Personality Traits and Fatigue in Multiple Sclerosis: A Narrative Review
Abstract
1. Introduction
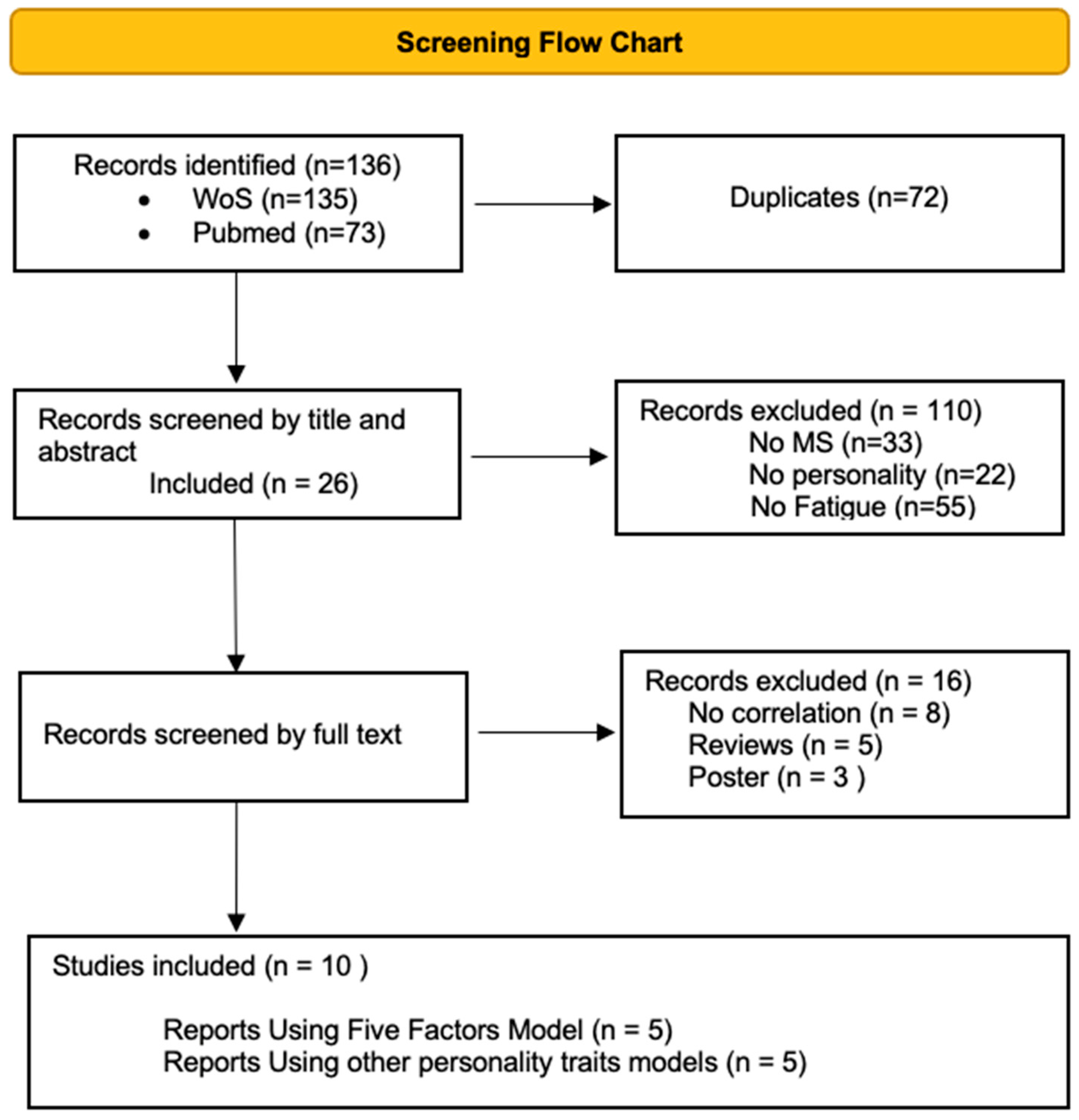
2. Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McGinley, M.P.; Goldschmidt, C.H.; Rae-Grant, A.D. Diagnosis and Treatment of Multiple Sclerosis: A Review. JAMA 2021, 325, 765–779. [Google Scholar] [CrossRef]
- D’Amico, E.; Patti, F.; Zanghì, A.; Chisari, C.G.; Fermo, S.L.; Zappia, M. Late-onset and young-onset relapsing-remitting multiple sclerosis: Evidence from a retrospective long-term follow-up study. Eur. J. Neurol. 2018, 25, 1425–1431. [Google Scholar] [CrossRef]
- Naseri, A.; Nasiri, E.; Sahraian, M.A.; Daneshvar, S.; Talebi, M. Clinical Features of Late-Onset Multiple Sclerosis: A Systematic Review and Meta-analysis. Mult. Scler. Relat. Disord. 2021, 50, 102816. [Google Scholar] [CrossRef]
- Zanghì, A.; Avolio, C.; Amato, M.P.; Filippi, M.; Trojano, M.; Patti, F.; D’amico, E.; Register, F.T.I.M. First-line therapies in late-onset multiple sclerosis: An Italian registry study. Eur. J. Neurol. 2021, 28, 4117–4123. [Google Scholar] [CrossRef] [PubMed]
- Zanghì, A.; D’amico, E.; Fermo, S.L.; Patti, F. Exploring polypharmacy phenomenon in newly diagnosed relapsing–remitting multiple sclerosis: A cohort ambispective single-centre study. Ther. Adv. Chronic Dis. 2021, 12, 2040622320983121. [Google Scholar] [CrossRef] [PubMed]
- Mirmosayyeb, O.; Brand, S.; Barzegar, M.; Afshari-Safavi, A.; Nehzat, N.; Shaygannejad, V.; Bahmani, D.S. Clinical Characteristics and Disability Progression of Early- and Late-Onset Multiple Sclerosis Compared to Adult-Onset Multiple Sclerosis. J. Clin. Med. 2020, 9, 1326. [Google Scholar] [CrossRef] [PubMed]
- Solaro, C.; Trabucco, E.; Uccelli, M.M. Pain and Multiple Sclerosis: Pathophysiology and Treatment. Curr. Neurol. Neurosci. Rep. 2012, 13, 320. [Google Scholar] [CrossRef] [PubMed]
- D’amico, E.; Zanghì, A.; Serra, A.; Murabito, P.; Zappia, M.; Patti, F.; Cocuzza, S. Management of dysphagia in multiple sclerosis: Current best practice. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Zanghì, A.; Cimino, S.; Urzì, D.; Privitera, S.; Zagari, F.; Lanza, G.; Patti, F.; D’amico, E. Pharmacotherapeutic management of lower urinary tract symptoms in Multiple Sclerosis patients. Expert Opin. Pharmacother. 2020, 21, 1449–1454. [Google Scholar] [CrossRef]
- Lakin, L.; Davis, B.E.; Binns, C.C.; Currie, K.M.; Rensel, M.R. Comprehensive Approach to Management of Multiple Sclerosis: Addressing Invisible Symptoms—A Narrative Review. Neurol. Ther. 2021, 10, 75–98. [Google Scholar] [CrossRef] [PubMed]
- Racke, M.K.; Frohman, E.M.; Frohman, T. Pain in Multiple Sclerosis: Understanding Pathophysiology, Diagnosis, and Management through Clinical Vignettes. Front. Neurol. 2022, 12, 799698. [Google Scholar] [CrossRef] [PubMed]
- Nazari, F.; Shaygannejad, V.; Sichani, M.M.; Mansourian, M.; Hajhashemi, V. Sexual dysfunction in women with multiple sclerosis: Prevalence and impact on quality of life. BMC Urol. 2020, 20, 15. [Google Scholar] [CrossRef] [PubMed]
- Lorefice, L.; Fenu, G.; Frau, J.; Coghe, G.; Marrosu, M.G.; Cocco, E. The burden of multiple sclerosis and patients’ coping strategies. BMJ Support. Palliat. Care 2018, 8, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Zanghì, A.; D’Amico, E.; Luca, M.; Ciaorella, M.; Basile, L.; Patti, F. Mental health status of relapsing-remitting multiple sclerosis Italian patients returning to work soon after the easing of lockdown during COVID-19 pandemic: A monocentric experience. Mult. Scler. Relat. Disord. 2020, 46, 102561. [Google Scholar] [CrossRef]
- D’Amico, E.; Chisari, C.G.; Arena, S.; Zanghì, A.; Toscano, S.; Fermo, S.L.; Maimone, D.; Castaing, M.; Sciacca, S.; Zappia, M.; et al. Cancer Risk and Multiple Sclerosis: Evidence from a Large Italian Cohort. Front. Neurol. 2019, 10, 337. [Google Scholar] [CrossRef]
- D’amico, E.; Zanghì, A.; Leone, C.; Tumani, H.; Patti, F. Treatment-Related Progressive Multifocal Leukoencephalopathy in Multiple Sclerosis: A Comprehensive Review of Current Evidence and Future Needs. Drug Saf. 2016, 39, 1163–1174. [Google Scholar] [CrossRef] [PubMed]
- Soelberg Sorensen, P. Safety concerns and risk management of multiple sclerosis therapies. Acta Neurol. Scand. 2017, 136, 168–186. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, E.; Zhu, C.; Wei, R.; Ma, L.; Dong, X.; Li, R.; Sun, F.; Zhou, Y.; Cui, Y.; et al. Comparative efficacy and safety of disease-modifying therapies in patients with relapsing multiple sclerosis: A systematic review and network meta-analysis. J. Am. Pharm. Assoc. 2023, 63, 8–22.e23. [Google Scholar] [CrossRef]
- D’amico, E.; Leone, C.; Zanghì, A.; Fermo, S.L.; Patti, F. Lateral and escalation therapy in relapsing-remitting multiple sclerosis: A comparative study. J. Neurol. 2016, 263, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, E.; Zanghì, A.; Gastaldi, M.; Patti, F.; Zappia, M.; Franciotta, D. Placing CD20-targeted B cell depletion in multiple sclerosis therapeutic scenario: Present and future perspectives. Autoimmun. Rev. 2019, 18, 665–672. [Google Scholar] [CrossRef] [PubMed]
- D’amico, E.; Zanghì, A.; Sciandra, M.; Borriello, G.; Callari, G.; Gallo, A.; Salemi, G.; Cottone, S.; Buccafusca, M.; Valentino, P.; et al. Discontinuation of teriflunomide and dimethyl fumarate in a large Italian multicentre population: A 24-month real-world experience. J. Neurol. 2019, 266, 411–416. [Google Scholar] [CrossRef] [PubMed]
- D’amico, E.; Zanghì, A.; Sciandra, M.; Lanzillo, R.; Callari, G.; Cortese, A.; Lus, G.; Lucchini, M.; Buccafusca, M.; Bonavita, S.; et al. Dimethyl fumarate vs. Teriflunomide: An Italian time-to-event data analysis. J. Neurol. 2020, 267, 3008–3020. [Google Scholar] [CrossRef]
- Zanghì, A.; Gallo, A.; Avolio, C.; Capuano, R.; Lucchini, M.; Petracca, M.; Bonavita, S.; Lanzillo, R.; Ferraro, D.; Curti, E.; et al. Exit Strategies in Natalizumab-Treated RRMS at High Risk of Progressive Multifocal Leukoencephalopathy: A Multicentre Comparison Study. Neurotherapeutics 2021, 18, 1166–1174. [Google Scholar] [CrossRef]
- D’amico, E.; Zanghì, A.; Callari, G.; Borriello, G.; Gallo, A.; Graziano, G.; Valentino, P.; Buccafusca, M.; Cottone, S.; Salemi, G.; et al. Comparable efficacy and safety of dimethyl fumarate and teriflunomide treatment in Relapsing-Remitting Multiple Sclerosis: An Italian real-word multicenter experience. Ther. Adv. Neurol. Disord. 2018, 11, 1756286418796404. [Google Scholar] [CrossRef]
- Manjunatha, R.T.; Habib, S.; Sangaraju, S.L.; Yepez, D.; Grandes, X.A. Multiple Sclerosis: Therapeutic Strategies on the Horizon. Cureus 2022, 14, e24895. [Google Scholar] [CrossRef] [PubMed]
- D’amico, E.; Zanghì, A.; Manuti, V.; Allegretta, C.; Amoruso, A.; Serviddio, G.; Avolio, C. MicroRNAs 181a and 125a are highly expressed in naïve RRMS: A pilot case–control study. J. Neurol. 2023, 270, 1150–1153. [Google Scholar] [CrossRef] [PubMed]
- D’amico, E.; Zanghì, A.; Parrinello, N.L.; Romano, A.; Palumbo, G.A.; Chisari, C.G.; Toscano, S.; Di Raimondo, F.; Zappia, M.; Patti, F. Immunological Subsets Characterization in Newly Diagnosed Relapsing–Remitting Multiple Sclerosis. Front. Immunol. 2022, 13, 819136. [Google Scholar] [CrossRef]
- Paul, A.; Comabella, M.; Gandhi, R. Biomarkers in Multiple Sclerosis. Cold Spring Harb. Perspect. Med. 2019, 9, a029058. [Google Scholar] [CrossRef]
- Yang, J.; Hamade, M.; Wu, Q.; Wang, Q.; Axtell, R.; Giri, S.; Mao-Draayer, Y. Current and Future Biomarkers in Multiple Sclerosis. Int. J. Mol. Sci. 2022, 23, 5877. [Google Scholar] [CrossRef]
- Bol, Y.; Duits, A.A.; Hupperts, R.M.; Vlaeyen, J.W.; Verhey, F.R. The psychology of fatigue in patients with multiple sclerosis: A review. J. Psychosom. Res. 2009, 66, 3–11. [Google Scholar] [CrossRef]
- Plow, M.; Gunzler, D.D.; Chang, J.H.C. Characterizing fatigue phenotypes with other symptoms and clinically relevant outcomes among people with multiple sclerosis. Qual. Life Res. 2023, 32, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Manjaly, Z.-M.; Harrison, N.A.; Critchley, H.D.; Do, C.T.; Stefanics, G.; Wenderoth, N.; Lutterotti, A.; Müller, A.; Stephan, K.E. Pathophysiological and cognitive mechanisms of fatigue in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2019, 90, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Rooney, S.; Wood, L.; Moffat, F.; Paul, L. Prevalence of fatigue and its association with clinical features in progressive and non-progressive forms of Multiple Sclerosis. Mult. Scler. Relat. Disord. 2019, 28, 276–282. [Google Scholar] [CrossRef]
- Wan, J.-J.; Qin, Z.; Wang, P.-Y.; Sun, Y.; Liu, X. Muscle fatigue: General understanding and treatment. Exp. Mol. Med. 2017, 49, e384. [Google Scholar] [CrossRef]
- Flachenecker, P. Definitions, Epidemiology, and Etiological Factors. In Fatigue in Multiple Sclerosis: Background, Clinic, Diagnostic, Therapy; Penner, I.-K., Ed.; Springer International Publishing: Cham, Swizerland, 2023; pp. 9–26. [Google Scholar]
- Gümüş, H. Fatigue Can Be Objectively Measured in Multiple Sclerosis: Multipl Sklerozda Yorgunluk Objektif Olarak Ölçülebilir. Noro Psikiyatr Ars. 2018, 55 (Suppl. 1), S76–S79. [Google Scholar] [PubMed]
- Colosimo, C.; Millefiorini, E.; Grasso, M.G.; Vinci, F.; Fiorelli, M.; Koudriavtseva, T.; Pozzilli, C. Fatigue in MS is associated with specific clinical features. Acta Neurol. Scand. 1995, 92, 353–355. [Google Scholar] [CrossRef]
- von Bismarck, O.; Dankowski, T.; Ambrosius, B.; Hessler, N.; Antony, G.; Ziegler, A.; Hoshi, M.-M.; Aly, L.; Luessi, F.; Groppa, S.; et al. Treatment choices and neuropsychological symptoms of a large cohort of early MS. Neurol.-Neuroimmunol. Neuroinflamm. 2018, 5, e446. [Google Scholar] [CrossRef]
- Flachenecker, P.; Müller, G.; König, H.; Meissner, H.; Toyka, K.V.; Rieckmann, P. [“Fatigue” in multiple sclerosis. Development and and validation of the “Würzburger Fatigue Inventory for MS”]. Nervenarzt 2006, 77, 165–166, 168–170, 172–174. [Google Scholar] [CrossRef]
- Braley, T.J.; Chervin, R.D. Fatigue in Multiple Sclerosis: Mechanisms, Evaluation, and Treatment. Sleep 2010, 33, 1061–1067. [Google Scholar] [CrossRef]
- Angioni, D.; Giudici, K.V.; Martinez, M.M.; Rolland, Y.; Vellas, B.; Barreto, P.D.S. Neuroimaging markers of chronic fatigue in older people: A narrative review. Aging Clin. Exp. Res. 2021, 33, 1487–1492. [Google Scholar] [CrossRef]
- Schreiber, H.; Lang, M.; Kiltz, K.; Lang, C. Is personality profile a relevant determinant of fatigue in multiple sclerosis? Front Neurol. 2015, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Ellison, P.M.; Goodall, S.; Kennedy, N.; Dawes, H.; Clark, A.; Pomeroy, V.; Duddy, M.; Baker, M.R.; Saxton, J.M. Neurostructural and Neurophysiological Correlates of Multiple Sclerosis Physical Fatigue: Systematic Review and Meta-Analysis of Cross-Sectional Studies. Neuropsychol. Rev. 2022, 32, 506–519. [Google Scholar] [CrossRef]
- AlSaeed, S.; Aljouee, T.; Alkhawajah, N.M.; Alarieh, R.; AlGarni, H.; Aljarallah, S.; Ayyash, M.; Abu-Shaheen, A. Fatigue, Depression, and Anxiety Among Ambulating Multiple Sclerosis Patients. Front. Immunol. 2022, 13, 844461. [Google Scholar] [CrossRef]
- Ayache, S.S.; Chalah, M.A. Fatigue in multiple sclerosis–Insights into evaluation and management. Neurophysiol. Clin. 2017, 47, 139–171. [Google Scholar] [CrossRef] [PubMed]
- Dean, J.; Keshavan, M. The neurobiology of depression: An integrated view. Asian J. Psychiatry 2017, 27, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-H.; Giuliani, F. The Role of Inflammation in Depression and Fatigue. Front. Immunol. 2019, 10, 1696. [Google Scholar] [CrossRef]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Concerto, C.; Rodolico, A.; Ciancio, A.; Messina, C.; Natale, A.; Mineo, L.; Battaglia, F.; Aguglia, E. Vitamin D and Depressive Symptoms in Adults with Multiple Sclerosis: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 19, 199. [Google Scholar] [CrossRef]
- Putzki, N.; Katsarava, Z.; Vago, S.; Diener, H.; Limmroth, V. Prevalence and Severity of Multiple-Sclerosis-Associated Fatigue in Treated and Untreated Patients. Eur. Neurol. 2008, 59, 136–142. [Google Scholar] [CrossRef]
- Kappos, L.; Fox, R.J.; Burcklen, M.; Freedman, M.S.; Havrdová, E.K.; Hennessy, B.; Hohlfeld, R.; Lublin, F.; Montalban, X.; Pozzilli, C.; et al. Ponesimod Compared with Teriflunomide in Patients with Relapsing Multiple Sclerosis in the Active-Comparator Phase 3 OPTIMUM Study: A Randomized Clinical Trial. JAMA Neurol. 2021, 78, 558–567. [Google Scholar] [CrossRef]
- Nourbakhsh, B.; Waubant, E.; Evers, A.W.M.; Solomon, A.J. Ethical considerations in the treatment of multiple sclerosis fatigue. Mult. Scler. Relat. Disord. 2021, 54, 103129. [Google Scholar] [CrossRef]
- Nourbakhsh, B.; Revirajan, N.; Morris, B.; Cordano, C.; Creasman, J.; Manguinao, M.; Krysko, K.; Rutatangwa, A.; Auvray, C.; Aljarallah, S.; et al. Safety and efficacy of amantadine, modafinil, and methylphenidate for fatigue in multiple sclerosis: A randomised, placebo-controlled, crossover, double-blind trial. Lancet Neurol. 2021, 20, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.N.; Howard, C.A.; Kemp, D.W. Modafinil for the Treatment of Multiple Sclerosis-Related Fatigue. Ann. Pharmacother. 2010, 44, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Cocco, E.; Fadda, P. Treatment of multiple sclerosis fatigue with the synthetic psychoactive drug modafinil. Exp. Neurol. 2022, 347, 113906. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.; Priore, R.L.; Miller, C.; Munschauer, F.; Jacobs, L. Personality disorder in multiple sclerosis correlates with cognitive impairment. J. Neuropsychiatry Clin. Neurosci. 2001, 13, 70–76. [Google Scholar] [CrossRef]
- Uca, A.U.; Uguz, F.; Kozak, H.H.; Turgut, K.; Tekin, G.; Altas, M.; Akpinar, Z. Personality disorders in pateints with multiple sclerosis: Prevalence and association with depressive and anxiety disorders and clinical features. Neurol. Asia 2016, 21, 55–61. [Google Scholar]
- McKay, K.A.; Tremlett, H.; Fisk, J.D.; Zhang, T.; Patten, S.B.; Kastrukoff, L.; Campbell, T.; Marrie, R.A.; For the CIHR Team in the Epidemiology and Impact of Comorbidity on Multiple Sclerosis. Psychiatric comorbidity is associated with disability progression in multiple sclerosis. Neurology 2018, 90, e1316–e1323. [Google Scholar] [CrossRef]
- Bruce, J.M.; Lynch, S.G. Personality traits in multiple sclerosis: Association with mood and anxiety disorders. J. Psychosom. Res. 2011, 70, 479–485. [Google Scholar] [CrossRef]
- Afshar, H.; Roohafza, H.R.; Keshteli, A.H.; Mazaheri, M.; Feizi, A.; Adibi, P. The association of personality traits and coping styles according to stress level. J. Res. Med. Sci. 2015, 20, 353–358. [Google Scholar]
- O’Brien, T.B.; DeLongis, A. The interactional context of problem-, emotion-, and relationship-focused coping: The role of the big five personality factors. J. Pers. 1996, 64, 775–813. [Google Scholar] [CrossRef]
- Mroczek, D.K.; Almeida, D.M. The Effect of Daily Stress, Personality, and Age on Daily Negative Affect. J. Pers. 2004, 72, 355–378. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Zonderman, A.B.; Ferrucci, L.; Terracciano, A. Personality Traits and Chronic Disease: Implications for Adult Personality Development. Journals Gerontol. Ser. B 2013, 68, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Concerto, C.; Rodolico, A.; Avanzato, C.; Fusar-Poli, L.; Signorelli, M.S.; Battaglia, F.; Aguglia, E. Autistic Traits and Attention-Deficit Hyperactivity Disorder Symptoms Predict the Severity of Internet Gaming Disorder in an Italian Adult Population. Brain Sci. 2021, 11, 774. [Google Scholar] [CrossRef]
- Smirni, D.; Smirni, P.; Lavanco, G.; Caci, B. Premorbid Personality Traits as Risk Factors for Behavioral Addictions: A Systematic Review of a Vulnerability Hypothesis. Children 2023, 10, 467. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Hampson, S.E. Personality Processes: Mechanisms by Which Personality Traits “Get Outside the Skin”. Annu. Rev. Psychol. 2012, 63, 315–339. [Google Scholar] [CrossRef] [PubMed]
- Matthews, G. Traits, cognitive processes and adaptation: An elegy for Hans Eysenck’s personality theory. Personal. Individ. Differ. 2016, 103, 61–67. [Google Scholar] [CrossRef]
- Eysenck, H.J. A reply to Costa and McCrae. P or A and C—The role of theory. Personal. Individ. Differ. 1992, 13, 867–868. [Google Scholar] [CrossRef]
- Davis, R.D. Millon: Essentials of his science, theory, classification, assessment, and therapy. J. Personal. Assess. 1999, 72, 330–352. [Google Scholar] [CrossRef]
- Strack, S. Introduction. J. Personal. Assess. 1999, 72, 323–329. [Google Scholar] [CrossRef]
- Bajraktarov, S.; Gudeva-Nikovska, D.; Manuå¡Eva, N.; Arsova, S. Personality Characteristics as Predictive Factors for the Occurrence of Depressive Disorder. Open Access Maced. J. Med. Sci. 2017, 5, 48–53. [Google Scholar] [CrossRef]
- McCrae, R.R.; John, O.P. An Introduction to the Five-Factor Model and Its Applications. J. Pers. 1992, 60, 175–215. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Cuzzola, M.F.; Latella, D.; Impellizzeri, F.; Todaro, A.; Rao, G.; Manuli, A.; Calabrò, R.S. How personality traits affect functional outcomes in patients with multiple sclerosis: A scoping review on a poorly understood topic. Mult. Scler. Relat. Disord. 2020, 46, 102560. [Google Scholar] [CrossRef]
- Kendler, K.S.; Kuhn, J.; Prescott, C.A. The Interrelationship of Neuroticism, Sex, and Stressful Life Events in the Prediction of Episodes of Major Depression. Am. J. Psychiatry 2004, 161, 631–636. [Google Scholar] [CrossRef]
- Kever, A.; Walker, E.L.; Riley, C.S.; Heyman, R.A.; Xia, Z.; Leavitt, V.M. Association of personality traits with physical function, cognition, and mood in multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 59, 103648. [Google Scholar] [CrossRef] [PubMed]
- Besharat, M.A.; Pourhosein, R.; Rostami, R.; Bazzazian, S. Perfectionism and fatigue in multiple sclerosis. Psychol. Health 2011, 26, 419–432. [Google Scholar] [CrossRef]
- Fernández-Muñoz, J.J.; Morón-Verdasco, A.; Cigarán-Méndez, M.; Muñoz-Hellín, E.; Pérez-De-Heredia-Torres, M.; Fernández-De-Las-Peñas, C. Disability, quality of life, personality, cognitive and psychological variables associated with fatigue in patients with multiple sclerosis. Acta Neurol. Scand. 2015, 132, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Incerti, C.C.; Argento, O.; Pisani, V.; Mannu, R.; Magistrale, G.; Di Battista, G.; Caltagirone, C.; Nocentini, U. A Preliminary Investigation of Abnormal Personality Traits in MS Using the MCMI-III. Appl. Neuropsychol. Adult 2015, 22, 452–458. [Google Scholar] [CrossRef]
- Matesic, I.; Marcinko, I. Identifying the relevant determinants of MS related fatigue: The role of the clinical indicators of disease and personality. Mult. Scler. Relat. Disord. 2020, 42, 102054. [Google Scholar] [CrossRef]
- Merkelbach, S.; König, J.; Sittinger, H. Personality traits in multiple sclerosis (MS) patients with and without fatigue experience. Acta Neurol. Scand. 2003, 107, 195–201. [Google Scholar] [CrossRef]
- Penner, I.-K.; Bechtel, N.; Raselli, C.; Stöcklin, M.; Opwis, K.; Kappos, L.; Calabrese, P. Fatigue in multiple sclerosis: Relation to depression, physical impairment, personality and action control. Mult. Scler. J. 2007, 13, 1161–1167. [Google Scholar] [CrossRef]
- Sindermann, C.; Saliger, J.; Nielsen, J.; Karbe, H.; Markett, S.; Stavrou, M.; Montag, C. Personality and Primary Emotional Traits: Disentangling Multiple Sclerosis Related Fatigue and Depression. Arch. Clin. Neuropsychol. 2018, 33, 552–561. [Google Scholar] [CrossRef]
- Spiegelberg, N.; Breuer, S.; Nielsen, J.; Saliger, J.; Montag, C.; Karbe, H.; Markett, S. Cognitive Fatigue Predicts Cognitive Failure in Multiple Sclerosis Patients and Healthy Controls: A Case-Control Study. Arch. Clin. Neuropsychol. 2021, 36, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Strober, L.B. Personality in multiple sclerosis (MS): Impact on health, psychological well-being, coping, and overall quality of life. Psychol. Health Med. 2017, 22, 152–161. [Google Scholar] [CrossRef]
- van der Werf, S.P.; Evers, A.; Jongen, P.J.; Bleijenberg, G. The role of helplessness as mediator between neurological disability, emotional instability, experienced fatigue and depression in patients with multiple sclerosis. Mult. Scler. J. 2003, 9, 89–94. [Google Scholar] [CrossRef]
- Fisk, J.D.; Ritvo, P.G.; Ross, L.; Haase, D.A.; Marrie, T.J.; Schlech, W.F. Measuring the functional impact of fatigue: Initial validation of the Fatigue Impact Scale. Clin. Infect. Dis. 1994, 18 (Suppl. 1), S79–S83. [Google Scholar] [CrossRef]
- Téllez, N.; Río, J.; Tintoré, M.; Nos, C.; Galán, I.; Montalban, X. Does the Modified Fatigue Impact Scale offer a more comprehensive assessment of fatigue in MS? Mult. Scler. 2005, 11, 198–202. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Wessely, S.; Powell, R. Fatigue syndromes: A comparison of chronic “postviral” fatigue with neuromuscular and affective disorders. J. Neurol. Neurosurg. Psychiatry 1989, 52, 940–948. [Google Scholar] [CrossRef] [PubMed]
- Beurskens, A.J.; Bültmann, U.; Kant, I.; Vercoulen, J.H.; Bleijenberg, G.; Swaen, G.M. Fatigue among working people: Validity of a questionnaire measure. Occup. Environ. Med. 2000, 57, 353–357. [Google Scholar] [CrossRef]
- Penner, I.; Raselli, C.; Stöcklin, M.; Opwis, K.; Kappos, L.; Calabrese, P. The Fatigue Scale for Motor and Cognitive Functions (FSMC): Validation of a new instrument to assess multiple sclerosis-related fatigue. Mult. Scler. J. 2009, 15, 1509–1517. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.; McCrae, R. Normal Personality Assessment in Clinical Practice: The NEO Personality Inventory. Psychol. Assess. 1992, 4, 5–13. [Google Scholar] [CrossRef]
- Caruso, J.C. Reliability Generalization of the Neo Personality Scales. Educ. Psychol. Meas. 2000, 60, 236–254. [Google Scholar] [CrossRef]
- Costa, P.T., Jr.; McCrae, R.R. The SAGE Handbook of Personality Theory and Assessment: Volume 2—Personality Measurement and Testing; SAGE Publications Ltd.: London, UK, 2008; Available online: https://sk.sagepub.com/reference/hdbk_personalitytheory2 (accessed on 16 April 2023).
- Goldberg, L.R.; Johnson, J.A.; Eber, H.W.; Hogan, R.; Ashton, M.C.; Cloninger, C.R.; Gough, H.G. The international personality item pool and the future of public-domain personality measures. J. Res. Pers. 2006, 40, 84–96. [Google Scholar] [CrossRef]
- Denollet, J. DS14: Standard Assessment of Negative Affectivity, Social Inhibition, and Type D Personality. Psychosom. Med. 2005, 67, 89–97. [Google Scholar] [CrossRef]
- Frost, R.O.; Marten, P.; Lahart, C.; Rosenblate, R. The dimensions of perfectionism. Cogn. Ther. Res. 1990, 14, 449–468. [Google Scholar] [CrossRef]
- Terry-Short, L.A.; Owens, G.; Slade, P.; Dewey, M.E. Positive and negative perfectionism. Personal. Individ. Differ. 1995, 18, 663–668. [Google Scholar] [CrossRef]
- Millon, T.; Davis, R.D. The MCMI–III: Present and future directions. J. Pers. Assess. 1997, 68, 69–85. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R.; Svrakic, D.M.; Przybeck, T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 975–990. [Google Scholar] [CrossRef]
- Cloninger, C.R.; Svrakic, D.M.; Bayon, C.; Przybeck, T.R. Measurement of Psychopathology as Variants of Personality; American Psychiatric Association: Washington, DC, USA, 1999. [Google Scholar]
- Fahrenberg, J.; Hampel, R.; Selg, H. Das Freiburger Persönlichkeitsinventar: FPI; Revidierte Fassung FPI-R und Teilweise Geänderte Fassung FPI-A1; Handanweisung; Verlag für Psychologie Hogrefe: Göttingen, Germany, 1989. [Google Scholar]
- Eysenck, H.J. Dimensions of personality: 16, 5 or 3?—Criteria for a taxonomic paradigm. Personal. Individ. Differ. 1991, 12, 773–790. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T. Adding Liebe und Arbeit: The Full Five-Factor Model and Well-Being. Pers. Soc. Psychol. Bull. 1991, 17, 227–232. [Google Scholar] [CrossRef]
- Miller, J.D.; Lynam, D.R.; Vize, C.; Crowe, M.; Sleep, C.; Maples-Keller, J.L.; Few, L.R.; Campbell, W.K. Vulnerable Narcissism Is (Mostly) a Disorder of Neuroticism. J. Pers. 2018, 86, 186–199. [Google Scholar] [CrossRef] [PubMed]
- Allroggen, M.; Rehmann, P.; Schürch, E.; Morf, C.C.; Kölch, M. The Relationship between Narcissism and Personality Traits of the Five-Factor-Model in Adolescents and Young Adults. Z. Kinder Jugendpsychiatrie Psychother. 2018, 46, 516–522. [Google Scholar] [CrossRef]
- Mols, F.; Denollet, J. Type D personality in the general population: A systematic review of health status, mechanisms of disease, and work-related problems. Health Qual. Life Outcomes 2010, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Boyle, L.L.M.D.; Lyness, J.M.M.D.; Duberstein, P.R.P.; Karuza, J.P.; King, D.A.P.; Messing, S.M.S.; Tu, X. Trait Neuroticism, Depression, and Cognitive Function in Older Primary Care Patients. Am. J. Geriatr. Psychiatry 2010, 18, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Weger, M.; Sandi, C. High anxiety trait: A vulnerable phenotype for stress-induced depression. Neurosci. Biobehav. Rev. 2018, 87, 27–37. [Google Scholar] [CrossRef]
- Estrada-López, M.; Reguera-García, M.M.; Rivera, F.J.P.; Molina, A.J. Physical disability and personality traits in multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 37, 101465. [Google Scholar] [CrossRef]
- Tarasiuk, J.; Kapica-Topczewska, K.; Czarnowska, A.; Chorąży, M.; Kochanowicz, J.; Kułakowska, A. Co-occurrence of Fatigue and Depression in People with Multiple Sclerosis: A Mini-Review. Front. Neurol. 2021, 12, 817256. [Google Scholar] [CrossRef]
- Otte, C.; Gold, S.M.; Penninx, B.W.; Pariante, C.M.; Etkin, A.; Fava, M.; Mohr, D.C.; Schatzberg, A.F. Major depressive disorder. Nat. Rev. Dis. Prim. 2016, 2, 16065. [Google Scholar] [CrossRef]
- Baquero, M.; Martín, N. Depressive symptoms in neurodegenerative diseases. World J. Clin. Cases 2015, 3, 682–693. [Google Scholar] [CrossRef]
- Thielscher, C.; Thielscher, S.; Kostev, K. The risk of developing depression when suffering from neurological diseases. Ger. Med. Sci. 2013, 11, Doc02. [Google Scholar] [CrossRef]
- Flachenecker, P.; Kümpfel, T.; Kallmann, B.; Gottschalk, M.; Grauer, O.; Rieckmann, P.; Trenkwalder, C.; Toyka, K.V. Fatigue in multiple sclerosis: A comparison of different rating scales and correlation to clinical parameters. Mult. Scler. J. 2002, 8, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, M.; Kuhlman, D.M.; Joireman, J.; Teta, P.; Kraft, M. A comparison of three structural models for personality: The big three, the big five, and the alternative five. J. Personal. Soc. Psychol. 1993, 65, 757. [Google Scholar] [CrossRef]
- Di Fabio, A.; Smith, M.M.; Saklofske, D.H. Perfectionism and a Healthy Attitude toward Oneself: Could Humor Be a Resource? Int. J. Environ. Res. Public Health 2019, 17, 201. [Google Scholar] [CrossRef]
- Mofield, E.; Peters, M.P.; Chakraborti-Ghosh, S. Perfectionism, Coping, and Underachievement in Gifted Adolescents: Avoidance vs. Approach Orientations. Educ. Sci. 2016, 6, 21. [Google Scholar] [CrossRef]
- Slade, P.; Owens, G. A Dual Process Model of Perfectionism Based on Reinforcement Theory. Behav. Modif. 1998, 22, 372–390. [Google Scholar] [CrossRef]
- Smith, M.M.; Arnett, P.A. Perfectionism and physical disability predict depression in multiple sclerosis. J. Psychosom. Res. 2013, 75, 187–189. [Google Scholar] [CrossRef]
- Stephan, Y.; Sutin, A.R.; Luchetti, M.; Canada, B.; Terracciano, A. Personality and fatigue: Meta-analysis of seven prospective studies. Sci. Rep. 2022, 12, 9156. [Google Scholar] [CrossRef]
- Henriques-Calado, J.; Duarte-Silva, M.E.; Keong, A.; Sacoto, C.; Junqueira, D. Personality Traits and Personality Disorders in Older Women: An Explorative Study between Normal Development and Psychopathology. Health Care Women Int. 2014, 35, 1303–1314. [Google Scholar] [CrossRef]
- Delva, M.; Delva, I.; Pinchuk, V.; Kryvchun, A.; Purdenko, T. Prevalence and predictors of fatigue in patients with episodic migraine. Wiadomości Lek. 2022, 75 Pt 2, 1970–1974. [Google Scholar] [CrossRef]
| Personality Trait Assessment | Fatigue Assessment | Other Assessments | Results | |
|---|---|---|---|---|
| Five-Factor Model | ||||
| Penner (2007) [82] Switzerland Cross-sectional study Participants: 41 Mean Age (SD): 41.80 (10.95) Female/Male: 24/17 MS Diagnosis: McDonald’s criteria Clinical status: 68.3% of patients have RR MS, 7.3% PP MS, 24.4% SP MS EDSS mean (SD): 3.1 (1.71) Years of illness (SD): 8 (7.22) Healthy controls: yes (41 controls) | NEO Five-Factor Inventory (NEO-FFI)
(only Neuroticism and Extroversion were assessed) | Fatigue Severity Scale (FSS) Modified fatigue impact scale (MFIS)
|
|
|
| Fernandez-Muños (2015) [78] Spain Cross-sectional study Participants: 108 Mean Age (SD): 44 (9) Female/Male: 59/49 MS Diagnosis: Modified McDonald’s criteria Clinical status: 74% of patients have RR MS, 8% PP MS, 18% SP MS EDSS mean (SD): 3.6 (1.6) Years of illness (SD): 12.8 (8) Healthy control: No | NEO Five-Factor Inventory (NEO-FFI)
| Fatigue Impact Scale (FIS) |
|
|
| Strober (2017) [85] United States Cross-sectional study Participants: 37 type D pos on 230 pwMS Mean Age (SD): 41.81 (9.82) Type D pos Female/Male: 33/4 Type D pos MS Diagnosis: McDonald’s criteria Clinical status: 97% RR MS EDSS mean (SD): NA Years of illness (SD): 7.18 (7.05) TypeD pos Healthy controls: no | NEO Five-Factor Inventory 3 (NEO-FFI-3)
International Personality Item Pool LOC scale (IPIP-LOC) Neuroticism (T > 60) and higher IPIP social discomfort were assessed to determine Type D personality | Modified fatigue impact scale (MFIS)
|
|
|
| Sindermann (2018) [83] Germany Cross-sectional study Participants: 52 Mean Age (SD): 45.13 (9.56) Female/Male: 43/9 MS Diagnosis: McDonald’s criteria Clinical status: 54% of patients have RR MS, 17% PP MS, 13% SP MS, 2% CIS, and 13% other. EDSS mean (SD): NA Years of illness (SD): 8.67 (7.36) Healthy controls: yes (screened by BDI-II score < 13) | NEO Five-Factor Inventory (NEO-FFI)
| Fatigue Scale for Motor and Cognitive Functions (FSMC)
|
|
|
| Spiegelberg (2021) [84] Germany Cross-sectional study Participants: 30 Mean Age (SD): 46.1 (9.6) Female/Male: 21/9 MS Diagnosis: McDonald’s criteria Clinical status: 80% of patients have RR MS, 13.3% SP MS, 3.3% CIS, and 3.3% other. EDSS median (range): 2.8 (1.5–7–5) Years of illness (SD): 9.1 (8.9) Healthy controls: yes | NEO Five-Factor Inventory (NEO-FFI)
| Fatigue Scale for Motor and Cognitive Functions (FSMC)
|
|
|
| Freiburg Personality | ||||
| Merkelbach (2003) [81] Germany Cross-sectional study Participants: 80 Mean Age (SD): 38.50 (9.0) Female/Male: 62/18 MS Diagnosis: Modified McDonald’s criteria Clinical status: 61.25% of patients have RR MS, 13.75% PP MS, 25% SP MS, EDSS mean (SD): 3.2 (1.4) Years of illness (SD): 9.10 (6.20) Healthy control: No | German Freiburg Personality Inventory—revised (FPI-R)
| Fatigue Severity Scale (FSS) Chronic Fatigue Scale (CFS) |
|
|
| Eysenck PEN system for personality | ||||
| Van Der Werf (2003) [86] Netherlands Cross-sectional study Participants:89 Mean Age (range): 41.9 (25–69) Female/Male: 63/26 MS Diagnosis: revised Poser criteria Clinical status: 58.4% of patients have RR MS, 41.6% SP MS and PP MS. EDSS mean (SD): 4.4 (1.8) Years of illness (SD): 9.1 (8.9) Healthy controls: No | Eysenck Personality Questionnaire (EPQ)
Subscale neuroticism was assessed as EI, emotional instability | Subjective Fatigue of the Checklist Individual Strength (CIS-Fatigue). |
|
|
| Skinnerian reinforcement theory | ||||
| Besharat (2011) [77] Iran Cross-sectional study Participants: 120 Mean Age (SD): 32.82 (8.22) Female/Male: 79/41 MS Diagnosis: Modified McDonald’s criteria Clinical status: 32.5% of patients have RR MS, 12.1% PP MS, 4.2% SP MS EDSS mean (SD): NA Years of illness (SD): 6.84 (3.99) Healthy control: yes | Positive and negative perfectionism scale (PANPS)
| Modified fatigue impact scale (MFIS) Fatigue severity scale (FSS) |
|
|
| Millon’s model | ||||
| Incerti (2015) [79] Italy D: Cross-sectional study Participants: 77 Mean Age (SD): 43.1 (9.8) Female/Male: 56/21 MS Diagnosis: Modified McDonald’s criteria Clinical status: 82.4% of patients have RR MS, 20.7% SP MS EDSS mean (SD): 3.2 (1.6) Years of illness (SD): 12.9 (7.5) Healthy control: No | Millon Clinical Multiaxial Inventory-III (MCMI-III):
| Modified fatigue impact scale (MFIS) |
|
|
| Temperament and character theory | ||||
| Matesic (2020) [80] Croatia Cross-sectional study Participants: 201 Mean Age (SD): 39.40 (10.81) Female/Male: 153/48 MS Diagnosis: Modified McDonald’s criteria Clinical status: 81.6% of patients have RR MS, 5% PP MS, 10.9% SP MS, 2.5% PR MS EDSS mean (SD): 2.6 (2.12) Years of illness (SD): 7.96 (6.38) Healthy control: No | Temperament and Character Inventory Revised (TCI-R),Four temperament dimensions
| Modified fatigue impact scale (MFIS) |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciancio, A.; Moretti, M.C.; Natale, A.; Rodolico, A.; Signorelli, M.S.; Petralia, A.; Altamura, M.; Bellomo, A.; Zanghì, A.; D’Amico, E.; et al. Personality Traits and Fatigue in Multiple Sclerosis: A Narrative Review. J. Clin. Med. 2023, 12, 4518. https://doi.org/10.3390/jcm12134518
Ciancio A, Moretti MC, Natale A, Rodolico A, Signorelli MS, Petralia A, Altamura M, Bellomo A, Zanghì A, D’Amico E, et al. Personality Traits and Fatigue in Multiple Sclerosis: A Narrative Review. Journal of Clinical Medicine. 2023; 12(13):4518. https://doi.org/10.3390/jcm12134518
Chicago/Turabian StyleCiancio, Alessia, Maria Claudia Moretti, Antimo Natale, Alessandro Rodolico, Maria Salvina Signorelli, Antonino Petralia, Mario Altamura, Antonello Bellomo, Aurora Zanghì, Emanuele D’Amico, and et al. 2023. "Personality Traits and Fatigue in Multiple Sclerosis: A Narrative Review" Journal of Clinical Medicine 12, no. 13: 4518. https://doi.org/10.3390/jcm12134518
APA StyleCiancio, A., Moretti, M. C., Natale, A., Rodolico, A., Signorelli, M. S., Petralia, A., Altamura, M., Bellomo, A., Zanghì, A., D’Amico, E., Avolio, C., & Concerto, C. (2023). Personality Traits and Fatigue in Multiple Sclerosis: A Narrative Review. Journal of Clinical Medicine, 12(13), 4518. https://doi.org/10.3390/jcm12134518








