Rifaximin Use, Adherence and Persistence in Patients with Hepatic Encephalopathy: A Real-World Study in the South of Italy
Abstract
1. Introduction
2. Methods
2.1. Data Sources
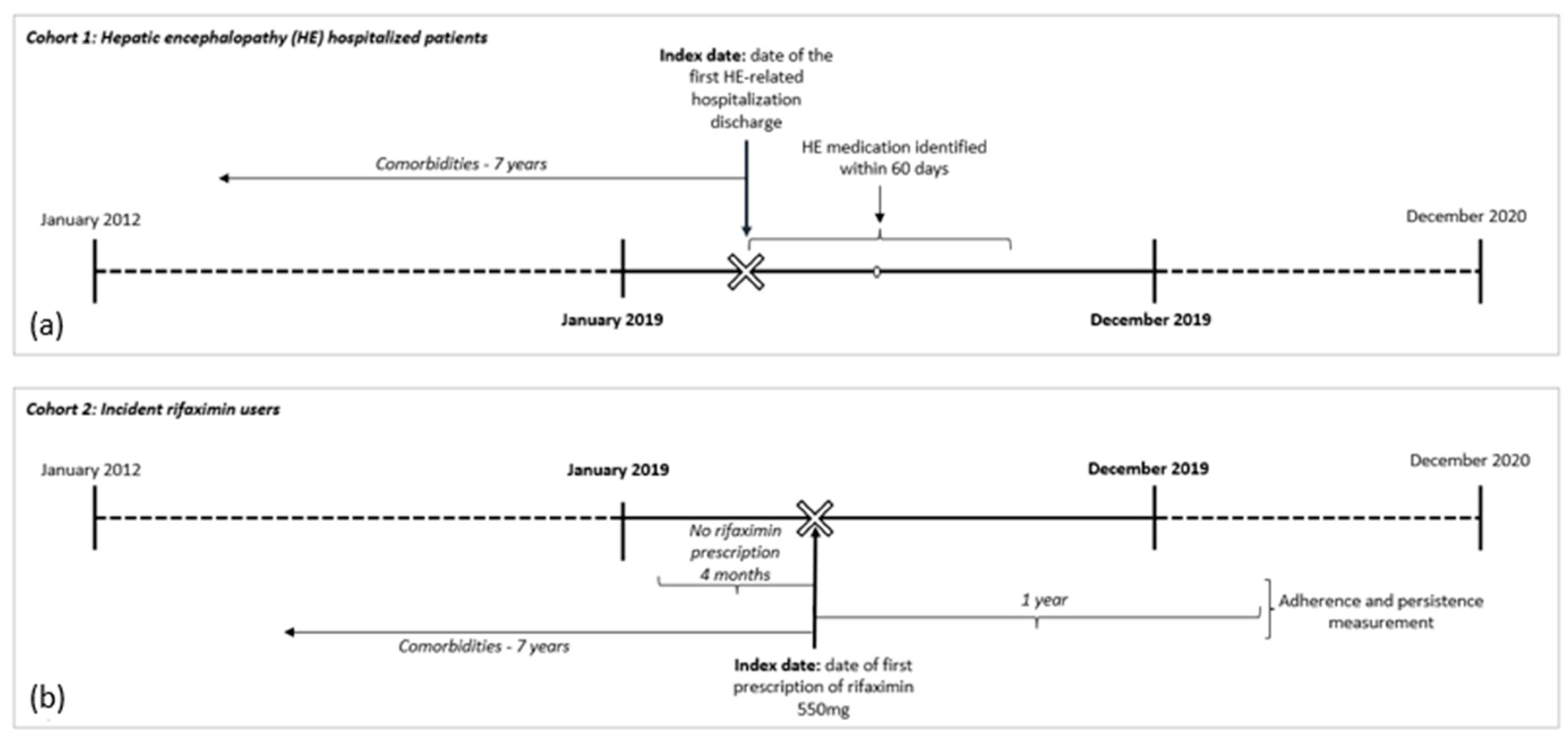
2.2. Study Design and Cohort Selection
2.2.1. Cohort 1—HE Hospitalized Patients
2.2.2. Cohort 2—Incident Rifaximin Users
2.2.3. Outcome for Cohort 1
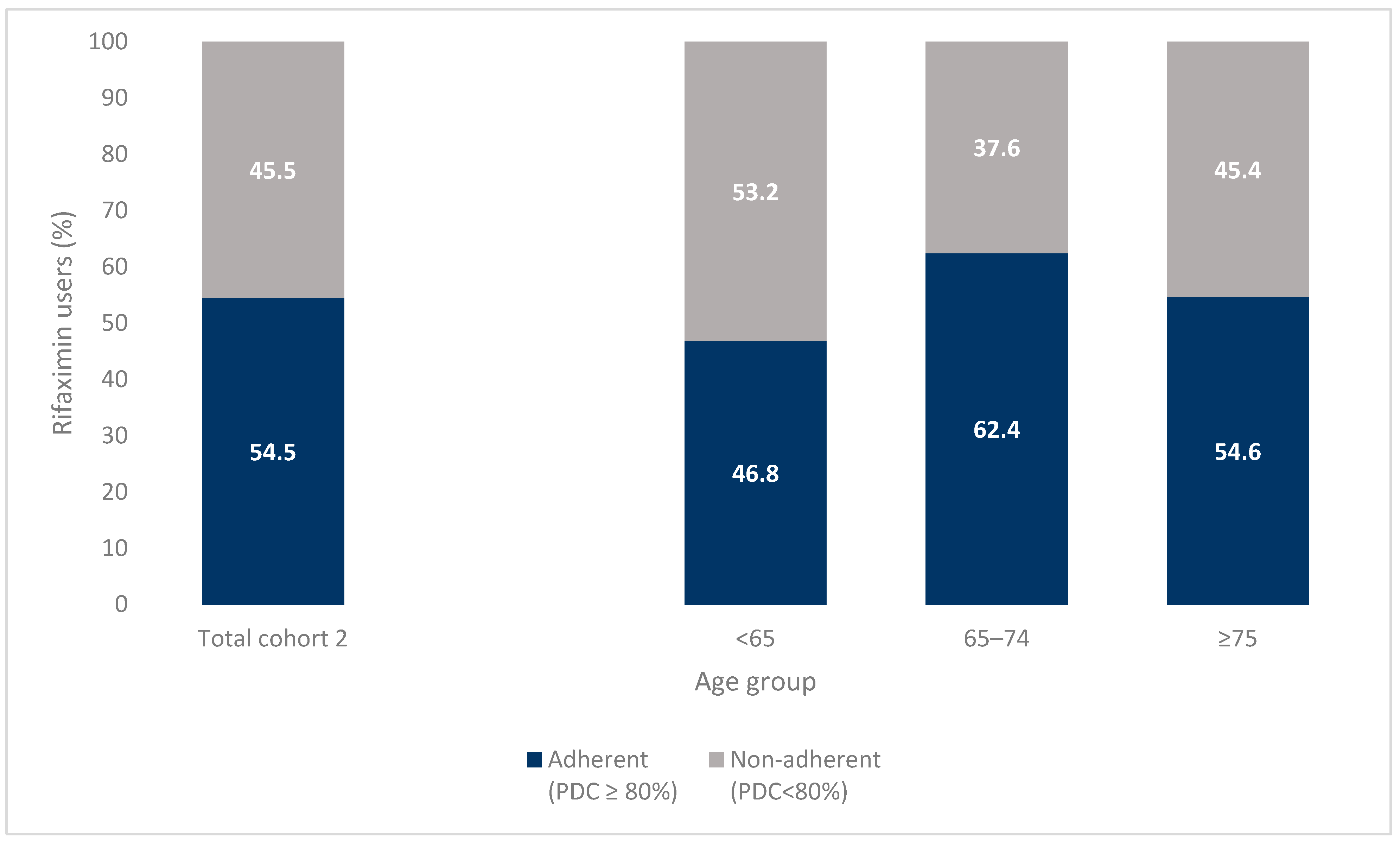
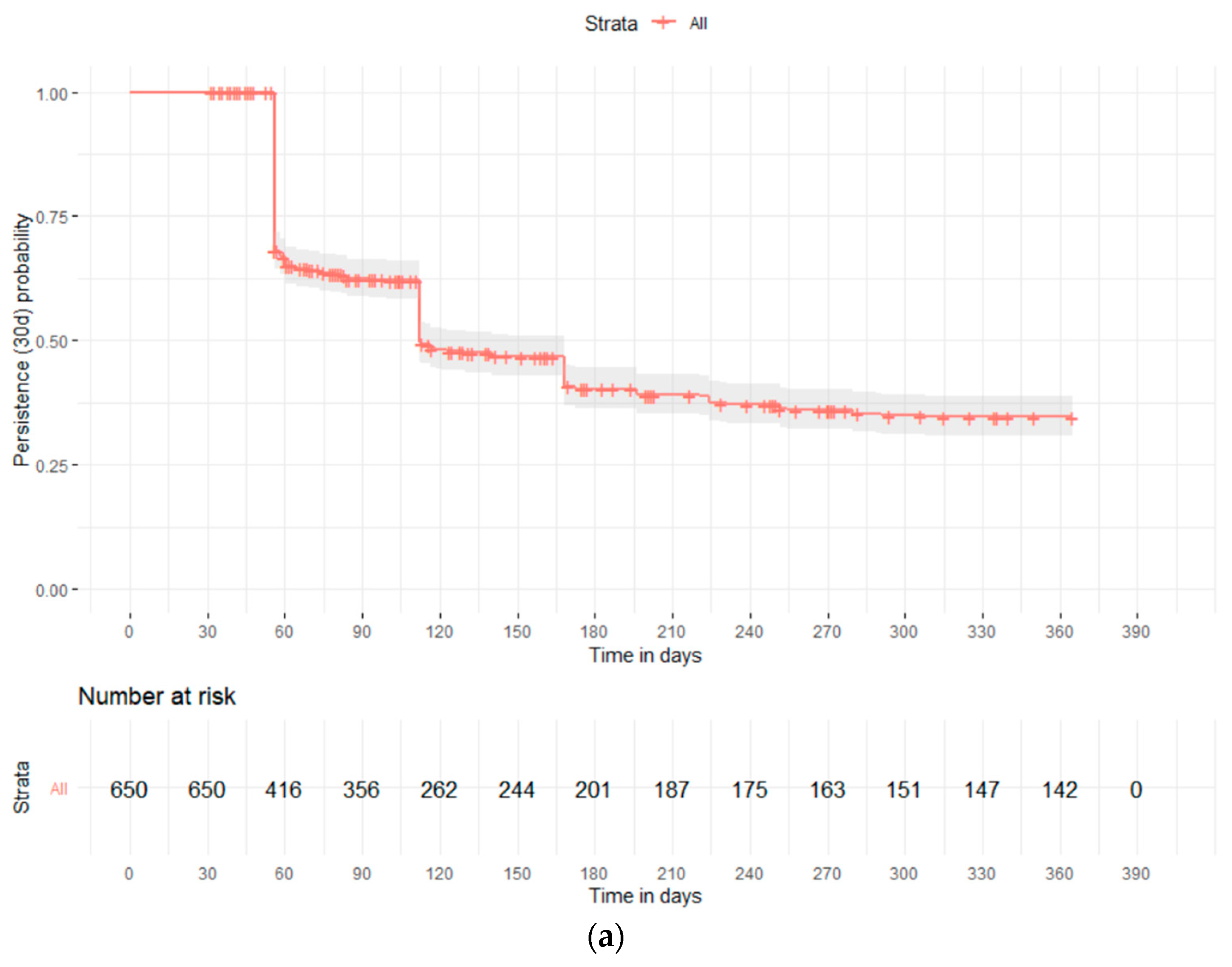
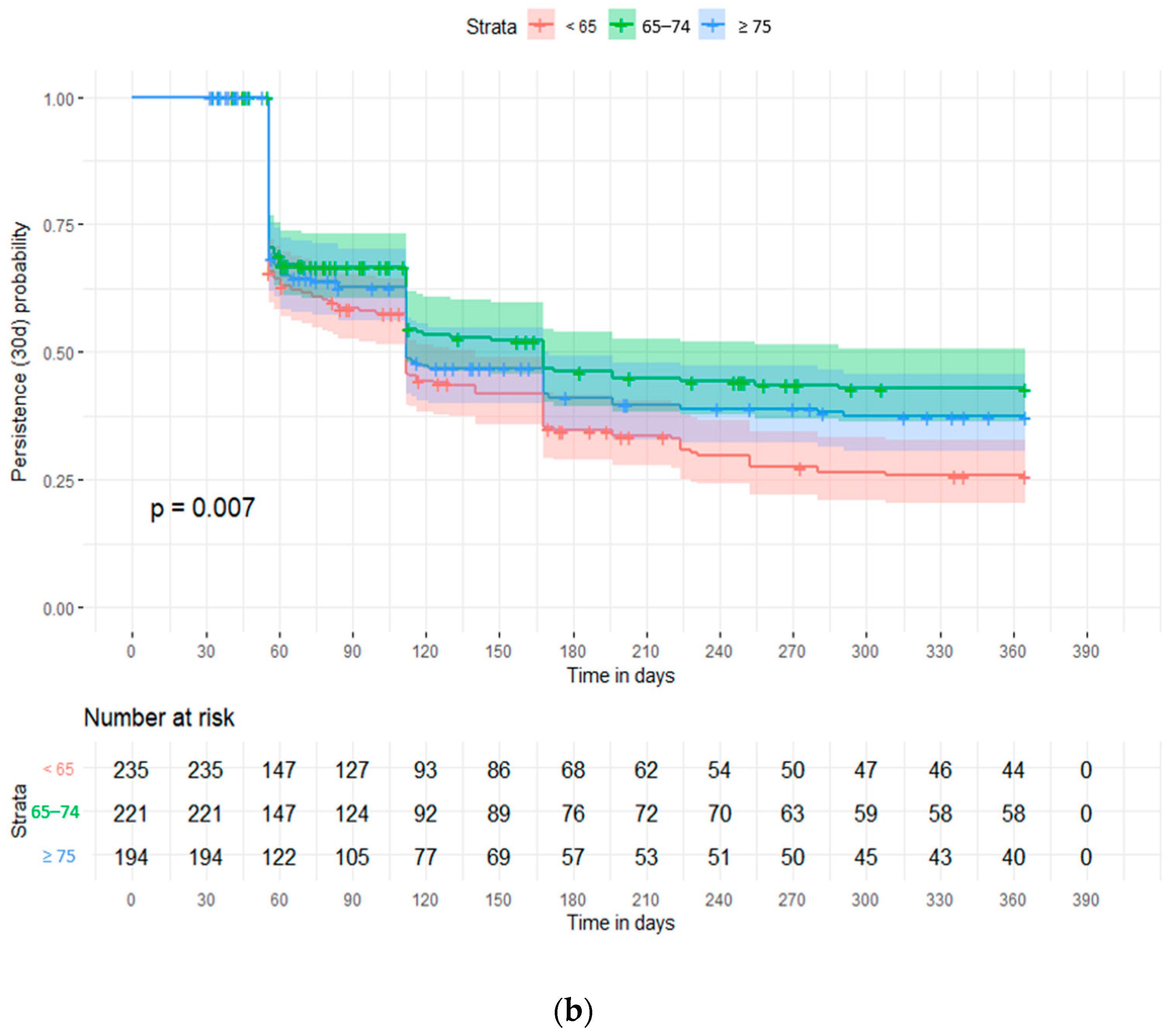
2.2.4. Outcome for Cohort 2
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Cammarota, S.; Citarella, A.; Bernardi, F.F.; Claar, E.; Fogliasecca, M.; Manzo, V.; Rosato, V.; Toraldo, B.; Trama, U.; Valente, A.; et al. Burden of Compensated and Decompensated Cirrhosis: Real World Data from an Italian Population-Based Cohort Study. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 4490–4498. [Google Scholar] [CrossRef]
- Bustamante, J.; Rimola, A.; Ventura, P.-J.; Navasa, M.; Cirera, I.; Reggiardo, V.; Rodés, J. Prognostic Significance of Hepatic Encephalopathy in Patients with Cirrhosis. J. Hepatol. 1999, 30, 890–895. [Google Scholar] [CrossRef]
- Fichet, J.; Mercier, E.; Genée, O.; Garot, D.; Legras, A.; Dequin, P.-F.; Perrotin, D. Prognosis and 1-Year Mortality of Intensive Care Unit Patients with Severe Hepatic Encephalopathy. J. Crit. Care 2009, 24, 364–370. [Google Scholar] [CrossRef]
- Neff, G.; Iii, W.Z. Systematic Review of the Economic Burden of Overt Hepatic Encephalopathy and Pharmacoeconomic Impact of Rifaximin. PharmacoEconomics 2018, 36, 809–822. [Google Scholar] [CrossRef]
- Vilstrup, H.; Amodio, P.; Bajaj, J.; Cordoba, J.; Ferenci, P.; Mullen, K.D.; Weissenborn, K.; Wong, P. Hepatic Encephalopathy in Chronic Liver Disease: 2014 Practice Guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J. Hepatol. 2014, 61, 642–659. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Wade, J.B.; Gibson, D.P.; Heuman, D.M.; Thacker, L.R.; Sterling, R.K.; Stravitz, T.R.; Luketic, V.; Fuchs, M.; White, M.B.; et al. The Multi-Dimensional Burden of Cirrhosis and Hepatic Encephalopathy on Patients and Caregivers. Am. J. Gastroenterol. 2011, 106, 1646–1653. [Google Scholar] [CrossRef]
- Bongaerts, G.; Severijnen, R.; Timmerman, H. Effect of Antibiotics, Prebiotics and Probiotics in Treatment for Hepatic Encephalopathy. Med. Hypotheses 2005, 64, 64–68. [Google Scholar] [CrossRef]
- Ponziani, F.R.; Zocco, M.A.; D’Aversa, F.; Pompili, M.; Gasbarrini, A. Eubiotic Properties of Rifaximin: Disruption of the Traditional Concepts in Gut Microbiota Modulation. World J. Gastroenterol. 2017, 23, 4491. [Google Scholar] [CrossRef]
- Montagnese, S.; Amato, E.; Schiff, S.; Facchini, S.; Angeli, P.; Gatta, A.; Amodio, P. A Patients’ and Caregivers’ Perspective on Hepatic Encephalopathy. Metab. Brain Dis. 2012, 27, 567–572. [Google Scholar] [CrossRef]
- Mencarelli, A.; Renga, B.; Palladino, G.; Claudio, D.; Ricci, P.; Distrutti, E.; Barbanti, M.; Baldelli, F.; Fiorucci, S. Inhibition of NF-ΚB by a PXR-Dependent Pathway Mediates Counter-Regulatory Activities of Rifaximin on Innate Immunity in Intestinal Epithelial Cells. Eur. J. Pharmacol. 2011, 668, 317–324. [Google Scholar] [CrossRef]
- Bannister, C.A.; Orr, J.G.; Reynolds, A.V.; Hudson, M.; Conway, P.; Radwan, A.; Morgan, C.L.; Currie, C.J. Natural History of Patients Taking Rifaximin-α for Recurrent Hepatic Encephalopathy and Risk of Future Overt Episodes and Mortality: A Post-Hoc Analysis of Clinical Trials Data. Clin. Ther. 2016, 38, 1081–1089.e4. [Google Scholar] [CrossRef] [PubMed]
- Hudson, M.; Schuchmann, M. Long-Term Management of Hepatic Encephalopathy with Lactulose and/or Rifaximin: A Review of the Evidence. Eur. J. Gastroenterol. Hepatol. 2019, 31, 434–450. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Lee, Y.B.; Lee, J.-H.; Nam, J.Y.; Chang, Y.; Cho, H.; Yoo, J.-J.; Cho, Y.Y.; Cho, E.J.; Yu, S.J.; et al. Rifaximin Treatment Is Associated with Reduced Risk of Cirrhotic Complications and Prolonged Overall Survival in Patients Experiencing Hepatic Encephalopathy. Aliment. Pharmacol. Ther. 2017, 46, 845–855. [Google Scholar] [CrossRef]
- Ryan, J.D.; Tsochatzis, E.A. Rifaximin Treatment for Encephalopathy Reduces Hospital Resource Use: Real-World Data Don’t Fail to IMPRESS. Frontline Gastroenterol. 2017, 8, 230–231. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chu, P.; Wang, W. Combination of Rifaximin and Lactulose Improves Clinical Efficacy and Mortality in Patients with Hepatic Encephalopathy. Drug Des. Dev. Ther. 2018, 13, 1–11. [Google Scholar] [CrossRef]
- Mullen, K.D.; Sanyal, A.J.; Bass, N.M.; Poordad, F.F.; Sheikh, M.Y.; Frederick, R.T.; Bortey, E.; Forbes, W.P. Rifaximin Is Safe and Well Tolerated for Long-Term Maintenance of Remission From Overt Hepatic Encephalopathy. Clin. Gastroenterol. Hepatol. 2014, 12, 1390–1397.e2. [Google Scholar] [CrossRef]
- Pantham, G.; Post, A.; Venkat, D.; Einstadter, D.; Mullen, K.D. A New Look at Precipitants of Overt Hepatic Encephalopathy in Cirrhosis. Dig. Dis. Sci. 2017, 62, 2166–2173. [Google Scholar] [CrossRef]
- Montagnese, S.; Rautou, P.-E.; Romero-Gómez, M.; Larsen, F.S.; Shawcross, D.L.; Thabut, D.; Vilstrup, H.; Weissenborn, K. EASL Clinical Practice Guidelines on the Management of Hepatic Encephalopathy. J. Hepatol. 2022, 77, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Montagnese, S.; Russo, F.P.; Amodio, P.; Burra, P.; Gasbarrini, A.; Loguercio, C.; Marchesini, G.; Merli, M.; Ponziani, F.R.; Riggio, O.; et al. Hepatic Encephalopathy 2018: A Clinical Practice Guideline by the Italian Association for the Study of the Liver (AISF). Dig. Liver Dis. 2019, 51, 190–205. [Google Scholar] [CrossRef]
- Bass, N.M.; Mullen, K.D.; Sanyal, A.; Poordad, F.; Neff, G.; Leevy, C.B.; Sigal, S.; Sheikh, M.Y.; Beavers, K.; Frederick, T.; et al. Rifaximin Treatment in Hepatic Encephalopathy. N. Engl. J. Med. 2010, 362, 1071–1081. [Google Scholar] [CrossRef]
- Adherence: Pharmacy Quality Alliance Adherence Measures. Available online: www.pqaalliance.org/adherence-measures (accessed on 3 July 2023).
- Cramer, J.A.; Roy, A.; Burrell, A.; Fairchild, C.J.; Fuldeore, M.J.; Ollendorf, D.A.; Wong, P.K. Medication Compliance and Persistence: Terminology and Definitions. Value Health 2008, 11, 44–47. [Google Scholar] [CrossRef]
- Geers, H.C.; Bouvy, M.L.; Heerdink, E.R. Estimates of Statin Discontinuation Rates Are Influenced by Exposure and Outcome Definitions. Ann. Pharmacother. 2011, 45, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Gao, Y.; Shi, L. Combination Therapy with Rifaximin and Lactulose in Hepatic Encephalopathy: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0267647. [Google Scholar] [CrossRef] [PubMed]
- Volk, M.L.; Burne, R.; Guérin, A.; Shi, S.; Joseph, G.J.; Heimanson, Z.; Ahmad, M. Hospitalizations and Healthcare Costs Associated with Rifaximin versus Lactulose Treatment among Commercially Insured Patients with Hepatic Encephalopathy in the United States. J. Med. Econ. 2021, 24, 202–211. [Google Scholar] [CrossRef]
- Stoll, A.M.; Guido, M.; Pence, A.; Gentene, A.J. Lack of Access to Rifaximin Upon Hospital Discharge Is Frequent and Results in Increased Hospitalizations for Hepatic Encephalopathy. Ann. Pharmacother. 2023, 57, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, R.S.; Brown, K.A.; Flamm, S.L.; Brown, R.S. Overt Hepatic Encephalopathy: Current Pharmacologic Treatments and Improving Clinical Outcomes. Am. J. Med. 2021, 134, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Di Pascoli, M.; Ceranto, E.; De Nardi, P.; Donato, D.; Gatta, A.; Angeli, P.; Pontisso, P. Hospitalizations Due to Cirrhosis: Clinical Aspects in a Large Cohort of Italian Patients and Cost Analysis Report. Dig. Dis. 2017, 35, 433–438. [Google Scholar] [CrossRef]
- Jinjuvadia, R.; Liangpunsakul, S. Trends in Alcoholic Hepatitis-Related Hospitalizations, Financial Burden, and Mortality in the United States. J. Clin. Gastroenterol. 2015, 49, 506–511. [Google Scholar] [CrossRef]
- Patidar, K.R.; Thacker, L.R.; Wade, J.B.; White, M.B.; Gavis, E.A.; Fagan, A.; Sterling, R.K.; Fuchs, M.; Siddiqui, M.S.; Matherly, S.; et al. Symptom Domain Groups of the Patient-Reported Outcomes Measurement Information System Tools Independently Predict Hospitalizations and Re-Hospitalizations in Cirrhosis. Dig. Dis. Sci. 2017, 62, 1173–1179. [Google Scholar] [CrossRef]
- Khokhar, N.; Qureshi, M.O.; Ahmad, S.; Ahmad, A.; Khan, H.H.; Shafqat, F.; Salih, M. Comparison of Once a Day Rifaximin to Twice a Day Dosage in the Prevention of Recurrence of Hepatic Encephalopathy in Patients with Chronic Liver Disease: Rifaximin Dosage in Hepatic Encephalopathy. J. Gastroenterol. Hepatol. 2015, 30, 1420–1422. [Google Scholar] [CrossRef]
- Lyon, K.C.; Likar, E.; Martello, J.L.; Regier, M. Retrospective Cross-Sectional Pilot Study of Rifaximin Dosing for the Prevention of Recurrent Hepatic Encephalopathy: Rifaximin Dosing for Hepatic Encephalopathy. J. Gastroenterol. Hepatol. 2017, 32, 1548–1552. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, K.M.; Attri, S.; Orlando, M.; Lelli, F.; Maida, V.; Damais-Thabut, D. Cost-Effectiveness of Rifaximin-α versus Lactulose for the Treatment of Recurrent Episodes of Overt Hepatic Encephalopathy: A Meta-Analysis. GastroHep 2022, 2022, 1298703. [Google Scholar] [CrossRef]
- Sherwin, L.B.; Ross, D.; Matteson-Kome, M.; Bechtold, M.; Deroche, C.; Wakefield, B. Patient Perspectives on Short-Course Pharmacotherapy: Barriers and Facilitators to Medication Adherence. J. Patient Exp. 2020, 7, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Garrido, M.; Turco, M.; Formentin, C.; Corrias, M.; De Rui, M.; Montagnese, S.; Amodio, P. An Educational Tool for the Prophylaxis of Hepatic Encephalopathy. BMJ Open Gastroenterol. 2017, 4, e000161. [Google Scholar] [CrossRef] [PubMed]
- West, S.L.; Savitz, D.A.; Koch, G.; Strom, B.L.; Guess, H.A.; Hartzema, A. Recall Accuracy for Prescription Medications: Self-Report Compared with Database Information. Am. J. Epidemiol. 1995, 142, 1103–1112. [Google Scholar] [CrossRef]

| HE Hospitalized Patients | Incident Rifaximin Users | |||
|---|---|---|---|---|
| N = 544 | N = 650 | |||
| n | % | n | % | |
| Gender | ||||
| Male | 337 | 61.9 | 411 | 63.2 |
| Female | 207 | 38.1 | 239 | 36.8 |
| Age (years) | ||||
| <65 | 216 | 39.7 | 235 | 36.2 |
| 65–74 | 171 | 31.4 | 221 | 34.0 |
| ≥75 | 157 | 28.9 | 194 | 29.8 |
| Cirrhosis complication | ||||
| Ascites | 286 | 52.6 | 223 | 34.3 |
| Varices | 212 | 39.0 | 199 | 30.6 |
| Portal hypertension | 118 | 21.7 | 128 | 19.7 |
| Hepatocellular carcinoma | 107 | 19.7 | 99 | 15.2 |
| Other * | 65 | 11.9 | 40 | 6.2 |
| Extra-hepatic comorbidities | ||||
| Diabetes | 198 | 36.4 | 185 | 28.5 |
| Cardiovascular disease | 179 | 32.9 | 138 | 21.2 |
| Chronic kidney disease | 148 | 27.2 | 93 | 14.3 |
| Cerebrovascular disease | 132 | 24.3 | 85 | 13.1 |
| Cancer | 46 | 8.5 | 76 | 11.7 |
| Psychiatric conditions | 9 | 1.7 | 13 | 2.0 |
| Number of extra-hepatic comorbidities | ||||
| 0 | 153 | 28.1 | 330 | 50.8 |
| 1 | 178 | 32.7 | 138 | 21.2 |
| ≥2 | 213 | 39.2 | 182 | 28.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pandico, F.; Citarella, A.; Cammarota, S.; Bernardi, F.F.; Claar, E.; Coppola, C.; Cozzolino, M.; De Rosa, F.; Di Gennaro, M.; Fogliasecca, M.; et al. Rifaximin Use, Adherence and Persistence in Patients with Hepatic Encephalopathy: A Real-World Study in the South of Italy. J. Clin. Med. 2023, 12, 4515. https://doi.org/10.3390/jcm12134515
Pandico F, Citarella A, Cammarota S, Bernardi FF, Claar E, Coppola C, Cozzolino M, De Rosa F, Di Gennaro M, Fogliasecca M, et al. Rifaximin Use, Adherence and Persistence in Patients with Hepatic Encephalopathy: A Real-World Study in the South of Italy. Journal of Clinical Medicine. 2023; 12(13):4515. https://doi.org/10.3390/jcm12134515
Chicago/Turabian StylePandico, Fulvio, Anna Citarella, Simona Cammarota, Francesca Futura Bernardi, Ernesto Claar, Carmine Coppola, Marianna Cozzolino, Federica De Rosa, Massimo Di Gennaro, Marianna Fogliasecca, and et al. 2023. "Rifaximin Use, Adherence and Persistence in Patients with Hepatic Encephalopathy: A Real-World Study in the South of Italy" Journal of Clinical Medicine 12, no. 13: 4515. https://doi.org/10.3390/jcm12134515
APA StylePandico, F., Citarella, A., Cammarota, S., Bernardi, F. F., Claar, E., Coppola, C., Cozzolino, M., De Rosa, F., Di Gennaro, M., Fogliasecca, M., Giordana, R., Pacella, D., Russo, A., Salerno, V., Scafa, L., & Trama, U. (2023). Rifaximin Use, Adherence and Persistence in Patients with Hepatic Encephalopathy: A Real-World Study in the South of Italy. Journal of Clinical Medicine, 12(13), 4515. https://doi.org/10.3390/jcm12134515








