroimaging 2021, 31, 446–458. [Google Scholar] [CrossRef]
- Iorga, E.R.; Costin, D. Vascular emergencies in neuro-ophthalmology. Rom. J. Ophthalmol. 2020, 64, 323–332. [Google Scholar] [CrossRef]
- Ramaswamy, S.; Rosso, M.; Levine, S.R. Body Lateropulsion in Stroke: Case Report and Systematic Review of Stroke Topography and Outcome. J. Stroke Cerebrovasc. Dis. 2021, 30, 105680. [Google Scholar] [CrossRef]
- Chen, H.Y.; Zhao, F.; Qin, J.Y.; Lin, H.M.; Su, J.P. Malignant meningioma with jugular vein invasion and carotid artery extension: A case report and review of the literature. World J. Clin. Cases 2020, 8, 6110–6121. [Google Scholar] [CrossRef]
- Nehete, L.S.; Konar, S.K.; Nandeesh, B.N.; Shukla, D.; Devi, B.I. Atypical presentation of extraspinal neurofibroma presenting with acute-onset monoparesis and Horner’s syndrome: Case report and review of literature. J. Craniovertebral Junction Spine 2019, 10, 188–191. [Google Scholar] [CrossRef]
- Go, J.A.; Al Othman, B.; Kini, A.; Beaver, H.A.; Lee, A.G. Vertebrobasilar ischemia (VBI) related neuro-ophthalmic syndromes after routine activities involving hyperextension or rotation of the neck (hairdresser syndrome). Eye 2020, 34, 901–905. [Google Scholar] [CrossRef]
- Teixeira, J.C.; Jackson, P.J. Internal Carotid Artery Dissection Presenting as Partial Horner’s Syndrome and Vertigo. Mil. Med. 2020, 185, e1840–e1842. [Google Scholar] [CrossRef]
- Song, J.X.; Lin, X.M.; Hao, Z.Q.; Wu, S.; Xing, Y.X. Ocular manifestations of internal carotid artery dissection. Int. J. Ophthalmol. 2019, 12, 834–839. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chang, H.W.; Chang, Y.H.; Lin, I.H.; Huang, H.Y.; Chang, C.H.; Chen, H.T.; Chen, Y.W.; Lin, T.L.; Hsu, C.J. Isolated Middle-Third Clavicle Fracture Causing Horner’s Syndrome: A Case Report and Literature Review. Front. Surg. 2021, 8, 640900. [Google Scholar] [CrossRef]
- Tvedten, E.; Richardson, J.; Husien, T.; Zghouzi, M. Horner Syndrome Secondary to Osteochondroma of the First Rib: A Case Report. Cureus 2021, 13, e14531. [Google Scholar] [CrossRef]
- Goeteyn, J.; Van Der Sanden, L.; Pesser, N.; Houterman, S.; van Sambeek, M.R.; van Nuenen, B.F.; Teijink, J.A. Redo surgery for neurogenic thoracic outlet syndrome is useful. J. Vasc. Surg. 2022, 76, 531–537.e1. [Google Scholar] [CrossRef]
- Keser, Z.; Chiang, C.-C.; Benson, J.C.; Pezzini, A.; Lanzino, G. Cervical Artery Dissections: Etiopathogenesis and Management. Vasc. Health Risk Manag. 2022, 18, 685–700. [Google Scholar] [CrossRef]
- Keser, Z.; Meschia, J.F.; Lanzino, G. Craniocervical Artery Dissections: A Concise Review for Clinicians. Mayo Clin. Proc. 2022, 97, 777–783. [Google Scholar] [CrossRef]
- Sverdlichenko, I.; Lam, C.; Donaldson, L.; Margolin, E. Horner Syndrome in Giant Cell Arteritis: Case Series and Review of the Literature. J. Neuro-Ophthalmol. 2022, 42, 340–345. [Google Scholar] [CrossRef]
- Straehley, I.; Varada, N.; Prokop, I.; Muxen, C. Horner Syndrome induced by toxoplasmosis infection in a patient with AIDS and disseminated herpes simplex virus. Am. J. Ophthalmol. Case Rep. 2020, 18, 100679. [Google Scholar] [CrossRef] [PubMed]
- Sanz Sánchez, C.I.; Morales-Angulo, C. Retropharyngeal Abscess. Clinical Review of Twenty-five Years. Acta Otorrinolaringol. Esp. 2021, 72, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Sati, W.O.; Haddad, M.; Anjum, S. A Case of Spinal Epidural Abscess Presenting with Horner Syndrome. Cureus 2021, 13, e14541. [Google Scholar] [CrossRef] [PubMed]
- Li, W.X.; He, K.X.; Dong, Y.B.; Liu, L.F.; Lu, C. Intracapsular Enucleation of Cervical Sympathetic Chain Schwannoma. Ear Nose Throat J. 2022, 1455613221124777, online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Patil, H.; Rege, S. Horner’s Syndrome due to Cervical Sympathetic Chain Schwannoma: A Rare Presentation and Review of Literature. Asian J. Neurosurg. 2019, 14, 1013–1016. [Google Scholar] [CrossRef]
- Shanmugathas, N.; Rajwani, K.M.; Dev, S. Pancoast tumour presenting as shoulder pain with Horner’s syndrome. BMJ Case Rep. 2019, 12, e227873. [Google Scholar] [CrossRef]
- Baudracco, I.; Grahovac, G.; Russo, V.M. Spontaneous cervical intradural disc herniation presenting with Brown-Séquard and Horner’s syndrome: Lesson learned from a very unique case. Eur. Spine J. 2017, 26 (Suppl. S1), 218–221. [Google Scholar] [CrossRef]
- Schubert, A.K.; Dinges, H.C.; Wulf, H.; Wiesmann, T. Interscalene versus supraclavicular plexus block for the prevention of postoperative pain after shoulder surgery: A systematic review and meta-analysis. Eur. J. Anaesthesiol. 2019, 36, 427–435. [Google Scholar] [CrossRef]
- Guglielmi, V.; Visser, J.; Arnold, M.; Sarikaya, H.; van den Berg, R.; Nederkoorn, P.J.; Leys, D.; Calvet, D.; Kloss, M.; Pezzini, A.; et al. Triple and quadruple cervical artery dissections: A systematic review of individual patient data. J. Neurol. 2019, 266, 1383–1388. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Allampalli, V.; Fisher, P.; Kaye, A.J.; Tran, A.; Cornett, E.M.; Imani, F.; Edinoff, A.N.; Djalali Motlagh, S.; Urman, R.D. Supraclavicular vs. Infraclavicular Brachial Plexus Nerve Blocks: Clinical, Pharmacological, and Anatomical Considerations. Anesthesiol. Pain Med. 2021, 11, e120658. [Google Scholar] [CrossRef] [PubMed]
- White, L.; Reardon, D.; Davis, K.; Velli, G.; Bright, M. Anterior suprascapular nerve block versus interscalene brachial plexus block for arthroscopic shoulder surgery: A systematic review and meta-analysis of randomized controlled trials. J. Anesth. 2022, 36, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Ji, X.; Zhang, X.; Ma, Q.; Yu, P.; Cai, X.; Yang, H. Suprascapular nerve block is a clinically attractive alternative to interscalene nerve block during arthroscopic shoulder surgery: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2021, 16, 376. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Yao, Y. Horner Syndrome Caused by Internal Jugular Vein Catheterization. J. Cardiothorac. Vasc. Anesth. 2020, 34, 1636–1640. [Google Scholar] [CrossRef]
- Shah, R.; Assis, F.; Alugubelli, N.; Okada, D.R.; Cardoso, R.; Shivkumar, K.; Tandri, H. Cardiac sympathetic denervation for refractory ventricular arrhythmias in patients with structural heart disease: A systematic review. Heart Rhythm 2019, 16, 1499–1505. [Google Scholar] [CrossRef]
- Mehl, S.C.; Whitlock, R.S.; Vasudevan, S.A.; Nuchtern, J.G.; Foster, J.H.; Mazziotti, M.V.; Naik-Mathuria, B. Thoracoscopic Resection of Thoracic Inlet Neuroblastic Tumors in Young Children. J. Laparoendosc. Adv. Surg. Technol. 2021, 31, 1475–1479. [Google Scholar] [CrossRef]
- Whitlock, R.S.; Mehl, S.C.; Larson, S.K.; Foster, J.H.; Hicks, J.; Nuchtern, J.G.; Sher, A.C.; Vasudevan, S.A.; Naik-Mathuria, B. Characteristics of benign neuroblastic tumors: Is surgery always necessary? J. Pediatr. Surg. 2021, 57, 1538–1543. [Google Scholar] [CrossRef]
- Cooke-Barber, J.; Scorletti, F.; Rymeski, B.; Eshelman-Kent, D.; Nagarajan, R.; Burns, K.; Jenkins, T.; Dasgupta, R. Long-term follow-up of surgical outcomes for patients with Wilms tumor and neuroblastoma. Cancer 2021, 127, 3232–3238. [Google Scholar] [CrossRef]
- Abdelhafeez, A.H.; Mansfield, S.; Talbot, L.; Murphy, A.J.; Davidoff, A.M. Improving Exposure Using Thoracoscopy for Apical Thoracic Neuroblastoma Encasing the Subclavian Vessels. J. Laparoendosc. Adv. Surg. Technol. 2021, 31, 589–593. [Google Scholar] [CrossRef]
- Yee, T.J.; Swong, K.; Park, P. Complications of anterior cervical spine surgery: A systematic review of the literature. J. Spine Surg. 2020, 6, 302–322. [Google Scholar] [CrossRef]
- Epstein, N.E. A Review of Complication Rates for Anterior Cervical Diskectomy and Fusion (ACDF). Surg. Neurol. Int. 2019, 10, 100. [Google Scholar] [CrossRef] [PubMed]
- Lubelski, D.; Pennington, Z.; Sciubba, D.M.; Theodore, N.; Bydon, A. Horner Syndrome after Anterior Cervical Discectomy and Fusion: Case Series and Systematic Review. World Neurosurg. 2020, 133, e68–e75. [Google Scholar] [CrossRef] [PubMed]
- Go, J.A.; Vickers, A.; Kaleekal, T.S.; Beaver, H.A.; Lee, A.G. Postoperative Horner Syndrome After Lung Transplantation. J. Neuro-Ophthalmol. 2020, 40, 504–506. [Google Scholar] [CrossRef] [PubMed]
- Giannaccare, G.; Gizzi, C.; Fresina, M. Horner Syndrome following Thyroid Surgery: The Clinical and Pharmacological Presentations. J. Ophthalmic Vis. Res. 2016, 11, 442–444. [Google Scholar] [CrossRef]
- Coskun, M.; Aydogan, A.; Gokce, C.; Ilhan, O.; Ozkan, O.V.; Gokce, H.; Oksuz, H. Irreversible Horner’s syndrome diagnosed by aproclonidine test due to benign thyroid nodule. Pak. J. Med. Sci. 2012, 29, 224–226. [Google Scholar] [CrossRef]
- Almog, Y.; Gepstein, R.; Kesler, A. Diagnostic value of imaging in horner syndrome in adults. J. Neuro-Ophthalmol. 2010, 30, 7–11. [Google Scholar] [CrossRef]
- Shaji, S.K.; Chan, J.; Hari, C. Benign thyroid swelling presenting as Horner’s syndrome. BMJ Case Rep. 2020, 13, e235313. [Google Scholar] [CrossRef]
- Tsakiridis, K.; Visouli, A.N.; Zarogoulidis, P.; Karapantzos, E.; Mpakas, A.; Machairiotis, N.; Stylianaki, A.; Christofis, C.; Katsikogiannis, N.; Courcoutsakis, N.; et al. Resection of a giant bilateral retrovascular intrathoracic goiter causing severe upper airway obstruction, 2 years after subtotal thyroidectomy: A case report and review of the literature. J. Thorac. Dis. 2012, 4 (Suppl. S1), 41–48. [Google Scholar] [CrossRef]
- Patel, S.; Ilsen, P.F. Acquired Horner’s syndrome: Clinical review. Optometry 2003, 74, 245–256. [Google Scholar]
- Donaldson, J.; Rodriguez-Gomez, I.; Parameswaran, R. Rapidly enlarging neck masses of the thyroid with Horner’s syndrome: A concise clinical review. Surgeon 2015, 13, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.D.; da Silva, T.L.N.; Luiz, H.; Manita, I.; Raimundo, L.; Portugal, J. Horner syndrome as a manifestation of thyroid carcinoma: A rare association. Arq. Bras. Endocrinol. Metabol. 2013, 57, 483–485. [Google Scholar] [CrossRef] [PubMed]
- Broome, J.T.; Gauger, P.G.; Miller, B.S.; Doherty, G.M. Anaplastic thyroid cancer manifesting as new-onset horner syndrome. Endocr. Pract. 2009, 15, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Yasmeen, T.; Khan, S.; Patel, S.G.; Reeves, W.A.; Gonsch, F.A.; De Bustros, A.; Kaplan, E.L. Clinical case seminar: Riedel’s thyroiditis: Report of a case complicated by spontaneous hypoparathyroidism, recurrent laryngeal nerve injury, and horner’s syndrome. J. Clin. Endocrinol. Metab. 2002, 87, 3543–3547. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Kim, S.H.; Lee, J.H.; Joo, W.I.; Chough, C.K.; Park, H.K.; Lee, K.J.; Rha, H.K. Brain Metastases of Papillary Thyroid Carcinoma with Horner’s Syndrome. Brain Tumor Res. Treat. 2014, 2, 132–137. [Google Scholar] [CrossRef]
- Leuchter, I.; Becker, M.; Mickel, R.; Dulguerov, P. Horner’s syndrome and thyroid neoplasms. ORL J. Otorhinolaryngol. Relat. Spec. 2002, 64, 49–52. [Google Scholar] [CrossRef]
- Smith, I.; Murley, R.S. Damage to the cervical sympathetic system during operations on the thyroid gland. Br. J. Surg. 1965, 52, 673–675. [Google Scholar] [CrossRef]
- Perréard, M.; Bailleul, H.; Babin, E. Post-thyroidectomy Horner’s syndrome. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2019, 136, 419–420. [Google Scholar] [CrossRef]
- Vilallonga, R.; Fort, J.M.; Mazarro, A.; Gonzalez, O.; Caubet, E.; Romero, G.; Armengol, M. Postthyroidectomy Horner’s Syndrome. Case Rep. Med. 2012, 2012, 316984. [Google Scholar] [CrossRef]
- González-Aguado, R.; Morales-Angulo, C.; Obeso-Agüera, S.; Longarela-Herrero, Y.; García-Zornoza, R.; Acle Cervera, L. Horner’s syndrome after neck surgery. Acta Otorrinolaringol. Esp. 2012, 63, 299–302. [Google Scholar] [CrossRef]
- Zhong, Y.; Yang, X.; Jiang, L.; Hu, R.; Jiang, Z.; Wang, M. Reverse “L” surgical approach for the management of giant tumors of the cervicothoracic junction. J. Thorac. Dis. 2020, 12, 3995–4001. [Google Scholar] [CrossRef] [PubMed]
- Punda, A.; Nika, Č.; Bedeković, V.; Košec, A. Delayed Horner Syndrome and Accessory Nerve Weakness After Papillary Thyroid Carcinoma Surgery. Ear Nose Throat J. 2021, 100 (Suppl. S2), 728S–729S. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Park, J.H.; Jeong, J.S.; Lee, C.R.; Park, S.; Lee, S.H.; Jeong, J.J.; Nam, K.-H.; Chung, W.Y.; Park, C.S. Prospects of robotic thyroidectomy using a gasless, transaxillary approach for the management of thyroid carcinoma. Surg. Laparosc. Endosc. Percutaneous Technol. 2011, 21, 223–229. [Google Scholar] [CrossRef]
- Kang, S.W.; Lee, S.C.; Lee, S.H.; Lee, K.Y.; Jeong, J.J.; Lee, Y.S.; Nam, K.-H.; Chang, H.S.; Chung, W.Y.; Park, C.S. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: The operative outcomes of 338 consecutive patients. Surgery 2009, 146, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- McCrory, D.; Kelly, A.; Korda, M. Postoperative Horner’s syndrome following excision of incidental cervical ganglioneuroma during hemithyroidectomy and parathyroid gland exploration. BMJ Case Rep. 2020, 13, e231514. [Google Scholar] [CrossRef] [PubMed]
- Baisakhiya, N.; Mukundan, S. Ganglioneuroma of the neck. J. Pak. Med. Assoc. 2008, 58, 699–701. [Google Scholar] [PubMed]
- Donatini, G.; Iacconi, P.; De Bartolomeis, C.; Iacconi, C.; Fattori, S.; Pucci, A.; Puccini, M.; Miccoli, P. Neck lesions mimicking thyroid pathology. Langenbecks Arch. Surg. 2008, 394, 435–440. [Google Scholar] [CrossRef]
- Harding, J.L.; Sywak, M.S.; Sidhu, S.; Delbridge, L.W. Horner’s syndrome in association with thyroid and parathyroid disease. ANZ J. Surg. 2004, 74, 442–445. [Google Scholar] [CrossRef]
- Tang, M.; Yin, S.; Yang, Z.; Sun, Y.; Chen, H.; Zhang, F. Horner syndrome after thyroid-related surgery: A review. Langenbeck’s Arch. Surg. 2022, 407, 3201–3208. [Google Scholar] [CrossRef]
- Min, Y.; Chen, H.; Wang, X.; Huang, Y.; Yin, G. Case report and literature review: Horner syndrome subsequent to endoscopic thyroid surgery. BMC Surg. 2021, 21, 36. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, X.; Gan, H.; Yu, D.; Sun, W.; Shi, Z. Horner syndrome as a postoperative complication after minimally invasive video-assisted thyroidectomy: A case report. Medicine 2017, 96, e8888. [Google Scholar] [CrossRef] [PubMed]
- Nakajo, A.; Arima, H.; Hirata, M.; Yamashita, Y.; Shinden, Y.; Hayashi, N.; Kawasaki, Y.; Arigami, T.; Uchikado, Y.; Mori, S.; et al. Bidirectional Approach of Video-Assisted Neck Surgery (BAVANS): Endoscopic complete central node dissection with craniocaudal view for treatment of thyroid cancer. Asian J. Endosc. Surg. 2017, 10, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Bozza, F.; Vigili, M.G.; Ruscito, P.; Marzetti, A.; Marzetti, F. Surgical management of parapharyngeal space tumours: Results of 10-year follow-up. Acta Otorhinolaryngol. Ital. 2009, 29, 10–15. [Google Scholar] [PubMed]
- Foma, W.; Pegbessou, E.; Amana, B.; Kpemissi, E. Left parapharyngeal ectopic goitre associated with eutopic thyroid and postoperative Horner’s syndrome. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2017, 134, 207–208. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, K.; Liu, J.; Xu, S.; Sun, Y.; Xu, M.; Wang, X. Surgical management of parapharyngeal lymph node metastases from thyroid carcinoma with transcervical approach. Surgery 2021, 171, 1233–1239. [Google Scholar] [CrossRef]
- Welch, K.; McHenry, C.R. Selective lateral compartment neck dissection for thyroid cancer. J. Surg. Res. 2013, 184, 193–199. [Google Scholar] [CrossRef]
- De Silva, W.D.D.; De Soysa, M.S.M.; Perera, B.L. Iatrogenic Horner’s syndrome: A rare complication of thyroid surgery. Ceylon Med. J. 2010, 55, 136. [Google Scholar] [CrossRef]
- Sapalidis, K.; Florou, M.; Tsopouridou, K.; Cheva, A.; Niki, M.; Pavlidis, E.; Koulouris, C.; Mantalovas, S.; Giannakidis, D.; Katsaounis, A.; et al. Horner’s Syndrome: An Uncommon Complication of Thyroidectomy and Selective Lateral Neck Dissection. Curr. Health Sci. J. 2019, 45, 111–115. [Google Scholar] [CrossRef]
- Seneviratne, S.A.; Kumara, D.S.; Drahaman, A.M.P. Horner’s syndrome: An unusual complication of thyroidectomy: A case report. J. Med. Case Rep. 2016, 10, 300. [Google Scholar] [CrossRef]
- Meng, K.; Tian, W.; Lv, Z.; Song, X. Horner’s syndrome subsequent to minimally invasive video-assisted thyroidectomy in two patients. Oncol. Lett. 2015, 10, 459–462. [Google Scholar] [CrossRef]
- Janjua, M.; Iftikhar, S.; Sarwar, M.; Farooq, M.; Naqi, S. Horner syndrome—A rare complication after thyroidectomy for benign thyroid swelling. Niger. J. Clin. Pract. 2021, 24, 1852. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Ge, Y.; Ren, P.; Liu, J.; Chen, G. Horner syndrome as a complication after thyroid microwave ablation: Case report and brief literature review. Medicine 2018, 97, e11884. [Google Scholar] [CrossRef] [PubMed]
- Ying, X.; Dandan, G.; Bin, C. Postoperative Horner’s syndrome after video-assisted thyroidectomy: A report of two cases. World J. Surg. Oncol. 2013, 11, 315. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, M.A.S.; Cabungcal, A.C. Horner syndrome after radical neck surgery for anaplastic thyroid carcinoma. BMJ Case Rep. 2015, 2015, bcr2015209324. [Google Scholar] [CrossRef]
- Vorländer, C.; Kohlhase, K.D.; Korkusuz, Y.; Erbelding, C.; Luboldt, W.; Baser, I.; Korkusuz, H. Comparison between microwave ablation and bipolar radiofrequency ablation in benign thyroid nodules: Differences in energy transmission, duration of application and applied shots. Int. J. Hyperth. 2018, 35, 216–225. [Google Scholar] [CrossRef]
- Heck, K.; Happel, C.; Grünwald, F.; Korkusuz, H. Percutaneous microwave ablation of thyroid nodules: Effects on thyroid function and antibodies. Int. J. Hyperth. 2015, 31, 560–567. [Google Scholar] [CrossRef]
- Wang, J.F.; Wu, T.; Hu, K.P.; Xu, W.; Zheng, B.W.; Tong, G.; Yao, Z.C.; Liu, B.; Ren, J. Complications Following Radiofrequency Ablation of Benign Thyroid Nodules: A Systematic Review. Chin. Med. J. 2017, 130, 1361–1370. [Google Scholar] [CrossRef]
- Kim, C.; Lee, J.H.; Choi, Y.J.; Kim, W.B.; Sung, T.Y.; Baek, J.H. Complications encountered in ultrasonography-guided radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers. Eur. Radiol. 2017, 27, 3128–3137. [Google Scholar] [CrossRef]
- Cheong, C.W.S.; Au, J.X.Y.; Lim, M.Y.; Fu, E.W.; Li, H.; Gan, J.Y. The efficacy and safety of high-intensity focused ultrasound in the treatment of benign thyroid nodules: A systematic review and meta-analysis from 1990 to 2021. Ann. Acad. Med. Singap. 2022, 51, 101–108. [Google Scholar] [CrossRef]
- Ben Hamou, A.; Monpeyssen, H. Horner’s Syndrome During High-Intensity Focused Ultrasound Ablation for a Benign Thyroid Nodule. AACE Clin. Case Rep. 2021, 7, 164–168. [Google Scholar] [CrossRef]
- Monpeyssen, H.; Ben Hamou, A.; Hegedüs, L.; Ghanassia, É.; Juttet, P.; Persichetti, A.; Bizzarri, G.; Bianchini, A.; Guglielmi, R.; Raggiunti, B.; et al. High-intensity focused ultrasound (HIFU) therapy for benign thyroid nodules: A 3-year retrospective multicenter follow-up study. Int. J. Hyperth. 2020, 37, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Gong, X.; Zhou, Q.; Chen, X.; Chen, X. Ultrasound-Guided Percutaneous Microwave Ablation for Solid Benign Thyroid Nodules: Comparison of MWA versus Control Group. Int. J. Endocrinol. 2017, 2017, 9724090. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Gong, X.; Zhou, Q.; Chen, X.; Chen, X.; Shi, B. US-guided percutaneous microwave ablation for the treatment of benign thyroid nodules. Endocr. J. 2017, 64, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Lang, B.H.-H.; Woo, Y.-C.; Wong, I.Y.-H.; Chiu, K.W.-H. Single-Session High-Intensity Focused Ultrasound Treatment for Persistent or Relapsed Graves Disease: Preliminary Experience in a Prospective Study. Radiology 2017, 285, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Pishdad, G.R.; Pishdad, P.; Pishdad, R. Horner’s syndrome as a complication of percutaneous ethanol treatment of thyroid nodule. Thyroid 2011, 21, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Lv, S.; Wang, Q.; Zhao, W.; Han, L.; Wang, Q.; Batchu, N.; Ulain, Q.; Zou, J.; Sun, C.; Du, J.; et al. A review of the postoperative lymphatic leakage. Oncotarget 2017, 8, 69062–69075. [Google Scholar] [CrossRef] [PubMed]
- Aznar, A.L.; Lloret, P.E.; Moreno, C.S.; Luna-Guibourg, R.; Negre, R.R. Laparoscopic approach for symptomatic pelvic and para-aortic lymphoceles. J. Turk. Gynecol. Assoc. 2022, 23, 60–62. [Google Scholar] [CrossRef]
- Ten Hove, A.S.; Tjiong, M.Y.; Zijlstra, I.A. Treatment of symptomatic postoperative pelvic lymphoceles: A systematic review. Eur. J. Radiol. 2021, 134, 109459. [Google Scholar] [CrossRef]
- Sommer, C.M.; Pieper, C.C.; Itkin, M.; Nadolski, G.J.; Hur, S.; Kim, J.; Maleux, G.; Kauczor, H.U.; Richter, G.M. Conventional Lymphangiography (CL) in the Management of Postoperative Lymphatic Leakage (PLL): A Systematic Review. Rofo 2020, 192, 1025–1035. [Google Scholar] [CrossRef]
- Majdalany, B.S.; El-Haddad, G. Contemporary lymphatic interventions for post-operative lymphatic leaks. Transl. Androl. Urol. 2020, 9 (Suppl. S1), S104–S113. [Google Scholar] [CrossRef]
- Moussa, A.M.; Camacho, J.C.; Maybody, M.; Gonzalez-Aguirre, A.J.; Ridouani, F.; Kim, D.; Laudone, V.P.; Santos, E. Percutaneous Lymphatic Embolization as Primary Management of Pelvic and Retroperitoneal Iatrogenic Lymphoceles. J. Vasc. Interv. Radiol. 2021, 32, 1529–1535. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.K.; Haddad, A.F.; Chan, A.K.; Eichler, C.M.; Tay, B.; Burch, S.; Chou, D.; Ames, C.P.; Mummaneni, P.V. Lymphocele after anterior lumbar interbody fusion: A review of 1322 patients. J. Neurosurg. Spine 2021, 35, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Touska, P.; A Constantinides, V.; Palazzo, F.F. A rare complication: Lymphocele following a re-operative right thyroid lobectomy for multinodular goitre. BMJ Case Rep. 2012, 2012, bcr0220125747. [Google Scholar] [CrossRef] [PubMed]
- Ohta, N.; Fukase, S.; Suzuki, Y.; Ishida, A.; Aoyagi, M. Treatments of various otolaryngological cystic diseases by OK-4321: Its in-dications and limitations. Laryngoscope 2010, 120, 2193–2196. [Google Scholar] [CrossRef] [PubMed]
- Lohela, P. Ultrasound-guided drainages and sclerotherapy. Eur. Radiol. 2002, 12, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Campisi, C.C.; Boccardo, F.M.; Piazza, C.; Campisi, C. Evolution of chylous fistula management after neck dissection. Curr. Opin. Otolaryngol. Head Neck Surg. 2013, 21, 150–156. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, B.W.; Chang, H.S.; Park, C.S. Factors predisposing to chyle leakage following thyroid cancer surgery without lateral neck dissection. Head Neck 2013, 35, 1149–1152. [Google Scholar] [CrossRef]
- Nowak, K.; Wierzbicka, M.; Szyfter, W. Chylous leakage--rare but still dangerous complication after neck surgery. Otolaryngol. Pol. 2011, 65, 128–131. [Google Scholar] [CrossRef]
- Huo, J.; Ou, D.; Chen, C.; Zhao, J. Local injection of hypertonic glucose for treating refractory chylous leakage: The first case report. Asian J. Surg. 2021, 44, 1568–1569. [Google Scholar] [CrossRef]
- Hong, Y.T.; Hong, K.H. Identification of lymphatic channels in the tracheoesophageal groove during central neck dissection for thyroid cancer. Head Neck 2018, 40, E87–E90. [Google Scholar] [CrossRef]
- Lorenz, K.; Abuazab, M.; Sekulla, C.; Nguyen-Thanh, P.; Brauckhoff, M.; Dralle, H. Management of lymph fistulas in thyroid surgery. Langenbecks Arch. Surg. 2010, 395, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, A.M.; Pappalardo, V.; Liu, X.; Wu, C.-W.; Anuwong, A.; Kim, H.Y.; Liu, R.; Lavazza, M.; Inversini, D.; Coppola, A.; et al. Usefulness of CBCT and guidance software for percutaneous embolization of a lymphatic leakage after thyroidectomy for cancer. Gland Surg. 2016, 5, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Moussa, A.M.; Maybody, M.; Gonzalez-Aguirre, A.J.; Buicko, J.L.; Shaha, A.R.; Santos, E. Thoracic Duct Embolization in Post-neck Dissection Chylous Leakage: A Case Series of Six Patients and Review of the Literature. Cardiovasc. Interv. Radiol. 2020, 43, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Ryu, K.H.; Baek, H.J.; Cho, S.B.; An, H.J.; Kim, J.P. Granulomatous lymphadenitis mimicking metastatic lymphadenopathy in the neck after lymphatic embolization of chyle leakage: A case report. Medicine. Medicine 2018, 97, e12744. [Google Scholar] [CrossRef]
- Kim, C.W.; Kim, J.S.; Lee, A.H.; Kim, Y.S. Viscum album extract (Helixor-M) treatment for thoracic duct injury after modified radical neck dissection: A case report. Gland Surg. 2021, 10, 832–836. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, S.M.; Chang, H.; Kim, B.W.; Lee, Y.S.; Lim, C.Y.; Chang, H.-S.; Park, C.S. Clinical Experience with n-Butyl-2-Cyanoacrylate in Performing Lateral Neck Dissection for Metastatic Thyroid Cancer. Surg. Innov. 2016, 23, 481–485. [Google Scholar] [CrossRef]
- Huo, J.; Guo, Y.; Hu, X.; Chen, X.; Liu, W.; Luo, L.; Shen, S.; Qu, R. Endoscopic Thyroidectomy with Level Vb Dissection Via a Chest-breast Approach: Technical Updates for Selective Lateral Neck Dissection. Surg. Laparosc. Endosc. Percutaneous Technol. 2021, 31, 342–345. [Google Scholar] [CrossRef]
- Sun, P.; Mak, T.K.; Li, J.; Wang, C. Endoscopic Left Central Lymph Node Dissection of Thyroid Cancer: Safe, Feasible, and Relatively Easy. Surg. Innov. 2021, 28, 747–753. [Google Scholar] [CrossRef]
- Qu, R.M.; Hu, X.; Guo, Y.; Zhou, X.; Huo, J.; Chen, Y.; Chen, X.; Liu, W.; Chen, C.; Mao, G.; et al. Endoscopic Lateral Neck Dissection (IIA, IIB, III, and IV) Using a Breast Approach: Outcomes from a Series of the First 24 Cases. Surg. Laparosc. Endosc. Percutaneous Technol. 2020, 31, 66–70. [Google Scholar] [CrossRef]
- Guo, Y.; Qu, R.; Huo, J.; Wang, C.; Hu, X.; Chen, C.; Liu, D.; Chen, W.; Xiong, J. Technique for endoscopic thyroidectomy with selective lateral neck dissection via a chest–breast approach. Surg. Endosc. 2019, 33, 1334–1341. [Google Scholar] [CrossRef]
- Park, I.; Her, N.; Kim, J.S.; Kim, J.-H.; Choe, J.-H. Management of chyle leakage after thyroidectomy, cervical lymph node dissection, in patients with thyroid cancer. Head Neck 2018, 40, 7–15. [Google Scholar] [CrossRef]
- Song, R.; Fei, X.; Cui, J.; Yu, X.; Zhang, Y.; Li, L.; Liu, Q. Treatment strategy for chylous leakage after dissection of central lymph nodes in thyroid cancer. Ann. Italy Chir. 2020, 91, 692–696. [Google Scholar]
- Polistena, A.; Vannucci, J.; Monacelli, M.; Lucchini, R.; Sanguinetti, A.; Avenia, S.; Santoprete, S.; Triola, R.; Cirocchi, R.; Puma, F.; et al. Thoracic duct lesions in thyroid surgery: An update on diagnosis, treatment and prevention based on a cohort study. Int. J. Surg. 2015, 28 (Suppl. S1), S33–S37. [Google Scholar] [CrossRef]
- Joaquim, A.F.; Makhni, M.C.; Riew, K.D. Post-operative nerve injuries after cervical spine surgery. Int. Orthop. 2019, 43, 791–795. [Google Scholar] [CrossRef]
- Xu, X.; Li, X.; Ren, F.; Dong, M.; Liu, M.; Chen, J. Primary chondroma of posterior mediastinum with Horner’s syndrome: A case report. World J. Surg. Oncol. 2018, 16, 209. [Google Scholar] [CrossRef]
- Chambers, D.; Bhatia, K. Horner’s syndrome following obstetric neuraxial blockade—A systematic review of the literature. Int. J. Obstet. Anesth. 2018, 35, 75–87. [Google Scholar] [CrossRef]
- Prezerakos, G.K.; Sayal, P.; Kourliouros, A.; Pericleous, P.; Ladas, G.; Casey, A. Paravertebral tumours of the cervicothoracic junction extending into the mediastinum: Surgical strategies in a no man’s land. Eur. Spine J. 2018, 27, 902–912. [Google Scholar] [CrossRef]
- Martin, T.J. Horner Syndrome: A Clinical Review. ACS Chem. Neurosci. 2018, 9, 177–186. [Google Scholar] [CrossRef]
- Riou-Comte, N.; Mione, G.; Humbertjean, L.; Ottenin, M.A.; Lacour, J.C.; Richard, S. Spontaneous cervical artery dissection in patients aged over 70 years: Two cases and systematic literature review. Clin. Interv. Aging 2017, 12, 1355–1362. [Google Scholar] [CrossRef]
- Guo, C.; Ma, J.; Ma, X.; Lu, B.; Wang, Y.; Tian, A.; Sun, L.; Wang, Y.; Dong, B.C.; Teng, Y.B. Supraclavicular block versus interscalene brachial plexus block for shoulder surgery: A meta-analysis of clinical control trials. Int. J. Surg. 2017, 45, 85–91. [Google Scholar] [CrossRef]
- Uludağ, I.F.; Sarıteke, A.; Öcek, L.; Zorlu, Y.; Şener, U.; Tokuçoğlu, F.; Uludağ, B. Neuromyelitis optica presenting with horner syndrome: A case report and review of literature. Mult. Scler. Relat. Disord. 2017, 14, 32–34. [Google Scholar] [CrossRef]
- Park, S.; Kim, T.S.; Kim, S.-K. Unusual Horner’s Syndrome in Recurrent Breast Cancer: Evaluation Using 18F-FDG PET/CT. Nucl. Med. Mol. Imaging 2016, 51, 93–96. [Google Scholar] [CrossRef]
- Ofri, A.; Malka, V.; Lodh, S. Horner’s syndrome in traumatic first rib fracture without carotid injury; review of anatomy and pathophysiology. Trauma Case Rep. 2017, 8, 1–4. [Google Scholar] [CrossRef]
- Vogiatzaki, T.; Tsikouras, P.; Tsoleridis, T.; Bachar, M.; Christofis, C.; Liberis, A.; Galazios, G. Horner’s syndrome and epidural anesthesia in labor and cesarean section. Clin. Exp. Obstet. Gynecol. 2017, 44, 337–340. [Google Scholar] [CrossRef]
- Kang, S.-W.; Lee, S.H.; Ryu, H.R.; Lee, K.Y.; Jeong, J.J.; Nam, K.-H.; Chung, W.Y.; Park, C.S. Initial experience with robot-assisted modified radical neck dissection for the management of thyroid carcinoma with lateral neck node metastasis. Surgery 2010, 148, 1214–1221. [Google Scholar] [CrossRef]
- Al-Hakami, H.A.; Al Garni, M.A.; Malas, M.; Abughanim, S.; Alsuraihi, A.; Al Raddadi, T. Surgical Complications After Thyroid Surgery: A 10-Year Experience at Jeddah, Saudi Arabia. Indian J. Otolaryngol. Head Neck Surg. 2019, 71 (Suppl. S1), 1012–1017. [Google Scholar] [CrossRef]
- Ban, E.J.; Yoo, J.Y.; Kim, W.W.; Son, H.Y.; Park, S.; Lee, S.H.; Lee, C.R.; Kang, S.-W.; Jeong, J.J.; Nam, K.-H.; et al. Surgical complications after robotic thyroidectomy for thyroid carcinoma: A single center experience with 3,000 patients. Surg. Endosc. 2014, 28, 2555–2563. [Google Scholar] [CrossRef]
- Lee, Y.S.; Nam, K.-H.; Chung, W.Y.; Chang, H.S.; Park, C.S. Postoperative complications of thyroid cancer in a single center experience. J. Korean Med. Sci. 2010, 25, 541–545. [Google Scholar] [CrossRef]
- Nistor, C.; Ciuche, A.; Motaş, C.; Motaş, N.; Bluoss, C.; Pantile, D.; Davidescu, M.; Horvat, T. Cervico-mediastinal thyroid masses—Our experience. Chirurgia 2014, 109, 34–43. [Google Scholar]
- Ciuche, A.; Nistor, C.; Motaş, C.; Horvat, T. Minimally invasive surgery in the treatment of malignant pleuro-pericardial effusions. Chirurgia 2012, 107, 206–212. [Google Scholar]
- Nistor, C.; Ranetti, A.E.; Ciuche, A.; Pantile, D.; Constantin, L.M.; Brincoveanu, R. Betadine in chemical pleurodesis. Farmacia 2014, 62, 897–906. [Google Scholar]
- Scappaticcio, L.; Maiorino, M.I.; Iorio, S.; Camponovo, C.; Piccardo, A.; Bellastella, G.; Docimo, G.; Esposito, K.; Trimboli, P. Thyroid surgery during the COVID-19 pandemic: Results from a systematic review. J. Endocrinol. Investig. 2021, 45, 181–188. [Google Scholar] [CrossRef]
- Boles, R.W.; Zheng, M.; Kwon, D. Expanded use of telemedicine for thyroid and parathyroid surgery in the COVID-19 era and beyond. Am. J. Otolaryngol. 2022, 43, 103393. [Google Scholar] [CrossRef]
- Ermer, J.P.; Ballester, J.M.S.; Go, B.C.; Philipson, B.; Gabriel, P.E.; Pryma, D.A.; Fraker, D.L.; Kelz, R.R.; Wachtel, H. Endocrine Surgical Procedures During COVID-19: Patient Prioritization and Time to Surgery. J. Surg. Res. 2021, 268, 459–464. [Google Scholar] [CrossRef]
- Demiral, M.; Binay, C.; Şimşek, E.; Ilhan, H. Horner Syndrome Secondary to Thyroid Surgery. Case Rep. Endocrinol. 2017, 2017, 1689039. [Google Scholar] [CrossRef]
- Karnak, I.; Ardıçlı, B.; Ekinci, S.; Çiftçi, A.; Orhan, D.; Kale, G.; Tanyel, F.C.; Şenocak, M.E. Papillary thyroid carcinoma does not have standard course in children. Pediatr. Surg. Int. 2011, 27, 931–936. [Google Scholar] [CrossRef]
- Yip, D.; Drachtman, R.; Amorosa, L.; Trooskin, S. Papillary thyroid cancer presenting as Horner syndrome. Pediatr. Blood Cancer 2010, 55, 739–741. [Google Scholar] [CrossRef]
- Van Santen, H.M.; Aronson, D.C.; Vulsma, T.; Tummers, R.F.H.M.; Geenen, M.M.; De Vijlder, J.J.M.; Van den Bos, C. Frequent adverse events after treatment for childhood-onset differentiated thyroid carcinoma: A single institute experience. Eur. J. Cancer 2004, 40, 1743–1751. [Google Scholar] [CrossRef]
- Kundel, A.; Thompson, G.B.; Richards, M.L.; Qiu, L.X.; Cai, Y.; Schwenk, F.W.; Lteif, A.N.; Pittock, S.T.; Kumar, S.; Tebben, P.J.; et al. Pediatric endocrine surgery: A 20-year experience at the mayo clinic. J. Clin. Endocrinol. Metab. 2014, 99, 399–406. [Google Scholar] [CrossRef]
- Mastronikolis, N.S.; Spiliopoulou, S.P.; Zolota, V.; Papadas, T.A. Horner’s Syndrome Incidental to Medullary Thyroid Carcinoma Excision: Case Report and Brief Literature Review. Case Rep. Otolaryngol. 2016, 2016, 7348175. [Google Scholar] [CrossRef]
- Buhr, H.J.; Lehnert, T.; Raue, F. New operative strategy in the treatment of metastasizing medullary carcinoma of the thyroid. Eur. J. Surg. Oncol. (EJSO) 1990, 16, 366–369. [Google Scholar] [PubMed]
- Khalatbari, H.; Ishak, G.E. Imaging of Horner syndrome in pediatrics: Association with neuroblastoma. Pediatr. Radiol. 2021, 51, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Chui, C.H.; Thirugnanam, A. Trapdoor anterior thoracotomy for cervicothoracic and apical thoracic neuroblastoma in children. Pediatr. Surg. Int. 2020, 36, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Kawabata, H. The prognostic value of concurrent Horner syndrome in surgical decision making at 3 months in total-type neonatal brachial plexus palsy. J. Hand Surg. Eur. Vol. 2018, 43, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Alvi, S.; Karadaghy, O.; Manalang, M.; Weatherly, R. Clinical manifestations of neuroblastoma with head and neck involvement in children. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 157–162. [Google Scholar] [CrossRef]
- Accogli, A.; Hamdan, F.F.; Poulin, C.; Nassif, C.; Rouleau, G.A.; Michaud, J.L.; Srour, M. A novel homozygous AP4B1 mutation in two brothers with AP-4 deficiency syndrome and ocular anomalies. Am. J. Med. Genet. A 2018, 176, 985–991. [Google Scholar] [CrossRef]
- Fierz, F.C.; Gerth-Kahlert, C. Long-Term Follow-Up in Children with Anisocoria: Cocaine Test Results and Patient Outcome. J. Ophthalmol. 2017, 2017, 7575040. [Google Scholar] [CrossRef]
- Martin, G.C.; Aymard, P.-A.; Denier, C.; Seghir, C.; Abitbol, M.; Boddaert, N.; Bremond-Gignac, D.; Robert, M.P. Usefulness of cocaine drops in investigating infant anisocoria. Eur. J. Paediatr. Neurol. 2017, 21, 852–857. [Google Scholar] [CrossRef]
- Wilson, T.J.; Chang, K.W.C.; Yang, L.J.S. Prediction Algorithm for Surgical Intervention in Neonatal Brachial Plexus Palsy. Neurosurgery 2018, 82, 335–342. [Google Scholar] [CrossRef]
- Braungart, S.; Craigie, R.J.; Farrelly, P.; Losty, P.D. Paediatric Horner’s syndrome: Is investigation for underlying malignancy always required? Arch. Dis. Child. 2019, 104, 984–987. [Google Scholar] [CrossRef]
- Han, J.; Park, S.Y.; Lee, J.-Y. Nationwide population-based incidence and etiologies of pediatric and adult Horner syndrome. J. Neurol. 2021, 268, 1276–1283. [Google Scholar] [CrossRef]
- Moussa, G.; Panthagani, J.; Gavens, E.; Singh, M.; Painter, S. A novel case and review of paediatric Horner syndrome. Eye 2020, 34, 1931–1933. [Google Scholar] [CrossRef]
- Nutt, R.; McLoone, E.; George, S.; O’Gallagher, M. Atypical Horner’s syndrome: Frequency, features and aetiology in a paediatric population. Eye 2020, 35, 811–816. [Google Scholar] [CrossRef]
- Donaldson, L.; Issa, M.; Dezard, V.; Margolin, E. Low probability of myasthenia Gravis in patients presenting to neuro-ophthalmology clinic for evaluation of isolated ptosis. Eur. J. Ophthalmol. 2022, 11206721221107300, online ahead of print. [Google Scholar] [CrossRef]
- Avdagic, E.; Phelps, P.O. Eyelid ptosis (Blepharoptosis) for the primary care practitioner. Dis. Mon. 2020, 66, 101040. [Google Scholar] [CrossRef]
- Latting, M.W.; Huggins, A.B.; Marx, D.P.; Giacometti, J.N. Clinical Evaluation of Blepharoptosis: Distinguishing Age-Related Ptosis from Masquerade Conditions. Semin. Plast. Surg. 2017, 31, 005–016. [Google Scholar] [CrossRef]
- Kitazawa, T.; Suito, M.; Nagaya, H. Blepharoptosis as a complication of percutaneous ethanol injection of thyroid cyst. J. Surg. Case Rep. 2022, 2022, rjac091. [Google Scholar] [CrossRef]
- Pavone, P.; Cho, S.Y.; Praticò, A.; Falsaperla, R.; Ruggieri, M.; Jin, D.-K. Ptosis in childhood: A clinical sign of several disorders: Case series reports and literature review. Medicine 2018, 97, e12124. [Google Scholar] [CrossRef]




| Reference Number within Main Text | Studied Population | Thyroidectomy | Central Neck Dissection |
|---|---|---|---|
| Adult population | |||
| [59] | case report (1 patient with HS) | + | |
| [60] | cases series (6 patients with HS) | + | |
| [61] | case series 21 patients with different tumors (1 patient with HS) | reverse “L” surgical approach | |
| [62] | case report (1 patient with HS) | + | Selective neck region VI dissection |
| [63] | retrospective study 1000 patients with thyroid cancer (1 patient with HS) | robot-assisted endoscopic thyroid surgery using a gasless, transaxillary approach | Ipsilateral central compartment node dissection (malignant cases) |
| [64] | retrospective study 338 patients (1 patient with HS) | robot-assisted endoscopic thyroid operations using a gasless, transaxillary approach | Ipsilateral central compartment node dissection (malignant cases) |
| [65] | case report (1 patient with HS) | left hemi-thyroidectomy in addition to ectopic parathyroid gland removal and four-gland parathyroid exploration (no pre-operatory imaging parathyroid adenoma localization) | |
| [70] | case report (1 patient with HS) | +(endoscopic thyroid surgery) | central lymph node dissection (endoscopic thyroid surgery) |
| [71] | case report (1 patient with HS) | +left-side minimally invasive video-assisted thyroidectomy | neck dissection |
| [72] | case series 16 patients (1 patient with HS) | endoscopic thyroid cancer surgery (new bidirectional approach of video-assisted neck surgery) | bilateral central node dissection (5/16 patients) |
| [74] | case report (1 patient with HS) | left parapharyngeal ectopic goiter | |
| [75] | retrospective study 97 patients (2 patients with HS = 2%) | Parapharyngeal lymph node metastases resection | |
| [76] | retrospective study 45 patients (2 patients with H = 5%) | + (19/45 synchro nous with lateral neck dissection) | selective lateral compartment neck dissection (5/45 bilateral) |
| [77] | case report (1 patient with HS) | left hemithyroidectomy | |
| [78] | case report (1 patient with HS) | total thyroidectomy | selective lateral neck dissection |
| [79] | case report (1 patient with HS) | + | |
| [80] | case report (2 patients with HS) | minimally invasive video-assisted thyroidectomy (total thyroidectomy) | |
| [81] | case report (1 patient with HS) | + | |
| [82] | case report (1 patient with HS) | thyroid microwave ablation | |
| [83] | case report (2 patients with HS) | video-assisted thyroidectomy | |
| [84] | case report (1 patient with HS) | thyroidectomy (palliative procedure for anaplastic thyroid carcinoma) | radical neck dissection (right side) |
| [85] | retrospective study60 patients (1 patient with HS) | thyroid microwave ablation (21/60) | |
| [150] | case report (1 patient with HS) | + | modified neck dissection type III (right side) + elective dissection at levels II, III, and IV (left side) |
| [151] | case series 11 patients (3 patients with HS) | + | modified radical neck dissection |
| Pediatric population | |||
| [145] | case report (1 patient with HS) | + | |
| [146] | retrospective study 16 patients with thyroid cancer (1 patient with HS) | + | cervical lymph node dissection (15/16) |
| [148] | retrospective study 25 patients with thyroid cancer (2 patients with HS) | + | lymph node dissection (15/25) |
| [149] | retrospective study 177 thyroid procedures (2 patients with HS) | total thyroidectomies (133/177) hemi-thyroidectomies (40/177) | central or lateral neck dissection (53/177) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carsote, M.; Nistor, C.-E.; Popa, F.L.; Stanciu, M. Horner’s Syndrome and Lymphocele Following Thyroid Surgery. J. Clin. Med. 2023, 12, 474. https://doi.org/10.3390/jcm12020474
Carsote M, Nistor C-E, Popa FL, Stanciu M. Horner’s Syndrome and Lymphocele Following Thyroid Surgery. Journal of Clinical Medicine. 2023; 12(2):474. https://doi.org/10.3390/jcm12020474
Chicago/Turabian StyleCarsote, Mara, Claudiu-Eduard Nistor, Florina Ligia Popa, and Mihaela Stanciu. 2023. "Horner’s Syndrome and Lymphocele Following Thyroid Surgery" Journal of Clinical Medicine 12, no. 2: 474. https://doi.org/10.3390/jcm12020474
APA StyleCarsote, M., Nistor, C.-E., Popa, F. L., & Stanciu, M. (2023). Horner’s Syndrome and Lymphocele Following Thyroid Surgery. Journal of Clinical Medicine, 12(2), 474. https://doi.org/10.3390/jcm12020474







