The Impact of Facial Burns on Short- and Long-Term Quality of Life and Psychological Distress—A Prospective Matched Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
- -
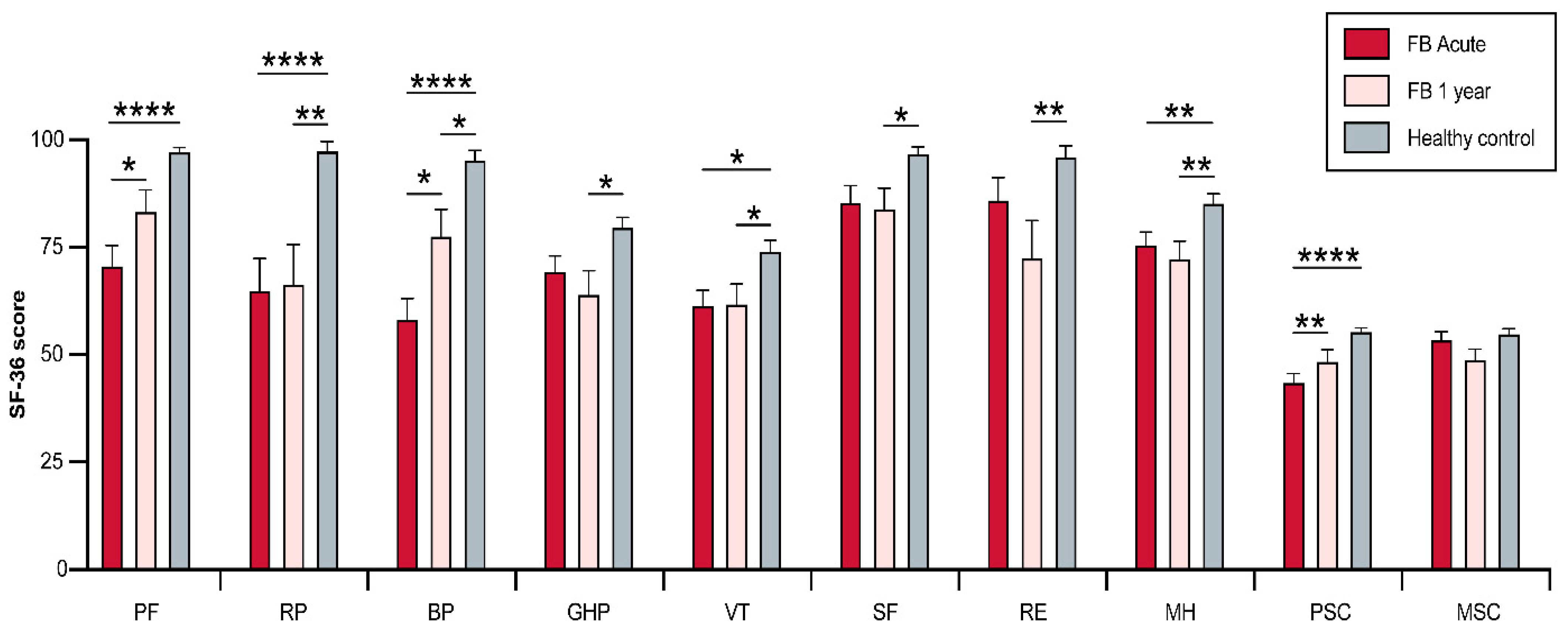
- The 36-Item Short Form (SF-36) is a widely employed tool that is used to evaluate QOL [12]. Thirty-six of the items are grouped to form eight domain subscales: PF: physical functioning, RP: physical role functioning, BP: bodily pain, GH: general health perception, VT: vitality, SF: social role functioning, RE: emotional role functioning, MH: mental health, in an aim to provide a measure of overall well-being: [12]. Despite its ease of use and application, this tool meets rigorous standards to provide validity and reliability in multiple medical settings [13,14].
- -
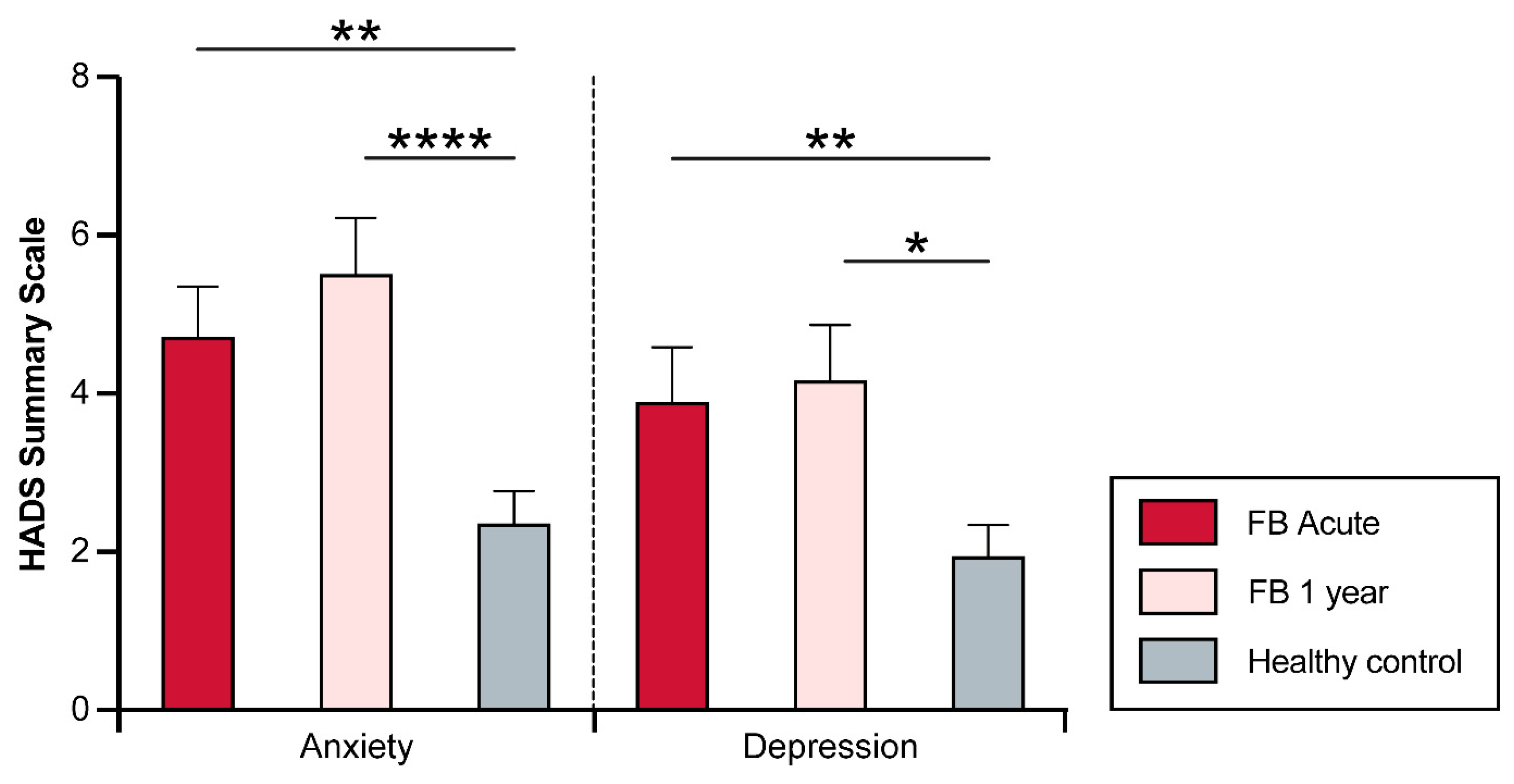
- The Hospital Anxiety and Depression Scale (HADS) is a fourteen-question instrument that is used to measure psychological distress in different clinical settings, with an emphasis on anxiety and depression [15]. Each item is ranked on a 4-point scale (0–3) based on severity, where 0 equals no symptoms, and 3 equals severe symptoms. Scores for each subscale can range from 0 to 21 with scores categorized as follows: 0–7 (normal), 8–10 (mild), 11–14 (moderate) 15–21 (severe). A higher score indicates more depressive symptoms [16]. Unlike other tools, HADS can change during the course of the disease allowing for the identification of psychological changes associated with treatments or interventions [15].
Statistical Analysis
3. Results
3.1. Patient Population
3.2. Physical and Psychosocial Functioning Summary Scores
3.3. Physical and Psychosocial Domains
3.4. Complicated Facial Burns (COMP)
3.5. Psychological Distress (HADS)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- James, S.L.; Lucchesi, L.R.; Bisignano, C.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Henry, N.J.; McCracken, D.; Roberts, N.L.; et al. Epidemiology of injuries from fire, heat and hot substances: Global, regional and national morbidity and mortality estimates from the Global Burden of Disease 2017 study. Inj. Prev. 2020, 26 (Suppl. 2), i36–i45. [Google Scholar] [CrossRef] [Green Version]
- Zatriqi, V.; Arifi, H.; Zatriqi, S.; Duci, S.; Rrecaj, S.; Martinaj, M. Facial burns—Our experience. Mater. Sociomed. 2013, 25, 26–27. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Liu, Y.; Deng, X.; Deng, C.; Pan, Y.; Hu, A. The Correlation Between Quality of Life and Acceptability of Disability in Patients with Facial Burn Scars. Front. Bioeng. Biotechnol. 2019, 7, 329. [Google Scholar] [CrossRef]
- Tagkalakis, P.; Demiri, E. A fear avoidance model in facial burn body image disturbance. Ann. Burns Fire Disasters 2009, 22, 203–207. [Google Scholar]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef]
- Wu, Z.; Zhang, Q.; Ye, G.; Zhang, H.; Heng, B.C.; Fei, Y.; Zhao, B.; Zhou, J. Structural and physiological changes of the human body upon SARS-CoV-2 infection. J. Zhejiang Univ. Sci. B. 2021, 22, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Ledrick, D.; Moore, A. Facial Burns. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Moi, A.L.; Haugsmyr, E.; Heisterkamp, H. Long-Term Study of Health and Quality of Life after Burn Injury. Ann. Burns Fire Disasters 2016, 29, 295–299. [Google Scholar] [PubMed]
- Khanna, D.; Tsevat, J. Health-related quality of life--an introduction. Am. J. Manag. Care 2007, 13 (Suppl. 9), S218–S223. [Google Scholar] [PubMed]
- Spronk, I.; Legemate, C.; Oen, I.; van Loey, N.; Polinder, S.; van Baar, M. Health related quality of life in adults after burn injuries: A systematic review. PLoS ONE 2018, 13, e0197507. [Google Scholar] [CrossRef] [Green Version]
- Beck, I.; Tapking, C.; Haug, V.; Nolte, S.; Böcker, A.; Stoppe, C.; Kneser, U.; Hirche, C.; Hundeshagen, G. Short- and long term hyposmia, hypogeusia, dysphagia and dysphonia after facial burn injury—A prospective matched cohort study. Burns 2023, 49, 380–387. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [Green Version]
- Brazier, J.E.; Harper, R.; Jones, N.M.; O’cathain, A.; Thomas, K.J.; Usherwood, T.; Westlake, L. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ 1992, 305, 160–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunevicius, A. Reliability and validity of the SF-36 Health Survey Questionnaire in patients with brain tumors: A cross-sectional study. Health Qual. Life Outcomes 2017, 15, 92. [Google Scholar] [CrossRef] [Green Version]
- Montazeri, A.; Vahdaninia, M.; Ebrahimi, M.; Jarvandi, S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual. Life Outcomes 2003, 1, 14. [Google Scholar] [CrossRef]
- Snaith, R.P.; Zigmond, A.S. The hospital anxiety and depression scale. Br. Med. J. (Clin. Res. Ed.) 1986, 292, 344. [Google Scholar] [CrossRef] [Green Version]
- Hutter, M.F.; Smolle, C.; Kamolz, L.P. Life after Burn, Part I: Health-Related Quality of Life, Employment and Life Satisfaction. Medicina 2022, 58, 599. [Google Scholar] [CrossRef]
- Smolle, C.; Hutter, M.F.; Kamolz, L.P. Life after Burn, Part II: Substance Abuse, Relationship and Living Situation of Burn Survivors. Medicina 2022, 58, 563. [Google Scholar] [CrossRef]
- Habib, Z.; Saddul, R.; Kamran, F. Perceptions and experiences of female burn survivors with facial disfigurement. Chin. J. Traumatol. 2021, 24, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Habib, Z.; Kausar, R.; Kamran, F. Handling traumatic experiences in facially disfigured female burn survivors. Burns 2021, 47, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, S.; Carloni, R.; Bertheuil, N.; Grolleau, J.L.; Auquit-Auckbur, I.; Chaput, B. Assessment of quality-of-life in patients with face-and-neck burns: The Burn-Specific Health Scale for Face and Neck (BSHS-FN). Burns 2018, 44, 1602–1609. [Google Scholar] [CrossRef]
- Tebble, N.J.; Adams, R.; Thomas, D.W.; Price, P. Anxiety and self-consciousness in patients with facial lacerations one week and six months later. Br. J. Oral. Maxillofac. Surg. 2006, 44, 520–525. [Google Scholar] [CrossRef]
- Altier, N.; Malenfant, A.; Forget, R.; Choinière, M. Long-term adjustment in burn victims: A matched-control study. Psychol. Med. 2002, 32, 677–685. [Google Scholar] [CrossRef]
- Edgar, D.; Dawson, A.; Hankey, G.; Phillips, M.; Wood, F. Demonstration of the validity of the SF-36 for measurement of the temporal recovery of quality of life outcomes in burns survivors. Burns 2010, 36, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Fauerbach, J.A.; Lezotte, D.; Hills, R.A.; Cromes, G.F.; Kowalske, K.; de Lateur, B.J.; Goodwin, C.W.; Blakeney, P.; Herndon, D.N.; Wiechman, S.A.; et al. Burden of burn: A norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function. J. Burn. Care Rehabil. 2005, 26, 21–32. [Google Scholar] [CrossRef]
- Fauerbach, J.A.; Lawrence, J.W.; Munster, A.M.; Palombo, D.A.; Richter, D. Prolonged adjustment difficulties among those with acute posttrauma distress following burn injury. J. Behav. Med. 1999, 22, 359–378. [Google Scholar] [CrossRef]
- Klein, M.B.; Lezotte, D.C.; Heltshe, S.; Fauerbach, J.; Holavanahalli, R.K.; Rivara, F.P.; Pham, T.; Engrav, L. Functional and psychosocial outcomes of older adults after burn injury: Results from a multicenter database of severe burn injury. J. Burn. Care Res. 2011, 32, 66–78. [Google Scholar] [CrossRef]
- Brown, B.C.; McKenna, S.P.; Siddhi, K.; McGrouther, D.A.; Bayat, A. The hidden cost of skin scars: Quality of life after skin scarring. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.E.; Griffiths, T.A. Psychological consequences of burn injury. Burns 1991, 17, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Thombs, B.D.; Haines, J.M.; Bresnick, M.G.; Magyar-Russell, G.; Fauerbach, J.A.; Spence, R.J. Depression in burn reconstruction patients: Symptom prevalence and association with body image dissatisfaction and physical function. Gen. Hosp. Psychiatry 2007, 29, 14–20. [Google Scholar] [CrossRef]
- Orwelius, L.; Willebrand, M.; Gerdin, B.; Ekselius, L.; Fredrikson, M.; Sjöberg, F. Long term health-related quality of life after burns is strongly dependent on pre-existing disease and psychosocial issues and less due to the burn itself. Burns 2013, 39, 229–235. [Google Scholar] [CrossRef] [Green Version]
- Oster, C.; Willebrand, M.; Dyster-Aas, J.; Kildal, M.; Ekselius, L. Validation of the EQ-5D questionnaire in burn injured adults. Burns 2009, 35, 723–732. [Google Scholar] [CrossRef] [PubMed]

| Group FB (n = 55) | Group CTR (n = 55) | p Value | |
|---|---|---|---|
| Age; Median (IQR) | 37.0 (24) | 38.5 (26) | 0.69 |
| Sex; n (% male) | 47 (85) | 47 (85) | 0.99 |
| Smoker; n (%) | 21 (39) | 12 (22) | 0.09 |
| Characteristic | Group FB (n = 55) |
|---|---|
| TBSA; median (IQR) | 11 (29) |
| Facial involvement (% of facial area) | 50 (40) |
| Cause of burn | 47 (85) |
| Flame/Flash | 4 (7) |
| Electricity | 3 (6) |
| Steam | 1 (2) |
| Contact | 50 (40) |
| Inhalation trauma | 4 (7) |
| LOS; median (IQR) | 17 (25) |
| LOS ICU; median (IQR) | 3 (18) |
| LOS/% TBSA; median (IQR) | 1.5 (1.3) |
| Mechanical ventilation; median days (IQR) | 0 (1) |
| Mortality | 0 (0) |
| Need for surgical treatment | |
| Acute | 9 (16) |
| Within one year | 4 (7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palackic, A.; Franco-Mesa, C.; Beck, I.; Nolte, S.; Tapking, C.; Panayi, A.C.; Stolle, A.; Haug, V.; Hirche, C.; Kneser, U.; et al. The Impact of Facial Burns on Short- and Long-Term Quality of Life and Psychological Distress—A Prospective Matched Cohort Study. J. Clin. Med. 2023, 12, 5057. https://doi.org/10.3390/jcm12155057
Palackic A, Franco-Mesa C, Beck I, Nolte S, Tapking C, Panayi AC, Stolle A, Haug V, Hirche C, Kneser U, et al. The Impact of Facial Burns on Short- and Long-Term Quality of Life and Psychological Distress—A Prospective Matched Cohort Study. Journal of Clinical Medicine. 2023; 12(15):5057. https://doi.org/10.3390/jcm12155057
Chicago/Turabian StylePalackic, Alen, Camila Franco-Mesa, Inessa Beck, Steffen Nolte, Christian Tapking, Adriana C. Panayi, Annette Stolle, Valentin Haug, Christoph Hirche, Ulrich Kneser, and et al. 2023. "The Impact of Facial Burns on Short- and Long-Term Quality of Life and Psychological Distress—A Prospective Matched Cohort Study" Journal of Clinical Medicine 12, no. 15: 5057. https://doi.org/10.3390/jcm12155057
APA StylePalackic, A., Franco-Mesa, C., Beck, I., Nolte, S., Tapking, C., Panayi, A. C., Stolle, A., Haug, V., Hirche, C., Kneser, U., & Hundeshagen, G. (2023). The Impact of Facial Burns on Short- and Long-Term Quality of Life and Psychological Distress—A Prospective Matched Cohort Study. Journal of Clinical Medicine, 12(15), 5057. https://doi.org/10.3390/jcm12155057












