Which Factors Were Related to the Number of COVID-19 Cases in the 2022/2023 Season Compared to the 2021/2022 Season in Europe?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Search and Extraction
2.2. Statistical Analysis
3. Results
3.1. Comparison of COVID-19 Infections in Analyzed Countries
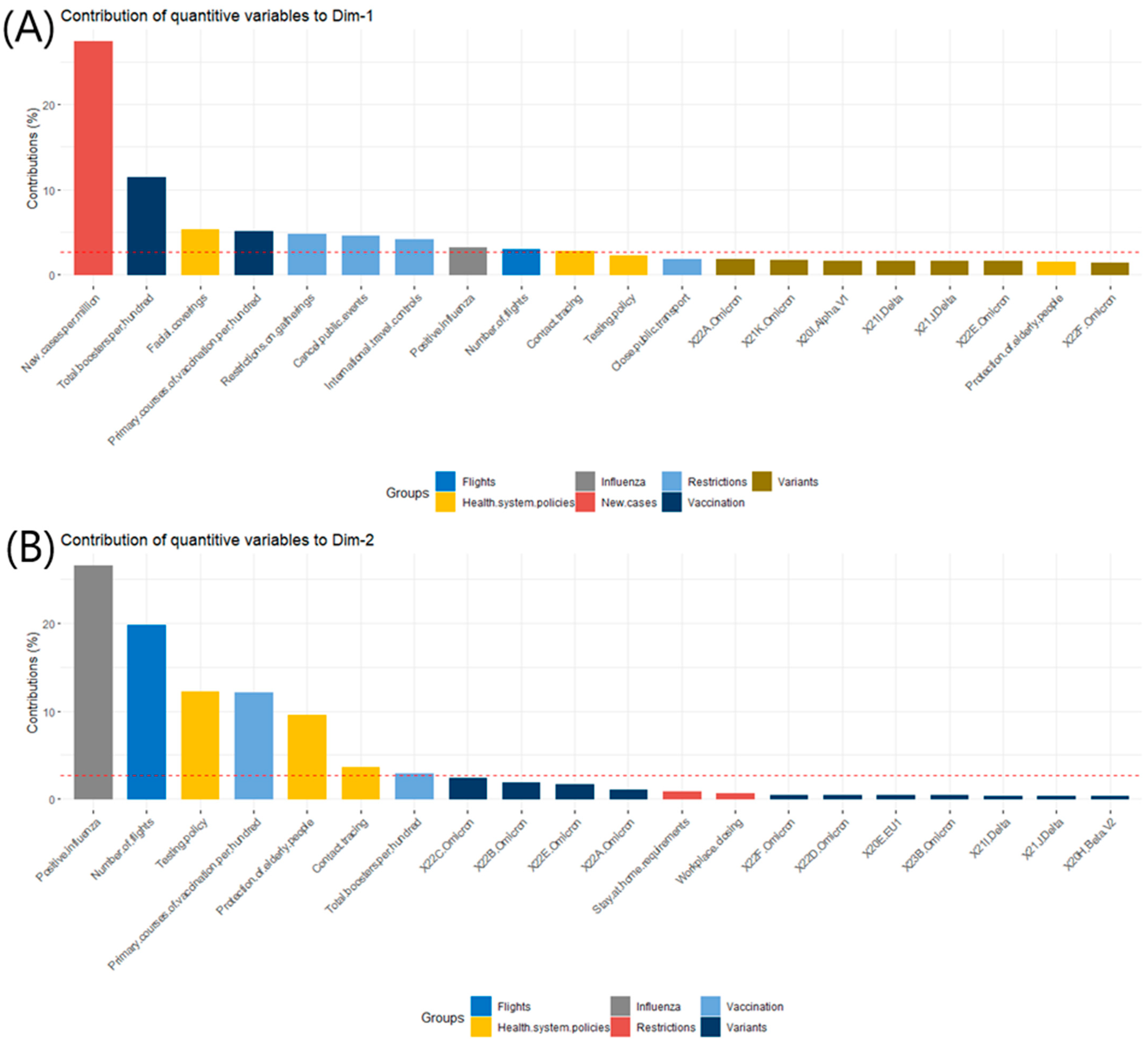
3.2. Definitions of the Contributing to the Dimensions: Dim-1 and Dim-2
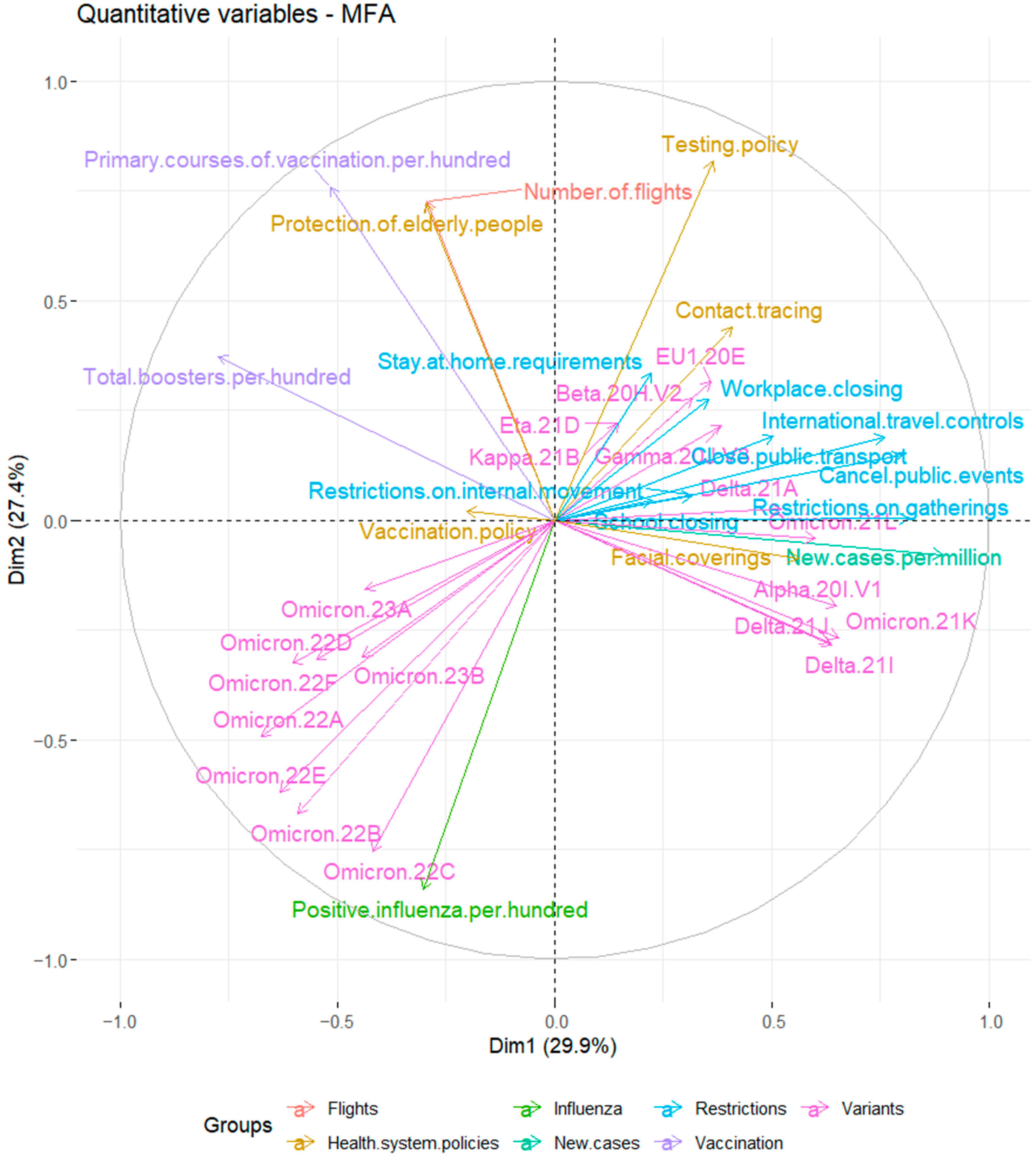
3.3. The Relationships between Analyzed Variables
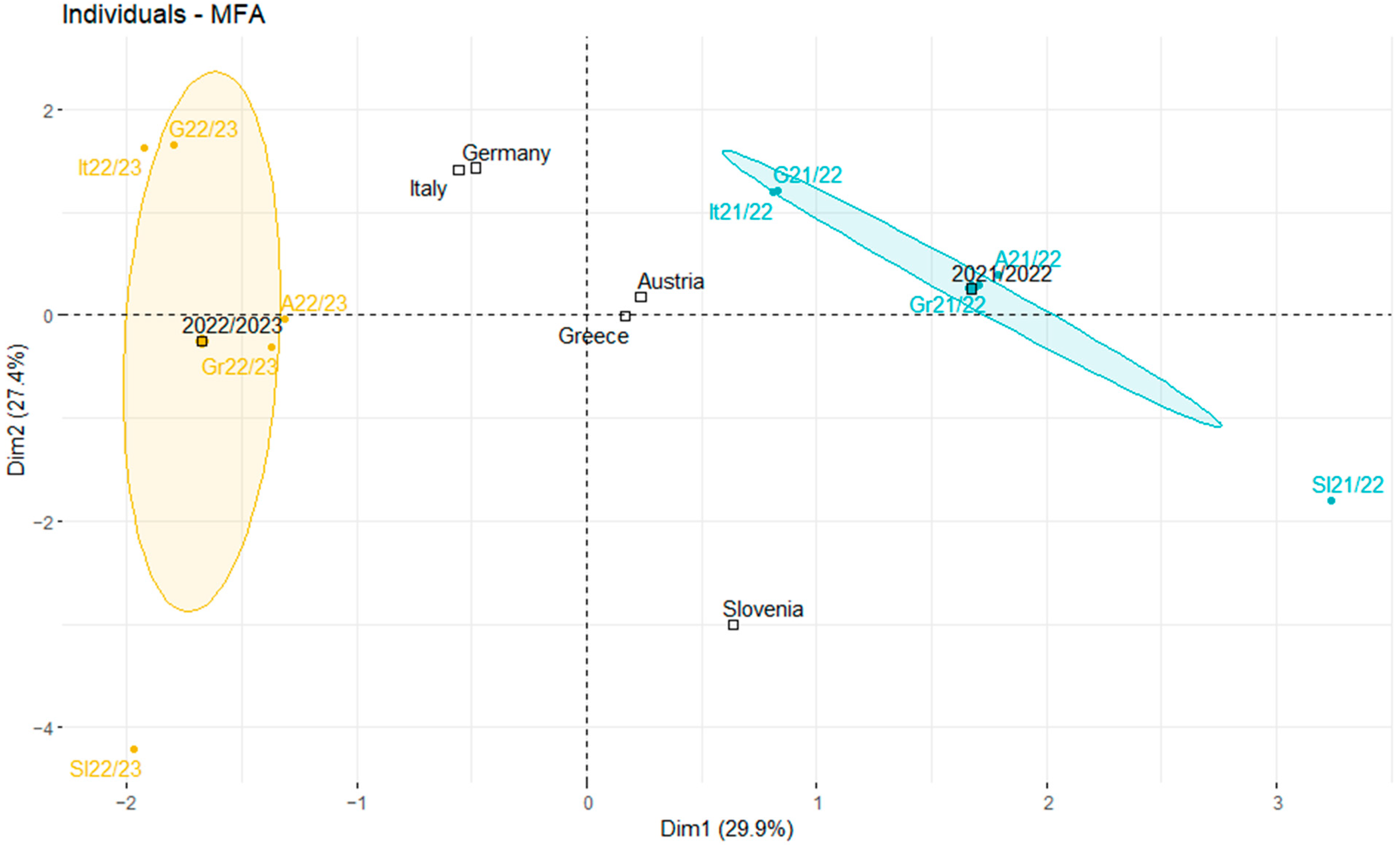
3.4. Comparison of Variable Profiles for Analyzed Countries in Autumn 2021 and 2022
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohamed, K.; Rzymski, P.; Islam, M.S.; Makuku, R.; Mushtaq, A.; Khan, A.; Ivanovska, M.; Makka, S.A.; Hashem, F.; Marquez, L.; et al. COVID-19 Vaccinations: The Unknowns, Challenges, and Hopes. J. Med. Virol. 2022, 94, 1336–1349. [Google Scholar] [CrossRef] [PubMed]
- Mohseni Afshar, Z.; Barary, M.; Hosseinzadeh, R.; Karim, B.; Ebrahimpour, S.; Nazary, K.; Sio, T.T.; Sullman, M.J.M.; Carson-Chahhoud, K.; Moudi, E.; et al. COVID-19 Vaccination Challenges: A Mini-Review. Hum. Vaccin. Immunother. 2022, 18, 2066425. [Google Scholar] [CrossRef]
- Wood, R.; Reinhardt, G.Y.; RezaeeDaryakenari, B.; Windsor, L.C. Resisting Lockdown: The Influence of COVID-19 Restrictions on Social Unrest. Int. Stud. Q. 2022, 66, sqac015. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the Effectiveness of Worldwide COVID-19 Government Interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 6 May 2023).
- Sobczak, M.; Pawliczak, R. Factors That Affect the COVID-19 Pandemic in Summer 2022 Compared to Summer 2021. Int. J. Environ. Res. Public Health 2022, 19, 12561. [Google Scholar] [CrossRef] [PubMed]
- da Costa, V.G.; Saivish, M.V.; Santos, D.E.R.; de Lima Silva, R.F.; Moreli, M.L. Comparative Epidemiology between the 2009 H1N1 Influenza and COVID-19 Pandemics. J. Infect. Public Health 2020, 13, 1797–1804. [Google Scholar] [CrossRef]
- Choreño-Parra, J.A.; Jiménez-Álvarez, L.A.; Cruz-Lagunas, A.; Rodríguez-Reyna, T.S.; Ramírez-Martínez, G.; Sandoval-Vega, M.; Hernández-García, D.L.; Choreño-Parra, E.M.; Balderas-Martínez, Y.I.; Martinez-Sánchez, M.E.; et al. Clinical and Immunological Factors That Distinguish COVID-19 From Pandemic Influenza A(H1N1). Front. Immunol. 2021, 12, 593595. [Google Scholar] [CrossRef]
- Bai, Y.; Tao, X. Comparison of COVID-19 and influenza characteristics. J. Zhejiang Univ. Sci. B 2021, 22, 87–98. [Google Scholar] [CrossRef]
- Luo, J.; Zhang, Z.; Zhao, S.; Gao, R. A Comparison of Etiology, Pathogenesis, Vaccinal and Antiviral Drug Development between Influenza and COVID-19. Int. J. Mol. Sci. 2023, 24, 6369. [Google Scholar] [CrossRef]
- Binns, E.; Koenraads, M.; Hristeva, L.; Flamant, A.; Baier-Grabner, S.; Loi, M.; Lempainen, J.; Osterheld, E.; Ramly, B.; Chakakala-Chaziya, J.; et al. Influenza and Respiratory Syncytial Virus during the COVID-19 Pandemic: Time for a New Paradigm? Pediatr. Pulmonol. 2022, 57, 38–42. [Google Scholar] [CrossRef]
- COVID-19 Vaccine Tracker|European Centre for Disease Prevention and Control. Available online: https://vaccinetracker.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab (accessed on 6 May 2023).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Available online: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-03-01..latest&facet=none&country=AUT~DEU~GRC~ITA~SVN&pickerSort=asc&pickerMetric=location&Metric=Confirmed+cases&Interval=7-day+rolling+average&Relative+to+Population=true&Color+by+test+positivity=false (accessed on 6 May 2023).
- CoVariants. Available online: https://covariants.org/per-country (accessed on 6 May 2023).
- Influenza Surveillance Outputs. Available online: https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring/influenza-surveillance-outputs (accessed on 6 May 2023).
- EUROCONTROL|Supporting European Aviation. Available online: https://www.eurocontrol.int/Economics/DailyTrafficVariation-States.html (accessed on 6 May 2023).
- Worldometer—Real Time World Statistics. Available online: https://www.worldometers.info/world-population/population-by-country/ (accessed on 6 May 2023).
- Abdi, H.; Williams, L.J.; Valentin, D. Multiple Factor Analysis: Principal Component Analysis for Multitable and Multiblock Data Sets: Multiple Factor Analysis. WIREs Comp. Stat. 2013, 5, 149–179. [Google Scholar] [CrossRef]
- Bécue-Bertaut, M.; Pagès, J. Multiple Factor Analysis and Clustering of a Mixture of Quantitative, Categorical and Frequency Data. Comput. Stat. Data Anal. 2008, 52, 3255–3268. [Google Scholar] [CrossRef]
- Dergiades, T.; Milas, C.; Mossialos, E.; Panagiotidis, T. Effectiveness of Government Policies in Response to the First COVID-19 Outbreak. PLoS Glob. Public Health 2022, 2, e0000242. [Google Scholar] [CrossRef]
- Brauner, J.M.; Mindermann, S.; Sharma, M.; Johnston, D.; Salvatier, J.; Gavenčiak, T.; Stephenson, A.B.; Leech, G.; Altman, G.; Mikulik, V.; et al. Inferring the Effectiveness of Government Interventions against COVID-19. Science 2021, 371, eabd9338. [Google Scholar] [CrossRef]
- Sobczak, M.; Pawliczak, R. COVID-19 Mortality Rate Determinants in Selected Eastern European Countries. BMC Public Health 2022, 22, 2088. [Google Scholar] [CrossRef]
- Halperin, D.T.; Hearst, N.; Hodgins, S.; Bailey, R.C.; Klausner, J.D.; Jackson, H.; Wamai, R.G.; Ladapo, J.A.; Over, M.; Baral, S.; et al. Revisiting COVID-19 Policies: 10 Evidence-Based Recommendations for Where to Go from Here. BMC Public Health 2021, 21, 2084. [Google Scholar] [CrossRef]
- Kuitunen, I.; Renko, M.; Tapiainen, T. The End of COVID-19 Restrictions for Children in Autumn 2021 Was Followed by an Unusually Early, High-peak Respiratory Syncytial Virus Epidemic. Acta Paediatr. 2023, 112, 146–148. [Google Scholar] [CrossRef]
- Lupu, D.; Tiganasu, R. COVID-19 and the Efficiency of Health Systems in Europe. Health Econ. Rev. 2022, 12, 14. [Google Scholar] [CrossRef]
- Klumpp, M.; Loske, D.; Bicciato, S. COVID-19 Health Policy Evaluation: Integrating Health and Economic Perspectives with a Data Envelopment Analysis Approach. Eur. J. Health Econ. 2022, 23, 1263–1285. [Google Scholar] [CrossRef]
- Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 9 May 2023).
- Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 9 May 2023).
- Elliott, P.; Eales, O.; Bodinier, B.; Tang, D.; Wang, H.; Jonnerby, J.; Haw, D.; Elliott, J.; Whitaker, M.; Walters, C.E.; et al. Dynamics of a National Omicron SARS-CoV-2 Epidemic during January 2022 in England. Nat. Commun. 2022, 13, 4500. [Google Scholar] [CrossRef] [PubMed]
- ECDC De-Escalates BA.2, BA.4 and BA.5 from Its List of Variants of Concern. Available online: https://www.ecdc.europa.eu/en/news-events/ecdc-de-escalates-ba2-ba4-and-ba5-its-list-variants-concern (accessed on 9 May 2023).
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A Global Database of COVID-19 Vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Alexandridi, M.; Mazej, J.; Palermo, E.; Hiscott, J. The Coronavirus Pandemic—2022: Viruses, Variants & Vaccines. Cytokine Growth Factor. Rev. 2022, 63, 1–9. [Google Scholar] [CrossRef]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The Concept of Classical Herd Immunity May Not Apply to COVID-19. J. Infect. Dis. 2022, 226, 195–198. [Google Scholar] [CrossRef]
- Agrawal, U.; Bedston, S.; McCowan, C.; Oke, J.; Patterson, L.; Robertson, C.; Akbari, A.; Azcoaga-Lorenzo, A.; Bradley, D.T.; Fagbamigbe, A.F.; et al. Severe COVID-19 Outcomes after Full Vaccination of Primary Schedule and Initial Boosters: Pooled Analysis of National Prospective Cohort Studies of 30 Million Individuals in England, Northern Ireland, Scotland, and Wales. Lancet 2022, 400, 1305–1320. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef] [PubMed]
- Chalkias, S.; Harper, C.; Vrbicky, K.; Walsh, S.R.; Essink, B.; Brosz, A.; McGhee, N.; Tomassini, J.E.; Chen, X.; Chang, Y.; et al. A Bivalent Omicron-Containing Booster Vaccine against COVID-19. N. Engl. J. Med. 2022, 387, 1279–1291. [Google Scholar] [CrossRef]
- Kohli, M.A.; Maschio, M.; Lee, A.; Fust, K.; Van de Velde, N.; Buck, P.O.; Weinstein, M.C. The Potential Clinical Impact of Implementing Different COVID-19 Boosters in Fall 2022 in the United States. J. Med. Econ. 2022, 25, 1127–1139. [Google Scholar] [CrossRef] [PubMed]
- Influenza Virus Characterization: Summary Report, Europe, October 2022; World Health Organization Regional Office for Europe and European Centre for Disease Prevention and Control: Copenhagen, Denmark; Stockholm, Sweden, 2022.
- Toback, S.; Galiza, E.; Cosgrove, C.; Galloway, J.; Goodman, A.L.; Swift, P.A.; Rajaram, S.; Graves-Jones, A.; Edelman, J.; Burns, F.; et al. Safety, immunogenicity, and efficacy of a COVID-19 vaccine (NVX-CoV2373) co-administered with seasonal influenza vaccines: An exploratory substudy of a randomised, observer-blinded, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2022, 10, 167–179. [Google Scholar] [CrossRef]
- Lazarus, R.; Baos, S.; Cappel-Porter, H.; Carson-Stevens, A.; Clout, M.; Culliford, L.; Emmett, S.R.; Garstang, J.; Gbadamoshi, L.; Hallis, B.; et al. Safety and immunogenicity of concomitant administration of COVID-19 vaccines (ChAdOx1 or BNT162b2) with seasonal influenza vaccines in adults in the UK (ComFluCOV): A multicentre, randomised, controlled, phase 4 trial. Lancet 2021, 398, 2277–2287. [Google Scholar] [CrossRef]
- Conlon, A.; Ashur, C.; Washer, L.; Eagle, K.A.; Hofmann Bowman, M.A. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am. J. Infect. Control 2021, 49, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Candelli, M.; Pignataro, G.; Torelli, E.; Gullì, A.; Nista, E.C.; Petrucci, M.; Saviano, A.; Marchesini, D.; Covino, M.; Ojetti, V.; et al. Effect of influenza vaccine on COVID-19 mortality: A retrospective study. Intern. Emerg. Med. 2021, 16, 1849–1855. [Google Scholar] [CrossRef] [PubMed]
- Joint Statement—Influenza Season Epidemic Kicks off Early in Europe as Concerns over RSV Rise and COVID-19 Is Still a Threat. Available online: https://www.who.int/europe/news/item/01-12-2022-joint-statement---influenza-season-epidemic-kicks-off-early-in-europe-as-concerns-over-rsv-rise-and-covid-19-is-still-a-threat (accessed on 12 May 2023).
- Download Historical Data (to 20 June 2022) on the Weekly Number of New Reported COVID-19 Cases and Deaths Worldwide. Available online: https://www.ecdc.europa.eu/en/publications-data/download-historical-data-20-june-2022-weekly-number-new-reported-covid-19-cases (accessed on 12 May 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sobczak, M.; Pawliczak, R. Which Factors Were Related to the Number of COVID-19 Cases in the 2022/2023 Season Compared to the 2021/2022 Season in Europe? J. Clin. Med. 2023, 12, 4517. https://doi.org/10.3390/jcm12134517
Sobczak M, Pawliczak R. Which Factors Were Related to the Number of COVID-19 Cases in the 2022/2023 Season Compared to the 2021/2022 Season in Europe? Journal of Clinical Medicine. 2023; 12(13):4517. https://doi.org/10.3390/jcm12134517
Chicago/Turabian StyleSobczak, Marharyta, and Rafał Pawliczak. 2023. "Which Factors Were Related to the Number of COVID-19 Cases in the 2022/2023 Season Compared to the 2021/2022 Season in Europe?" Journal of Clinical Medicine 12, no. 13: 4517. https://doi.org/10.3390/jcm12134517
APA StyleSobczak, M., & Pawliczak, R. (2023). Which Factors Were Related to the Number of COVID-19 Cases in the 2022/2023 Season Compared to the 2021/2022 Season in Europe? Journal of Clinical Medicine, 12(13), 4517. https://doi.org/10.3390/jcm12134517






