Cemented Sacroiliac Screw Fixation versus Conservative Therapy in Fragility Fractures of the Posterior Pelvic Ring: A Matched-Pair Analysis of a Prospective Observational Study
Abstract
:1. Introduction
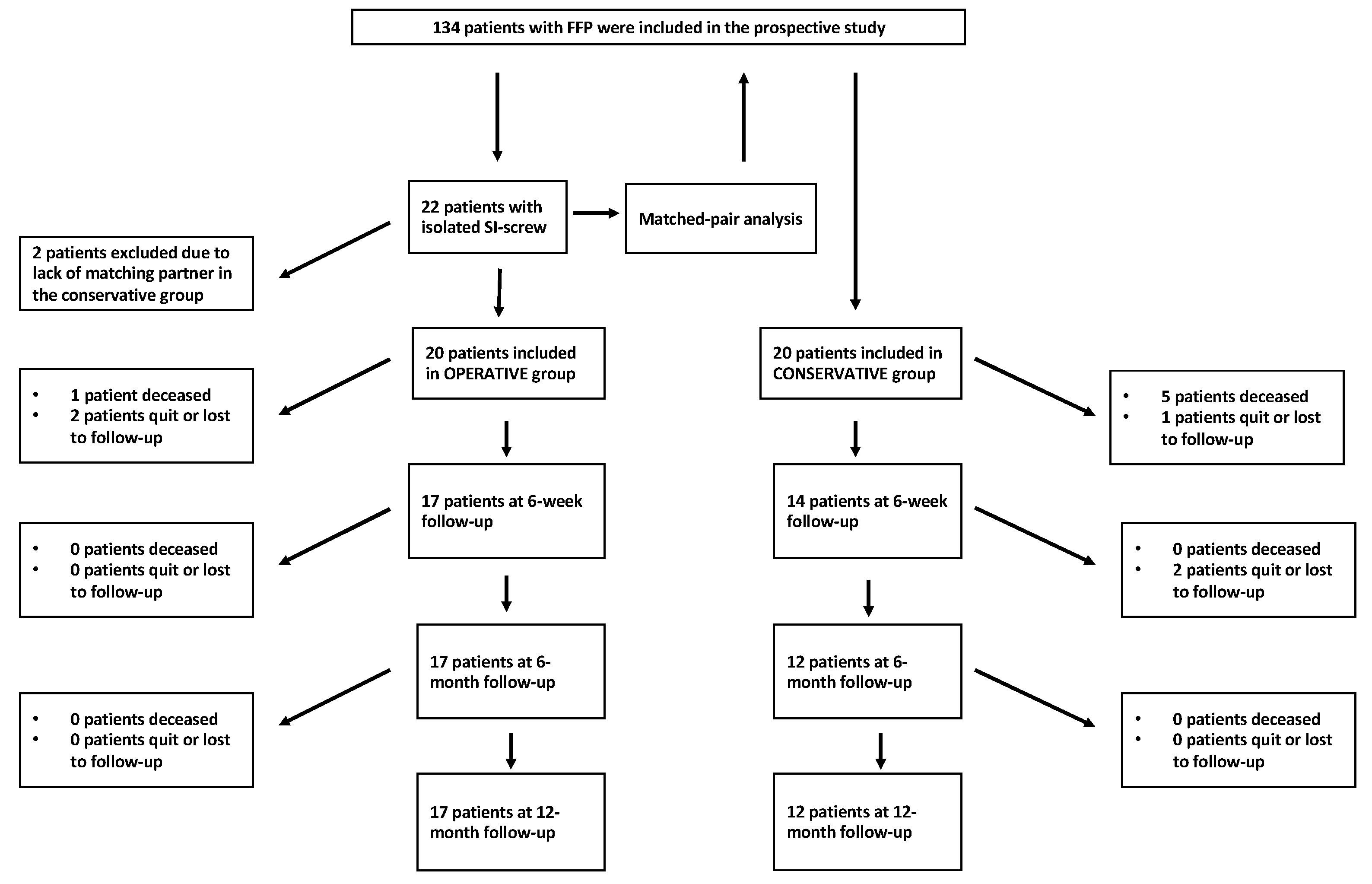
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buller, L.T.; Best, M.J.; Quinnan, S.M. A Nationwide Analysis of Pelvic Ring Fractures: Incidence and Trends in Treatment, Length of Stay, and Mortality. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 9–17. [Google Scholar] [CrossRef]
- Kannus, P.; Parkkari, J.; Niemi, S.; Sievänen, H. Low-Trauma Pelvic Fractures in Elderly Finns in 1970–2013. Calcif. Tissue Int. 2015, 97, 577–580. [Google Scholar] [CrossRef]
- Andrich, S.; Haastert, B.; Neuhaus, E.; Neidert, K.; Arend, W.; Ohmann, C.; Grebe, J.; Vogt, A.; Jungbluth, P.; Rösler, G.; et al. Epidemiology of Pelvic Fractures in Germany: Considerably High Incidence Rates among Older People. PLoS ONE 2015, 10, e0139078. [Google Scholar] [CrossRef]
- Maier, G.S.; Kolbow, K.; Lazovic, D.; Horas, K.; Roth, K.E.; Seeger, J.B.; Maus, U. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch. Gerontol. Geriatr. 2016, 67, 80–85. [Google Scholar] [CrossRef]
- Rommens, P.M.; Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013, 44, 1733–1744. [Google Scholar] [CrossRef]
- Oberkircher, L.; Ruchholtz, S.; Rommens, P.M.; Hofmann, A.; Bücking, B.; Krüger, A. Osteoporotic Pelvic Fractures. Dtsch. Arztebl. Int. 2018, 115, 70–80. [Google Scholar] [CrossRef]
- Breuil, V.; Roux, C.H.; Testa, J.; Albert, C.; Chassang, M.; Brocq, O.; Euller-Ziegler, L. Outcome of osteoporotic pelvic fractures: An underestimated severity. Survey of 60 cases. Jt. Bone Spine 2008, 75, 585–588. [Google Scholar] [CrossRef]
- Rommens, P.M.; Arand, C.; Hopf, J.C.; Mehling, I.; Dietz, S.O.; Wagner, D. Progress of instability in fragility fractures of the pelvis: An observational study. Injury 2019, 50, 1966–1973. [Google Scholar] [CrossRef]
- Ueda, Y.; Inui, T.; Kurata, Y.; Tsuji, H.; Saito, J.; Shitan, Y. Prolonged pain in patients with fragility fractures of the pelvis may be due to fracture progression. Eur. J. Trauma. Emerg. Surg. 2021, 47, 507–513. [Google Scholar] [CrossRef]
- Höch, A.; Pieroh, P.; Gras, F.; Hohmann, T.; Märdian, S.; Holmenschlager, F.; Keil, H.; Palm, H.-G.; Herath, S.C.; Josten, C.; et al. Age and “general health”-beside fracture classification-affect the therapeutic decision for geriatric pelvic ring fractures: A German pelvic injury register study. Int. Orthop. 2019, 43, 2629–2636. [Google Scholar] [CrossRef]
- Rommens, P.M.; Arand, C.; Hofmann, A.; Wagner, D. When and How to Operate Fragility Fractures of the Pelvis? Indian. J. Orthop. 2019, 53, 128–137. [Google Scholar] [CrossRef]
- Oberkircher, L.; Lenz, J.; Bücking, B.; Eschbach, D.; Aigner, R.; Bliemel, C.; Schoeneberg, C.; Ruchholtz, S.; Hack, J. Which factors influence treatment decision in fragility fractures of the pelvis?—Results of a prospective study. BMC Musculoskelet. Disord. 2021, 22, 690. [Google Scholar] [CrossRef] [PubMed]
- Saklad, M. Grading of patients for surgical procedures. Anesthesiology 1941, 2, 281–284. [Google Scholar] [CrossRef]
- Lübke, N.; Meinck, M.; Von Renteln-Kruse, W. The Barthel Index in geriatrics. A context analysis for the Hamburg Classification Manual. Z. Gerontol. Geriatr. 2004, 37, 316–326. [Google Scholar] [CrossRef]
- Hinz, A.; Klaiberg, A.; Brähler, E.; König, H.H. The Quality of Life Questionnaire EQ-5D: Modelling and norm values for the general population. Psychother. Psychosom. Med. Psychol. 2006, 56, 42–48. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Van Gulik, T.M.; Raaymakers, E.L.; Broekhuizen, A.H.; Karthaus, A.J. Complications and late therapeutic results of conservatively managed, unstable pelvic ring disruptions. Neth. J. Surg. 1987, 39, 175–178. [Google Scholar] [PubMed]
- Miranda, M.A.; Riemer, B.L.; Butterfield, S.L.; Burke, C.J. Pelvic ring injuries. A long term functional outcome study. Clin. Orthop. Relat. Res. 1996, 329, 152–159. [Google Scholar] [CrossRef]
- Henderson, R.C. The long-term results of nonoperatively treated major pelvic disruptions. J. Orthop. Trauma 1989, 3, 41–47. [Google Scholar] [CrossRef]
- Chen, P.H.; Hsu, W.H.; Li, Y.Y.; Huang, T.W.; Huang, T.J.; Peng, K.T. Outcome analysis of unstable posterior ring injury of the pelvis: Comparison between percutaneous iliosacral screw fixation and conservative treatment. Biomed. J. 2013, 36, 289–294. [Google Scholar]
- Grubor, P.; Milicevic, S.; Biscevic, M.; Tanjga, R. Selection of treatment method for pelvic ring fractures. Med. Arh. 2011, 65, 278–282. [Google Scholar] [CrossRef]
- Höch, A.; Pieroh, P.; Henkelmann, R.; Josten, C.; Böhme, J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: A prospective, observational study with 1-year follow-up. BMC Surg. 2017, 17, 132. [Google Scholar] [CrossRef] [PubMed]
- Höch, A.; Özkurtul, O.; Pieroh, P.; Josten, C.; Böhme, J. Outcome and 2-Year Survival Rate in Elderly Patients with Lateral Compression Fractures of the Pelvis. Geriatr. Orthop. Surg. Rehabil. 2017, 8, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Hopf, J.C.; Krieglstein, C.F.; Müller, L.P.; Koslowsky, T.C. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury 2015, 46, 1631–1636. [Google Scholar] [CrossRef]
- Morris, R.O.; Sonibare, A.; Green, D.J.; Masud, T. Closed pelvic fractures: Characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad. Med. J. 2000, 76, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Reito, A.; Kuoppala, M.; Pajulammi, H.; Hokkinen, L.; Kyrölä, K.; Paloneva, J. Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: A comparison with an age-matched femoral neck fracture cohort and general population. BMC Geriatr. 2019, 19, 315. [Google Scholar] [CrossRef] [PubMed]


| FFP Classification | Conservative | Sacroiliac Screw |
|---|---|---|
| IIa | n = 4 (20%) | n = 4 (20%) |
| IIb | n = 11 (55%) | n = 11 (55%) |
| IIc | n = 4 (20%) | n = 4 (20%) |
| IIIb | n = 1 (5%) | n = 1 (5%) |
| Conservative | Sacroiliac Screw | p Value | |
|---|---|---|---|
| Age | 82.1 ± 5.5 years | 80.8 ± 6.8 years | 0.511 |
| Gender (male/female) | 2/18 | 4/16 | 0.376 |
| BMI | 25.6 ± 4.4 kg/m2 | 26.3 ± 4.7 kg/m2 | 0.741 |
| ASA score | 2.9 ± 0.9 | 2.7 ± 0.5 | 0.531 |
| MMST | 22.3 ± 6.4 | 23.7 ± 5.9 | 0.533 |
| Barthel index pre-fracture | 85.5 ± 17.7 | 88.5 ± 12.2 | 0.925 |
| Mobility pre-fracture | 13.3 ± 2.9 | 14.5 ± 1.5 | 0.277 |
| Hospital stay | 8.6 ± 2.9 | 13.3 ± 4.1 | <0.001 |
| Operation time | - | 38.4 ± 16.5 | |
| Admission—surgery (d) | - | 4.9 ± 3.4 |
| Conservative | Sacroiliac Screw | p Value | |
|---|---|---|---|
| VAS admission | 8.5 ± 1.5 | 7.5 ± 2.5 | 0.258 |
| VAS day 4 | 3.5 ± 1.8 | 3.9 ± 2.3 | 0.540 |
| VAS 6 weeks | 3.4 ± 2.8 | 2.3 ± 2.4 | 0.231 |
| VAS 6 months | 2.1 ± 2.7 | 2.4 ± 3.1 | 0.981 |
| VAS 12 months | 2.0 ± 2.7 | 1.9 ± 2.9 | 0.905 |
| Conservative | Sacroiliac Screw | p Value | |
|---|---|---|---|
| Barthel pre-injury | 85.5 ± 17.7 | 88.5 ± 12.2 | 0.925 |
| Barthel admission | 42.0 ± 24.8 | 33.4 ± 15.9 | 0.209 |
| Barthel 6 weeks | 55.6 ± 31.2 | 74.2 ± 23.5 | 0.051 |
| Barthel 6 months | 58.8 ± 26.6 | 76.8 ± 17.3 | 0.036 |
| Barthel 12 months | 67.5 ± 24.7 | 75.6 ± 18.0 | 0.322 |
| Conservative | Sacroiliac Screw | p Value | |
|---|---|---|---|
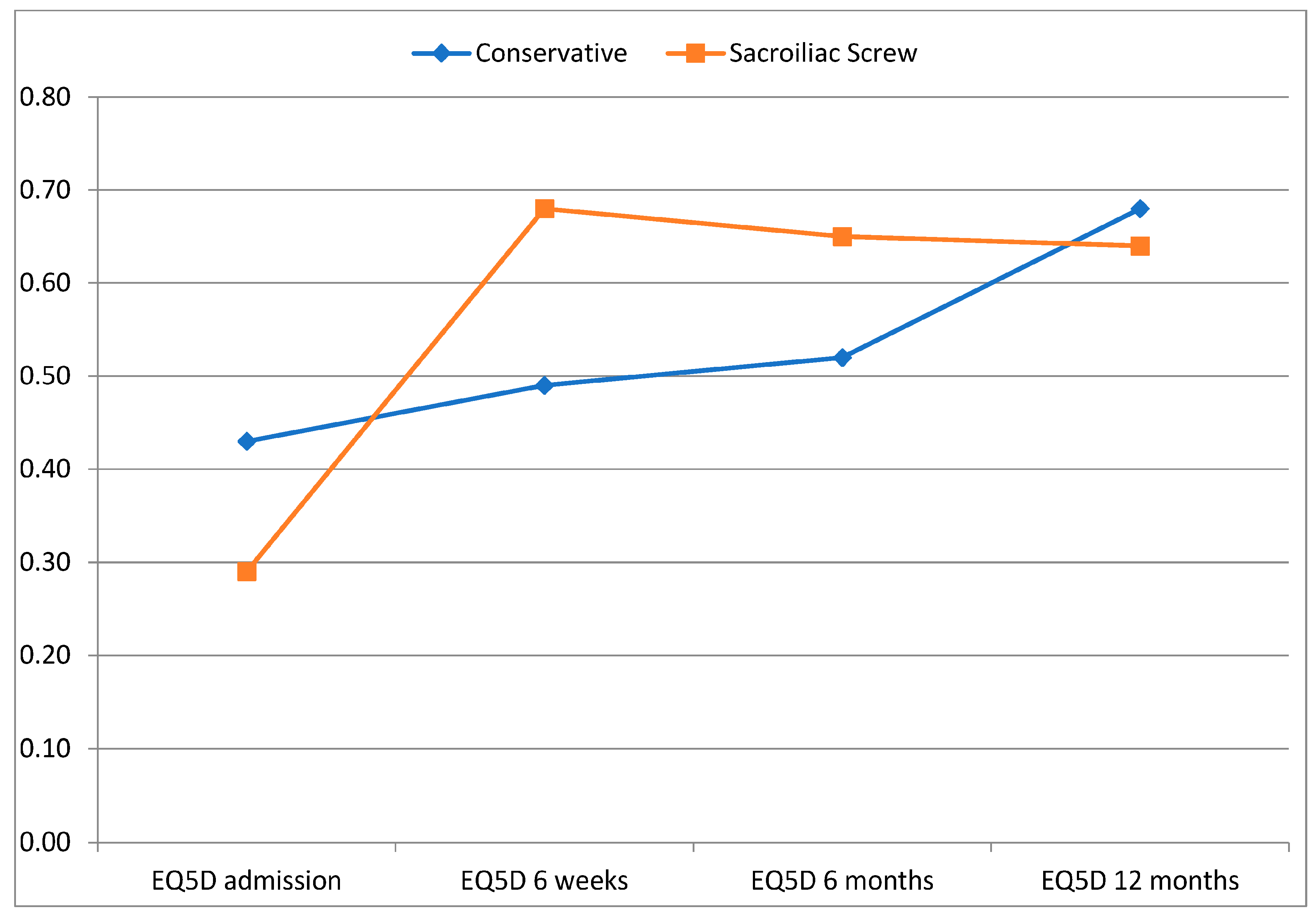
| EQ-5D admission | 0.43 ± 0.24 | 0.29 ± 0.15 | 0.026 |
| EQ-5D 6 weeks | 0.49 ± 0.25 | 0.68 ± 0.23 | 0.030 |
| EQ-5D 6 months | 0.52 ± 0.25 | 0.65 ± 0.27 | 0.204 |
| EQ-5D 12 months | 0.68 ± 0.22 | 0.64 ± 0.30 | 0.681 |
| Conservative | Sacroiliac Screw | p Value | |
|---|---|---|---|
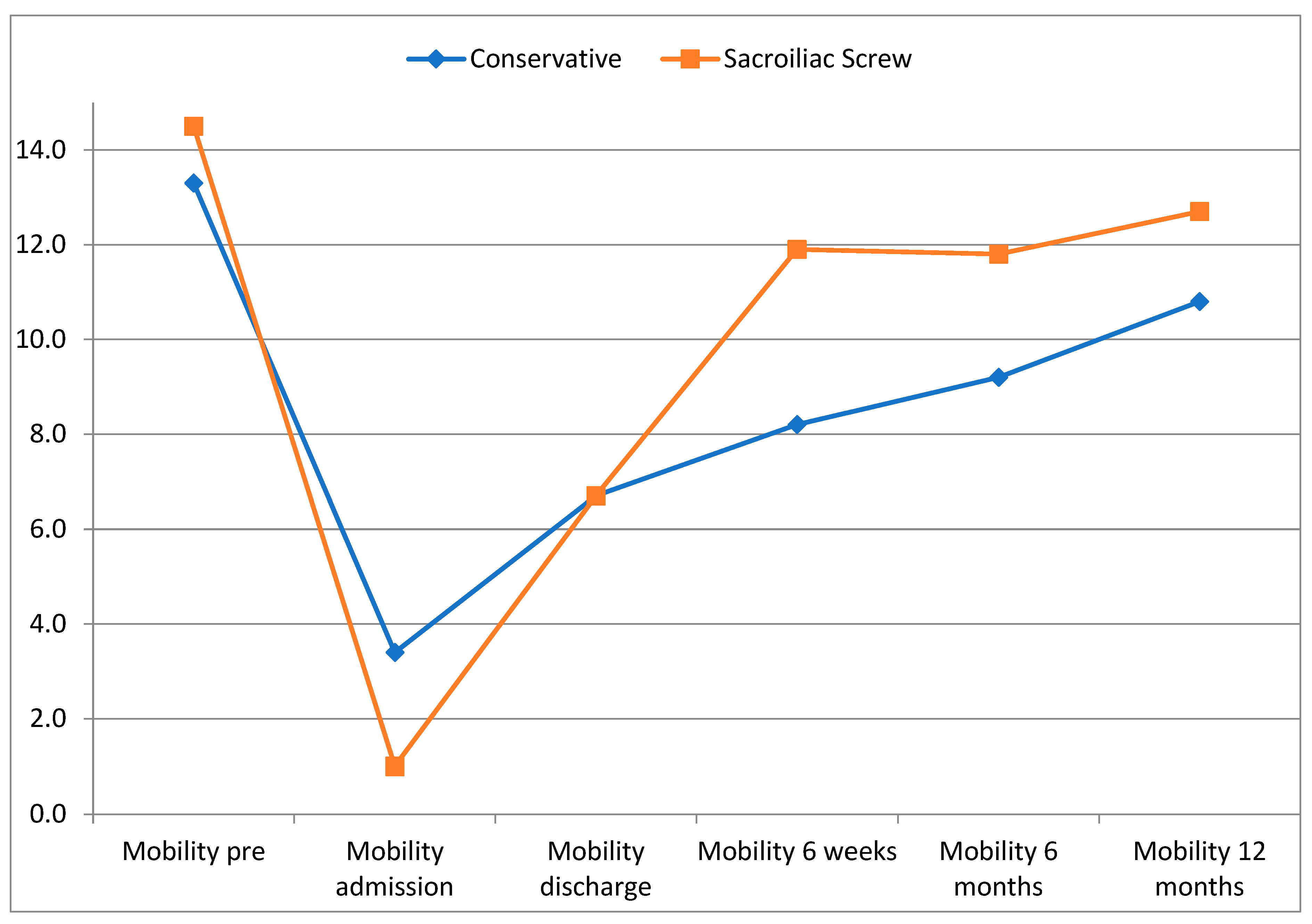
| Mobility pre-fracture | 13.3 ± 2.9 | 14.5 ± 1.5 | 0.277 |
| Mobility admission | 3.4 ± 5.0 | 1.0 ± 3.1 | 0.166 |
| Mobility discharge | 6.7 ± 5.6 | 6.7 ± 4.9 | 0.986 |
| Mobility 6 weeks | 8.2 ± 4.7 | 11.9 ± 4.2 | 0.019 |
| Mobility 6 months | 9.2 ± 4.5 | 11.8 ± 3.0 | 0.145 |
| Mobility 12 months | 10.8 ± 4.2 | 12.7 ± 3.1 | 0.263 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aigner, R.; Föhr, J.; Lenz, J.; Knauf, T.; Bäumlein, M.; Ruchholtz, S.; Oberkircher, L.; Hack, J. Cemented Sacroiliac Screw Fixation versus Conservative Therapy in Fragility Fractures of the Posterior Pelvic Ring: A Matched-Pair Analysis of a Prospective Observational Study. J. Clin. Med. 2023, 12, 5850. https://doi.org/10.3390/jcm12185850
Aigner R, Föhr J, Lenz J, Knauf T, Bäumlein M, Ruchholtz S, Oberkircher L, Hack J. Cemented Sacroiliac Screw Fixation versus Conservative Therapy in Fragility Fractures of the Posterior Pelvic Ring: A Matched-Pair Analysis of a Prospective Observational Study. Journal of Clinical Medicine. 2023; 12(18):5850. https://doi.org/10.3390/jcm12185850
Chicago/Turabian StyleAigner, Rene, Jan Föhr, Julia Lenz, Tom Knauf, Martin Bäumlein, Steffen Ruchholtz, Ludwig Oberkircher, and Juliana Hack. 2023. "Cemented Sacroiliac Screw Fixation versus Conservative Therapy in Fragility Fractures of the Posterior Pelvic Ring: A Matched-Pair Analysis of a Prospective Observational Study" Journal of Clinical Medicine 12, no. 18: 5850. https://doi.org/10.3390/jcm12185850
APA StyleAigner, R., Föhr, J., Lenz, J., Knauf, T., Bäumlein, M., Ruchholtz, S., Oberkircher, L., & Hack, J. (2023). Cemented Sacroiliac Screw Fixation versus Conservative Therapy in Fragility Fractures of the Posterior Pelvic Ring: A Matched-Pair Analysis of a Prospective Observational Study. Journal of Clinical Medicine, 12(18), 5850. https://doi.org/10.3390/jcm12185850






