A Real-Life Study of Combined Treatment with Long-Term Non-Invasive Ventilation and High Flow Nasal Cannula in Patients with End-Stage Chronic Obstructive Lung Disease
Abstract
1. Introduction
2. Methods
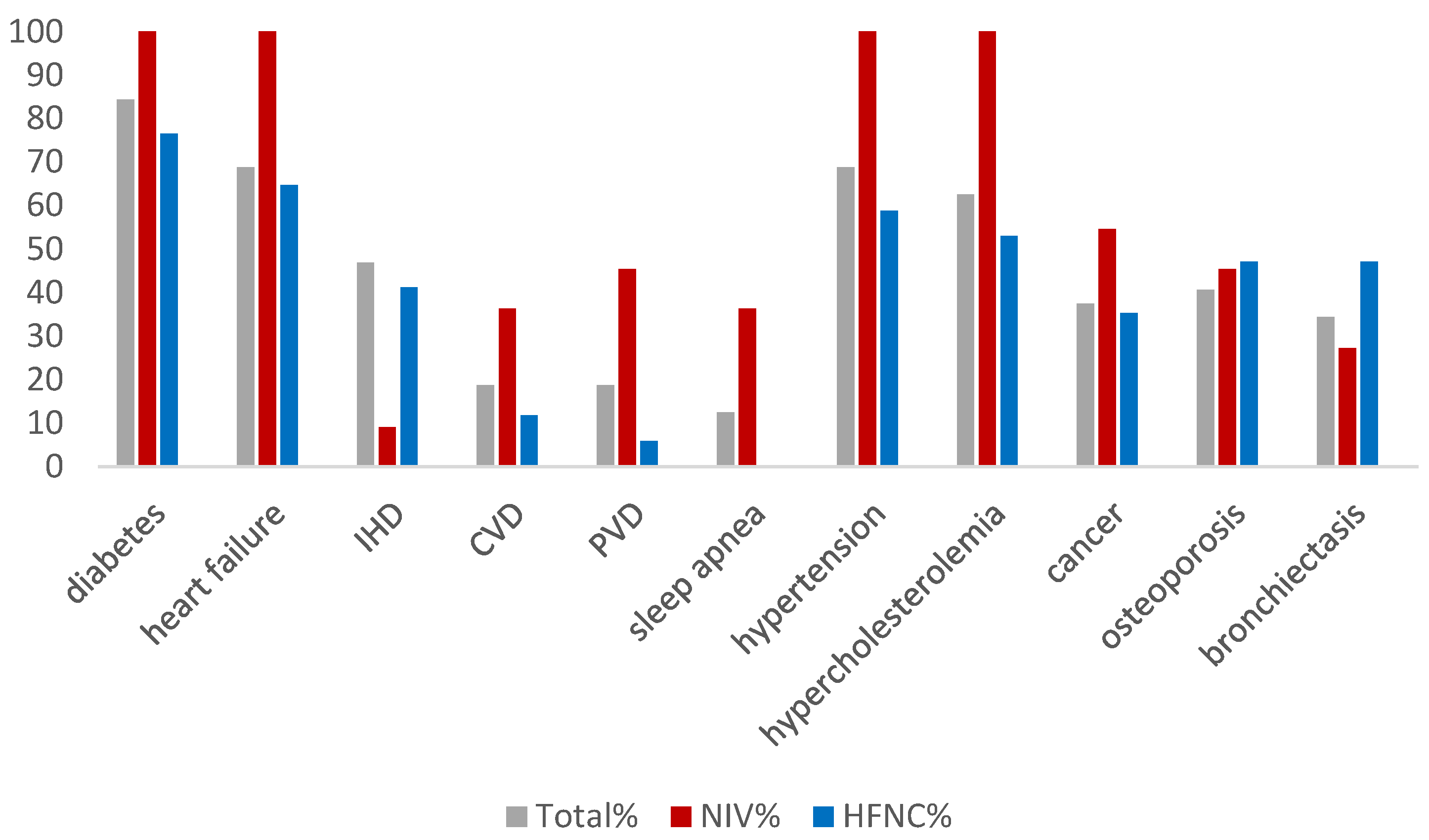
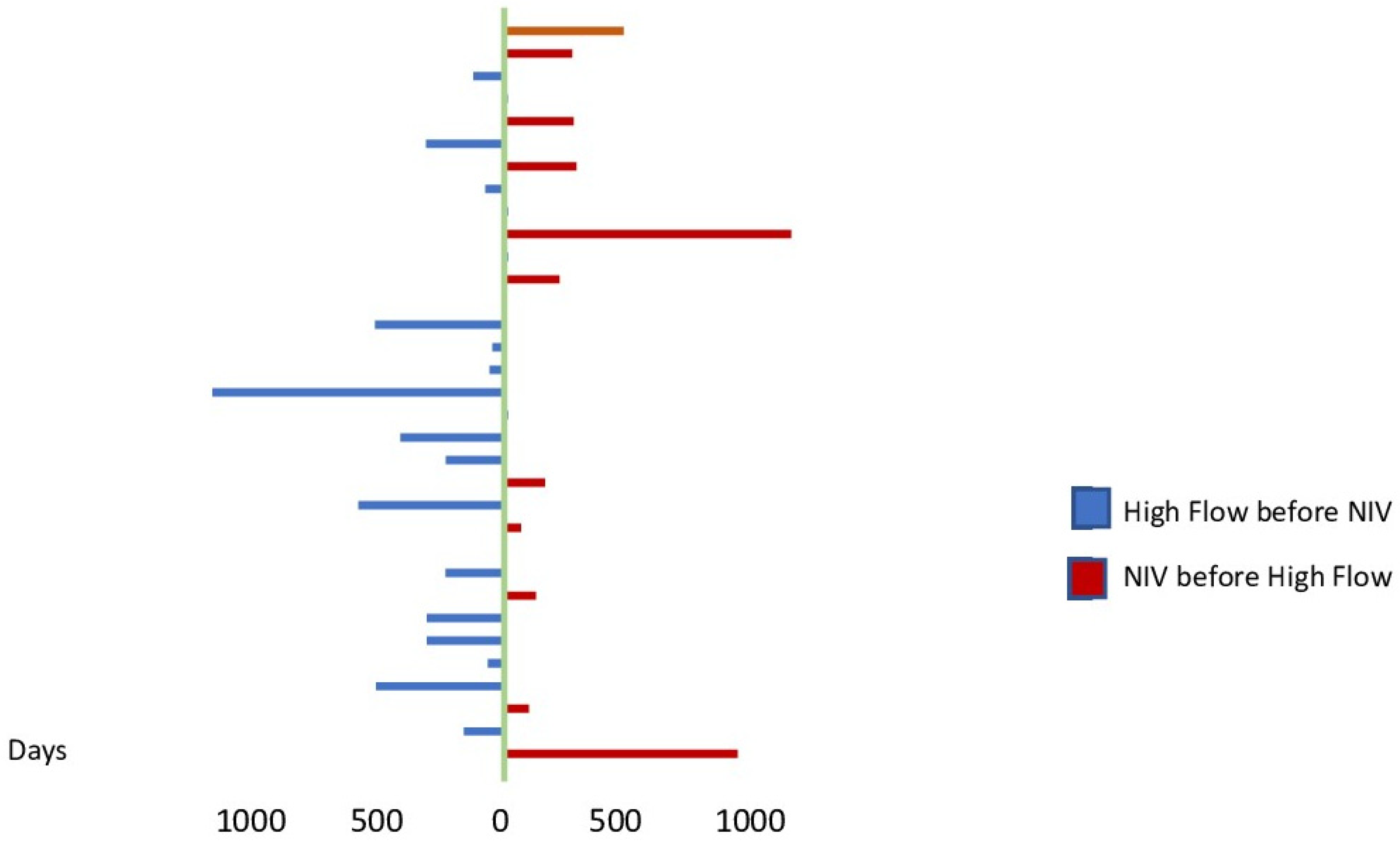
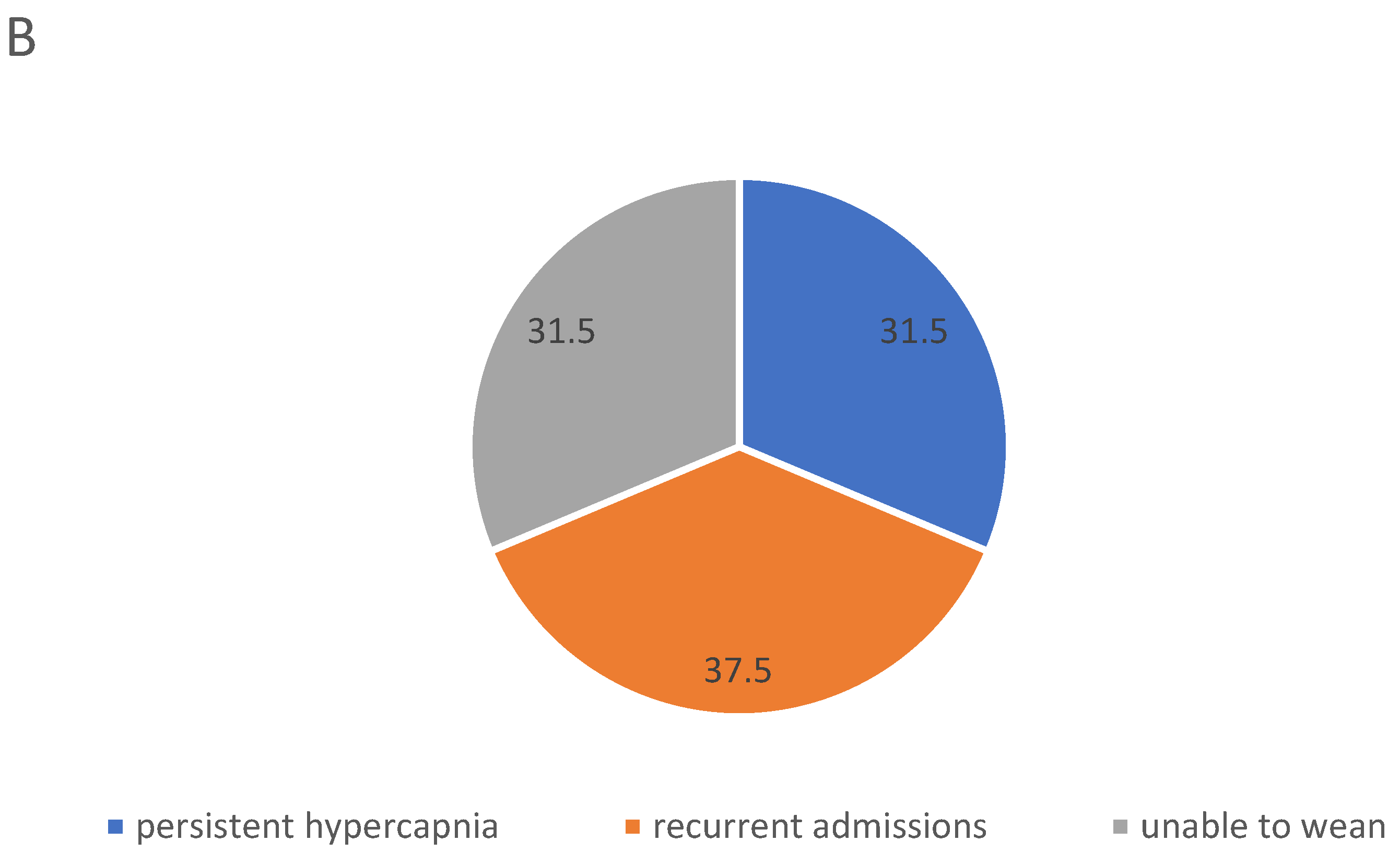
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adeloye, D.; Song, P.; Zhu, Y.; Campbell, H.; Sheikh, A.; Rudan, I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: A systematic review and modelling analysis. Lancet Respir. Med. 2022, 10, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Augusti, A.; Beasley, R.; Crinerc, G.J.; Halpind, D.; Anzuetoe, A.; Barnesf, P.; Bourbeaug, J.; Hanh, M.K.; Martinezi, F.J.; de Ocaj, M.M.; et al. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Lung Disease 2023. 2023. Available online: https://goldcopd.org/2023-gold-report-2/ (accessed on 1 May 2023).
- Sundh, J.; Ekström, M. Risk factors for developing hypoxic respiratory failure in COPD. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 2095–2100. [Google Scholar] [CrossRef] [PubMed]
- Zysman, M.; Burgel, P.; Brinchault-rabin, G.; Nesme-meyer, P.; Court-fortune, I.; Jebrak, G.; Chanez, P. Burden and Characteristics of Severe Chronic Hypoxemia in a Real-World Cohort of Subjects with COPD. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, D.A. Interpretation of ABGs. Available online: https://www.thoracic.org/professionals/clinical-resources/critical-care/clinical-education/abgs.php (accessed on 1 May 2023).
- Dreher, M.; Neuzeret, P.C.; Windisch, W.; Martens, D.; Hoheisel, G.; Gröschel, A.; Woehrle, H.; Fetsch, T.; Graml, A.; Köhnlein, T. Prevalence of chronic hypercapnia in severe chronic obstructive pulmonary disease: Data from the homevent registry. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 2377–2384. [Google Scholar] [CrossRef]
- Kotanen, P.; Brander, P.; Kreivi, H.R. The prevalence of non-invasive ventilation and long-term oxygen treatment in Helsinki University Hospital area, Finland. BMC Pulm. Med. 2022, 22, 248. [Google Scholar] [CrossRef]
- Kim, V.; Benditt, J.O.; Wise, R.A.; Sharafkhaneh, A. Oxygen therapy in chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 2008, 5, 513–518. [Google Scholar] [CrossRef]
- Csoma, B.; Vulpi, M.R.; Dragonieri, S.; Bentley, A.; Felton, T.; Lázár, Z.; Bikov, A. Hypercapnia in COPD: Causes, Consequences, and Therapy. J. Clin. Med. 2022, 11, 3180. [Google Scholar] [CrossRef]
- Gunasekaran, K.; Murthi, S.; Elango, K.; Rahi, M.S.; Thilagar, B.; Ramalingam, S.; Voruganti, D.; Paramasivam, V.K.; Kolandaivel, K.P.; Arora, A.; et al. The impact of diabetes mellitus in patients with chronic obstructive pulmonary disease (COPD) hospitalization. J. Clin. Med. 2021, 10, 235. [Google Scholar] [CrossRef]
- De Miguel Díez, J.; Morgan, J.C.; García, R.J. The association between COPD and heart failure risk: A review. Int. J. Chronic Obstr. Pulm. Dis. 2013, 8, 305–312. [Google Scholar] [CrossRef]
- Locke, B.W.; Lee, J.J.; Sundar, K.M. OSA and Chronic Respiratory Disease: Mechanisms and Epidemiology. Int. J. Environ. Res. Public Health 2022, 19, 5473. [Google Scholar] [CrossRef]
- GROUP NOTT. Continuous or Nocturnal Oxygen Therapy in Hypoxemic Chronic Obstructive Lung Disease. Ann. Intern. Med. 1980, 93, 391. Available online: http://annals.org/article.aspx?doi=10.7326/0003-4819-93-3-391 (accessed on 1 May 2023). [CrossRef] [PubMed]
- Storgaard, L.H.; Hockey, H.; Laursen, B.S.; Weinreich, U.M. Long-term effects of oxygen-enriched nasal high flow treatment in COPD with chronic hypoxemic respiratory failure. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Storgaard, L.H.; Weinreich, U.M.; Laursen, B.S. COPD Patients’ Experience of Long-Term Domestic Oxygen-Enriched Nasal High Flow Treatment: A Qualitative Study. COPD J. Chronic Obstr. Pulm. Dis. 2020, 17, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Holm, C.P.; Gantzhorn, E.K.; Weinreich, U.M.; Sonne, T.P.; Wilcke, T. LT-NIV. 2020. Available online: https://lungemedicin.dk/wp-content/uploads/2021/05/KOL-LT-NIV-DLS-2020.pdf (accessed on 1 May 2023).
- Danish Respiratory Society High Flow Hjemmebehandling. 2022. Available online: lungemedicin.dk (accessed on 1 May 2023).
- Weinreich, U.M.; Juhl, K.S.; Søby Christophersen, M.; Gundestrup, S.; Hanifa, M.A.; Jensen, K.; Andersen, F.D.; Hilberg, O.; Storgaard, L.H. The Danish respiratory society guideline for long-term high flow nasal cannula treatment, with or without supplementary oxygen. Eur. Clin. Respir. J. 2023, 10, 2178600. [Google Scholar] [CrossRef] [PubMed]
- Hansen, E.F.; Titlestad, I.L.; Gundestrup, S.; Hedsund, C.; Holm og Jost Wessels, C.P. Dansk Lungemedicinsk Selskab Guideline Kronisk Obstruktiv Lungesygdom (KOL) i Exacerbation og Non Invasiv Ventilation (NIV). DLS Guideline. 2022, pp. 1–5. Available online: https://lungemedicin.dk/kol-exacerbation-og-niv/ (accessed on 1 May 2023).
- Marsaa, K.; Gundestrup, S.; Jensen, J.U.; Lange, P.; Løkke, A.; Roberts, N.B.; Shaker, S.B.; Sørensen, A.R.; Titlestad, I.L.; Thomsen, L.H.; et al. Danish respiratory society position paper: Palliative care in patients with chronic progressive non-malignant lung diseases. Eur. Clin. Respir. J. 2018, 5, 1530029. [Google Scholar] [CrossRef]
- Putcha, N.; Drummond, M.; Wise, R.; Hansel, N. Comorbidities and Chronic Obstructive Pulmonary Disease: Prevalence, Influence on Outcomes, and Management. Semin. Respir. Crit. Care Med. 2015, 36, 575–591. [Google Scholar] [CrossRef]
- Chetty, U.; McLean, G.; Morrison, D.; Agur, K.; Guthrie, B.; Mercer, S.W. Chronic obstructive pulmonary disease and comorbidities: A large cross-sectional study in primary care. Br. J. Gen. Pract. 2017, 67, e321–e328. [Google Scholar] [CrossRef]
- Sawalha, S.; Hedman, L.; Backman, H.; Stenfors, N.; Rönmark, E.; Lundbäck, B.; Lindberg, A. The impact of comorbidities on mortality among men and women with COPD: Report from the OLIN COPD study. Ther. Adv. Respir. Dis. 2019, 13, 1753466619860058. [Google Scholar] [CrossRef]
- Ergan, B.; Oczkowski, S.; Rochwerg, B.; Carlucci, A.; Chatwin, M.; Clini, E.; Elliott, M.; Gonzalez-bermejo, J.; Hart, N.; Lujan, M.; et al. European Respiratory Society Guideline on Long-term Home Non-Invasive Ventilation for Management of Chronic Obstructive Pulmonary Disease. Eur. Respir. J. 2019, 54, 1901003. [Google Scholar] [CrossRef]
- Murphy, P.B.; Rehal, S.; Arbane, G.; Bourke, S.; Calverley, P.M.A.; Crook, A.M.; Dowson, L.; Duffy, N.; Gibson, G.J.; Hughes, P.D.; et al. Effect of Home Noninvasive Ventilation With Oxygen Therapy vs. Oxygen Therapy Alone on Hospital Readmission or Death After an Acute COPD Exacerbation. JAMA 2017, 317, 2177. [Google Scholar] [CrossRef]
- Nagata, K.; Horie, T.; Chohnabayashi, N.; Jinta, T.; Tsugitomi, R.; Shiraki, A.; Tokioka, F.; Kadowaki, T.; Watanabe, A.; Fukui, M.; et al. Home High-Flow Nasal Cannula Oxygen Therapy for Stable Hypercapnic COPD: A Randomized Clinical Trial. Am. J. Respir. Crit. Care Med. 2022, 206, 1326–1335. Available online: http://www.ncbi.nlm.nih.gov/pubmed/35771533 (accessed on 1 May 2023). [CrossRef] [PubMed]
- Bräunlich, J.; Seyfarth, H.J.; Wirtz, H. Nasal High-flow versus non-invasive ventilation in stable hypercapnic COPD: A preliminary report. Multidiscip. Respir. Med. 2015, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Crimi, C.; Nolasco, S.; Campisi, R.; Nigro, M.; Impellizzeri, P.; Cortegiani, A.; Noto, A.; Gramegna, A.; Vancheri, C.; Blasi, F. Long-Term Domiciliary High-Flow Nasal Therapy in Patients with Bronchiectasis: A Preliminary Retrospective Observational Case-Control Study. J. Clin. Med. 2022, 11, 7323. [Google Scholar] [CrossRef] [PubMed]
- Storgaard, L.H.; Hockey, H.U.; Weinreich, U.M. Development in PaCO 2 over 12 months in patients with COPD with persistent hypercapnic respiratory failure treated with high-flow nasal cannula—Post-hoc analysis from a randomised controlled trial. BMJ Open Respir. Res. 2020, 7, 10–14. [Google Scholar] [CrossRef]
- Weinreich, U.M. Domiciliary high-flow treatment in patients with COPD and chronic hypoxic failure: In whom can we reduce exacerbations and hospitalizations? PLoS ONE 2020, 14, e0227221. [Google Scholar] [CrossRef]
- Crimi, C.; Noto, A.; Princi, P.; Cuvelier, A.; Masa, J.F.; Simonds, A.; Elliott, M.W.; Wijkstra, P.; Windisch, W.; Nava, S. Domiciliary Non-invasive Ventilation in COPD: An International Survey of Indications and Practices. COPD J. Chronic Obstr. Pulm. Dis. 2016, 13, 483–490. [Google Scholar] [CrossRef]
- Steindal, S.A.; Hofsø, K.; Aagaard, H.; Mariussen, K.L.; Andresen, B.; Christensen, V.L.; Heggdal, K.; Karlsen, M.M.W.; Kvande, M.E.; Kynø, N.M.; et al. Non-invasive ventilation in the palliative care of patients with chronic obstructive pulmonary disease: A scoping review protocol. BMJ Open 2021, 11, e048344. [Google Scholar] [CrossRef]
- Duarte, J.C.; Santos, O.; Lousada, C.; Reis-Pina, P. High-flow oxygen therapy in palliative care: A reality in a near future? Pulmonology 2021, 27, 479–480. [Google Scholar] [CrossRef]
- Pennec, S.; Gaymu, J.; Riou, F.; Morand, E.; Pontone, S.; Aubry, R.; Cases, C. A majority of people would prefer to die at home, but few actually do so. Popul. Soc. 2015, 524, 1–4. [Google Scholar]
- Hall, J.; Turner, A.M.; Dretzke, J.; Moore, D.; Jowett, S. Cost-effectiveness of domiciliary non-invasive ventilation in patients with chronic obstructive pulmonary disease. Thorax 2022, 77, 976–986. [Google Scholar] [CrossRef]
- Dretzke, J.; Blissett, D.; Dave, C.; Rahul Mukherjee, M.P.; Dretzke, J.; Blissett, D.; Dave, C.; Bayliss, S.; Wu, X.; Jordan, R.; et al. The cost-effectiveness of domiciliary non-invasive ventilation in patients with end-stage chronic obstructive pulmonary disease: A systematic review and economic evaluation. Health Technol. Assess. 2015, 19, 1–246. [Google Scholar] [CrossRef] [PubMed]
- Milne, R.J.; Hockey, H.; Rea, H. Long-term air humidification therapy is cost-effective for patients with moderate or severe chronic obstructive pulmonary disease or bronchiectasis. Value Health 2014, 17, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, S.S.; Pedersen, K.M.; Weinreich, U.M.; Ehlers, L. Economic Evaluation of Community-Based Case Management of Patients Suffering From Chronic Obstructive Pulmonary Disease. Appl. Health Econ. Health Policy 2017, 15, 413–424. [Google Scholar] [CrossRef] [PubMed]



| Total Study Population | |
|---|---|
| Sex (%female) | 60.6 |
| Age (years) | 67.2 (7.1) |
| MRC-score | 4.7 (0.3) |
| FEV1, % | 28.6 (8.3) |
| BMI (kg/m2) | 29.0 (5.8) |
| Smoking status, present/former/never (%) | 33/67/0 |
| Time between initiation of long-term oxygen therapy and respiratory support (months) | 31 (12.7) |
| Number of hospitalizations twelve months before initiation of first respiratory support | 2.1 (1.6) |
| Number of hospitalizations twelve months after initiation of first respiratory support | 1.6 (0.4) |
| PaO2 at baseline (kPa) | 7.4 (0.82) |
| PaCO2 at baseline (kPa) | 7.9 (1.42) |
| HCO3 at baseline (mmol/L) | 32.5 (5.0) |
| LT-NIV (N = 16) | LT-HFNC (N = 17) | p-Value | |
|---|---|---|---|
| Sex, (%female) | 56.2 | 65.0 | 0.72 |
| Age (years) | 68.3 (7.5) | 66.8 (7.3) | 0.55 |
| MRC-score | 4.8 (0.2) | 4.5 (0.5) | 0.92 |
| FEV1% | 30.5 (8.8) | 27.1 (8.2) | 0.26 |
| BMI | 28.9 (6.5) | 28.6 (5.5) | 0.68 |
| Smoking status Present/former/never (%) | 25/75/0 | 35/65/0 | 0.23 |
| PaO2 at initiation (kPa) | 7.2 (0.9) | 7.6 (2.1) | 0.24 |
| PaCO2 at initiation(kPa) | 8.8 (0.9) | 7.1 (1.3) | 0.002 |
| St. Bicarbonate at initiation (mmol/L) | 34.4 (5.4) | 30.7 (4.0) | 0.10 |
| Number of hospitalizations twelve months before initiation of respiratory support | 2.9 (0.5) | 2.5 (0.4) | 0.13 |
| Number of hospitalizations twelve months after initiation of respiratory support | 1.6 (0.4) | 1.5 (0.4) | 0.84 |
| LT-HFNC as Second Device | LT-NIV as Second Device | |
|---|---|---|
| pO2, kPa | 6.9 (1.6) | 8.1 (1.1) |
| pCO2, kPa | 8.2 (0.7) | 7.8 (1.1) |
| St. Bicarbonate, mmol/L | 31.4 (3.4) | 32.1 (3.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weinreich, U.M.; Storgaard, L.H. A Real-Life Study of Combined Treatment with Long-Term Non-Invasive Ventilation and High Flow Nasal Cannula in Patients with End-Stage Chronic Obstructive Lung Disease. J. Clin. Med. 2023, 12, 4485. https://doi.org/10.3390/jcm12134485
Weinreich UM, Storgaard LH. A Real-Life Study of Combined Treatment with Long-Term Non-Invasive Ventilation and High Flow Nasal Cannula in Patients with End-Stage Chronic Obstructive Lung Disease. Journal of Clinical Medicine. 2023; 12(13):4485. https://doi.org/10.3390/jcm12134485
Chicago/Turabian StyleWeinreich, Ulla Møller, and Line Hust Storgaard. 2023. "A Real-Life Study of Combined Treatment with Long-Term Non-Invasive Ventilation and High Flow Nasal Cannula in Patients with End-Stage Chronic Obstructive Lung Disease" Journal of Clinical Medicine 12, no. 13: 4485. https://doi.org/10.3390/jcm12134485
APA StyleWeinreich, U. M., & Storgaard, L. H. (2023). A Real-Life Study of Combined Treatment with Long-Term Non-Invasive Ventilation and High Flow Nasal Cannula in Patients with End-Stage Chronic Obstructive Lung Disease. Journal of Clinical Medicine, 12(13), 4485. https://doi.org/10.3390/jcm12134485






