Sex-Comparative Outcomes of the T-Branch Device for the Treatment of Complex Aortic Aneurysms
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Patient Cohort
2.2. Data Collection
2.3. Definitions
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Total Cohort
3.2. Baseline Characteristics
3.3. Intra-Operative Details
3.4. Early Outcomes
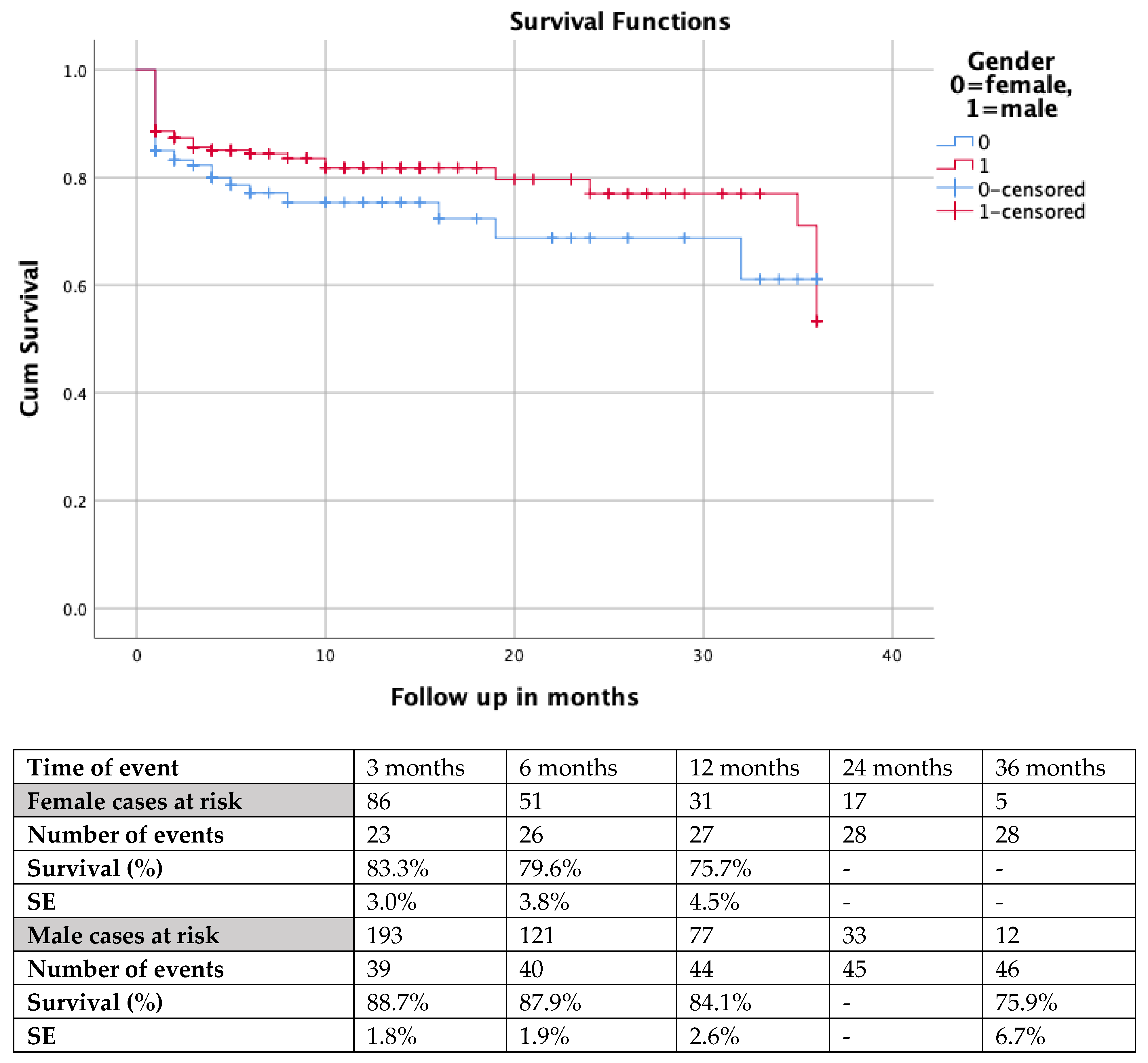
3.5. Follow-Up Findings
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nana, P.; Spanos, K.; Behrent, C.A.; Dakis, K.; Brotis, A.; Kouvelos, G.; Giannoukas, A.; Kölbel, T. Editor’s Choice-Sex Specific Outcomes After Complex Fenestrated and Branched Endovascular Aortic Repair: A Systematic Review and Meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2022, 64, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Erben, Y.; Bews, K.A.; Hanson, K.T.; Da Rocha-Franco, J.A.; Money, S.R.; Stone, W.; Farres, H.; Meltzer, A.J.; Gloviczki, P.; Oderich, G.S.; et al. Female Sex is a Marker for Higher Morbidity and Mortality after Elective Endovascular Aortic Aneurysm Repair: A National Surgical Quality Improvement Program Analysis. Ann. Vasc. Surg. 2020, 69, 1–8. [Google Scholar] [CrossRef]
- Pouncey, A.L.; David, M.; Morris, R.I.; Ulug, P.; Martin, G.; Bicknell, C.; Powell, J.T. Editor’s Choice-Systematic Review and Meta-Analysis of Sex Specific Differences in Adverse Events After Open and Endovascular Intact Abdominal Aortic Aneurysm Repair: Consistently Worse Outcomes for Women. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Nana, P.; Dakis, K.; Brotis, A.; Spanos, K.; Kouvelos, G.; Spanos, K.; Kouvelos, G.; Eckstein, H.-H.; Giannoukas, A. A systematic review and meta-analysis on early mortality after abdominal aortic aneurysm repair in females in urgent and elective settings. J. Vasc. Surg. 2022, 75, 1082–1088. [Google Scholar] [CrossRef]
- Nana, P.; Spanos, K.; Behrendt, C.A.; Dakis, K.; Brotis, A.; Kouvelos, G.; Giannoukas, A.; Kolbel, T. Thirty-day mortality in females after elective and urgent abdominal aortic aneurysm repair. J. Cardiovasc. Surg. 2023, ahead of print. [Google Scholar] [CrossRef]
- Ulug, P.; Sweeting, M.J.; von Allmen, R.S.; Thompson, S.G.; Powell, J.T.; SWAn collaborators. Morphological suitability for endovascular repair, non-intervention rates, and operative mortality in women and men assessed for intact abdominal aortic aneurysm repair: Systematic reviews with meta-analysis. Lancet 2017, 389, 2482–2491. [Google Scholar] [CrossRef] [PubMed]
- Storck, M.; Nolte, T.; Tenholt, M.; Maene, L.; Maleux, G.; Scheinert, D. Women and men derive comparable benefits from an ultra-low-profile endograft: 1-year results of the European OVATION registry. J. Cardiovasc. Surg. 2017, 58, 658–664. [Google Scholar] [CrossRef]
- Witheford, M.; Chong, D.S.T.; Martin-Gonzalez, T.; Van Calster, K.; Davis, M.; Prent, A.; Haulon, S.; Mastracci, T.M. Women undergoing endovascular thoracoabdominal aortic aneurysm repair differ significantly from their male counterparts preoperatively and postoperatively. J. Vasc. Surg. 2020, 71, 748–757. [Google Scholar] [CrossRef]
- Latz, C.A.; Boitano, L.; Wang, L.J.; Chou, E.; DeCarlo, C.; Pendleton, A.A.; Mohebali, J.; Conrad, M. Female Sex Portends Worse Long-Term Survival after Open Type I-III Thoracoabdominal Aneurysm Repair. Ann. Vasc. Surg. 2021, 70, 162–170. [Google Scholar] [CrossRef]
- Latz, C.A.; Boitano, L.T.; Wang, L.J.; Mohebali, J.; Tanious, A.; Schwartz, S.I.; Conrad, M. Sex-related outcomes after open type IV thoracoabdominal aortic aneurysm repair. J. Vasc. Surg. 2021, 73, 443–450. [Google Scholar] [CrossRef]
- Nana, P.; Spanos, K.; Kölbel, T.; Panuccio, G.; Jama, K.; Jakimowicz, T.; Rohlffs, F. Early and mid-term outcomes of females treated with t-Branch off the shelf device. Ann. Vasc. Surg. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Kölbel, T.; Spanos, K.; Jama, K.; Behrendt, C.-A.; Panuccio, G.; Eleshra, A.; Rohlffs, F.; Jakimowicz, T. Early outcomes of the t-Branch off-the-shelf multi-branched stent graft in 542 patients for elective and urgent aortic pathologies: A retrospective observational study. J. Vasc. Surg. 2021, 74, 1817–1824. [Google Scholar] [CrossRef]
- Oderich, G.S.; Forbes, T.L.; Chaer, R.; Davies, M.G.; Lindsay, T.F.; Mastracci, T.; Singh, M.J.; Timaran, C.; Woo, E.Y. Reporting standards for endovascular aortic repair of aneurysms involving the renal-mesenteric arteries. J. Vasc. Surg. 2021, 73, 4S–52S. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef]
- Behrendt, C.A.; Panuccio, G.; Kuchenbecker, J.; Rohlffs, F.; Heidemann, F.; Debus, E.S.; Spanos, K.; Kölbel, T. How Does Female Sex Affect Complex Endovascular Aortic Repair? A Single Centre Cohort Study. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 849–856. [Google Scholar] [CrossRef]
- Rieß, H.; Debus, E.S.; Schwaneberg, T.; Sedrakyan, A.; Kölbel, T.; Tsilimparis, N.; Larena-Avellaneda, A.; Behrendt, C.-A. Gender disparities in fenestrated and branched endovascular aortic repair. Eur. J. Cardiothorac. Surg. 2019, 55, 338–344. [Google Scholar] [CrossRef]
- Moghadamyeghaneh, Z.; Sgroi, M.D.; Chen, S.L.; Kabutey, N.-K.; Stamos, M.J.; Fujitani, R.M. Risk factors and outcomes of postoperative ischemic colitis in contemporary open and endovascular abdominal aortic aneurysm repair. J. Vasc. Surg. 2016, 63, 866–872. [Google Scholar] [CrossRef]
- Yousef, S.; Brown, J.A.; Aranda-Michel, E.; Serna-Gallegos, D.; Wang, Y.; Ogami, T.; Sultan, I. Sex-Related Differences in Clinical Outcomes After Thoracic Endovascular Aortic Repair. J. Am. Heart Assoc. 2023, 12, e025520. [Google Scholar] [CrossRef]
- Jin, G.; Liu, C.; Fei, Z.; Xu, M. A systematic review and meta-analysis on sex disparities in the outcomes of fenestrated branched endovascular aortic aneurysm repair. J. Vasc. Surg. 2023, 77, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Isernia, G.; Simonte, G.; Gallitto, E.; Bertoglio, L.; Fargion, A.; Melissano, G.; Chiesa, R.; Lenti, M.; Pratesi, C.; Faggioli, G.; et al. Sex Influence on Fenestrated and Branched Endovascular Aortic Aneurysm Repair: Outcomes from a National Multicenter Registry. J. Endovasc. Ther. 2022, 15266028221137498. [Google Scholar] [CrossRef]
- Khoury, M.K.; Timaran, D.E.; Soto-Gonzalez, M.; Timaran, C.H. Fenestrated-branched endovascular aortic repair in patients with chronic kidney disease. J. Vasc. Surg. 2020, 72, 66–72. [Google Scholar] [CrossRef]
- Edman, N.I.; Schanzer, A.; Crawford, A.; Oderich, G.S.; Farber, M.A.; Schneider, D.B.; Timaran, C.H.; Beck, A.W.; Eagleton, M.; Sweet, M.P.; et al. Sex-related outcomes after fenestrated-branched endovascular aneurysm repair for thoracoabdominal aortic aneurysms in the U.S. Fenestrated and Branched Aortic Research Consortium. J. Vasc. Surg. 2021, 74, 861–870. [Google Scholar] [CrossRef]
- Ulug, P.; Powell, J.T.; Warschkow, R.; von Allmen, R.S. Editor’s Choice–Sex Specific Differences in the Management of Descending Thoracic Aortic Aneurysms: Systematic Review with Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. 2019, 58, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Forbes, S.M.; Mahmood, D.N.; Rocha, R.; Tan, K.; Ouzounian, M.; Chung, J.C.Y.; Lindsay, T.F. Females experience elevated early morbidity and mortality, but similar midterm survival compared to males after branched/fenestrated endovascular aortic aneurysm repair. J. Vasc. Surg. 2023, 77, 1349–1358. [Google Scholar] [CrossRef]
- Spanos, K.; Theodorakopoulou, M.; Debus, S.E.; Rohlffs, F.; Heidemann, F.; Kölbel, T.; Tsilimparis, N. Accurate Orientation of the t-Branch Off-the-Shelf Multibranched Endograft After Deployment in Urgent Cases. J. Endovasc. Ther. 2018, 25, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Motta, F.; Crowner, J.R.; Kalbaugh, C.A.; Marston, W.A.; Pascarella, L.; McGinigle, K.L.; Kibbe, M.R.; Farber, M.A. Outcomes and complications after fenestrated-branched endovascular aortic repair. J. Vasc. Surg. 2019, 70, 15–22. [Google Scholar] [CrossRef]
- Ma, Y.; Siddiqui, M.S.; Farhan, S.A.; Albuquerque, F.C.; Larson, R.A.; Levy, M.M.; Chery, J.; Newton, D.H. A meta-analysis on the effect of proximal landing zone location on stroke and mortality in thoracic endovascular aortic repair. J. Vasc. Surg. 2023, ahead of print. [Google Scholar] [CrossRef]
- Oyama, N.; Gona, P.; Salton, C.J.; Chuang, M.L.; Jhaveri, R.R.; Blease, S.J.; Manning, A.R.; Lahiri, M.; Botnar, R.M.; Levy, D.; et al. Differential impact of age, sex, and hypertension on aortic atherosclerosis: The Framingham Heart Study. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 155–159. [Google Scholar] [CrossRef] [PubMed]
| Aneurysm Characteristics | Female Cohort (154 Cases) | Male Cohort (388 Cases) | p |
|---|---|---|---|
| Aneurysm diameter (mm) | 73.8 ± 5.9 | 76.8 ± 5.8 | 0.59 |
| Thoracoabdominal aneurysm | 143 (94.2%) | 355 (91.5%) | 0.83 |
| I | 21 (13.6%) | 12 (3.1%) | <0.001 |
| II | 22 (14.3%) | 51 (13.1%) | 0.63 |
| III | 46 (29.8%) | 76 (19.6%) | 0.07 |
| IV | 44 (28.6%) | 195 (50.3%) | 0.008 |
| V | 10 (6.5%) | 21 (5.4%) | 0.65 |
| I–III | 89 (57.8%) | 139 (35.8%) | 0.004 |
| Pararenal aneurysm | 10 (6.4%) | 4 (0.7%) | 0.003 |
| Juxtarenal aneurysm | 1 (0.6%) | 29 (7.5%) | 0.002 |
| Comorbidities | Female Cohort (154 Cases) | Male Cohort (388 Cases) | p |
|---|---|---|---|
| Coronary artery disease | 70 (45.5%) | 217 (55.9%) | 0.028 |
| Myocardial infarction | 21 (13.6%) | 95 (24.5%) | 0.005 |
| CABG | 8 (5.2%) | 51 (13.1%) | 0.007 |
| PTCA/stenting | 17 (11.0%) | 30 (7.7%) | 0.58 |
| Hypertension | 142 (92.2%) | 355 (91.5%) | 0.786 |
| Dyslipidemia | 89 (57.8%) | 243 (62.6%) | 0.279 |
| Smoking | 74 (48.1%) | 218 (56.2%) | 0.087 |
| -Active smoking | 38 (24.7%) | 84 (21.6%) | 0.447 |
| COPD | 30 (19.6%) | 72 (18.6%) | 0.778 |
| Diabetes mellitus | 24 (15.6%) | 64 (16.5%) | 0.795 |
| Chronic renal disease | 53 (34.6%) | 166 (37.7%) | 0.237 |
| -Dialysis dependent | 2 (1.3%) | 7 (1.8%) | 0.68 |
| Stroke | 12 (7.8%) | 37 (9.5%) | 0.52 |
| Transient ischemic attack | 3 (1.9%) | 14 (3.6%) | 0.32 |
| Peripheral arterial disease | 77 (50.3%) | 39 (48.1%) | 0.36 |
| Previous aortic repair | 45 (29.2%) | 133 (34.3%) | 0.26 |
| Previous ascending repair | 11 (7.1%) | 14 (3.6%) | 0.077 |
| ASA score | |||
| I | 2 (1.3%) | 9 (2.3%) | 0.46 |
| II | 21 (13.8%) | 76 (19.7%) | 0.17 |
| III | 111 (73.0%) | 261 (67.8%) | 0.64 |
| IV | 18 (11.9%) | 39 (10.2%) | 0.62 |
| Post-Operative Events at 30 Days | Female Cohort | Male Cohort | p |
|---|---|---|---|
| Mortality | 25 (16.2%) | 42 (10.8%) | 0.084 |
| MAE | 52 (33.7%) | 83 (21.4%) | 0.022 |
| SCI | 21 (13.6%) | 36 (9.3%) | 0.183 |
| -Paraplegia | 11 (7.1%) | 15 (3.8%) | 0.11 |
| SIRS | 7 (4.5%) | 7 (1.8%) | 0.07 |
| Myocardial infarction | 5 (3.2%) | 5 (1.3%) | 0.135 |
| Respiratory failure | 5 (3.2%) | 7 (1.8%) | 0.315 |
| Stroke | 5 (3.2%) | 7 (1.8%) | 0.315 |
| -Major | 2 (1.3%) | 0 (0%) | 0.011 |
| Acute kidney injury | 22 (14.3%) | 50 (12.9%) | 0.705 |
| -Dialysis | 7 (4.5%) | 14 (3.6%) | 0.624 |
| Bowel ischemia | 3 (1.9%) | 7 (1.8%) | 0.91 |
| -Ischemia needing resection or not responding to medical treatment | 1 (0.6%) | 0 (0%) | 0.14 |
| Wound complications needing access site revision | 33 (21.4%) | 47 (12.1%) | <0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nana, P.; Jama, K.; Kölbel, T.; Spanos, K.; Panuccio, G.; Jakimowicz, T.; Rohlffs, F. Sex-Comparative Outcomes of the T-Branch Device for the Treatment of Complex Aortic Aneurysms. J. Clin. Med. 2023, 12, 5811. https://doi.org/10.3390/jcm12185811
Nana P, Jama K, Kölbel T, Spanos K, Panuccio G, Jakimowicz T, Rohlffs F. Sex-Comparative Outcomes of the T-Branch Device for the Treatment of Complex Aortic Aneurysms. Journal of Clinical Medicine. 2023; 12(18):5811. https://doi.org/10.3390/jcm12185811
Chicago/Turabian StyleNana, Petroula, Katarzyna Jama, Tilo Kölbel, Konstantinos Spanos, Giuseppe Panuccio, Tomasz Jakimowicz, and Fiona Rohlffs. 2023. "Sex-Comparative Outcomes of the T-Branch Device for the Treatment of Complex Aortic Aneurysms" Journal of Clinical Medicine 12, no. 18: 5811. https://doi.org/10.3390/jcm12185811
APA StyleNana, P., Jama, K., Kölbel, T., Spanos, K., Panuccio, G., Jakimowicz, T., & Rohlffs, F. (2023). Sex-Comparative Outcomes of the T-Branch Device for the Treatment of Complex Aortic Aneurysms. Journal of Clinical Medicine, 12(18), 5811. https://doi.org/10.3390/jcm12185811






