Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Sample
2.2. Measures
- •
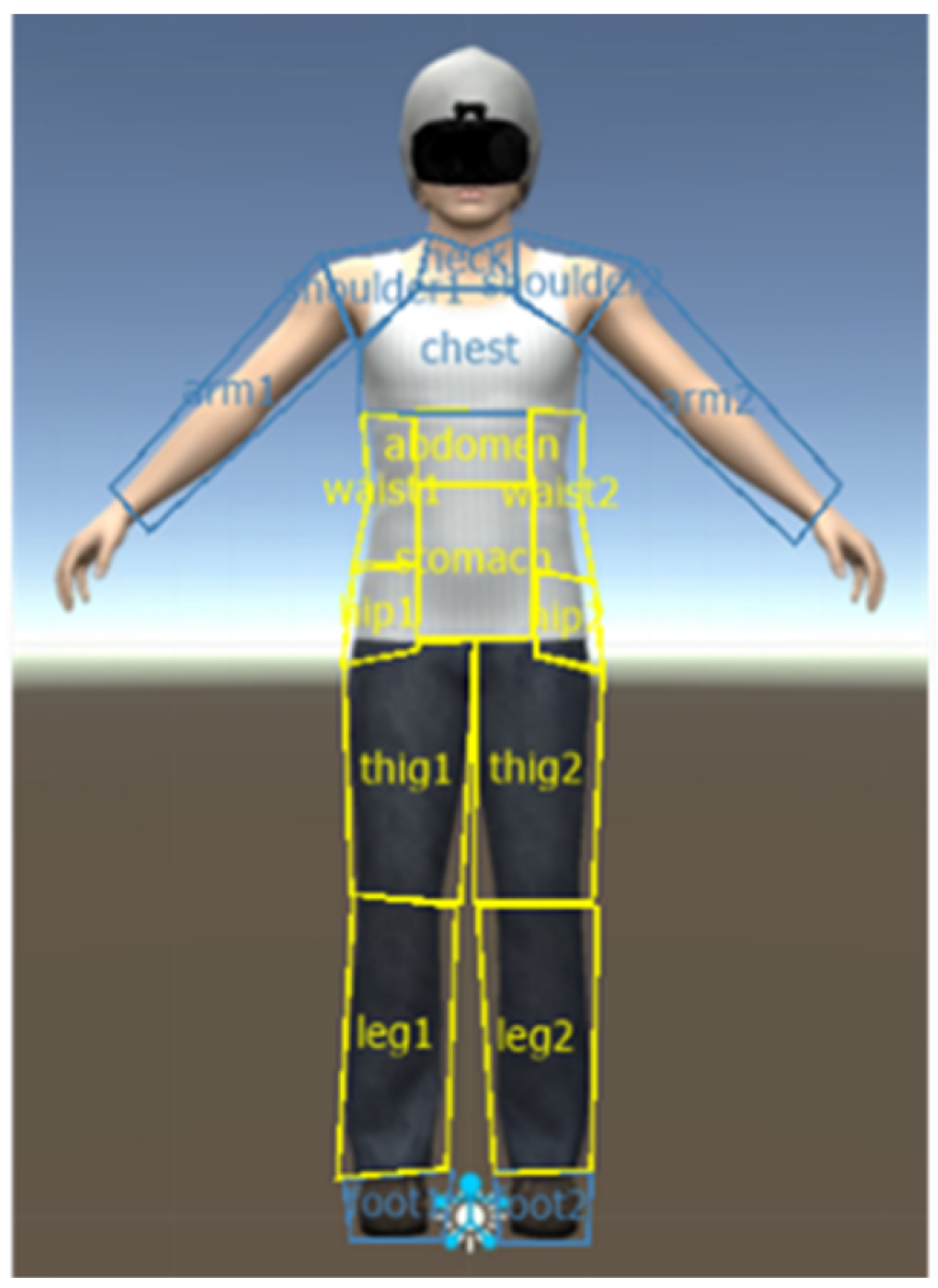
- Weight-related AOIs encompassed body regions commonly associated with measures of eating disorders, including the stomach, hips, waist, thighs, and legs.
- •
- Non-weight-related AOIs included body parts less correlated with eating disorders: neck, chest, shoulders, arms, and feet.
2.3. Instruments
2.4. Procedure
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crow, S. Eating disorders and risk of death. Am. J. Psychiatry 2013, 170, 824–825. [Google Scholar] [CrossRef] [PubMed]
- Favaro, A.; Caregaro, L.; Tenconi, E.; Bosello, R.; Santonastaso, P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J. Clin. Psychiatry 2009, 70, 1715–1721. [Google Scholar] [CrossRef]
- Goschke, T. Dysfunctions of decision-making and cognitive control as transdiagnostic mechanisms of mental disorders: Advances, gaps, and needs in current research. Int. J. Methods Psychiatr. Res. 2014, 23 (Suppl. S1), 41–57. [Google Scholar] [CrossRef]
- Lee, M.; Shafran, R. Information processing biases in eating disorders. Clin. Psychol. Rev. 2004, 24, 215–238. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; White, M.A.; York-Crowe, E.; Stewart, T.M. Cognitive-behavioral theories of eating disorders. Behav. Modif. 2004, 28, 711–738. [Google Scholar] [CrossRef]
- Bar-Haim, Y.; Lamy, D.; Pergamin, L.; Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychol. Bull. 2007, 133, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Olivares, L.; Marnet-Fiol, R.; Santos-Carrasco, I.M.; Borszewski, B.; et al. AN-VR-BE. A randomized controlled trial for reducing fear of gaining weight and other eating disorder symptoms in anorexia nervosa through virtual reality-based body exposure. J. Clin. Med. 2021, 10, 682. [Google Scholar] [CrossRef]
- Battagliese, G.; Lombardo, C. Attentional bias in psychopathology. Psicoter. Cogn. E Comport. 2011, 17, 75–98. [Google Scholar]
- Rodgers, R.F.; DuBois, R.H. Cognitive biases to appearance-related stimuli in body dissatisfaction: A systematic review. Clin. Psychol. Rev. 2016, 46, 1–11. [Google Scholar] [CrossRef]
- Stice, E.; Ng, J.; Shaw, H. Risk factors and prodromal eating pathology. J. Child Psychol. Psychiatry 2010, 51, 518–525. [Google Scholar] [CrossRef]
- Smith, E.; Rieger, E. The effect of attentional bias toward shape- and weight-related information on body dissatisfaction. Int. J. Eat. Disord. 2006, 39, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Glashouwer, K.A.; Masselman, I.; de Jong, P.J. Reducing body dissatisfaction by means of an evaluative conditioning procedure in undergraduate women: A replication study. Behav. Res. Ther. 2019, 121, 103435. [Google Scholar] [CrossRef] [PubMed]
- Cass, J.; Giltrap, G.; Talbot, D. Female body dissatisfaction and attentional bias to body images evaluated using visual search. Front. Psychol. 2020, 10, 2821. [Google Scholar] [CrossRef] [PubMed]
- Griffen, T.C.; Naumann, E.; Hildebrandt, T. Mirror exposure therapy for body image disturbances and eating disorders: A review. Clin. Psychol. Rev. 2018, 65, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Porras-Garcia, B.; Miquel, H.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez, J. The way we look at our own body really matters! Body-related attentional bias as a predictor of worse clinical outcomes after a virtual reality body exposure therapy. Annu. Rev. Cybertherapy Telemed. 2021, 19, 99. [Google Scholar]
- Renwick, B.; Campbell, I.C.; Schmidt, U. Attention bias modification: A new approach to the treatment of eating disorders? Int. J. Eat. Disord. 2013, 46, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Bar-Haim, Y. Research review: Attention bias modification (ABM): A novel treatment for anxiety disorders. J. Child Psychol. Psychiatry 2010, 51, 859–870. [Google Scholar] [CrossRef]
- Hallion, L.S.; Ruscio, A.M. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychol. Bull. 2011, 137, 940–958. [Google Scholar] [CrossRef]
- Dikstein, H.; Gilon-Mann, T.; Halevi-Yosef, R.; Enoch-Levi, A.; Hamdan, S.; Gur, E.; Haim, Y.B.; Lazarov, A.; Treasure, J.; Stein, D. Attention bias modification add-on to inpatient treatment for young women with anorexia nervosa—A randomized controlled trial. Eur. Eat. Disord. Rev. 2023, 31, 285–302. [Google Scholar] [CrossRef]
- Brockmeyer, T.; Friederich, H.C.; Küppers, C.; Chowdhury, S.; Harms, L.; Simmonds, J.; Gordon, G.; Potterton, R.; Schmidt, U. Approach bias modification training in bulimia nervosa and binge-eating disorder: A pilot randomized controlled trial. Int. J. Eat. Disord. 2019, 52, 520–529. [Google Scholar] [CrossRef]
- Schmitz, F.; Svaldi, J. Effects of bias modification training in binge eating disorder. Behav. Ther. 2017, 48, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.; Mulgrew, K.E.; Rune, K.; Allen, A. Attention bias for appearance words can be reduced in women: Results from a single-session attention bias modification task. J. Behav. Ther. Exp. Psychiatry 2018, 61, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Loughnan, S.A.; Mulgrew, K.E.; Lane, B.R. Attention bias modification produces no changes to appearance-related bias, state or trait body dissatisfaction in nonclinical women. Health Psychol. Open 2015, 2, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.; Rieger, E. The effect of attentional training on body dissatisfaction and dietary restriction. Eur. Eat. Disord. Rev. 2009, 17, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Engel, S.G.; Robinson, M.D.; Wonderlich, S.J.; Meier, B.P.; Wonderlich, S.A.; Crosby, R.D.; Steffen, K.J.; Mitchell, J.E. Does the avoidance of body and shape concerns reinforce eating disordered attitudes? Evidence from a manipulation study. Eat. Behav. 2006, 7, 368–374. [Google Scholar] [CrossRef]
- Smeets, E.; Jansen, A.; Roefs, A. Bias for the (un)attractive self: On the role of attention in causing body (dis)satisfaction. Health Psychol. 2011, 30, 360–367. [Google Scholar] [CrossRef]
- MacLeod, C.; Mathews, A.; Tata, P. Attentional bias in emotional disorders. J. Abnorm. Psychol. 1986, 95, 15–20. [Google Scholar] [CrossRef]
- Hertel, P.T.; Mathews, A. Cognitive bias modification: Past perspectives, current findings, and future applications. Perspect. Psychol. Sci. 2011, 6, 521–536. [Google Scholar] [CrossRef]
- Heeren, A.; Mogoașe, C.; Philippot, P.; McNally, R.J. Attention bias modification for social anxiety: A systematic review and meta-analysis. Clin. Psychol. Rev. 2015, 40, 76–90. [Google Scholar] [CrossRef]
- Clus, D.; Larsen, M.E.; Lemey, C.; Berrouiguet, S. The use of virtual reality in patients with eating disorders: Systematic review. J. Med. Internet Res. 2018, 20, e157. [Google Scholar] [CrossRef]
- Perpiñá, C.; Botella, C.; Baños, R.M. Virtual reality in eating disorders. Eur. Eat. Disord. Rev. 2003, 278, 261–278. [Google Scholar] [CrossRef]
- Gutiérrez-Maldonado, J.; Ferrer-García, M.; Dakanalis, A.; Riva, G. Virtual reality: Applications to eating disorders. In The Oxford Handbook of Eating Disorders, 2nd ed.; Agras, W.S., Robinson, A.H., Eds.; Oxford University Press: Oxford, UK, 2018; pp. 148–153. [Google Scholar]
- Pla-Sanjuanelo, J.; Ferrer-García, M.; Vilalta-Abella, F.; Riva, G.; Dakanalis, A.; Ribas-Sabaté, J.; Andreu-Gracia, A.; Fernandez-Aranda, F.; Sanchez-Diaz, I.; Escandón-Nagel, N.; et al. Testing virtual reality-based cue-exposure software: Which cue-elicited responses best discriminate between patients with eating disorders and healthy controls? Eat. Weight. Disord. 2017, 24, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Kerr-Gaffney, J.; Harrison, A.; Tchanturia, K. Eye-tracking research in eating disorders: A systematic review. Int. J. Eat. Disord. 2018, 52, 3–27. [Google Scholar] [CrossRef] [PubMed]
- Miquel-Nabau, H.; Briseño-Oloriz, N.; Porras-Garcia, B.; Ascione, M.; Meschberger-Annweiler, F.A.; Ferrer-Garcia, M.; Moreno-Sanchez, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez Maldonado, J. Modification of body-related attentional bias through virtual reality and eye-tracking in healthy participants: Implications for anorexia nervosa treatments. Brain Sci. 2023, 13, 764. [Google Scholar] [CrossRef] [PubMed]
- Meschberger-Annweiler, F.A.; Ascione, M.; Porras-Garcia, B.; Ferrer-Garcia, M.; Moreno-Sanchez, M.; Miquel-Nabau, H.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez-Maldonado, J. An attentional bias modification task, through virtual reality and eye-tracking technologies, to enhance the treatment of anorexia nervosa. J. Clin. Med. 2023, 12, 2185. [Google Scholar] [CrossRef] [PubMed]
- Herpertz-Dahlmann, B.; Dempfle, A.; Egberts, K.M.; Kappel, V.; Konrad, K.; Vloet, J.A.; Bühren, K. Outcome of childhood anorexia nervosa—The results of a five- to ten-year follow-up study. Int. J. Eat. Disord. 2018, 51, 295–304. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height-Forage, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Gardner, R.M.; Jappe, L.M.; Gardner, L. Development and validation of a new figural drawing scale for body-image assessment: The BIAS-BD. J. Clin. Psychol. 2009, 65, 113–122. [Google Scholar] [CrossRef]
- Reed, D.L.; Thompson, J.K.; Brannick, M.T.; Sacco, W.P. Development and validation of the Physical Appearance State and Trait Anxiety Scale (PASTAS). J. Anxiety Disord. 1991, 5, 323–332. [Google Scholar] [CrossRef]
- Jacob, R.J.K.; Karn, K.S. Eye tracking in human-computer interaction and usability research: Ready to deliver the promises. In The Mind’s Eye: Cognitive and Applied Aspects of Eye Movement Research; Hyönä, J., Radach, R., Deubel, H., Eds.; Elsevier: Amsterdam, The Netherlands, 2003; pp. 573–605. [Google Scholar]
- Jiang, M.Y.W.; Vartanian, L.R. A review of existing measures of attentional biases in body image and eating disorders research: Attentional measures in body image research. Aust. J. Psychol. 2018, 70, 3–17. [Google Scholar] [CrossRef]
- Bauer, A.; Schneider, S.; Waldorf, M.; Braks, K.; Huber, T.J.; Adolph, D.; Vocks, S. Selective visual attention towards oneself and associated state body satisfaction: An eye-tracking study in adolescents with different types of eating disorders. J. Abnorm. Child Psychol. 2017, 45, 1647–1661. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Yilmaz, L.; Sen, Y.O.; Olszewska, A.; Ghita, A.; Serrano-Troncoso, E.; Treasure, J.; Gutiérrez-Maldonado, J. Body-related attentional bias as mediator of the relationship between body mass index and body dissatisfaction. Eur. Eat. Disord. Rev. 2020, 28, 454–464. [Google Scholar] [CrossRef]
- Waltemate, T.; Gall, D.; Roth, D.; Botsch, M.; Latoschik, M.E. The impact of avatar personalization and immersion on virtual body ownership, presence, and emotional response. IEEE Trans. Vis. Comput. Graph. 2018, 24, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K.; Riva, G.; Gutiérrez-Maldonado, J. Virtual reality in the assessment and treatment of weight-related disorders. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 67–73. [Google Scholar] [CrossRef]
- Lazarov, A.; Abend, R.; Seidner, S.; Pine, D.S.; Bar-Haim, Y. The effects of training contingency awareness during attention bias modification on learning and stress reactivity. Behav. Ther. 2017, 48, 638–650. [Google Scholar] [CrossRef]
- MacLeod, C.; Koster, E.H.; Fox, E. Whither cognitive bias modification research? Commentary on the special section articles. J. Abnorm. Psychol. 2009, 118, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Tuschen-Caffier, B.; Bender, C.; Caffier, D.; Klenner, K.; Braks, K.; Svaldi, J. Selective visual attention during mirror exposure in anorexia and bulimia nervosa. PLoS ONE 2015, 10, e0145886. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T. Cognitive Therapy and the Emotional Disorders; International University Press: New York, NY, USA, 1976. [Google Scholar]
- Clark, D.M. Anxiety disorders: Why they persist and how to treat them. Behav. Res. Ther. 1999, 37 (Suppl. S1), S5–S27. [Google Scholar] [CrossRef] [PubMed]
- Mogg, K.; Bradley, B.P. A cognitive-motivational analysis of anxiety. Behav. Res. Ther. 1998, 36, 809–848. [Google Scholar] [CrossRef]
- Poole, A.; Ball, L.J.; Phillips, P. In search of salience: A response time and eye movement analysis of bookmark recognition. In People and Computers XVIII-Design for Life: Proceedings of HCI 2004; Fincher, S., Markopolous, P., Moore, D., Ruddle, R., Eds.; Springer: London, UK, 2004; pp. 363–378. [Google Scholar]
- Yarbus, A.L. Eye Movements and Vision; Plenum Press: New York, NY, USA, 1967. [Google Scholar]
- Fisher, D.F.; Monty, R.A.; Senders, J.W. Eye Movements: Cognition and Visual Perception; Routledge: Oxfordshire, UK, 2017; Volume 8. [Google Scholar]
- Goldberg, J.H.; Kotval, X.P. Computer interface evaluation using eye movements: Methods and constructs. Int. J. Ind. Ergon. 1999, 24, 631–645. [Google Scholar] [CrossRef]
- LeDoux, J.E.; Pine, D.S. Using neuroscience to help understand fear and anxiety: A two-system framework. Am. J. Psychiatry 2016, 173, 1083–1093. [Google Scholar] [CrossRef]
- Shechner, T.; Bar-Haim, Y. Threat monitoring and attention-bias modification in anxiety and stress-related disorders. Curr. Dir. Psychol. Sci. 2016, 25, 431–437. [Google Scholar] [CrossRef]
- Corbetta, M.; Shulman, G.L. Control of goal-directed and stimulus-driven attention in the brain. Nat. Rev. Neurosci. 2002, 3, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Yiend, J. The effects of emotion on attention: A review of attentional processing of emotional information. Cogn. Emot. 2010, 24, 3–47. [Google Scholar] [CrossRef]
- Eysenck, M.W.; Derakshan, N.; Santos, R.; Calvo, M.G. Anxiety and cognitive performance: Attentional control theory. Emotion 2007, 7, 336–353. [Google Scholar] [CrossRef]
- Hakamata, Y.; Lissek, S.; Bar-Haim, Y.; Britton, J.C.; Fox, N.A.; Leibenluft, E.; Ernst, M.; Pine, D.S. Attention bias modification treatment: A meta-analysis toward the establishment of novel treatment for anxiety. Biol. Psychiatry 2010, 68, 982–990. [Google Scholar] [CrossRef]
- Balleine, B.W.; O’Doherty, J.P. Human and rodent homologies in action control: Corticostriatal determinants of goal-directed and habitual action. Neuropsychopharmacology 2010, 35, 48–69. [Google Scholar] [CrossRef] [PubMed]
- Pine, D.S.; Helfinstein, S.M.; Bar-Haim, Y.; Nelson, E.; Fox, N.A. Challenges in developing novel treatments for childhood disorders: Lessons from research on anxiety. Neuropsychopharmacology 2009, 34, 213–228. [Google Scholar] [CrossRef]
- Browning, M.; Holmes, E.A.; Murphy, S.E.; Goodwin, G.M.; Harmer, C.J. Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biol. Psychiatry 2009, 67, 919–925. [Google Scholar] [CrossRef]
- Grafton, B.; MacLeod, C.; Rudaizky, D.; Holmes, E.A.; Salemink, E.; Fox, E.; Notebaert, L. Confusing procedures with process when appraising the impact of cognitive bias modification on emotional vulnerability. Br. J. Psychiatry 2017, 211, 266–271. [Google Scholar] [CrossRef]
- Kuckertz, J.M.; Amir, N. Attention bias modification for anxiety and phobias: Current status and future directions. Curr. Psychiatry Rep. 2015, 17, 9. [Google Scholar] [CrossRef]
- MacLeod, C.; Clarke, P.J.F. The attentional bias modification approach to anxiety intervention. Clin. Psychol. Sci. 2015, 3, 58–78. [Google Scholar] [CrossRef]
- Mouatt, B.; Smith, A.; Mellow, M.; Parfitt, G.; Smith, R.; Stanton, T. The use of virtual reality to influence motivation, affect, enjoyment, and engagement during exercise: A scoping review. Front. Virtual Real. 2020, 1, 564664. [Google Scholar] [CrossRef]
- Boendermaker, W.J.; Prins, P.J.; Wiers, R.W. Cognitive bias modification for adolescents with substance use problems—Can serious games help? J. Behav. Ther. Exp. Psychiatry 2015, 49 Pt A, 13–20. [Google Scholar] [CrossRef]
- Gorrell, S.; Murray, S.B. Eating disorders in males. Child Adolesc. Psychiatr. Clin. 2019, 28, 641–651. [Google Scholar] [CrossRef]
- Fiske, L.; Fallon, E.A.; Blissmer, B.; Redding, C.A. Prevalence of body dissatisfaction among United States adults: Review and recommendations for future research. Eat. Behav. 2014, 15, 357–365. [Google Scholar] [CrossRef] [PubMed]

| Clinical Characteristic | Number of Patients |
|---|---|
| Subtype of anorexia nervosa | |
| Restrictive Anorexia Nervosa | 22 |
| Purgative Anorexia Nervosa | 1 |
| Comorbidities | |
| Major Depressive Disorder | 2 |
| Major Depressive Disorder and Mild Intellectual Disability | 1 |
| Post-Traumatic Stress Disorder | 1 |
| Social Anxiety Disorder | 2 |
| Obsessive Compulsive Disorder | 1 |
| Pharmacological Treatment | |
| Antipsychotics | 2 |
| Antidepressants | 11 |
| Anxiolytics | 2 |
| Antipsychotics and Antidepressants | 8 |
| Antipsychotics and Anxiolytics | 1 |
| Antidepressants and Anxiolytics | 4 |
| Antidepressants, Anxiolytics, and Antipsychotics | 4 |
| Pre-Assessment Time | Post-Assessment Time | Paired Samples t-Test | Effect Size | ||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | t | p | Cohen’s d * | |
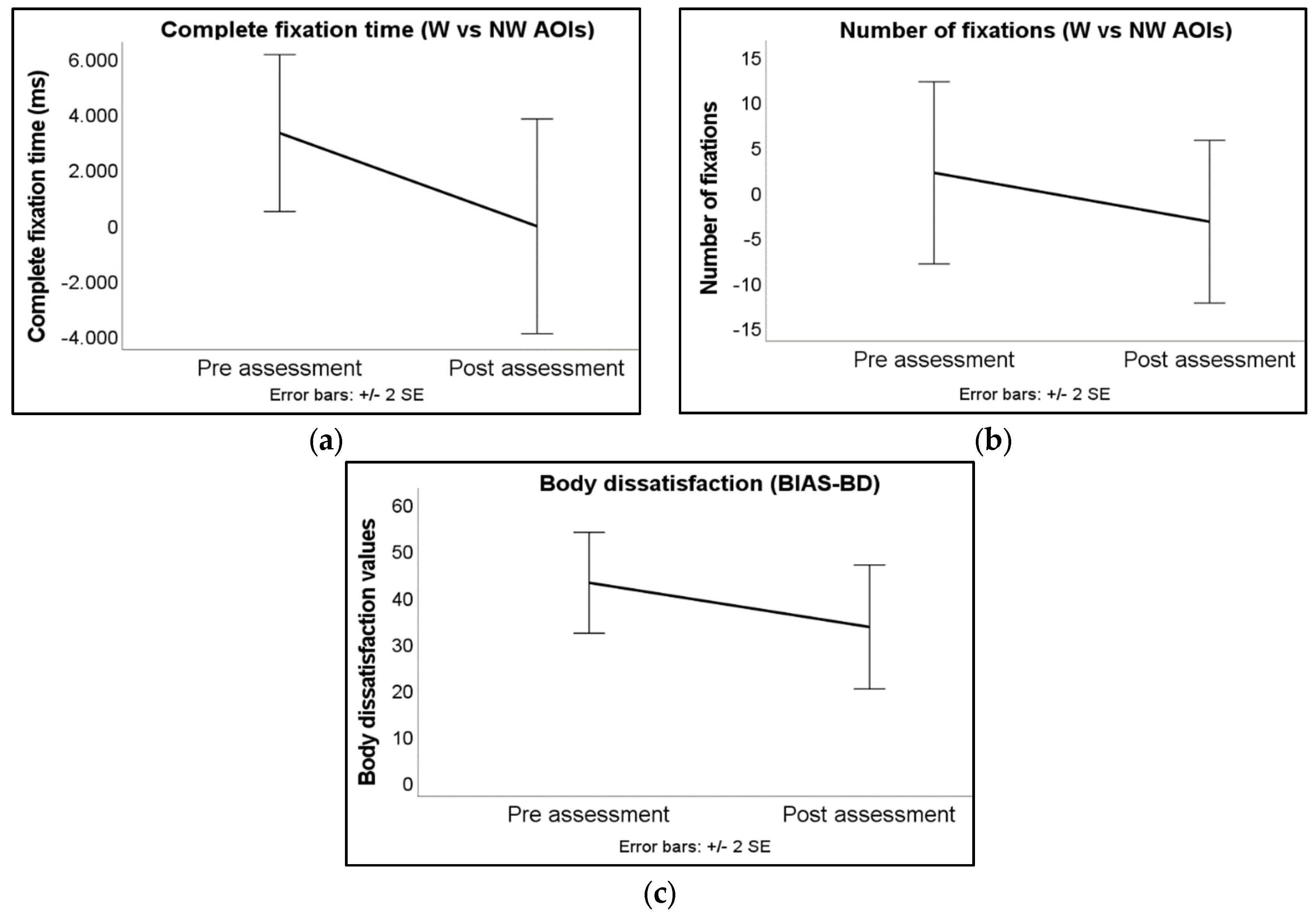
| Complete fixation time (in ms) | 3269.88 (5837.05) | −94.88 (7988.81) | 1.863 | * 0.040 | 0.452 |
| Body dissatisfaction | 42.83 (26.14) | 33.26 (32.14) | 1.880 | * 0.037 | 0.392 |
| Pre-Assessment Time | Post-Assessment Time | Wilcoxon Signed-Rank Test | Effect Size | ||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | z | p | r2 * | |
| Number of fixations | 2.00 (20.80) | −3.41 (18.56) | −0.592 | 0.554 | −0.100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ascione, M.; Carulla-Roig, M.; Miquel-Nabau, H.; Porras-Garcia, B.; Meschberger-Annweiler, F.-A.; Serrano-Troncoso, E.; Ferrer-Garcia, M.; Moreno-Sánchez, M.; Gutierrez-Maldonado, J. Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients. J. Clin. Med. 2023, 12, 5932. https://doi.org/10.3390/jcm12185932
Ascione M, Carulla-Roig M, Miquel-Nabau H, Porras-Garcia B, Meschberger-Annweiler F-A, Serrano-Troncoso E, Ferrer-Garcia M, Moreno-Sánchez M, Gutierrez-Maldonado J. Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients. Journal of Clinical Medicine. 2023; 12(18):5932. https://doi.org/10.3390/jcm12185932
Chicago/Turabian StyleAscione, Mariarca, Marta Carulla-Roig, Helena Miquel-Nabau, Bruno Porras-Garcia, Franck-Alexandre Meschberger-Annweiler, Eduardo Serrano-Troncoso, Marta Ferrer-Garcia, Manuel Moreno-Sánchez, and Jose Gutierrez-Maldonado. 2023. "Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients" Journal of Clinical Medicine 12, no. 18: 5932. https://doi.org/10.3390/jcm12185932
APA StyleAscione, M., Carulla-Roig, M., Miquel-Nabau, H., Porras-Garcia, B., Meschberger-Annweiler, F.-A., Serrano-Troncoso, E., Ferrer-Garcia, M., Moreno-Sánchez, M., & Gutierrez-Maldonado, J. (2023). Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients. Journal of Clinical Medicine, 12(18), 5932. https://doi.org/10.3390/jcm12185932






