Assessment by Women on Selected Aspects of Quality of Life and on Disease Acceptance after Undergoing Urogynecological Procedures for Urinary Incontinence
Abstract
1. Introduction
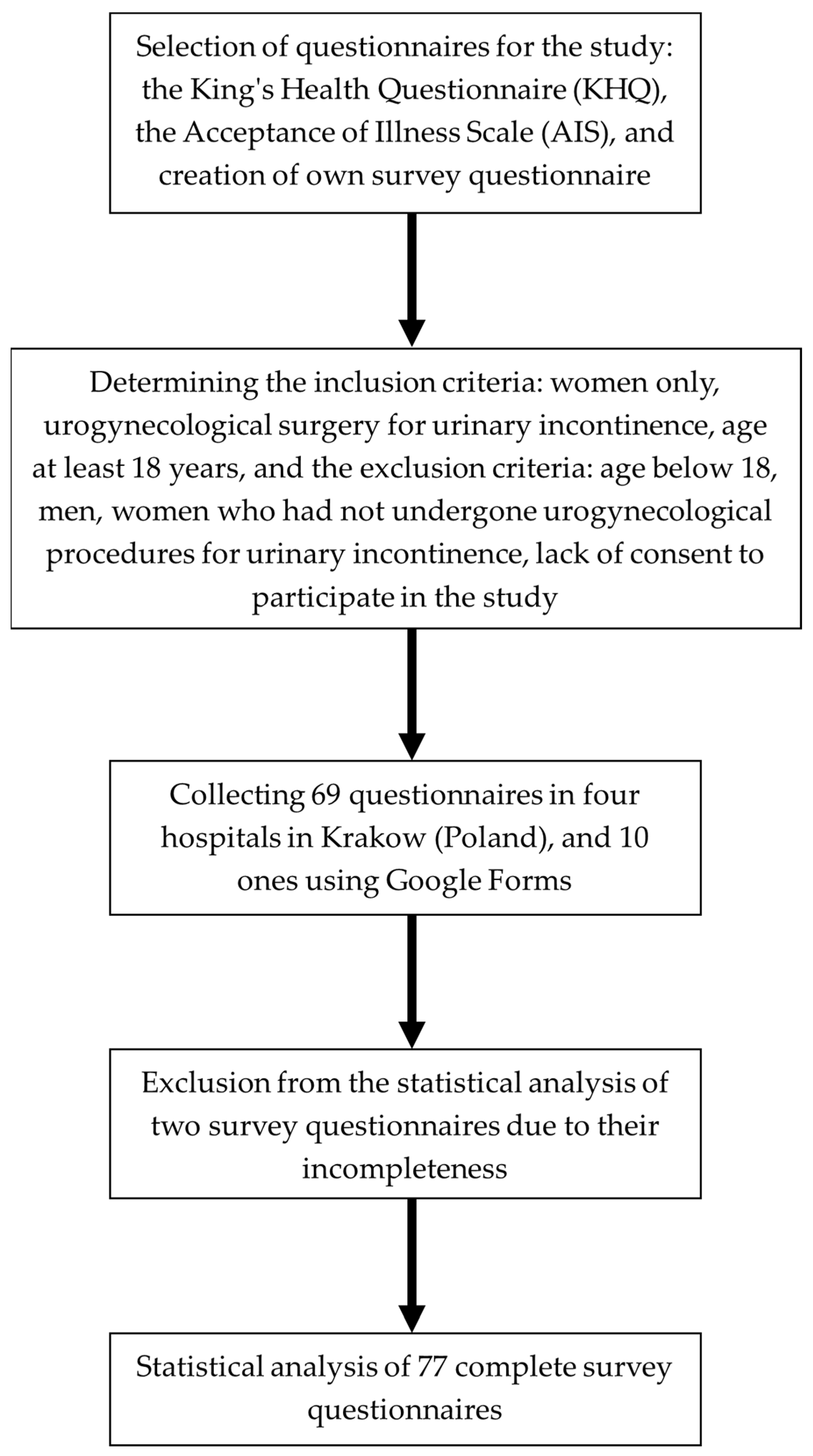
2. Materials and Methods
Statistical Analysis
3. Results
3.1. The KHQ Results
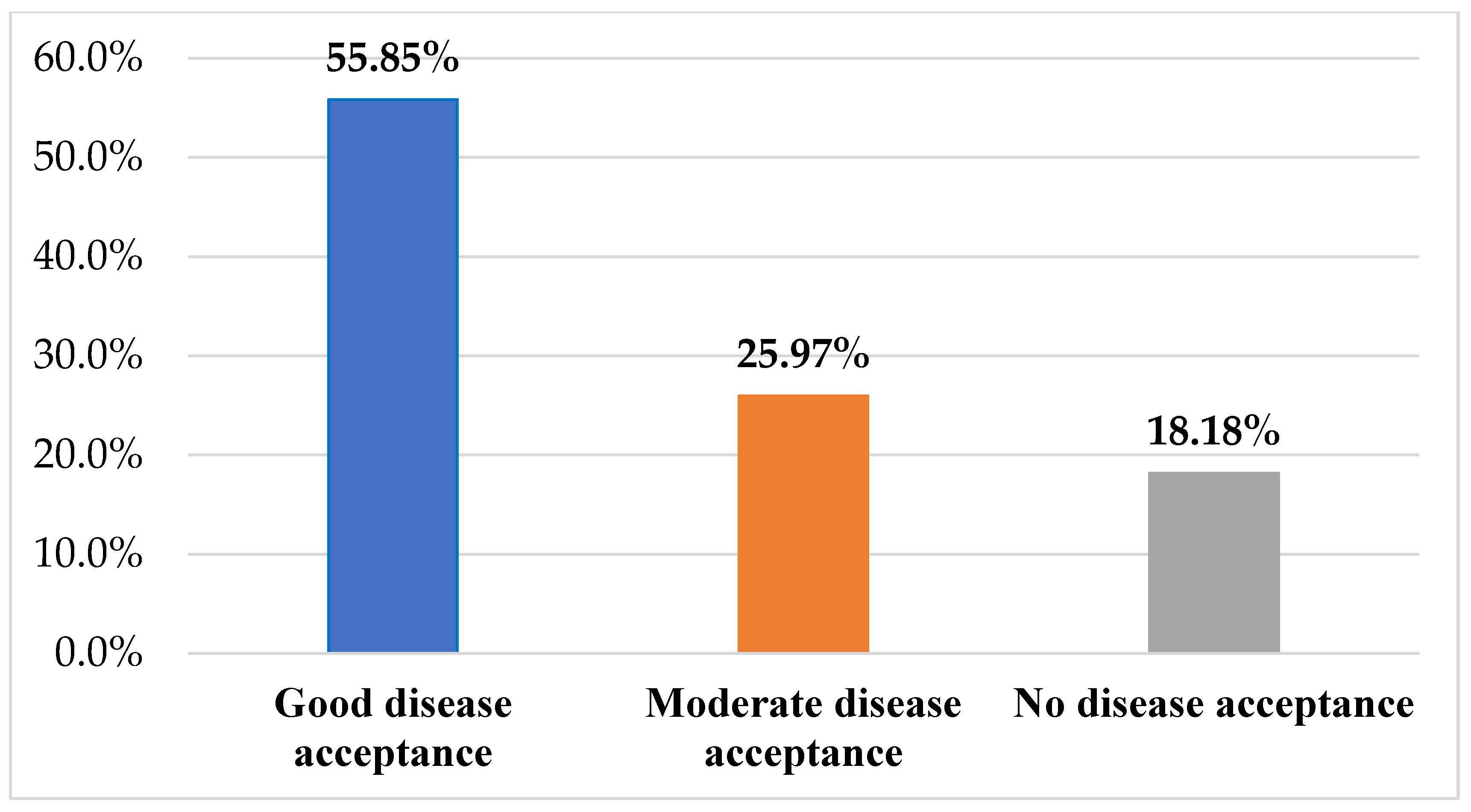
3.2. The AIS Scale Results
3.3. Correlation between the AIS Scale and the KHQ
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Åström, Y.; Asklund, I.; Lindam, A.; Sjöström, M. Quality of life in women with urinary incontinence seeking care using e-health. BMC Womens Health 2021, 21, 337. [Google Scholar] [CrossRef] [PubMed]
- Elenskaia, K.; Haidvogel, K.; Heidinger, C.; Doerfler, D.; Umek, W.; Hanzal, E. The greatest taboo: Urinary incontinence as a source of shame and embarrassment. Wien Klin Wochenschr. 2011, 123, 607–610. [Google Scholar] [CrossRef] [PubMed]
- Bardsley, A. An overview of urinary incontinence. Br. J. Nurs. 2016, 25, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Schreiber Pedersen, L.; Lose, G.; Høybye, M.T.; Jürgensen, M.; Waldmann, A.; Rudnicki, M. Predictors and reasons for help-seeking behavior among women with urinary incontinence. Int. Urogynecol. J. 2017, 29, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Gümüşsoy, S.; Kavlak, O.; Donmez, S. Investigation of body image, self-esteem, and quality of life in women with urinary incontinence. Int. J. Nurs. Pr. 2019, 25, e12762. [Google Scholar] [CrossRef]
- Corrado, B.; Giardulli, B.; Polito, F.; Aprea, S.; Lanzano, M.; Dodaro, C. The Impact of Urinary Incontinence on Quality of Life: A Cross-Sectional Study in the Metropolitan City of Naples. Geriatrics 2020, 5, 96. [Google Scholar] [CrossRef]
- Steibliene, V.; Aniuliene, R.; Aniulis, P.; Raskauskiene, N.; Adomaitiene, V. Affective Symptoms and Health-Related Quality of Life Among Women with Stress Urinary Incontinence: Cross-Sectional Study. Neuropsychiatr. Dis. Treat. 2020, 16, 535–544. [Google Scholar] [CrossRef]
- Moran, P.A.; Dwyer, P.L.; Ziccone, S.P. Urinary leakage during coitus in women. J. Obstet. Gynaecol. 1999, 19, 286–288. [Google Scholar]
- Coyne, K.S.; Sexton, C.C.; Irwin, D.E.; Kopp, Z.S.; Kelleher, C.J.; Milsom, I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: Results from the EPIC study. BJU Int. 2008, 101, 1388–1395. [Google Scholar] [CrossRef]
- Özdemir, K.; Şahin, S.; Özerdoğan, N.; Ünsal, A. Evaluation of urinary incontinence and quality of life in married women aged between 20 and 49 years (Sakarya, Turkey). Turk. J. Med. Sci. 2018, 48, 100–109. [Google Scholar] [CrossRef]
- Kwon, B.E.; Kim, G.Y.; Son, Y.J.; Roh, Y.S.; You, M.A. Quality of life of women with urinary incontinence: A systematic literature review. Int. Neurourol. J. 2010, 14, 133–138. [Google Scholar] [CrossRef]
- Pizzol, D.; Demurtas, J.; Celotto, S.; Maggi, S.; Smith, L.; Angiolelli, G.; Trott, M.; Yang, L.; Veronese, N. Urinary incontinence and quality of life: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2021, 33, 25–35. [Google Scholar] [CrossRef]
- Hashim, H.; Blanker, M.H.; Drake, M.J.; Djurhuus, J.C.; Meijlink, J.; Morris, V.; Petros, P.; Wen, J.G.; Wein, A. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 2019, 38, 499–508. [Google Scholar] [CrossRef]
- Lukacz, E.S.; Santiago-Lastra, Y.; Albo, M.E.; Brubaker, L. Urinary Incontinence in Women: A Review. JAMA 2017, 318, 1592–1604. [Google Scholar] [CrossRef] [PubMed]
- Martínez Agulló, E.; Ruíz Cerdá, J.L.; Gómez Pérez, L.; Rebollo, P.; Pérez, M.; Chaves, J. Impact of urinary incontinence and over-active bladder syndrome on health-related quality of life of working middle-aged patients and institutionalized elderly patients. Actas Urol. Esp 2010, 34, 242–250. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Post, M.W. Definitions of quality of life: What has happened and how to move on. Top Spinal Cord Inj. Rehabil. 2014, 20, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Senra, C.; Pereira, M.G. Quality of life in women with urinary incontinence. Rev. Assoc. Med. Bras. (1992) 2015, 61, 178–183. [Google Scholar] [CrossRef]
- Fernandes, S.; Carvalho Coutinho, E.; Carvalho Duarte, J.; Batista Nelas, P.A.; Correia Balula Chaves, C.M.; Amaral, O. Quality of life in women with Urinary Incontinence. J. Nurs. 2015, 4, 93–99. [Google Scholar] [CrossRef]
- Mikuš, M.; Kalafatić, D.; Vrbanić, A.; Šprem Goldštajn, M.; Herman, M.; Živković Njavro, M.; Živković, K.; Marić, G.; Ćorić, M. Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial. Medicina (Kaunas) 2022, 58, 1863. [Google Scholar] [CrossRef]
- Frutos-Reoyo, E.J.; Luque-Linero, P.; Cantalapiedra-Puentes, E.; Mendi-Gabarain, I.; Bermejo-de la Fuente, P.; Candau-Pérez, E.D. Factores pronósticos del resultado del tratamiento rehabilitador en la incontinencia urinaria femenina. Actas Urológicas Españolas 2023, 47, 376–381. [Google Scholar] [CrossRef]
- Riemsma, R.; Hagen, S.; Kirschner-Hermanns, R.; Norton, C.; Wijk, H.; Andersson, K.E.; Chapple, C.; Spinks, J.; Wagg, A.; Hutt, E.; et al. Can incontinence be cured? A systematic review of cure rates. BMC Med. 2017, 15, 63. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, C.J.; Cardozo, L.D.; Khullar, V.; Salvatore, S. A new questionnaire to assess the quality of life of urinary incontinent women. Br. J. Obstet. Gynaecol 1997, 104, 1374–1379. [Google Scholar] [CrossRef] [PubMed]
- Felton, B.J.; Revenson, T.A.; Hinrichsen, G.A. Stress and coping in the explanation of psychological adjustment among chronically ill adults. Soc. Sci. Med. 1984, 18, 889–898. [Google Scholar] [CrossRef]
- Skorupska, K.; Grzybowska, M.E.; Kubik-Komar, A.; Rechberger, T.; Miotla, P. Identification of the Urogenital Distress Inventory-6 and the Incontinence Impact Questionnaire-7 cutoff scores in urinary incontinent women. Health Qual Life Outcomes 2021, 19, 87. [Google Scholar] [CrossRef]
- Malik, R.D.; Hess, D.S.; Christie, A.; Carmel, M.E.; Zimmern, P.E. Domain Comparison Between 6 Validated Questionnaires Administered to Women With Urinary Incontinence. Urology 2019, 132, 75–80. [Google Scholar] [CrossRef]
- Kieres, P.; Skorupska, K.; Mlodawski, J.; Misiek, M.; Rokita, W.; Rechberger, T. Reliability of The King’s Health Questionnaire and the International Consultation on Incontinence Modular Questionnaire (ICIQ-SF) Short Form in assessing urinary incontinence effects in Polish women. Ginekol. Pol. 2021, 92, 850–855. [Google Scholar] [CrossRef]
- Wróbel, A.; Skorupska, K.; Rechberger, E.; Woźniak, A.; Miotla, P.; Kubik-Komar, A.; Skorupski, P.; Rechberger, T. Reliability of the Polish version of the Overactive Bladder Symptom Score (OABSS) questionnaire: Correlation of the OABSS with urodynamic study and the UDI-6 and IIQ-7 questionnaires. Int. Urogynecol. J. 2019, 30, 2135–2139. [Google Scholar] [CrossRef]
- Mikuš, M.; Ćorić, M.; Matak, L.; Škegro, B.; Vujić, G.; Banović, V. Validation of the UDI-6 and the ICIQ-UI SF—Croatian version. Int. Urogynecol. J. 2020, 31, 2625–2630. [Google Scholar] [CrossRef]
- Brandt, F.; Solomayer, E.F.; Sklavounos, P. Correlation between the Incontinence Severity Index (ISI) and the quality of life dimensions of the King’s Health Questionnaire (KHQ) in German-speaking urinary incontinent women. J. Gynecol. Obstet. Hum Reprod. 2022, 51, 102288. [Google Scholar] [CrossRef] [PubMed]
- Minassian, V.A.; Devore, E.; Hagan, K.; Grodstein, F. Severity of urinary incontinence and effect on quality of life in women by incontinence type. Obstet. Gynecol. 2013, 121, 1083–1090. [Google Scholar] [CrossRef]
- Burzyński, B.; Kwiatkowska, K.; Sołtysiak-Gibała, Z.; Bryniarski, P.; Przymuszała, P.; Wlaźlak, E.; Rzymski, P. Impact of stress urinary incontinence on female sexual activity. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 643–653. [Google Scholar] [PubMed]
- Nilsson, M.; Lalos, O.; Lindkvist, H.; Lalos, A. How do urinary incontinence and urgency affect women’s sexual life? Acta Obstet. Et Gynecol. Scand. 2011, 90, 621–628. [Google Scholar] [CrossRef] [PubMed]
| Variables | M | SD | |
|---|---|---|---|
| Age | 54.46 | 12.20 | |
| Time since surgery | 4.35 | 4.82 | |
| Duration of illness | 5.04 | 3.32 | |
| N | % | ||
| Marital status | married | 59 | 76.62% |
| widowed | 12 | 15.58% | |
| divorced | 4 | 5.19% | |
| single | 1 | 1.30% | |
| casual relationship | 1 | 1.30% | |
| Type of delivery | natural childbirth | 62 | 80.52% |
| cesarean section | 11 | 14.29% | |
| both natural childbirth and cesarean section | 4 | 5.19% | |
| Type of urinary incontinence | stress urinary incontinence | 43 | 55.84% |
| mixed incontinence | 20 | 25.97% | |
| overactive bladder (urge incontinence) | 4 | 5.19% | |
| Urogynecological procedures | TVT sling | 25 | 32.47% |
| TOT sling | 23 | 29.87% | |
| vaginoplasty | 16 | 20.78% | |
| colposuspension | 6 | 7.79% | |
| no specific answer | 7 | 9.09% |
| Impact of Bladder Dysfunction on Daily Life as Assessed by Women | N | % |
|---|---|---|
| Not at all | 10 | 12.99 |
| Somewhat | 22 | 28.57 |
| Moderate | 19 | 24.68 |
| Very | 26 | 33.77 |
| Exacerbation of Symptoms Related to Bladder Function | None | Somewhat | Moderate | Rather Severe |
|---|---|---|---|---|
| Frequent use of toilet | 18 (23.38%) | 13 (16.88%) | 38 (49.35%) | 8 (10.39%) |
| Nocturia: getting up during the night to micturate | 19 (24.68%) | 23 (29.87%) | 28 (36.36%) | 7 (9.09%) |
| Sudden urge: a strong and difficult to control urge to urinate | 30 (38.96%) | 20 (25.97%) | 19 (24.68%) | 8 (10.39%) |
| Urge incontinence: urinary leakage associated with a strong need to urinate | 25 (32.47%) | 16 (20.78%) | 23 (29.87%) | 13 (16.88%) |
| Stress urinary incontinence: release of urine with physical activity, including coughing, sneezing, running | 21 (27.27%) | 23 (29.87%) | 12 (15.58%) | 21 (27.27%) |
| Bedwetting at night | 49 (63.64%) | 16 (20.78%) | 9 (11.69%) | 3 (3.90%) |
| Urinary incontinence during intercourse: urinary leakage | 55 (71.43%) | 13 (16.88%) | 8 (1.30%) | 1 (1.30%) |
| Frequent bladder infections | 33 (42.86%) | 21 (27.27%) | 18 (23.38%) | 5 (6.49%) |
| Bladder pain | 40 (51.95%) | 22 (28.57%) | 13 (16.88%) | 2 (2.60%) |
| Urinating difficulty | 45 (58.44%) | 17 (22.08%) | 13 (16.88%) | 2 (2.60%) |
| The Level and Extent of Limitations in the Performance of Daily Activities in the Subjective Assessment of Respondents | None | Somewhat | Moderate | Rather Severe | |
|---|---|---|---|---|---|
| Performing daily household chores such as cleaning, cooking, shopping | 33 (42.86%) | 27 (35.06%) | 12 (15.58%) | 5 (6.49%) | |
| Performing professional duties (work) and other activities outside the home | 23 (29.87%) | 33 (42.86%) | 16 (20.78%) | 5 (6.49%) | |
| Type and degree of physical and social limitation | None | Somewhat | Moderate | Rather severe | |
| Impact on physical activity, e.g., walking, running, playing sports, going to the gym, etc. | 25 (32.47%) | 32 (41.56%) | 12 (15.58%) | 8 (10.39%) | |
| Traveling | 23 (29.87%) | 30 (38.96%) | 19 (24.68%) | 5 (6.49%) | |
| Limiting social contacts | 45 (58.44%) | 15 (19.48%) | 12 (15.58%) | 5 (6.49%) | |
| Social gatherings, e.g., friends, acquaintances | 48 (62.34%) | 18 (23.38%) | 8 (10.39%) | 3 (3.90%) | |
| Personal life | Not applicable | None | Somewhat | Moderate | Rather severe |
| Impact on relationship with partner | 26 (33.77%) | 29 (37.66%) | 16 (20.78%) | 4 (5.19%) | 2 (2.60%) |
| Impact on sex life | 30 (38.96%) | 23 (29.87%) | 18 (23.38%) | 3 (3.90%) | 3 (3.90%) |
| Impact on family life | 17 (22.08%) | 38 (49.35%) | 15 (19.48%) | 5 (6.49%) | 2 (2.60%) |
| Type and intensity of emotions | None | Somewhat | Moderate | Rather severe | |
| Sense of despondency | 30 (38.96%) | 36 (46.75%) | 6 (7.79%) | 5 (6.49%) | |
| Sense of uncertainty | 26 (33.77%) | 37 (48.05%) | 6 (7.79%) | 8 (10.39%) | |
| Lowered self-esteem | 47 (61.04%) | 18 (23.38%) | 8 (10.39%) | 4 (5.19%) | |
| Level of rest and well-being as subjectively assessed by respondents | Never | Sometimes | Often | Continuous | |
| Sleep disorders | 17 (22.08%) | 49 (63.64%) | 8 (10.39%) | 3 (3.90%) | |
| Feelings of fatigue or exhaustion | 28 (36.36%) | 38 (49.35%) | 10 (12.99%) | 1 (1.30%) | |
| Type and severity of discomfort as subjectively assessed by subjects | Never | Sometimes | Often | Continuous | |
| Wearing sanitary pads to keep underwear dry | 13 (16.88%) | 24 (31.17%) | 17 (22.08%) | 23 (29.87%) | |
| Paying special attention to the amount of fluid intake | 18 (23.38%) | 20 (25.97%) | 29 (37.66%) | 10 (12.99%) | |
| The need to change underwear as a result of urine wetting | 14 (18.18%) | 20 (25.97%) | 20 (25.97%) | 23 (29.87%) | |
| Emitting an unpleasant odor | 11 (14.29%) | 25 (32.47%) | 24 (31.17%) | 17 (22.08%) | |
| Feelings of shame and embarrassment due to bladder dysfunction | 21 (27.27%) | 30 (38.96%) | 14 (18.18%) | 12 (15.58%) | |
| Quality of Life Measured by the KHQ | N | M | SD | Min | Max | Me |
|---|---|---|---|---|---|---|
| General health | 77 | 28.90 | 19.89 | 0.0 | 75.0 | 25.0 |
| Impact of bladder problems on life | 77 | 59.74 | 35.18 | 0.0 | 100.0 | 66.67 |
| Limitations in performing daily activities | 77 | 31.60 | 28.17 | 0.0 | 100.0 | 33.33 |
| Physical limitations | 77 | 35.28 | 28.09 | 0.0 | 100.0 | 33.33 |
| Social limitations | 77 | 19.48 | 26.42 | 0.0 | 100.0 | 0.0 |
| Personal life | 52 | 19.23 | 26.07 | 0.0 | 100.0 | 0.0 |
| Emotions | 77 | 26.26 | 26.30 | 0.0 | 100.0 | 22.22 |
| Sleep/effort | 77 | 29.22 | 21.32 | 0.0 | 100.0 | 33.33 |
| Measures of discomfort severity | 77 | 52.81 | 26.30 | 0.0 | 100.0 | 58.33 |
| Symptom severity scale | 77 | 9.73 | 5.87 | 0.0 | 23.0 | 10.0 |
| Quality of Life Measured by the KHQ | Correlation with Time Since Surgery | Correlation with Age | ||||
|---|---|---|---|---|---|---|
| N | R | p | N | R | p | |
| General health | 77 | −0.007697 | 0.947029 | 77 | 0.242346 | 0.033707 |
| Impact of bladder problems on life | 77 | −0.068215 | 0.555539 | 77 | −0.213992 | 0.061655 |
| Limitations in performing daily activities | 77 | −0.047073 | 0.684348 | 77 | 0.251398 | 0.027421 |
| Physical limitations | 77 | −0.051267 | 0.657909 | 77 | 0.141897 | 0.218316 |
| Social limitations | 77 | 0.029256 | 0.800599 | 77 | 0.179496 | 0.118282 |
| Personal life | 52 | 0.134097 | 0.343248 | 52 | 0.214453 | 0.126843 |
| Emotions | 77 | −0.275918 | 0.015144 | 77 | 0.095812 | 0.407157 |
| Sleep/effort | 77 | 0.085877 | 0.457713 | 77 | 0.177132 | 0.123289 |
| Measures of discomfort severity | 77 | −0.039211 | 0.734929 | 77 | 0.101124 | 0.381522 |
| Symptom severity scale | 77 | 0.017807 | 0.877838 | 77 | 0.090110 | 0.435766 |
| AIS Scale | N | M | SD | Min | Max | Me |
|---|---|---|---|---|---|---|
| Overall score | 77 | 29.06 | 10.23 | 8.0 | 40.0 | 32.0 |
| Quality of Life Measured by the KHQ | Correlation with Acceptance Level of the Disease as Measured by the AIS Scale | ||
|---|---|---|---|
| N | R | p | |
| General health | 77 | −0.236060 | 0.038748 |
| Impact of bladder problems on life | 77 | −0.153440 | 0.182759 |
| Limitations in performing daily activities | 77 | −0.526714 | 0.000001 |
| Physical limitations | 77 | −0.554072 | <0.00001 |
| Social limitations | 77 | −0.474735 | 0.000013 |
| Personal life | 52 | −0.318305 | 0.021465 |
| Emotions | 77 | −0.602849 | <0.00001 |
| Sleep/effort | 77 | −0.496894 | 0.000004 |
| Measures of discomfort severity | 77 | −0.563252 | 0.000000 |
| Symptom severity scale | 77 | −0.398549 | 0.000331 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baczewska, B.; Wiśniewska, K.; Muraczyńska, B.; Pasek, M.; Słuszniak, J.; Gębicka, K.; Guzak, B. Assessment by Women on Selected Aspects of Quality of Life and on Disease Acceptance after Undergoing Urogynecological Procedures for Urinary Incontinence. J. Clin. Med. 2023, 12, 4894. https://doi.org/10.3390/jcm12154894
Baczewska B, Wiśniewska K, Muraczyńska B, Pasek M, Słuszniak J, Gębicka K, Guzak B. Assessment by Women on Selected Aspects of Quality of Life and on Disease Acceptance after Undergoing Urogynecological Procedures for Urinary Incontinence. Journal of Clinical Medicine. 2023; 12(15):4894. https://doi.org/10.3390/jcm12154894
Chicago/Turabian StyleBaczewska, Bożena, Katarzyna Wiśniewska, Bożena Muraczyńska, Małgorzata Pasek, Jolanta Słuszniak, Katarzyna Gębicka, and Beata Guzak. 2023. "Assessment by Women on Selected Aspects of Quality of Life and on Disease Acceptance after Undergoing Urogynecological Procedures for Urinary Incontinence" Journal of Clinical Medicine 12, no. 15: 4894. https://doi.org/10.3390/jcm12154894
APA StyleBaczewska, B., Wiśniewska, K., Muraczyńska, B., Pasek, M., Słuszniak, J., Gębicka, K., & Guzak, B. (2023). Assessment by Women on Selected Aspects of Quality of Life and on Disease Acceptance after Undergoing Urogynecological Procedures for Urinary Incontinence. Journal of Clinical Medicine, 12(15), 4894. https://doi.org/10.3390/jcm12154894






