Effects of Isolated Myofascial Release Therapy in Patients with Chronic Low Back Pain—A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Protocol Registration
2.2. Data Sources
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Assessment
3. Results
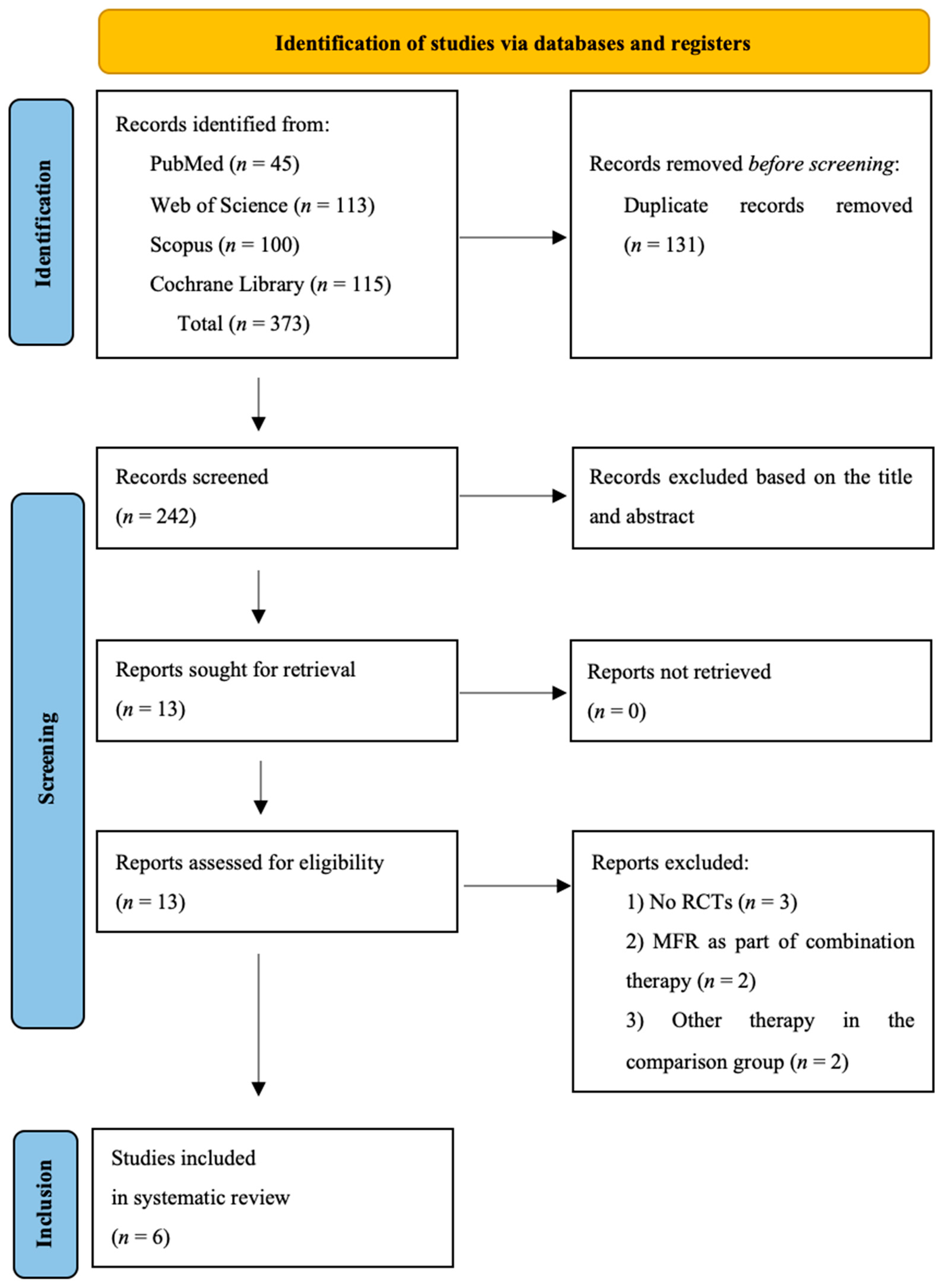
3.1. Study Selection
3.2. Study Characteristics
3.2.1. Overview of Included Studies
3.2.2. Intervention Characteristics and Outcome Measures
3.3. Quality Assessment
3.4. Synthesis of Results
3.4.1. The Effect of Isolated MFR on Pain
3.4.2. The Effect of Isolated MFR on Range of Motion
3.4.3. The Effect of Isolated MFR on Functional Disability
3.4.4. The Effect of Isolated MFR on Fear-Avoidance Beliefs
3.4.5. The Effect of Isolated MFR on Muscle Activity
3.4.6. The Effect of Isolated MFR on Postural Stability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gandey, A. Low back pain—Normal part of adolescence. Arch. Pediatr. Adolesc. Med. 2009, 163, 65–71. [Google Scholar]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- DePalma, M.J.; Ketchum, J.M.; Saullo, T. What is the source of Chronic Low Back Pain and does age Play a Role? Pain Med. 2011, 12, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Shmagel, A.; Foley, R.; Ibrahim, H. Epidemiology of Chronic Low Back Pain in US Adults: Data from the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 2016, 68, 1688–1694. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Langevin, H.M.; Fox, J.R.; Koptiuch, C.; Badger, G.J.; Greenan-Naumann, A.C.; Bouffard, N.A.; Konofagou, E.E.; Lee, W.N.; Triano, J.J.; Henry, S.M. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskelet. Disord. 2011, 12, 203. [Google Scholar] [CrossRef] [PubMed]
- Manheim, C.J. The Myofascial Release Manual; SLACK Incorporated: West Deptford, NJ, USA, 2008. [Google Scholar]
- Marizeiro, D.F.; Florêncio, A.C.L.; Nunes, A.C.L.; Campos, N.G.; Lima, P.O.P. Immediate effects of diaphragmatic myofascial release on the physical and functional outcomes in sedentary women: A randomized placebo-controlled trial. J. Bodyw. Mov. Ther. 2018, 22, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Tozzi, P.; Bongiorno, D.; Vitturini, C. Fascial release effects on patients with non-specific cervical or lumbar pain. J. Bodyw. Mov. Ther. 2011, 15, 405–416. [Google Scholar] [CrossRef]
- Chen, Y.H.; Chai, H.M.; Shau, Y.W.; Wang, C.L.; Wang, S.F. Increased sliding of transverse abdominis during contraction after myofascial release in patients with chronic low back pain. Man. Ther. 2016, 23, 69–75. [Google Scholar] [CrossRef]
- Shah, Y.; Arkesteijn, M.; Thomas, D.; Whyman, J.; Passfield, L. The acute effects of integrated myofascial techniques on lumbar paraspinal blood flow compared with kinesio-taping: A pilot study. J. Bodyw. Mov. Ther. 2017, 21, 459–467. [Google Scholar] [CrossRef]
- Ożóg, P.; Weber-Rajek, M.; Radzimińska, A.; Goch, A. Analysis of Muscle Activity following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial. J. Clin. Med. 2021, 10, 4039. [Google Scholar] [CrossRef] [PubMed]
- Ożóg, P.; Weber-Rajek, M.; Radzimińska, A.; Goch, A. Analysis of postural stability following the application of myofascial release techniques for low back pain-a randomized-controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 2198. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wu, J.; Wang, X.; Wu, J.; Ren, Z. The effects of myofascial release technique for patients with low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2021, 59, 102737. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Wang, Y.; Ye, X.; Chen, Z.; Zhou, R.; Ye, Z.; Huang, J.; Zhu, Y.; Chen, G.; Xu, X. Myofascial release for chronic low back pain: A systematic review and meta-analysis. Front. Med. 2021, 8, 697986. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- De Morton, N.A. The PEDro scale is a valid measure of the methodolo- gical quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Arguisuelas, M.D.; Lisón, J.F.; Sánchez-Zuriaga, D.; Martínez-Hurtado, I.; Doménech-Fernández, J. Effects of myofascial release in nonspecific chronic low back pain: A randomized clinical trial. Spine 2017, 42, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Arguisuelas, M.D.; Lisón, J.F.; Doménech-Fernández, J.; Martínez-Hurtado, I.; Salvador Coloma, P.; Sánchez-Zuriaga, D. Effects of myofascial release in erector spinae myoelectric activity and lumbar spine kinematics in non-specific chronic low back pain: Randomized controlled trial. Clin. Biomech. 2019, 63, 27–33. [Google Scholar] [CrossRef]
- Sakabe, F.F.; Mazer, D.A.; Cia, J.A.; Sakabe, D.I.; Bortolazzo, G.L. Effects of myofascial techniques on pain, mobility and function in patients with low back pain: A double-blind, controlled and randomized trial. Man. Ther. Posturology Rehabil. J. 2020, 18, 1–6. [Google Scholar] [CrossRef]
- Paulo, L.R.; Lacerda, A.C.R.; Martins, F.L.M.; Fernandes, J.S.C.; Vieira, L.S.; Guimarães, C.Q.; Ballesteros, S.S.G.; Anjos, M.T.S.D.; Tavares, P.A.; Fonseca, S.F.D.; et al. Can a single trial of a thoracolumbar myofascial release technique reduce pain and disability in chronic low back pain? A randomized balanced crossover study. J. Clin. Med. 2021, 10, 2006. [Google Scholar] [CrossRef]
- Boutron, I.; Moher, D.; Altman, D.; Schulz, K.; Ravaud, P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: Explanation and elaboration. ACP J. Club. 2008, 148, 295–309. [Google Scholar] [CrossRef]
| Authors, Year | Country | Study Design | Mean Age in Years (SD) | Sample Size | Male/Female | |||
|---|---|---|---|---|---|---|---|---|
| EG | CG | EG | CG | EG | CG | |||
| Arguisuelas et al., 2017 [18] | Spain | Parallel RCT | 46.6 (10.3) | 46.4 (11.4) | 27 | 27 | 11/16 | 10/17 |
| Arguisuelas et al., 2019 [19] | Spain | Parallel RCT | 47.2 (9.8) | 48.6 (10.1) | 18 | 18 | 6/12 | 6/12 |
| Sakabe et al., 2020 [20] | Brazil | Parallel RCT | 30.7 (11.2) | CG: 32.1 (13.16) HCG: 27.4 (10.4) | 20 | 20 (CG)/20 (HG) | 25/35 | |
| Ożóg et al., 2021 [12] | Poland | Parallel RCT | 49.4 (5.9) | 48.9 (5.4) | 59 | 54 | 33/26 | 26/28 |
| Ożóg et al., 2023 [13] | Poland | Parallel RCT | 49.4 (5.9) | 48.9 (5.4) | 59 | 54 | 33/26 | 26/28 |
| Paulo et al., 2021 [21] | Brazil | Crossover RCT | 36 | All participants (n = 41) underwent three situations in a randomized and balanced order: EG, CG, PG | 16/25 | |||
| Authors, year | Intervention Length, Frequency, and Duration | Outcome Measures | Measurement Time | Main Findings | |
|---|---|---|---|---|---|
| EG | CG | ||||
| Arguisuelas et al., 2017 [18] | MFR (40 min. each; twice a week; 2 weeks) | Sham MFR | SF-MPQ VAS RMQ FABQ | Pre-treatment, week 2 (post-treatment), week 12 (follow-up) | MFR therapy in the EG resulted in a significant improvement in pain intensity and disability compared to the CG. The authors also concluded that although there were minimal clinically significant differences in pain and disability (within the 95% CI), it remains uncertain whether this improvement is clinically significant |
| Arguisuelas et al., 2019 [19] | MFR (40 min. each; twice a week; 2 weeks) | Sham MFR | SF-MPQ RMQ sEMG | Pre-treatment, week 2 (post-treatment) | The MFR protocol contributed to normalizing the flexion-relaxation response in individuals who did not show myoelectric silence before the intervention. Additionally, it also showed a significant reduction in pain intensity and disability compared to the CG |
| Sakabe et al., 2020 [20] | MFR (40 min. each; once a week; 3 weeks) | No intervention | VAS ODI Sit and Reach Test FTF test Measurement of lateral spine inclinations | Pre-treatment, immediately after the 1st MFR session, 7 days after the treatment (reevaluation), 1 month after the treatment (follow-up) | The MFR protocol led to a reduction in pain intensity and lumbar disability degree, along with improved mobility in subjects with CLBP as evaluated through the Sit and Reach and FTF tests. The effects lasted for a month after the end of treatment |
| Paulo et al., 2021 [21] | MFR (5 min.; single intervention) | CG: no intervention. PG: active trunk movements | NRPS PPT ODI | Pre-treatment, immediately after the MFR session | A single trial of a thoracolumbar MFR was insufficient to reduce pain intensity and disability in subjects with CLBP |
| Ożóg et al., 2021 [12] | MFR (40 min.; single intervention) | No intervention | sEMG | Pre-treatment, immediately after the MFR session, 1 month after the treatment (follow-up) | A single MFR treatment in the EG led to an immediate decrease in resting activity of the ES and MF muscles in the lumbodorsal spine area. Data collected one month after the treatment confirm the maintenance of the treatment effect in terms of muscular activity of the ES and MF muscles in the lumbosacral spine |
| Ożóg et al., 2023 [13] | MFR (40 min.; single intervention) | No intervention | Posturography | Pre-treatment, immediately after the MFR session, 1 month after the treatment (follow-up) | A single MFR treatment in the TLF did not aggravate postural stability immediately after the therapy in the EG. Moreover, after one month, postural stability did not improve compared with the results recorded before the treatment. The values of the stabilometric parameters one month after the intervention did not change significantly in the EG compared with the CG |
| Study/Criteria of the PEDro Scale | Arguisuelas, 2017 [18] | Arguisuelas, 2019 [19] | Sakabe, 2020 [20] | Paulo, 2021 [21] | Ożóg, 2021 [12] | Ożóg, 2023 [13] |
|---|---|---|---|---|---|---|
| Eligibility | + | + | + | + | + | + |
| Randomization | + | + | + | + | + | + |
| Allocation of subjects | + | + | - | - | + | + |
| Similar groups at baseline in terms of the most important prognostic indicators | + | + | + | + | + | + |
| Blinded subjects | + | + | - | - | - | - |
| Blinded therapist | - | - | - | - | - | - |
| Blinded evaluators | + | + | - | + | - | - |
| Adequate follow-up | + | + | + | + | + | + |
| Intention of treatment | + | + | + | + | + | + |
| Comparison between groups | + | + | + | + | + | + |
| Estimated points and variability | + | + | + | + | + | + |
| Total score | 9 | 9 | 6 | 7 | 7 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ożóg, P.; Weber-Rajek, M.; Radzimińska, A. Effects of Isolated Myofascial Release Therapy in Patients with Chronic Low Back Pain—A Systematic Review. J. Clin. Med. 2023, 12, 6143. https://doi.org/10.3390/jcm12196143
Ożóg P, Weber-Rajek M, Radzimińska A. Effects of Isolated Myofascial Release Therapy in Patients with Chronic Low Back Pain—A Systematic Review. Journal of Clinical Medicine. 2023; 12(19):6143. https://doi.org/10.3390/jcm12196143
Chicago/Turabian StyleOżóg, Piotr, Magdalena Weber-Rajek, and Agnieszka Radzimińska. 2023. "Effects of Isolated Myofascial Release Therapy in Patients with Chronic Low Back Pain—A Systematic Review" Journal of Clinical Medicine 12, no. 19: 6143. https://doi.org/10.3390/jcm12196143
APA StyleOżóg, P., Weber-Rajek, M., & Radzimińska, A. (2023). Effects of Isolated Myofascial Release Therapy in Patients with Chronic Low Back Pain—A Systematic Review. Journal of Clinical Medicine, 12(19), 6143. https://doi.org/10.3390/jcm12196143





