Desktop Virtual Reality Offers a Novel Approach to Minimize Pain and Anxiety during Burn Wound Cleaning/Debridement in Infants and Young Children: A Randomized Crossover Pilot Study
Abstract
1. Introduction
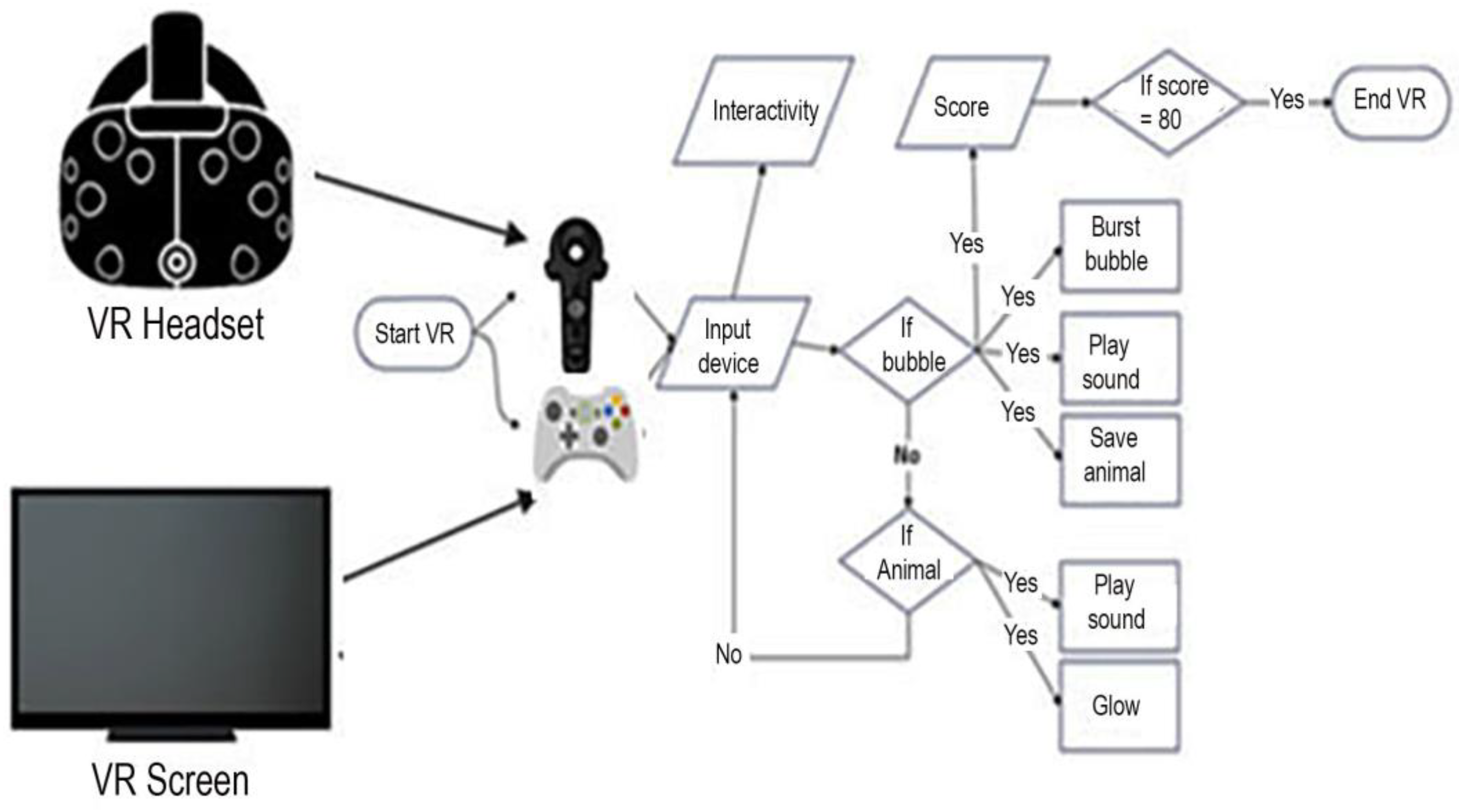
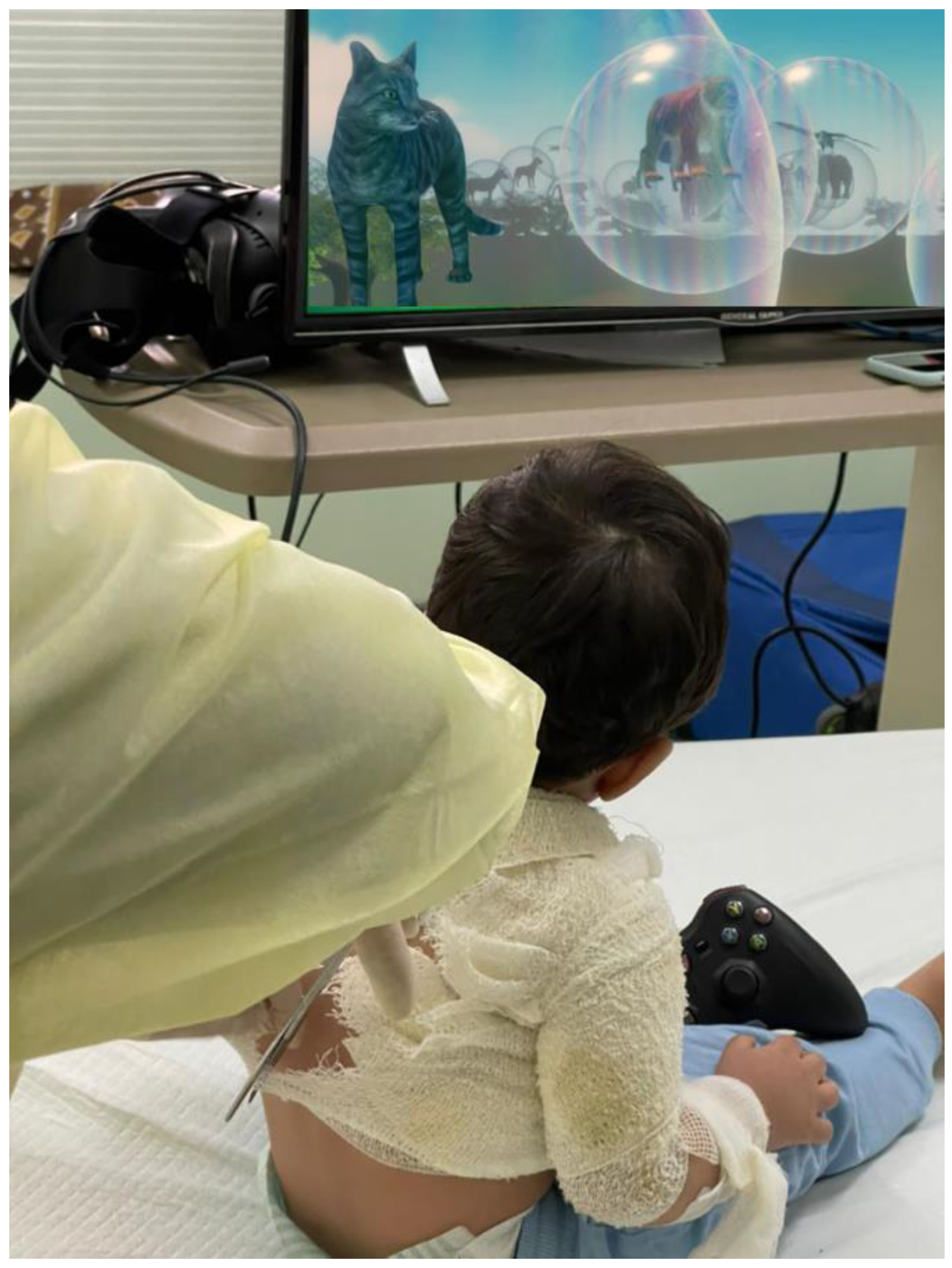
1.1. Desktop Virtual Reality System Design
1.2. Software and Materials
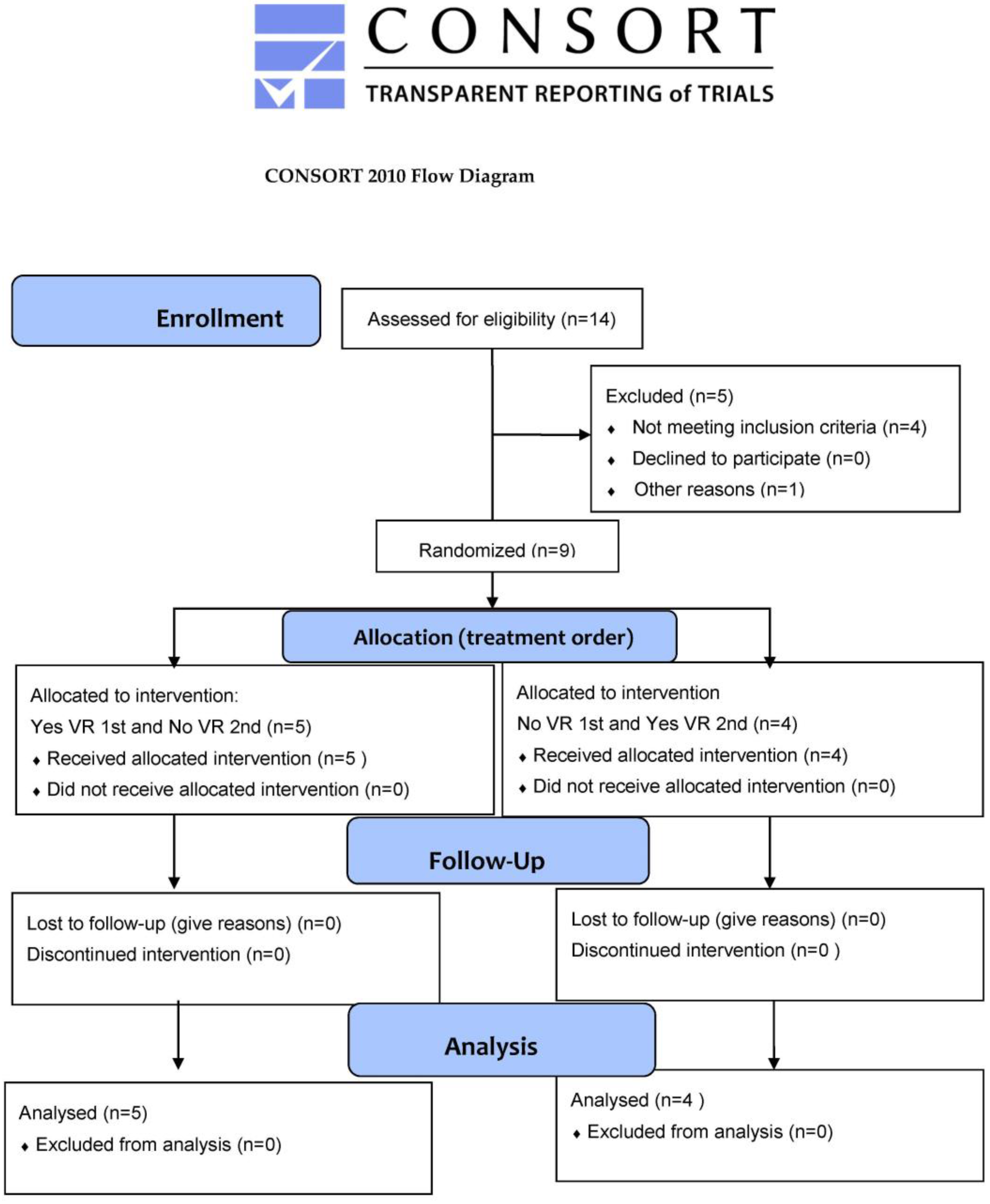
2. Materials and Methods
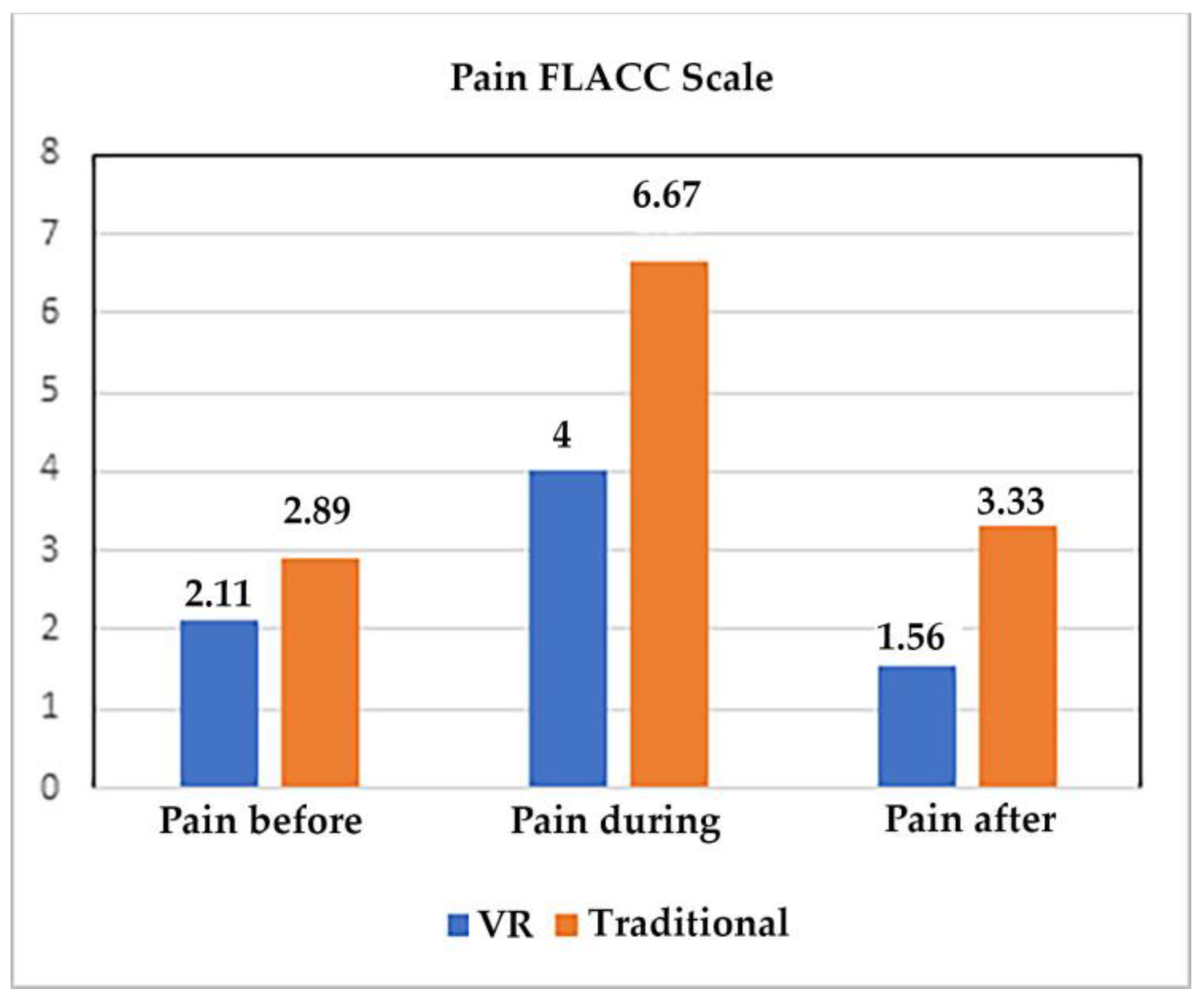
3. Results
Joy Scale Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Frestadius, A.; Grehn, F.; Kildal, M.; Huss, F.; Fredén, F. Intranasal dexmedetomidine and rectal ketamine for young children undergoing burn wound procedures. Burns 2022, 48, 1445–1451. [Google Scholar] [CrossRef] [PubMed]
- Hubara, E.; Berzon, B.; E Nellis, M.; Ram, R.; Kassif Lerner, R.; Alfandary Many, Y.; Feldman, O.; Pessach, I. Safety of pediatric sedation and analgesia during burn dressing changes by pediatric residents. Paediatr. Anaesth. 2023, 33, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Pan, Q.; Xu, L.; Lin, R.; Dai, J.; Chen, X.; Jiang, M.; Chen, Z. Comparison of analgesic and anxiolytic effects of nitrous oxide in burn wound treatment: A single-blind prospective randomized controlled trial. Medicine 2019, 98, e18188. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J.K.; Voss, J.; Ganatra, H.; Langner, T.; Chalise, P.; Stokes, S.; Bhavsar, D.; Kovac, A.L. Sedation and Analgesia During Pediatric Burn Dressing Change: A Survey of American Burn Association Centers. J. Burn. Care Res. 2019, 40, 287–293. [Google Scholar] [CrossRef]
- Wall, S.L.; Clarke, D.L.; Allorto, N.L. Analgesia protocols for burns dressings: Challenges with implementation. Burns 2019, 45, 1680–1684. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.A.; De Young, A.; Kimble, R.; Kenardy, J. Impact of Parental Acute Psychological Distress on Young Child Pain-Related Behavior Through Differences in Parenting Behavior During Pediatric Burn Wound Care. J. Clin. Psychol. Med. Settings 2019, 26, 516–529. [Google Scholar] [CrossRef]
- Chapman, C.R.; Vierck, C.J. The Transition of Acute Postoperative Pain to Chronic Pain: An Integrative Overview of Research on Mechanisms. J. Pain 2017, 18, 359.E1–359.E8. [Google Scholar] [CrossRef]
- Noel, M.; Rabbitts, J.A.; Tai, G.G.; Palermo, T.M. Remembering pain after surgery: A longitudinal examination of the role of pain catastrophizing in children’s and parents’ recall. Pain 2015, 156, 800–808. [Google Scholar] [CrossRef]
- Rabbitts, J.A.; Fisher, E.; Rosenbloom, B.N.; Palermo, T.M. Prevalence and Predictors of Chronic Postsurgical Pain in Children: A Systematic Review and Meta-Analysis. J. Pain 2017, 18, 605–614. [Google Scholar] [CrossRef]
- Rosenberg, L.; Rosenberg, M.; Sharp, S.; Thomas, C.R.; Humphries, H.F.; Holzer, C.E., 3rd; Herndon, D.N.; Meyer, W.J., 3rd. Does Acute Propranolol Treatment Prevent Posttraumatic Stress Disorder, Anxiety, and Depression in Children with Burns? J. Child Adolesc. Psychopharmacol. 2018, 28, 117–123. [Google Scholar] [CrossRef]
- Boretsky, K.; Mason, K. In the Arms of Morpheus without Morphia; Mitigating the United States Opioid Epidemic by Decreasing the Surgical Use of Opioids. J. Clin. Med. 2021, 10, 1472. [Google Scholar] [CrossRef] [PubMed]
- FDA. FDA Drug Safety Communication. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-approves-label-changes-use-general-anesthetic-and-sedation-drugs (accessed on 20 October 2022).
- Wang, E.; Thomas, J.J.; Rodriguez, S.T.; Kennedy, K.M.; Caruso, T.J. Virtual reality for pediatric periprocedural care. Curr. Opin. Anaesthesiol. 2021, 34, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Bakri, M.H.; Ismail, E.A.; Ali, M.S.; Elsedfy, G.O.; Sayed, T.A.; Ibrahim, A. Behavioral and emotional effects of repeated general anesthesia in young children. Saudi J. Anaesth. 2015, 9, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Schneuer, F.J.; Bentley, J.P.; Davidson, A.J.; Holland, A.J.; Badawi, N.; Martin, A.J.; Skowno, J.; Lain, S.J.; Nassar, N. The impact of general anesthesia on child development and school performance: A population-based study. Paediatr. Anaesth. 2018, 28, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Peng, Y.; Wang, Y. Long-duration general anesthesia influences the intelligence of school age children. BMC Anesthesiol. 2017, 17, 170. [Google Scholar] [CrossRef]
- Caruso, T.J.; O′Connell, C.; Qian, J.J.; Kung, T.; Wang, E.; Kinnebrew, S.; Pearson, M.; Kist, M.; Menendez, M.; Rodriguez, S.T. Retrospective Review of the Safety and Efficacy of Virtual Reality in a Pediatric Hospital. Pediatr. Qual. Saf. 2020, 5, e293. [Google Scholar] [CrossRef]
- Lerwick, J.L. Minimizing pediatric healthcare-induced anxiety and trauma. World J. Clin. Pediatr. 2016, 5, 143–150. [Google Scholar] [CrossRef]
- Lopez, U.; Martin, J.; van Assche, M.; Fleury Schubert, A.; Fournet, M.; Quartier, V.; Habre, W.; Van der Linden, M. Classification of postoperative behavior disturbances in preschool children: A qualitative study. Paediatr. Anaesth. 2019, 29, 712–720. [Google Scholar] [CrossRef]
- Keefe, F.J.; Main, C.J.; George, S.Z. Advancing Psychologically Informed Practice for Patients With Persistent Musculoskeletal Pain: Promise, Pitfalls, and Solutions. Phys. Ther. 2018, 98, 398–407. [Google Scholar] [CrossRef]
- Patterson, D.R. Clinical Hypnosis for Pain Control; American Psychological Association: Washington, DC, USA, 2010. [Google Scholar]
- Birnie, K.A.; Chambers, C.T.; Spellman, C.M. Mechanisms of distraction in acute pain perception and modulation. Pain 2017, 158, 1012–1013. [Google Scholar] [CrossRef]
- Rivas, E. Music Intervention for the Burn Population; The University of Arizona: Tucson, AZ, USA, 2019. [Google Scholar]
- Rohilla, L.; Agnihotri, M.; Trehan, S.K.; Sharma, R.K.; Ghai, S. Effect of Music Therapy on Pain Perception, Anxiety, and Opioid Use During Dressing Change Among Patients With Burns in India: A Quasi-experimental, Cross-over Pilot Study. Ostomy Wound Manag. 2018, 64, 40–46. [Google Scholar] [CrossRef]
- Hyland, E.J.; D′Cruz, R.; Harvey, J.G.; Moir, J.; Parkinson, C.; Holland, A.J.A. An assessment of early Child Life Therapy pain and anxiety management: A prospective randomised controlled trial. Burns 2015, 41, 1642–1652. [Google Scholar] [CrossRef]
- Yildirim, M.; Koroglu, E.; Yucel, C.; Kirlak, S.; Sen, S. The effect of hospital clown nurse on children′s compliance to burn dressing change. Burns 2019, 45, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G. Virtual reality: A new tool for interdisciplinary psychology research. CyberPsychol. Behav. 1998, 1, 195–200. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Doctor, J.N.; Patterson, D.R.; Carrougher, G.J.; Furness, T.A., 3rd. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 2000, 85, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Honzel, E.; Murthi, S.; Brawn-Cinani, B.; Colloca, G.; Kier, C.; Varshney, A.; Colloca, L. Virtual reality, music, and pain: Developing the premise for an interdisciplinary approach to pain management. Pain 2019, 160, 1909–1919. [Google Scholar] [CrossRef]
- Hitching, R.; Hoffman, H.G.; Garcia-Palacios, A.; Adamson, M.M.; Madrigal, E.; Alhalabi, W.; Alhudali, A.; Sampaio, M.; Peterson, B.; Fontenot, M.R.; et al. The Emerging Role of Virtual Reality as an Adjunct to Procedural Sedation and Anesthesia: A Narrative Review. J. Clin. Med. 2023, 12, 843. [Google Scholar] [CrossRef]
- Peterson, B.N.; Hitching, R.; Howard, L.; Zhu, K.; Fontenot, M.R.; Alhalabi, W.; Seibel, A.; Harris, O.A.; Madrigal, E.; Adamson, M.M.; et al. Immersive Virtual Reality: A Safe, Scalable, Non-opioid Analgesic for Military and Veteran Patients. Front. Virtual Real. 2021, 2, 843. [Google Scholar] [CrossRef]
- Smith, K.L.; Wang, Y.; Colloca, L. Impact of Virtual Reality Technology on Pain and Anxiety in Pediatric Burn Patients: A Systematic Review and Meta-Analysis. Front. Virtual Real. 2022, 2, 751735. [Google Scholar] [CrossRef]
- Trost, Z.; France, C.; Anam, M.; Shum, C. Virtual reality approaches to pain: Toward a state of the science. Pain 2021, 162, 325–331. [Google Scholar] [CrossRef]
- Merriam-Webster. Merriam-Webster Dictionary. Available online: https://www.merriam-webster.com/dictionary/virtual%20reality (accessed on 3 March 2023).
- Hoffman, H.G. Interacting with virtual objects via embodied avatar hands reduces pain intensity and diverts attention. Sci. Rep. 2021, 11, 10672. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Fontenot, M.R.; Garcia-Palacios, A.; Greenleaf, W.J.; Alhalabi, W.; Curatolo, M.; Flor, H. Adding tactile feedback increases avatar ownership and makes virtual reality more effective at reducing pain in a randomized crossover study. Sci. Rep. 2023, 13, 7915. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G. Virtual-reality therapy. Sci. Am. 2004, 291, 58–65. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Chambers, G.T.; Meyer, W.J., 3rd; Arceneaux, L.L.; Russell, W.J.; Seibel, E.J.; Richards, T.L.; Sharar, S.R.; Patterson, D.R. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Ann. Behav. Med. 2011, 41, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Rodriguez, R.A.; Gonzalez, M.; Bernardy, M.; Pena, R.; Beck, W.; Patterson, D.R.; Meyer, W.J., 3rd. Immersive Virtual Reality as an Adjunctive Non-opioid Analgesic for Pre-dominantly Latin American Children With Large Severe Burn Wounds During Burn Wound Cleaning in the Intensive Care Unit: A Pilot Study. Front. Hum. Neurosci. 2019, 13, 262. [Google Scholar] [CrossRef] [PubMed]
- Maani, C.V.; Hoffman, H.G.; Morrow, M.; Maiers, A.; Gaylord, K.; McGhee, L.L.; DeSocio, P.A. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J. Trauma. 2011, 71, S125–S130. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Richards, T.L.; Coda, B.; Bills, A.R.; Blough, D.; Richards, A.L.; Sharar, S.R. Modulation of thermal pain-related brain activity with virtual reality: Evidence from fMRI. Neuroreport 2004, 15, 1245–1248. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Richards, T.L.; Van Oostrom, T.; Coda, B.A.; Jensen, M.P.; Blough, D.K.; Sharar, S.R. The analgesic effects of opioids and immersive virtual reality distraction: Evidence from subjective and functional brain imaging assessments. Anesth. Analg. 2007, 105, 1776–1783. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Patterson, D.R.; Rodriguez, R.A.; Pena, R.; Beck, W.; Meyer, W.J. Virtual Reality Analgesia for Children With Large Severe Burn Wounds During Burn Wound Debridement. Front. Virtual Real. 2020, 1, 1–11. [Google Scholar] [CrossRef]
- Khadra, C.; Ballard, A.; Dery, J.; Paquin, D.; Fortin, J.S.; Perreault, I.; Labbe, D.R.; Hoffman, H.G.; Bouchard, S.; LeMay, S. Projector-based virtual reality dome environment for procedural pain and anxiety in young children with burn injuries: A pilot study. J. Pain Res. 2018, 11, 343–353. [Google Scholar] [CrossRef]
- Khadra, C.; Ballard, A.; Paquin, D.; Cotes-Turpin, C.; Hoffman, H.G.; Perreault, I.; Fortin, J.S.; Bouchard, S.; Theroux, J.; Le May, S. Effects of a projector-based hybrid virtual reality on pain in young children with burn injuries during hydrotherapy sessions: A within-subject randomized crossover trial. Burns 2020, 46, 1571–1584. [Google Scholar] [CrossRef] [PubMed]
- ABA. American Burn Association. Available online: https://ameriburn.org/wp-content/uploads/2018/12/nbaw2019_statsdataresources_120618-1.pdf (accessed on 3 March 2023).
- Liaw, S.Y.; Sutini; Chua, W.L.; Tan, J.Z.; Levett-Jones, T.; Ashokka, B.; Te Pan, T.L.; Lau, S.T.; Ignacio, J. Desktop Virtual Reality Versus Face-to-Face Simulation for Team-Training on Stress Levels and Performance in Clinical Deterioration: A Randomised Controlled Trial. J. Gen. Intern. Med. 2023, 38, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Anguera, J.A.; Javed, S.V.; Khan, M.A.; Wang, G.; Gazzaley, A. Enhanced Attention Using Head-mounted Virtual Reality. J. Cogn. Neurosci. 2020, 32, 1438–1454. [Google Scholar] [CrossRef]
- Campbell, D.; Stanley, J.C. Experimental and Quasi-Experimental Designs for Research; Houghton Mifflin Company: Boston, MA, USA, 1963; Volume 6. [Google Scholar]
- LeBaron, S.; Zeltzer, L. Assessment of acute pain and anxiety in children and adolescents by self-reports, observer reports, and a behavior checklist. J. Consult. Clin. Psychol. 1984, 52, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Merkel, S.I.; Voepel-Lewis, T.; Shayevitz, J.R.; Malviya, S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatr. Nurs. 1997, 23, 293–297. [Google Scholar]
- Voepel-Lewis, T.; Zanotti, J.; Dammeyer, J.A.; Merkel, S. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am. J. Crit. Care 2010, 19, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Breau, L.M.; Finley, G.A.; McGrath, P.J.; Camfield, C.S. Validation of the Non-communicating Children’s Pain Checklist-Postoperative Version. Anesthesiology 2002, 96, 528–535. [Google Scholar] [CrossRef]
- Nair, A.S.; Diwan, S. Pain scores and statistical analysis—The conundrum. Ain-Shams J. Anesthesiol. 2020, 12, 35. [Google Scholar] [CrossRef]
- Alrimy, T.; Alhalabi, W.; Malibari, A.A.; Alzahrani, F.S.; Alrajhi, S.; Alhalabi, M.; Hoffman, H.G. Virtual Reality Animal Rescue World: Pediatric virtual reality analgesia during just noticeable pressure pain in children aged 2-10 years old (crossover design). Front. Psychol. 2022, 13, 963765. [Google Scholar] [CrossRef]
- Kipping, B.; Rodger, S.; Miller, K.; Kimble, R.M. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: A prospective randomized controlled trial. Burns 2012, 38, 650–657. [Google Scholar] [CrossRef]
- McCaul, K.D.; Malott, J.M. Distraction and coping with pain. Psychol Bull. 1984, 95, 516–533. [Google Scholar] [CrossRef]
- Schulz, K.F.; Grimes, D.A. Blinding in randomised trials: Hiding who got what. Lancet 2002, 359, 696–700. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.I.; SooHoo, M.; Laikin, A.M.; Lane, A.S.; Klein, M.J. Effect of an Immersive Virtual Reality Intervention on Pain and Anxiety Associated With Peripheral Intravenous Catheter Placement in the Pediatric Setting: A Randomized Clinical Trial. JAMA Netw Open 2021, 4, e2122569. [Google Scholar] [CrossRef] [PubMed]
- Galena, H.J. Complications occurring from diagnostic venipuncture. J. Fam. Pract. 1992, 34, 582–584. [Google Scholar] [PubMed]
- AppleVisionPro. Available online: https://www.apple.com/apple-vision-pro/? (accessed on 4 July 2023).
- Elite, V.X. Available online: https://www.vive.com/us/product/vive-xr-elite/overview/ (accessed on 3 March 2023).

| Frequency | Percent | ||||||
|---|---|---|---|---|---|---|---|
| Gender | Male | 3 | 33.0% | ||||
| Female | 6 | 67.0% | |||||
| Hospitalized | Yes | 8 | 89% | ||||
| No (Clinic) | 1 | 11% | |||||
| Cause of Injury | Thermal (Scaled) | ||||||
| Burn | 9 | 100.0% | |||||
| Hospital | King Abdulaziz | 4 | 44.5% | ||||
| Alnoor | 4 | 44.5% | |||||
| IMC | 1 | 11.0% | |||||
| Background Medication | Paracetamol | 9 | 100.0% | ||||
| Total | 9 | 100.0% | |||||
| Minimum | Maximum | Mean | Std. D | ||||
| Age in months 10 | 10 | 60 | 18.89 | 15.90 | |||
| Weight | 8 | 16 | 10.31 | 2.39 | |||
| Burn extent | 3% | 22% | 10% | 6% | |||
| Previous wound care sessions | 1 | 15 | 4.33 | 4.18 | |||
| Injury/Burn Type | Frequency | Percent |
|---|---|---|
| Deep partial thickness (second degree) | 2 | 22.2% |
| Superficial (first degree), Superficial thickness (second degree) | 1 | 11.1% |
| Superficial thickness (second degree) | 3 | 33.3% |
| Superficial thickness (second degree), Full thickness (third degree) | 1 | 11.1% |
| Superficial thickness (second degree), deep thickness (second degree) | 2 | 22.2% |
| Total | 9 | 100% |
| Areas of Burn | Frequency | Percent |
| anterior trunk, right legs, right posterior trunk, right hand | 1 | 11.1% |
| Both Legs | 1 | 11.1% |
| chest | 1 | 11.1% |
| Face & Chest | 2 | 22.2% |
| left leg and hand | 1 | 11.1% |
| Right hand, left leg | 1 | 11.1% |
| right side of face, right upper limb and truck, hand | 1 | 11.1% |
| thigh, both legs (anterior aspect), genitalia | 1 | 11.1% |
| Total | 9 | 100% |
| Group | N | Mean (Std. D) | Two Tailed p-Value | |
|---|---|---|---|---|
| Pain Before Wound care | VR | 9 | 2.11 (SD = 1.69) | p > 0.05 NS |
| Traditional | 9 | 2.89 (SD = 2.32) | ||
| Pain During Wound care | VR | 9 | 4.00 (SD = 2.24) | p< 0.01 ** |
| Traditional | 9 | 6.67 (SD = 2.45) | ||
| Pain After Wound care | VR | 9 | 1.56 (1.13) | p < 0.05 * |
| Traditional | 9 | 3.33 (1.73) | ||
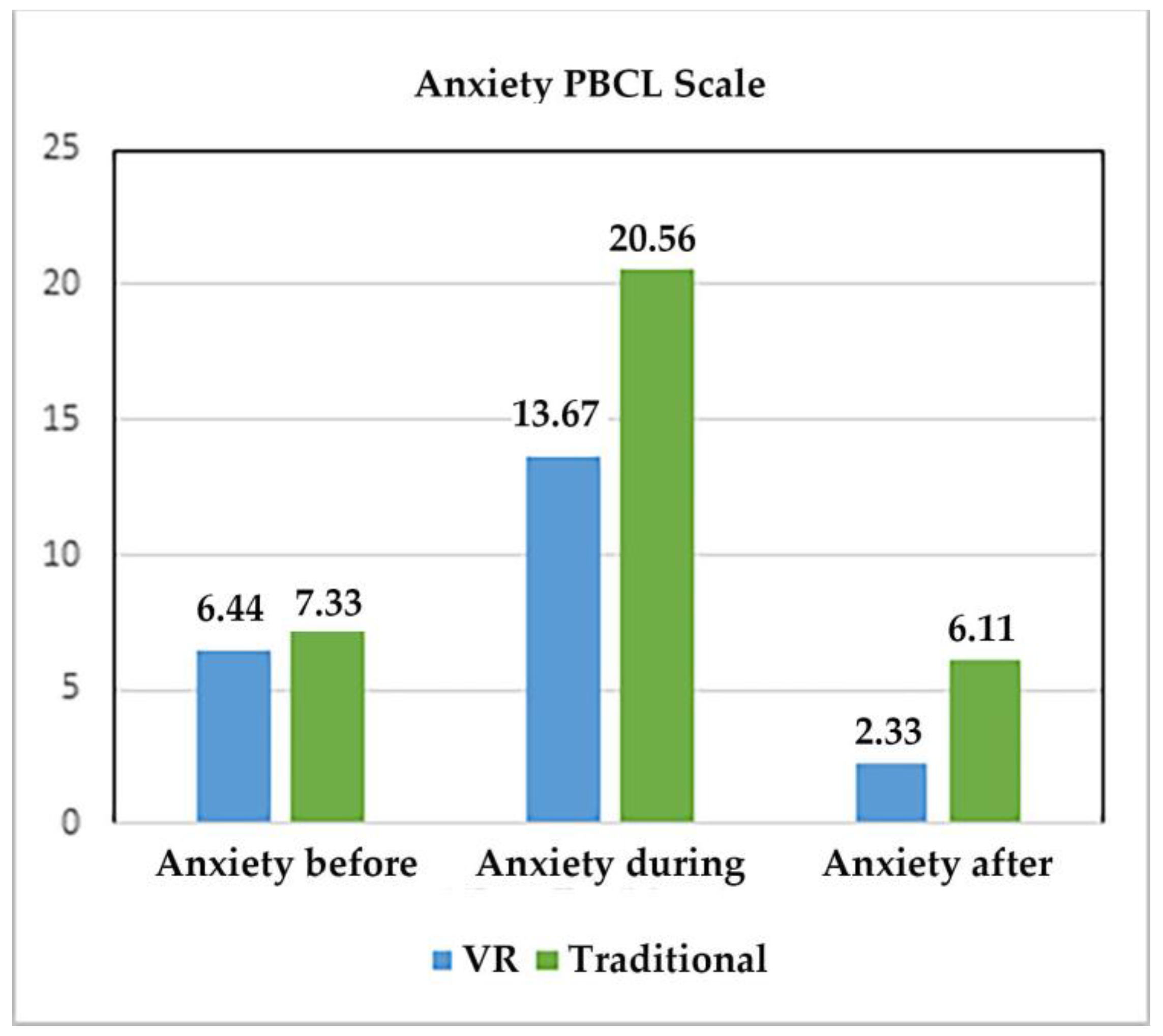
| Anxiety Before Wound care | VR | 9 | 6.44 (SD = 7.30) | Z = 1.19 p > 0.05 NS |
| Traditional | 9 | 7.33 (SD = 7.62) | ||
| Anxiety During Wound care | VR | 9 | 13.67 (SD = 8.93) | Z = 2.67, p < 0.01 ** |
| Traditional | 9 | 20.56 (SD = 8.58) | ||
| Anxiety After Wound care | VR | 9 | 2.33 (SD = 1.80) | Z = 2.25, p < 0.05 * |
| Traditional | 9 | 6.11 (SD = 4.70) |
| Group | N | Mean (Std. D) | Two Tailed p-Value | |
|---|---|---|---|---|
| Pain Before Wound care | VR | 9 | 1.89 (1.17) | p > 0.05 NS |
| Traditional | 9 | 2.11 (1.05) | ||
| Pain During Wound care | VR | 9 | 2.56 (1.01) | p < 0.05 * |
| Traditional | 9 | 4.00 (1.12) | ||
| Pain after Wound Care | VR | 9 | 1.67 (0.87) | p > 0.05 NS |
| Traditional | 9 | 2.56 (1.33) | ||
| Anxiety Before Wound care | VR | 9 | 2.67 (1.73) | p > 0.05 NS |
| Traditional | 9 | 2.78 (1.92) | ||
| Anxiety During Wound care | VR | 9 | 2.89 (1.36) | p < 0.01 ** |
| Traditional | 9 | 4.67 (0.71) | ||
| Anxiety After Wound care | VR | 9 | 1.56 (0.88) | p < 0.05 * |
| Traditional | 9 | 3.11 (1.45) |
| Question 1 | Virtual Reality helped the child control his/her pain. | 100% responded either total agree or agree (33% total agree, 67% agree). |
| Question 2 | VR helped the child to cooperate during the medical procedure | 100% responded either total agree or agree (42% total agree, 52% agree). |
| Question 3 | Use of VR delayed the wound care process related to the procedure | 100% responded either totally disagree, or disagree (17% totally disagree, 83% disagree). |
| Question 4 | I would use VR again to distract children during a painful procedure | 100% responded either totally agree or agree (75% totally agree, 25% agree). |
| Question 5 | The VR game was adapted/suitable to the age group of children | 100% responded either totally agree or agree (62% totally agree, 38% agree). |
| Question 6 | The VR device was adapted/suitable to the clinic’s environment | 100% responded either totally agree or agree (67% totally agree, 33% agree). |
| Question 7 | VR is an intervention worth implementing to distract children | 100% responded either totally agree or agree (75% totally agree, 25% agree). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrimy, T.; Alhalabi, W.; Malibari, A.; Alzahrani, F.; Alrajhi, S.; Yamani, A.; Ahmed, H.; Abduljawad, A.; Nasser, E.; ALattar, S.; et al. Desktop Virtual Reality Offers a Novel Approach to Minimize Pain and Anxiety during Burn Wound Cleaning/Debridement in Infants and Young Children: A Randomized Crossover Pilot Study. J. Clin. Med. 2023, 12, 4985. https://doi.org/10.3390/jcm12154985
Alrimy T, Alhalabi W, Malibari A, Alzahrani F, Alrajhi S, Yamani A, Ahmed H, Abduljawad A, Nasser E, ALattar S, et al. Desktop Virtual Reality Offers a Novel Approach to Minimize Pain and Anxiety during Burn Wound Cleaning/Debridement in Infants and Young Children: A Randomized Crossover Pilot Study. Journal of Clinical Medicine. 2023; 12(15):4985. https://doi.org/10.3390/jcm12154985
Chicago/Turabian StyleAlrimy, Taima, Wadee Alhalabi, Areej Malibari, Fatma Alzahrani, Sharifah Alrajhi, Ayman Yamani, Halah Ahmed, Amro Abduljawad, Essam Nasser, Samar ALattar, and et al. 2023. "Desktop Virtual Reality Offers a Novel Approach to Minimize Pain and Anxiety during Burn Wound Cleaning/Debridement in Infants and Young Children: A Randomized Crossover Pilot Study" Journal of Clinical Medicine 12, no. 15: 4985. https://doi.org/10.3390/jcm12154985
APA StyleAlrimy, T., Alhalabi, W., Malibari, A., Alzahrani, F., Alrajhi, S., Yamani, A., Ahmed, H., Abduljawad, A., Nasser, E., ALattar, S., Alharby, B., Khalid, H., Alhalabi, M., Hoffman, H. G., & Mason, K. P. (2023). Desktop Virtual Reality Offers a Novel Approach to Minimize Pain and Anxiety during Burn Wound Cleaning/Debridement in Infants and Young Children: A Randomized Crossover Pilot Study. Journal of Clinical Medicine, 12(15), 4985. https://doi.org/10.3390/jcm12154985





