A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with Idiopathic Pulmonary Fibrosis: The PolExNIB Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
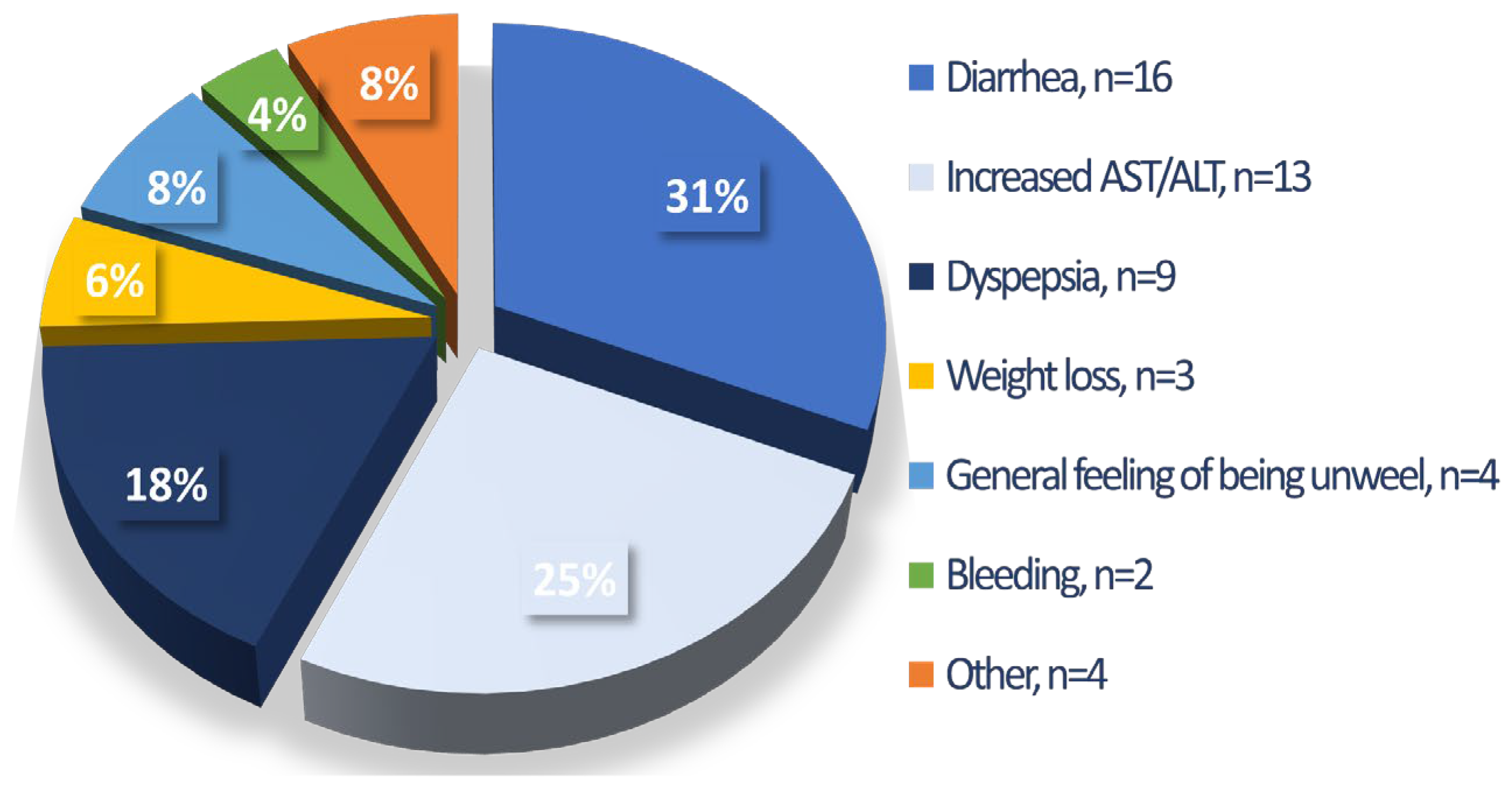
3.2. Tolerability, Safety, and Drug Persistence
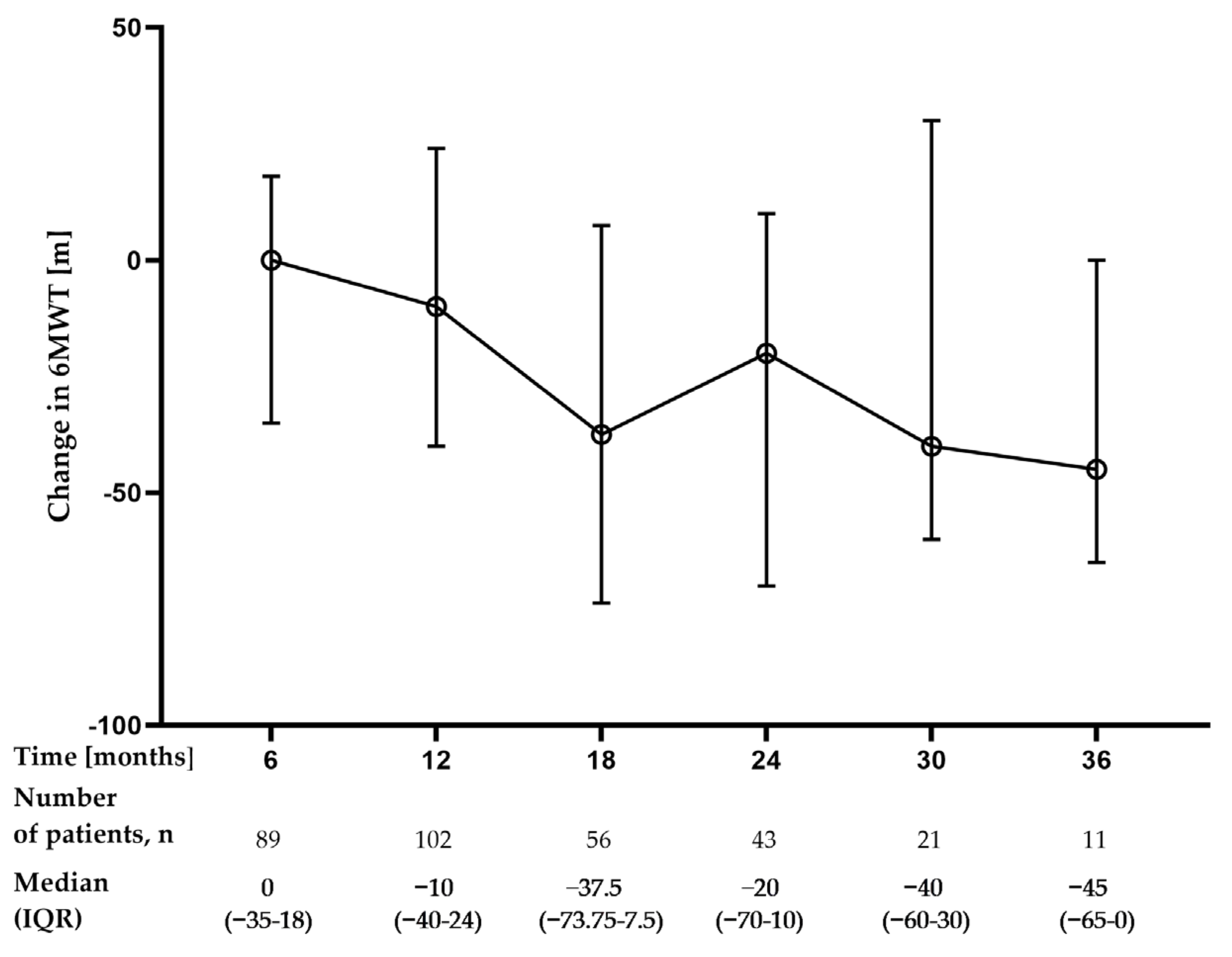
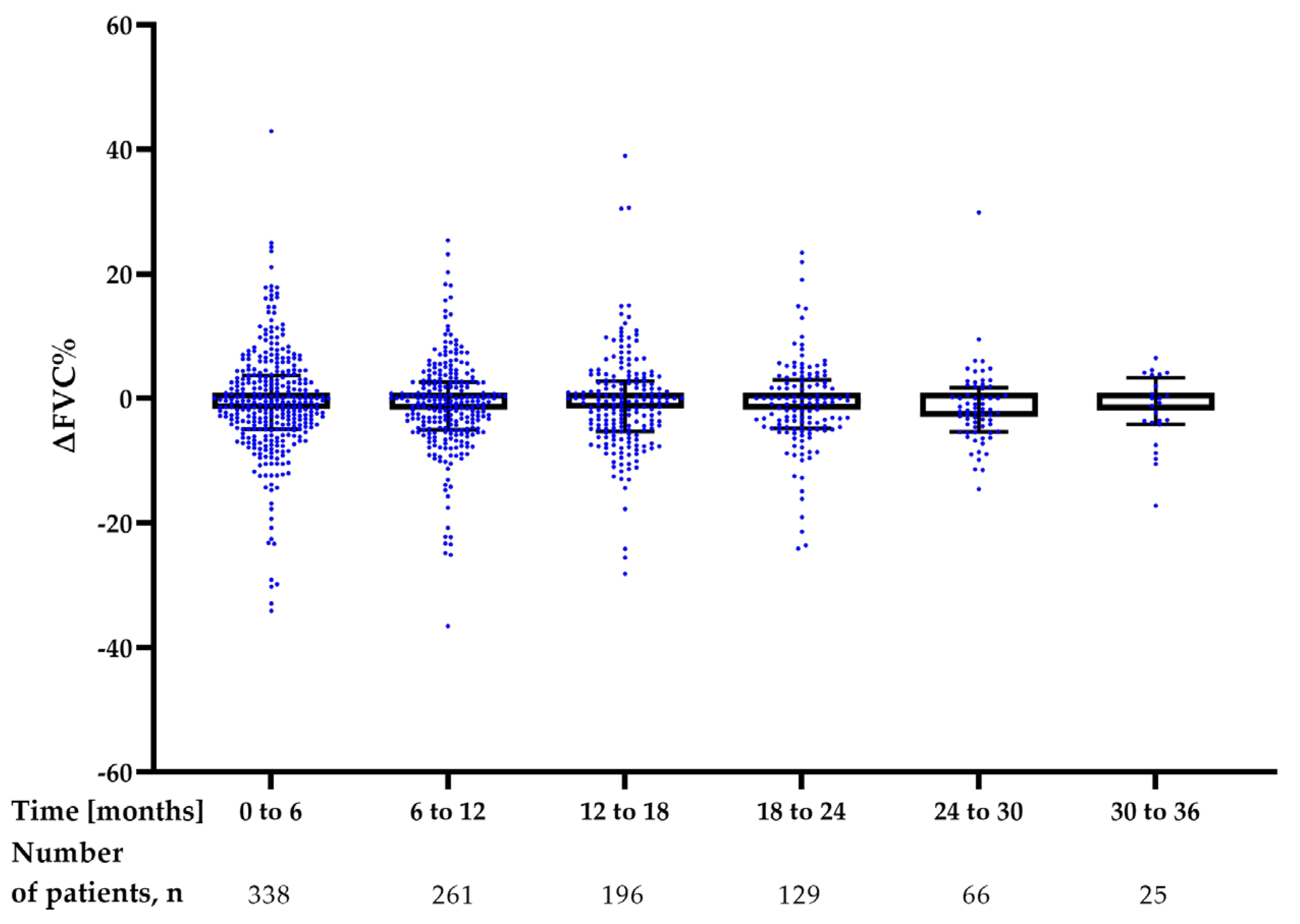
3.3. Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raghu, G.; Remy-Jardin, M.; Myers, J.L.; Richeldi, L.; Ryerson, C.J.; Lederer, D.J.; Behr, J.; Cottin, V.; Danoff, S.K.; Morell, F.; et al. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2018, 198, e44–e68. [Google Scholar] [CrossRef]
- Lederer, D.J.; Martinez, F.J. Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2018, 378, 1811–1823. [Google Scholar] [CrossRef]
- Kim, D.S.; Collard, H.R.; King, T.E. Classification and natural history of the idiopathic interstitial pneumonias. Proc. Am. Thorac. Soc. 2006, 3, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Noble, P.W.; Albera, C.; Bradford, W.Z.; Costabel, U.; Glassberg, M.K.; Kardatzke, D.; King, T.E.; Lancaster, L.; Sahn, S.A.; Szwarcberg, J.; et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): Two randomised trials. Lancet Lond. Engl. 2011, 377, 1760–1769. [Google Scholar] [CrossRef] [PubMed]
- King, T.E.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2083–2092. [Google Scholar] [CrossRef]
- Richeldi, L.; du Bois, R.M.; Raghu, G.; Azuma, A.; Brown, K.K.; Costabel, U.; Cottin, V.; Flaherty, K.R.; Hansell, D.M.; Inoue, Y.; et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2071–2082. [Google Scholar] [CrossRef]
- Raghu, G.; Rochwerg, B.; Zhang, Y.; Garcia, C.A.C.; Azuma, A.; Behr, J.; Brozek, J.L.; Collard, H.R.; Cunningham, W.; Homma, S.; et al. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2015, 192, e3–e19. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, W.J.; Bestry, I.; Białas, A.J.; Boros, P.W.; Grzanka, P.; Jassem, E.; Jastrzębski, D.; Klimczak, D.; Langfort, R.; Lewandowska, K.; et al. Guidelines of the Polish Respiratory Society for diagnosis and treatment of idiopathic pulmonary fibrosis. Adv. Respir. Med. 2020, 88, 41–93. [Google Scholar] [CrossRef]
- Piotrowski, W.J.; Martusewicz-Boros, M.M.; Białas, A.J.; Lewandowska, K. Idiopathic pulmonary fibrosis (IPF)—Common practice in Poland before the “antifibrotic drugs era”. Adv. Respir. Med. 2017, 85, 136–142. [Google Scholar] [CrossRef]
- Idiopathic Pulmonary Fibrosis Clinical Research Network; Raghu, G.; Anstrom, K.J.; King, T.E.; Lasky, J.A.; Martinez, F.J. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N. Engl. J. Med. 2012, 366, 1968–1977. [Google Scholar] [CrossRef]
- Bonella, F.; Kreuter, M.; Hagmeyer, L.; Neurohr, C.; Keller, C.; Kohlhaeufl, M.J.; Müller-Quernheim, J.; Milger, K.; Prasse, A. German Nintedanib Compassionate Use Consortium Insights from the German Compassionate Use Program of Nintedanib for the Treatment of Idiopathic Pulmonary Fibrosis. Respir. Int. Rev. Thorac. Dis. 2016, 92, 98–106. [Google Scholar] [CrossRef]
- Toellner, H.; Hughes, G.; Beswick, W.; Crooks, M.G.; Donaldson, C.; Forrest, I.; Hart, S.P.; Leonard, C.; Major, M.; Simpson, A.J.; et al. Early clinical experiences with nintedanib in three UK tertiary interstitial lung disease centres. Clin. Transl. Med. 2017, 6, 41. [Google Scholar] [CrossRef]
- Galli, J.A.; Pandya, A.; Vega-Olivo, M.; Dass, C.; Zhao, H.; Criner, G.J. Pirfenidone and nintedanib for pulmonary fibrosis in clinical practice: Tolerability and adverse drug reactions. Respirology 2017, 22, 1171–1178. [Google Scholar] [CrossRef]
- Tzouvelekis, A.; Karampitsakos, T.; Kontou, M.; Granitsas, A.; Malliou, I.; Anagnostopoulos, A.; Ntolios, P.; Tzilas, V.; Bouros, E.; Steiropoulos, P.; et al. Safety and efficacy of nintedanib in idiopathic pulmonary fibrosis: A real-life observational study in Greece. Pulm. Pharmacol. Ther. 2018, 49, 61–66. [Google Scholar] [CrossRef]
- Yoon, H.-Y.; Park, S.; Kim, D.S.; Song, J.W. Efficacy and safety of nintedanib in advanced idiopathic pulmonary fibrosis. Respir. Res. 2018, 19, 203. [Google Scholar] [CrossRef]
- Harari, S.; Caminati, A.; Poletti, V.; Confalonieri, M.; Gasparini, S.; Lacedonia, D.; Luppi, F.; Pesci, A.; Sebastiani, A.; Spagnolo, P.; et al. A Real-Life Multicenter National Study on Nintedanib in Severe Idiopathic Pulmonary Fibrosis. Respir. Int. Rev. Thorac. Dis. 2018, 95, 433–440. [Google Scholar] [CrossRef]
- Nakamura, M.; Okamoto, M.; Fujimoto, K.; Ebata, T.; Tominaga, M.; Nouno, T.; Zaizen, Y.; Kaieda, S.; Tsuda, T.; Kawayama, T.; et al. A retrospective study of the tolerability of nintedanib for severe idiopathic pulmonary fibrosis in the real world. Ann. Transl. Med. 2019, 7, 262. [Google Scholar] [CrossRef]
- Brunnemer, E.; Wälscher, J.; Tenenbaum, S.; Hausmanns, J.; Schulze, K.; Seiter, M.; Heussel, C.P.; Warth, A.; Herth, F.J.F.; Kreuter, M. Real-World Experience with Nintedanib in Patients with Idiopathic Pulmonary Fibrosis. Respir. Int. Rev. Thorac. Dis. 2018, 95, 301–309. [Google Scholar] [CrossRef]
- Pereira, C.A.d.C.; Baddini-Martinez, J.A.; Baldi, B.G.; Jezler, S.F.d.O.; Rubin, A.S.; Alves, R.L.R.; Zonzin, G.A.; Quaresma, M.; Trampisch, M.; Rabahi, M.F. Safety and tolerability of nintedanib in patients with idiopathic pulmonary fibrosis in Brazil. J. Bras. Pneumol. 2019, 45, e20180414. [Google Scholar] [CrossRef]
- Cerri, S.; Monari, M.; Guerrieri, A.; Donatelli, P.; Bassi, I.; Garuti, M.; Luppi, F.; Betti, S.; Bandelli, G.; Carpano, M.; et al. Real-life comparison of pirfenidone and nintedanib in patients with idiopathic pulmonary fibrosis: A 24-month assessment. Respir. Med. 2019, 159, 105803. [Google Scholar] [CrossRef]
- Antoniou, K.; Markopoulou, K.; Tzouvelekis, A.; Trachalaki, A.; Vasarmidi, E.; Organtzis, J.; Tzilas, V.; Bouros, E.; Kounti, G.; Rampiadou, C.; et al. Efficacy and safety of nintedanib in a Greek multicentre idiopathic pulmonary fibrosis registry: A retrospective, observational, cohort study. ERJ Open Res. 2020, 6, 00172–02019. [Google Scholar] [CrossRef] [PubMed]
- Dobashi, M.; Tanaka, H.; Taima, K.; Itoga, M.; Ishioka, Y.; Shiratori, T.; Okumura, F.; Tabe, C.; Tanaka, Y.; Morimoto, T.; et al. The efficacy of nintedanib in 158 patients with idiopathic pulmonary fibrosis in real-world settings: A multicenter retrospective study. SAGE Open Med. 2021, 9, 20503121211023356. [Google Scholar] [CrossRef] [PubMed]
- Talwar, D.; Prajapat, D.K.; Talwar, D. Real world efficacy and safety of nintedanib in idiopathic pulmonary fibrosis: A single center, observational study from India. Lung India 2022, 39, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Levra, S.; Guida, G.; Sprio, A.E.; Crosa, F.; Ghio, P.C.; Bertolini, F.; Carriero, V.; Albera, C.; Ricciardolo, F.L.M. Long-Term Safety of Antifibrotic Drugs in IPF: A Real-World Experience. Biomedicines 2022, 10, 3229. [Google Scholar] [CrossRef] [PubMed]
- Harari, S.; Pesci, A.; Albera, C.; Poletti, V.; Amici, C.; Crespi, G.; Campolo, B.; Vancheri, C.; FIBRONET study group. Nintedanib in IPF: Post hoc Analysis of the Italian FIBRONET Observational Study. Respiration 2022, 101, 577–584. [Google Scholar] [CrossRef]
- Majewski, S.; Białas, A.J.; Buchczyk, M.; Gomółka, P.; Górska, K.; Jagielska-Len, H.; Jarzemska, A.; Jassem, E.; Jastrzębski, D.; Kania, A.; et al. A multicentre retrospective observational study on Polish experience of pirfenidone therapy in patients with idiopathic pulmonary fibrosis: The PolExPIR study. BMC Pulm. Med. 2020, 20, 122. [Google Scholar] [CrossRef]
- Raghu, G.; Collard, H.R.; Egan, J.J.; Martinez, F.J.; Behr, J.; Brown, K.K.; Colby, T.V.; Cordier, J.-F.; Flaherty, K.R.; Lasky, J.A.; et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011, 183, 788–824. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Stanojevic, S.; Graham, B.L.; Cooper, B.G.; Thompson, B.R.; Carter, K.W.; Francis, R.W.; Hall, G.L. Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur. Respir. J. 2017, 50, 1700010. [Google Scholar] [CrossRef]
- Ley, B.; Ryerson, C.J.; Vittinghoff, E.; Ryu, J.H.; Tomassetti, S.; Lee, J.S.; Poletti, V.; Buccioli, M.; Elicker, B.M.; Jones, K.D.; et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann. Intern. Med. 2012, 156, 684–691. [Google Scholar] [CrossRef]
- Wollin, L.; Wex, E.; Pautsch, A.; Schnapp, G.; Hostettler, K.E.; Stowasser, S.; Kolb, M. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015, 45, 1434–1445. [Google Scholar] [CrossRef]
- Richeldi, L.; Costabel, U.; Selman, M.; Kim, D.S.; Hansell, D.M.; Nicholson, A.G.; Brown, K.K.; Flaherty, K.R.; Noble, P.W.; Raghu, G.; et al. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2011, 365, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Demosthenes, P. Real-world data: A brief review of the methods, applications, challenges and opportunities. BMC Med. Res. Methodol. 2022, 22, 287. [Google Scholar] [CrossRef] [PubMed]
- Grześk, G.; Woźniak-Wiśniewska, A.; Błażejewski, J.; Górny, B.; Wołowiec, Ł.; Rogowicz, D.; Nowaczyk, A. The Interactions of Nintedanib and Oral Anticoagulants—Molecular Mechanisms and Clinical Implications. Int. J. Mol. Sci. 2020, 22, 282. [Google Scholar] [CrossRef] [PubMed]
- Richeldi, L.; Cottin, V.; du Bois, R.M.; Selman, M.; Kimura, T.; Bailes, Z.; Schlenker-Herceg, R.; Stowasser, S.; Brown, K.K. Nintedanib in patients with idiopathic pulmonary fibrosis: Combined evidence from the TOMORROW and INPULSIS(®) trials. Respir. Med. 2016, 113, 74–79. [Google Scholar] [CrossRef]
- Kolonics-Farkas, A.M.; Šterclová, M.; Mogulkoc, N.; Kus, J.; Hájková, M.; Müller, V.; Jovanovic, D.; Tekavec-Trkanjec, J.; Littnerová, S.; Hejduk, K.; et al. Anticoagulant Use and Bleeding Risk in Central European Patients with Idiopathic Pulmonary Fibrosis (IPF) Treated with Antifibrotic Therapy: Real-World Data from EMPIRE. Drug Saf. 2020, 43, 971–980. [Google Scholar] [CrossRef]
- Kärkkäinen, M.; Nurmi, H.; Kettunen, H.-P.; Selander, T.; Purokivi, M.; Kaarteenaho, R. Underlying and immediate causes of death in patients with idiopathic pulmonary fibrosis. BMC Pulm. Med. 2018, 18, 69. [Google Scholar] [CrossRef]
- Myall, K.J.; Martinovic, J.L.; West, A. How COVID-19 interacts with interstitial lung disease. Breathe 2022, 18, 210158. [Google Scholar] [CrossRef]
- Cilli, A.; Hanta, I.; Uzer, F.; Coskun, F.; Sevinc, C.; Deniz, P.P.; Parlak, M.; Altunok, E.; Tertemiz, K.C.; Ursavas, A. Characteristics and outcomes of COVID-19 patients with IPF: A multi-center retrospective study. Respir. Med. Res. 2022, 81, 100900. [Google Scholar] [CrossRef]
- Swigris, J.J.; Wamboldt, F.S.; Behr, J.; du Bois, R.M.; King, T.E.; Raghu, G.; Brown, K.K. The 6 minute walk in idiopathic pulmonary fibrosis: Longitudinal changes and minimum important difference. Thorax 2010, 65, 173–177. [Google Scholar] [CrossRef]
- Holland, A.E.; Hill, C.J.; Dowman, L.; Glaspole, I.; Goh, N.; Lee, A.L.; McDonald, C.F. Short- and Long-Term Reliability of the 6-Minute Walk Test in People With Idiopathic Pulmonary Fibrosis. Respir. Care 2018, 63, 994–1001. [Google Scholar] [CrossRef]
- Nathan, S.D.; Yang, M.; Morgenthien, E.A.; Stauffer, J.L. FVC variability in patients with idiopathic pulmonary fibrosis and role of 6-min walk test to predict further change. Eur. Respir. J. 2020, 55, 1902151. [Google Scholar] [CrossRef]
- Bois, R.M.d.; Albera, C.; Bradford, W.Z.; Costabel, U.; Leff, J.A.; Noble, P.W.; Sahn, S.A.; Valeyre, D.; Weycker, D.; King, T.E. 6-minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2014, 43, 1421–1429. [Google Scholar] [CrossRef]
- Pesonen, I.; Gao, J.; Kalafatis, D.; Carlson, L.; Sköld, M.; Ferrara, G. Six-minute walking test outweighs other predictors of mortality in idiopathic pulmonary fibrosis. A real-life study from the Swedish IPF registry. Respir. Med. X 2020, 2, 100017. [Google Scholar] [CrossRef]
- Du Bois, R.M.; Weycker, D.; Albera, C.; Bradford, W.Z.; Costabel, U.; Kartashov, A.; Lancaster, L.; Noble, P.W.; Sahn, S.A.; Szwarcberg, J.; et al. Six-minute-walk test in idiopathic pulmonary fibrosis: Test validation and minimal clinically important difference. Am. J. Respir. Crit. Care Med. 2011, 183, 1231–1237. [Google Scholar] [CrossRef]
- Majewski, S.; Białas, A.J.; Barczyk, A.R.; Batura-Gabryel, H.; Buchczyk, M.; Doboszyńska, A.; Górska, K.; Grabowska-Szkudlarz, L.; Jagielska-Len, H.; Jarzemska, A.; et al. A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with IPF: The PolExNIB Study. In B22. Emerging Management of Fibrotic Ilds; American Thoracic Society International Conference Abstracts; American Thoracic Society: New York, NY, USA, 2022; p. A2428. [Google Scholar]





| Number of Patients, n (%) | 501 (100) |
|---|---|
| City of Bydgoszcz, n (%) | 26 (5.2) |
| City of Cracow (2 centers), n (%) | 57 (11.4) |
| City of Gdansk, n (%) | 36 (7.2) |
| City of Katowice, n (%) | 13 (2.6) |
| City of Lodz (2 centers), n (%) | 55 (11) |
| City of Lublin, n (%) | 22 (4.3) |
| City of Olsztyn, n (%) | 23 (4.6) |
| City of Poznan (2 centers), n (%) | 61 (12.2) |
| City of Szczecin, n (%) | 25 (5) |
| City of Warsaw (2 centers), n (%) | 114 (22.7) |
| City of Zabrze, n (%) | 49 (9.8) |
| City of Zielona Gora, n (%) | 20 (4) |
| Sex, male/female, n (%) | 349 (69.66)/152 (30.34) |
| Age (years), median (IQR) | 70.9 (65–75.7) |
| Smoking history | |
| Never smokers, n (%) | 134 (26.7) |
| Former smokers, n (%) | 326 (65.1) |
| Active smokers, n (%) | 41 (8.1) |
| Pack-years, median (IQR) | 28 (20–40) |
| Comorbidities | |
| Hypertension, n (%) | 313 (62.5) |
| Hyperlipidemia, n (%) | 186 (37.1) |
| Coronary artery disease, n (%) | 128 (25.5) |
| History of myocardial infarction, n (%) | 65 (13) |
| Atrial fibrillation, n (%) | 32 (6.4) |
| Heart failure, n (%) | 66 (13.2) |
| Pulmonary hypertension, n (%) | 60 (12) |
| Gastroesophageal reflux disease, n (%) | 134 (26.7) |
| Diabetes, n (%) | 134 (26.7) |
| Emphysema, n (%) | 106 (21.2) |
| Depression, n (%) | 52 (10.4) |
| Obstructive sleep apnea, n (%) | 32 (6.4) |
| Benign prostate hypertrophy, n (%) | 96 (19.2) |
| Neoplastic disease history, n (%) | 55 (11) |
| Osteoarthritis, n (%) | 149 (29.8) |
| Hypothyroidism, n (%) | 46 (9.2) |
| Concomitant medications | |
| Antihypertensive drugs, n (%) | 330 (65.9) |
| Acetylsalicylic acid monotherapy, n (%) | 160 (31.9) |
| Anticoagulants, n (%) | 34 (6.8) |
| Acetylsalicylic acid + anticoagulant therapy, n (%) | 9 (1.8) |
| Proton-pump inhibitors, n (%) | 163 (32.5) |
| Statins, n (%) | 205 (40.9) |
| Antidiabetic medications, n (%) | 116 (23.1) |
| HRCT pattern | |
| Radiologic UIP pattern, n (%) | 419 (83.6) |
| Radiologic probable UIP pattern (%) | 68 (13.6) |
| Radiologic inconsistent for UIP pattern, n (%) | 12 (2.4) |
| Lung biopsy procedures | |
| TBLC, n (%) | 18 (3.6) |
| SLB, n (%) | 38 (7.6) |
| BAL procedure, n (%) | 102 (20.7) |
| Time from first symptoms to diagnosis (months), median (IQR) | 12 (6–28) |
| Time from diagnosis to start of nintedanib therapy (months), median (IQR) | 3 (1–11) |
| Pulmonary function | |
| FVC (l), median (IQR) | 2.8 (2.3–3.5) |
| FVC (% of predicted), median (IQR) | 80.2 (68.5–95) |
| TLCO (mmol/min/kPa), median (IQR) | 4.1 (3.2–5.3) |
| TLCO (% of predicted), median (IQR) | 55.9 (42.2–69) |
| Blood oxygenation | |
| SpO2 at rest (%), median (IQR) | 94 (91–96) |
| 6MWT (n = 288) | |
| Distance (meters), mean (SD) | 436.8 (102.3) |
| Desaturation, (∆%), median (IQR) | 5 (2–8) |
| GAP score, median (IQR) | 3 (3–4) |
| GAP index | |
| Stage I, n (%) | 294 (58.9) |
| Stage II, n (%) | 178 (35.7) |
| Stage III, n (%) | 27 (5.4) |
| Oxygen therapy | |
| Home oxygen therapy, n (%) | 69 (13.8) |
| Portable sources of oxygen, n (%) | 26 (5.2) |
| IPF treatment in the past before initiation of nintedanib | |
| No treatment, n (%) | 377 (75.2) |
| Pirfenidone, n (%) | 88 (17.6) |
| CS, n (%) | 41 (8.2) |
| NAC, n (%) | 1 (0.2) |
| CS + NAC + AZA, n (%) | 4 (0.8) |
| Clinical trial, n (%) | 7 (1.4) |
| Full dose treatment 150 mg b.i.d., n (%) | 334 (66.7) |
| Reduced dose treatment 100 mg b.i.d., n (%) | 167 (33.3) |
| Intermittent drug interruption and/or dose reduction, n (%) | 101 (20.2) |
| ADRs | |
| Diarrhea, n (%) | 227 (45.3) |
| Nausea, n (%) | 104 (20.8) |
| Vomiting, n (%) | 41 (8.2) |
| Abdominal discomfort, n (%) | 148 (29.5) |
| Decreased appetite, n (%) | 150 (29.9) |
| Weight, n (%) | 161 (32.1) |
| Fatigue, n (%) | 96 (19.2) |
| Increased levels of AST/ALT, n (%) | 77 (15.4) |
| Hepatotoxicity AST/ALT > 3 ULN, n (%) | 31 (6.2) |
| Bleeding, n (%) | 20 (4) |
| Nintedanib exposure, (months), median (IQR) | 15 (7–25.5) |
| Reasons for treatment discontinuation | |
| ADRs, n (%) | 51 (10.2) |
| Disease progression, n (%) | 23 (4.6) |
| Death, n (%) | 58 (11.6) |
| Patient’s decision, n (%) | 33 (6.6) |
| Lung transplantation, n (%) | 2 (0.4) |
| Neoplastic disease, n (%) | 11 (2.2) |
| Other, n (%) | 25 (5) |
| 0–6 Months | 6–12 Months | 12–18 Months | 18–24 Months | 24–30 Months | 30–36 Months | |
|---|---|---|---|---|---|---|
| ∆FVC% | −0.96 (−4.94–3.51) | −0.8 (−4.9–2.84) | −0.7 (−5.24–2.89) | −0.9 (−4.8–2.99) | −2.05 (−5.37–1.68) | −1.22 (−5.86–2.86) |
| ∆TLCO% | −3.18 (−9.69–1.32) | −1.8 (−6.02–2.29) | −1.35 (−6.2–2.17) | −2.04 (−7.09–1.37) | −0.32 (−6.91–2.9) | −2.18 (−7.28–0.84) |
| p 6–12 vs. 0–6 | p 12–18 vs. 0–6 | p 18–24 vs. 0–6 | p 24–30 vs. 0–6 | p 30–36 vs. 0–6 | ||
| ∆FVC% | 0.33 | 0.18 | 0.25 | 0.07 | 0.7 | |
| ∆TLCO% | 0.24 | 0.18 | 0.83 | 0.11 | 0.89 |
| 0–6 Months | 6–12 Months | 12–18 Months | 18–24 Months | 24–30 Months | 30–36 Months | |
|---|---|---|---|---|---|---|
| ∆FVC% | ||||||
| Significant improvement (∆FVC > 10%), n (%) | 28 (8.3) | 19 (7.4) | 14 (7.2) | 6 (4.6) | 1 (1.5) | 0 (0) |
| Marginal improvement (10% ≥ ∆FVC > 5%), n (%) | 38 (11.3) | 25 (9.8) | 17 (8.7) | 14 (10.8) | 3 (4.5) | 1 (4.2) |
| Stabilization (+5% ≥ ∆FVC > −5%), n (%) | 191 (56.8) | 149 (58.2) | 113 (58.0) | 80 (62.0) | 45 (68.2) | 17 (70.8) |
| Marginal decline (−5% ≥ ∆FVC > −10%), n (%) | 48 (14.2) | 45 (17.6) | 35 (17.9) | 21 (16.3) | 14 (21.2) | 3 (12.5) |
| Significant decline (∆FVC ≤ −10%), n (%) | 31 (9.2) | 18 (7.0) | 16 (8.2) | 8 (6.2) | 3 (4.5) | 3 (12.5) |
| n | 336 | 256 | 195 | 129 | 66 | 24 |
| ∆TLCO% | ||||||
| Significant improvement (∆TLCO > 15%), n (%) | 17 (5.4) | 18 (7.6) | 12 (6.6) | 4 (3.2) | 1 (1.6) | 0 (0) |
| Stabilization (+15% ≥ ∆TLCO > −15%), n (%) | 250 (79.1) | 200 (84) | 160 (87.4) | 111 (90.2) | 59 (93.6) | 24 (96) |
| Significant decline (∆TLCO ≤ −15%), n (%) | 49 (15.5) | 20 (8.4) | 11 (6.0) | 8 (6.5) | 3 (4.8) | 1 (4) |
| n | 316 | 238 | 183 | 123 | 63 | 25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majewski, S.; Białas, A.J.; Barczyk, A.; Batura-Gabryel, H.; Buchczyk, M.; Doboszyńska, A.; Górska, K.; Grabowska-Skudlarz, L.; Jagielska-Len, H.; Jarzemska, A.; et al. A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with Idiopathic Pulmonary Fibrosis: The PolExNIB Study. J. Clin. Med. 2023, 12, 4635. https://doi.org/10.3390/jcm12144635
Majewski S, Białas AJ, Barczyk A, Batura-Gabryel H, Buchczyk M, Doboszyńska A, Górska K, Grabowska-Skudlarz L, Jagielska-Len H, Jarzemska A, et al. A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with Idiopathic Pulmonary Fibrosis: The PolExNIB Study. Journal of Clinical Medicine. 2023; 12(14):4635. https://doi.org/10.3390/jcm12144635
Chicago/Turabian StyleMajewski, Sebastian, Adam J. Białas, Adam Barczyk, Halina Batura-Gabryel, Małgorzata Buchczyk, Anna Doboszyńska, Katarzyna Górska, Luiza Grabowska-Skudlarz, Hanna Jagielska-Len, Agnieszka Jarzemska, and et al. 2023. "A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with Idiopathic Pulmonary Fibrosis: The PolExNIB Study" Journal of Clinical Medicine 12, no. 14: 4635. https://doi.org/10.3390/jcm12144635
APA StyleMajewski, S., Białas, A. J., Barczyk, A., Batura-Gabryel, H., Buchczyk, M., Doboszyńska, A., Górska, K., Grabowska-Skudlarz, L., Jagielska-Len, H., Jarzemska, A., Jassem, E., Jastrzębski, D., Kania, A., Koprowski, M., Krawczyk, M., Krenke, R., Lewandowska, K., Mackiewicz, B., Martusewicz-Boros, M. M., ... Piotrowski, W. J. (2023). A Real-World Multicenter Retrospective Observational Study on Polish Experience with Nintedanib Therapy in Patients with Idiopathic Pulmonary Fibrosis: The PolExNIB Study. Journal of Clinical Medicine, 12(14), 4635. https://doi.org/10.3390/jcm12144635











