Identification of Perioperative Procedural and Hemodynamic Risk Factors for Developing Colonic Ischemia after Ruptured Infrarenal Abdominal Aortic Aneurysm Surgery: A Single-Centre Retrospective Cohort Study
Abstract
1. Introduction
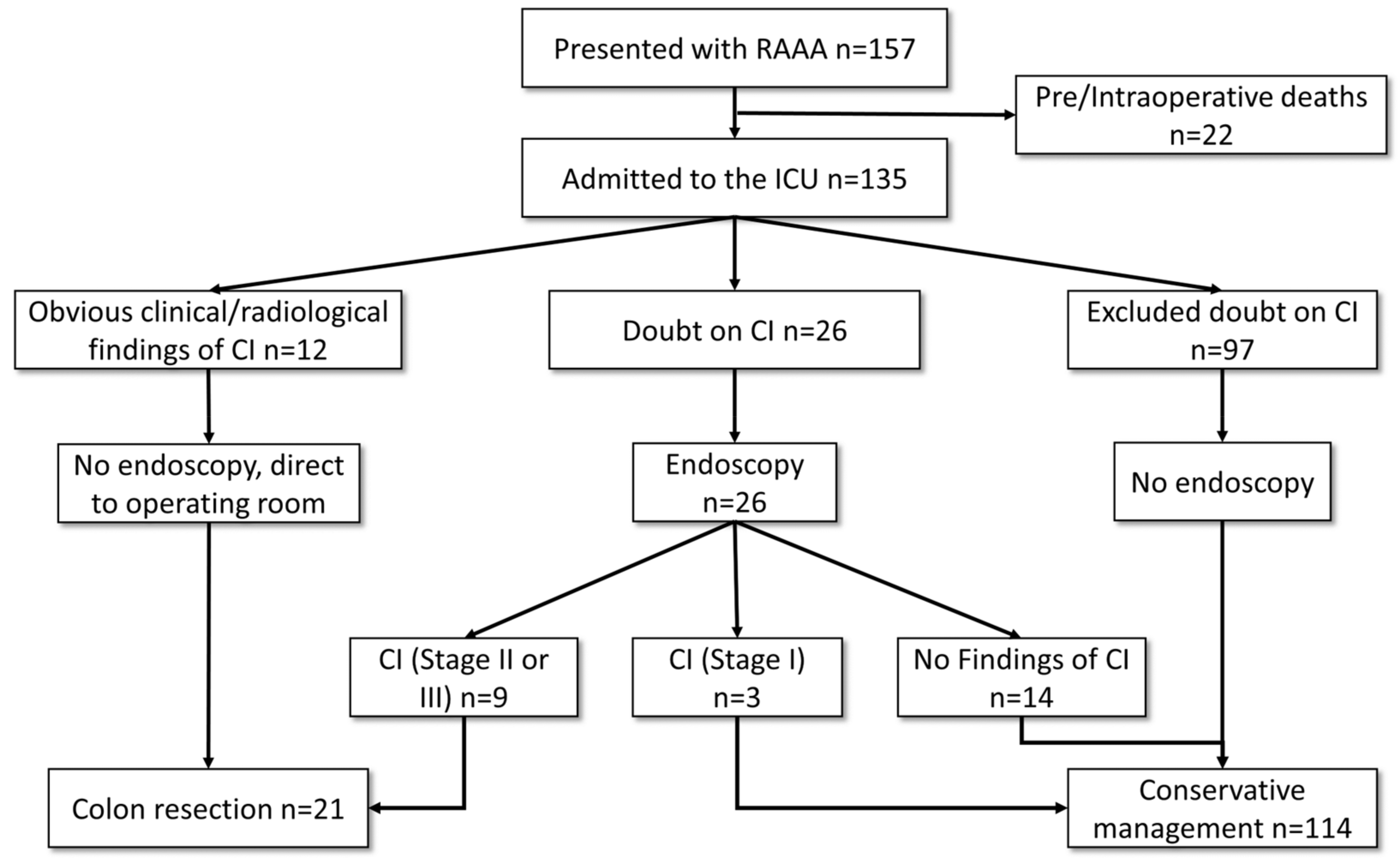
2. Materials and Methods
Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Björck, M.; Bergqvist, D.; Troëng, T. Incidence and clinical presentation of bowel ischaemia after aortoiliac surgery—2930 operations from a population-based registry in Sweden. Eur. J. Vasc. Endovasc. Surg. 1996, 12, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, T.S.; Rockman, C.B.; Riles, E.; Douglas, D.; Adelman, M.A.; Jacobowitz, G.R.; Gagne, P.J.; Nalbandian, M.N.; Cayne, N.S.; Lamparello, P.J.; et al. Ischemic complications after endovascular abdominal aortic aneurysm repair. J. Vasc. Surg. 2004, 40, 703–709; discussion 709–710. [Google Scholar] [CrossRef] [PubMed]
- Becquemin, J.-P.; Majewski, M.; Fermani, N.; Marzelle, J.; Desgrandes, P.; Allaire, E.; Roudot-Thoraval, F. Colon ischemia following abdominal aortic aneurysm repair in the era of endovascular abdominal aortic repair. J. Vasc. Surg. 2008, 47, 258–263; discussion 263. [Google Scholar] [CrossRef] [PubMed]
- Behrendt, C.-A.; Rieß, H.C.; Schwaneberg, T.; Larena-Avellaneda, A.; Kölbel, T.; Tsilimparis, N.; Spanos, K.; Debus, E.S.; Sedrakyan, A. Incidence, Predictors, and Outcomes of Colonic Ischaemia in Abdominal Aortic Aneurysm Repair. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Champagne, B.J.; Darling, R.C.; Daneshmand, M.; Kreienberg, P.B.; Lee, E.C.; Mehta, M.; Roddy, S.P.; Chang, B.B.; Paty, P.S.K.; Ozsvath, K.J.; et al. Outcome of aggressive surveillance colonoscopy in ruptured abdominal aortic aneurysm. J. Vasc. Surg. 2004, 39, 792–796. [Google Scholar] [CrossRef]
- Levison, J.A.; Halpern, V.J.; Kline, R.G.; Faust, G.R.; Cohen, J.R. Perioperative predictors of colonic ischemia after ruptured abdominal aortic aneurysm. J. Vasc. Surg. 1999, 29, 40–45; discussion 45–47. [Google Scholar] [CrossRef]
- Ultee, K.H.J.; Zettervall, S.L.; Soden, P.A.; Darling, J.; Bertges, D.J.; Verhagen, H.J.M.; Schermerhorn, M.L. Incidence of and risk factors for bowel ischemia after abdominal aortic aneurysm repair. J. Vasc. Surg. 2016, 64, 1384–1391. [Google Scholar] [CrossRef]
- Lee, M.J.; Daniels, S.L.; Drake, T.M.; Adam, I.J. Risk factors for ischaemic colitis after surgery for abdominal aortic aneurysm: A systematic review and observational meta-analysis. Int. J. Color. Dis. 2016, 31, 1273–1281. [Google Scholar] [CrossRef]
- Djavani, K.; Wanhainen, A.; Valtysson, J.; Björck, M. Colonic ischaemia and intra-abdominal hypertension following open repair of ruptured abdominal aortic aneurysm. Br. J. Surg. 2009, 96, 621–627. [Google Scholar] [CrossRef]
- Meissner, M.H.; Johansen, K.H. Colon Infarction After Ruptured Abdominal Aortic Aneurysm. Arch. Surg. 1992, 127, 979–985. [Google Scholar] [CrossRef]
- Jalalzadeh, H.; van Schaik, T.G.; Duin, J.J.; Indrakusuma, R.; van Beek, S.C.; Vahl, A.C.; Wisselink, W.; Balm, R.; Koelemay, M.J.W. The Value of Sigmoidoscopy to Detect Colonic Ischaemia After Ruptured Abdominal Aortic Aneurysm Repair. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 229–237. [Google Scholar] [CrossRef]
- Willemsen, S.I.; ten Berge, M.G.; van Eps, R.G.S.; Veger, H.T.C.; van Overhagen, H.; van-Dijk, L.C.; Putter, H.; Wever, J.J. Nationwide Study to Predict Colonic Ischemia after Abdominal Aortic Aneurysm Repair in The Netherlands. Ann. Vasc. Surg. 2021, 73, 407–416. [Google Scholar] [CrossRef]
- Omran, S.; Gröger, S.; Schawe, L.; Berger, C.; Konietschke, F.; Treskatsch, S.; Greiner, A.; Angermair, S. Preoperative and ICU Scoring Models for Predicting the In-Hospital Mortality of Patients With Ruptured Abdominal Aortic Aneurysms. J. Cardiothorac. Vasc. Anesth. 2021, 35, 3700–3707. [Google Scholar] [CrossRef]
- Moszkowicz, D.; Mariani, A.; Trésallet, C.; Menegaux, F. Ischemic colitis: The ABCs of diagnosis and surgical management. J. Visc. Surg. 2013, 150, 19–28. [Google Scholar] [CrossRef]
- Fukui, S.; Higashio, K.; Murao, S.; Endo, A.; Akira, T.; Yamakawa, K. Optimal target blood pressure in critically ill adult patients with vasodilatory shock: A protocol for a systematic review and meta-analysis. BMJ Open 2021, 11, e048512. [Google Scholar] [CrossRef]
- Marshall, J.C. Choosing the Best Blood Pressure Target for Vasopressor Therapy. JAMA 2020, 323, 931–933. [Google Scholar] [CrossRef]
- Piotrowski, J.J.; Ripepi, A.J.; Yuhas, J.P.; Alexander, J.J.; Brandt, C.P. Colonic ischemia: The Achilles heel of ruptured aortic aneurysm repair. Am. Surg. 1996, 62, 557–560; discussion 560–561. [Google Scholar]
- Lewejohann, J.C.; Hansen, M.; Braasch, H.; Zimmermann, C.; Muhl, E.; Keck, T. Appropriate fluid resuscitation of septic shock patients pretreated with high doses of catecholamines. Intensive Care Med. Exp. 2015, 3, A225. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Fluid Resuscitation for Combat Casualties; Pope, A.; French, G.; Longnecker, D.E. (Eds.) Fluid Resuscitation: State of the Science for Treating Combat Casualties and Civilian Injuries: Experience With and Complications of Fluid Resuscitation; National Academies Press (US): Washington, DC, USA, 1999.
- Sautner, T.; Wessely, C.; Riegler, M.; Sedivy, R.; Götzinger, P.; Losert, U.; Roth, E.; Jakesz, R.; Függer, R. Early effects of catecholamine therapy on mucosal integrity, intestinal blood flow, and oxygen metabolism in porcine endotoxin shock. Ann. Surg. 1998, 228, 239–248. [Google Scholar] [CrossRef]
- Hasibeder, W. Gastrointestinal microcirculation: Still a mystery? Br. J. Anaesth. 2010, 105, 393–396. [Google Scholar] [CrossRef]
- Gelman, S.; Mushlin, P.S. Catecholamine-induced changes in the splanchnic circulation affecting systemic hemodynamics. Anesthesiology 2004, 100, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Bruder, L.; Schawe, L.; Gebauer, B.; Frese, J.P.; de Bucourt, M.; Beyer, K.; Pratschke, J.; Greiner, A.; Omran, S. Evaluation of Open Surgical and Endovascular Treatment Options for Visceral Artery Erosions after Pancreatitis and Pancreatic Surgery. Curr. Oncol. 2022, 29, 2472–2482. [Google Scholar] [CrossRef] [PubMed]
- Williamson, J.S.; Ambler, G.K.; Twine, C.P.; Williams, I.M.; Williams, G.L. Elective Repair of Abdominal Aortic Aneurysm and the Risk of Colonic Ischaemia: Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 31–39. [Google Scholar] [CrossRef]
- Lee, K.B.; Lu, J.; Macsata, R.A.; Patel, D.; Yang, A.; Ricotta, J.J.; Amdur, R.L.; Sidawy, A.N.; Nguyen, B.-N. Inferior mesenteric artery replantation does not decrease the risk of ischemic colitis after open infrarenal abdominal aortic aneurysm repair. J. Vasc. Surg. 2019, 69, 1825–1830. [Google Scholar] [CrossRef] [PubMed]
- Senekowitsch, C.; Assadian, A.; Assadian, O.; Hartleb, H.; Ptakovsky, H.; Hagmüller, G.W. Replanting the inferior mesentery artery during infrarenal aortic aneurysm repair: Influence on postoperative colon ischemia. J. Vasc. Surg. 2006, 43, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.; Marotta, M.; Scordi-Bello, I.; Tammaro, Y.; Marin, M.; Divino, C. Ischemic Colitis after Endovascular Aortoiliac Aneurysm Repair: A 10-Year Retrospective Study. Arch. Surg. 2009, 144, 900–903. [Google Scholar] [CrossRef]
- Gurakar, M.; Locham, S.; Alshaikh, H.N.; Malas, M.B. Risk factors and outcomes for bowel ischemia after open and endovascular abdominal aortic aneurysm repair. J. Vasc. Surg. 2019, 70, 869–881. [Google Scholar] [CrossRef]
- Omran, S.; Müller, V.; Schawe, L.; Bürger, M.; Kapahnke, S.; Bruder, L.; Haidar, H.; Konietschke, F.; Greiner, A. Outcomes of Endurant II Stent Graft According to Anatomic Severity Grade Score. J. Endovasc. Ther. 2022, 11, 7420. [Google Scholar] [CrossRef]
- Omran, S.; Konietschke, F.; Mueller, V.; de Bucourt, M.; Frese, J.P.; Greiner, A. Development of a Novel Scoring Model to Estimate the Severity Grade of Mesenteric Artery Stenosis. J. Clin. Med. 2022, 11, 7420. [Google Scholar] [CrossRef]
- Al-Diery, H.; Phillips, A.; Evennett, N.; Pandanaboyana, S.; Gilham, M.; Windsor, J.A. The Pathogenesis of Nonocclusive Mesenteric Ischemia: Implications for Research and Clinical Practice. J. Intensive Care Med. 2019, 34, 771–781. [Google Scholar] [CrossRef]
- Sun, J.; Yuan, J.; Li, B. SBP Is Superior to MAP to Reflect Tissue Perfusion and Hemodynamic Abnormality Perioperatively. Front. Physiol. 2021, 12, 705558. [Google Scholar] [CrossRef]
- Futier, E.; Lefrant, J.-Y.; Guinot, P.-G.; Godet, T.; Lorne, E.; Cuvillon, P.; Bertran, S.; Leone, M.; Pastene, B.; Piriou, V.; et al. Effect of Individualized vs Standard Blood Pressure Management Strategies on Postoperative Organ Dysfunction among High-Risk Patients Undergoing Major Surgery: A Randomized Clinical Trial. JAMA 2017, 318, 1346–1357. [Google Scholar] [CrossRef]
- Di Giantomasso, D.; May, C.N.; Bellomo, R. Norepinephrine and vital organ blood flow during experimental hyperdynamic sepsis. Intensive Care Med. 2003, 29, 1774–1781. [Google Scholar] [CrossRef]
- Hiltebrand, L.B.; Koepfli, E.; Kimberger, O.; Sigurdsson, G.H.; Brandt, S. Hypotension during fluid-restricted abdominal surgery: Effects of norepinephrine treatment on regional and microcirculatory blood flow in the intestinal tract. Anesthesiology 2011, 114, 557–564. [Google Scholar] [CrossRef]
- Brennan, C.A.; Osei-Bonsu, P.; McClenaghan, R.E.; Nassar, A.; Forget, P.; Kaye, C.; Ramsay, G. Vasoactive agents in acute mesenteric ischaemia in critical care. A systematic review. F1000Research 2021, 10, 453. [Google Scholar] [CrossRef]
- Hajjar, L.A.; Vincent, J.L.; Barbosa Gomes Galas, F.R.; Rhodes, A.; Landoni, G.; Osawa, E.A.; Melo, R.R.; Sundin, M.R.; Grande, S.M.; Gaiotto, F.A.; et al. Vasopressin versus Norepinephrine in Patients with Vasoplegic Shock after Cardiac Surgery: The VANCS Randomized Controlled Trial. Anesthesiology 2017, 126, 85–93. [Google Scholar] [CrossRef]




| Characteristics | Total | CI | Non-CI | OR (95% Confidence Interval) | Univariate Analysis (p) |
|---|---|---|---|---|---|
| Number | 135 (100) | 24 (18) | 111 (82) | ||
| Demographics | |||||
| Age (y) | 75 (IQR 68–81) | 79 (IQR 72–81) | 74 (IQR 67–81) | 0.97 (0.92–1.02) | 0.220 |
| Male | 111 (82) | 22 (92) | 89 (80) | 2.7 (0.6–12.4) | 0.246 |
| Medical history | |||||
| Coronary artery disease | 28 (21) | 9 (38) | 19 (17) | 2.9 (1.1–7.6) | 0.026 * |
| Diabetes mellitus | 25 (19) | 6 (25) | 19 (17) | 1.6 (0.6–4.6) | 0.389 |
| Hypertension | 103 (76) | 19 (79) | 84 (76) | 1.2 (0.4–3.6) | 0.715 |
| Hyperlipoproteinemia | 19 (14) | 2 (8) | 17 (15) | 0.5 (0.1–2.3) | 0.525 |
| COPD | 34 (25) | 5 (21) | 29 (26) | 0.7 (0.3–2.2) | 0.588 |
| Renal insufficiency | 46 (34) | 9 (38) | 37 (33) | 1.2 (0.5 –3.0) | 0.696 |
| Smoking | 41 (30) | 9 (38) | 32 (29) | 1.5 (0.6–3.7) | 0.402 |
| Peripheral arterial disease | 15 (11) | 4 (17) | 11 (10) | 1.8 (0.5–6.3) | 0.307 |
| Malignancy | 22 (16) | 4 (17) | 18 (16) | 1.0 (0.3–3.4) | 1 |
| Preoperative status of IMA | |||||
| Patent | 68 (50) | 8 (33) | 60 (54) | 2.4 (0.9–5.9) | 0.066 |
| Occluded | 67 (50) | 16 (67) | 51 (46) | 2.4 (0.9–5.9) | 0.066 |
| Postoperative status of patent IMA | |||||
| IMA ligation | 37 (27) | 6 (25) | 31 (28) | 0.5 (0.1–1.9) | 0.406 |
| IMA replantation | 3 (2) | 1 (4) | 2 (2) | 2.4 (0.2–27.2) | 0.447 |
| IMA Overstenting | 28 (21) | 1 (4) | 27 (24) | 0.1 (0.02–1.1) | 0.045 |
| Status of internal iliac arteries | |||||
| Patent | 116 (86) | 18 (75) | 98 (88) | 0.4 (0.1–1.2) | 0.107 |
| Unilateral IIA occlusion | 11 (8) | 3 (13) | 8 (7) | 1.8 (0.5–7.5) | 0.412 |
| Bilateral IIA occlusion | 8 (6) | 3 (13) | 5 (5) | 3.0 (0.7–13.7) | 0.150 |
| Uni-/Bilateral IIA occlusion | 19 (14) | 6 (25) | 13 (12) | 2.5 (0.8–7.5) | 0.107 |
| Characteristics | Total | CI | Non-CI | OR (95% Confidence Interval) | p |
|---|---|---|---|---|---|
| Number | 135 (100) | 24 (18) | 111 (82) | ||
| Univariate analysis | |||||
| Preoperative Variables | |||||
| Coronary artery disease | 28 (21) | 9 (38) | 19 (17) | 2.9 (1.1–7.6) | 0.026 * |
| Preoperative hemodynamic instability | 54 (40) | 17 (71) | 37 (33) | 4.9 (1.9–12.7) | <0.001 * |
| Preoperative cardiopulmonary resuscitation | 11 (8) | 6 (25) | 5 (5) | 7.0 (2.0–25.6) | 0.004 * |
| Preoperative loss of consciousness | 27 (20) | 10 (42) | 17 (15) | 3.9 (1.5–10.3) | 0.009 * |
| Age > 76 y | 61 (46) | 14 (58) | 47 (43) | 1.8 (0.8–4.5) | 0.153 |
| Maximum aortic diameter in mm | 78 ± 21 | 85 ± 16 | 77 ± 21 | 0.98 (0.96–1.0) | 0.129 |
| Intraoperative Variables | |||||
| Open aortic repair | 98 (73) | 22 (92) | 76 (69) | 5.1 (1.1–22.7) | 0.021 * |
| PRBCs ≥ 5 units | 71 (53) | 18 (75) | 53 (48) | 3.3 (1.2–8.9) | 0.015 * |
| Suprarenal clamping | 32 (24) | 6 (25) | 26 (23) | 1.1 (0.4–3.0) | 0.869 |
| Operating time ≥ 200 min | 67 (50) | 18 (75) | 49 (44) | 3.8 (1.4–10.3) | 0.006 * |
| Variables from POD1 | |||||
| NE > 64 µg/kg | 45 (33) | 20 (83) | 25 (23) | 17.2 (5.4–55.0) | <0.001 * |
| PH < 7.3 | 56 (42) | 17 (71) | 39 (35) | 4.5 (1.7–11.7) | 0.001 * |
| arterial lactate > 5 mmol/L | 49 (36) | 19 (79) | 30 (27) | 10.3 (3.5–29.9) | <0.001 * |
| MAP | 79 ± 9 | 79 ± 8 | 79 ± 9 | 0.99 (0.95–1.05) | 0.977 |
| MAP < 65 mmHg | 10 (7) | 2 (8) | 8 (7) | 1.17 (0.23–5.89) | 1.0 |
| HR | 85 ± 14 | 87 ± 14 | 85 ± 15 | 0.99 (0.96–1.02) | 0.495 |
| Hemoglobin < 9 g/dL | 27 (20) | 8 (33) | 19 (17) | 2.4 (0.9–6.3) | 0.091 |
| FT ≥ 5 L | 40 (30) | 10 (42) | 30 (28) | 1.9 (0.8–4.7) | 0.154 |
| Creatinine > 190 mmol | 12 (9) | 3 (13) | 9 (8) | 1.6 (0.4–6.4) | 0.447 |
| Multivariable analysis | RD (95% confidence interval) | ||||
| NE > 64 µg/kg | 0.40 (0.25–0.55) | <0.001 * | |||
| Operating time ≥ 200 min | 0.18 (0.05–0.31) | 0.042 * | |||
| PH < 7.3 | 0.21 (0.07–0.35) | 0.019 * |
| Total | CI | Non-CI | p | |
|---|---|---|---|---|
| Complications | ||||
| Overall | 76 (56) | 16 (67) | 60 (54) | 0.259 |
| Respiratory | 59 (44) | 10 (42) | 49 (44) | 0.824 |
| Cardiac | 26 (19) | 7 (29) | 19 (17) | 0.251 |
| Abdominal compartment syndrome | 10 (7) | 4 (17) | 6 (5) | 0.077 |
| Renal failure | 40 (30) | 10 (42) | 30 (27) | 0.154 |
| Multiple organ failure | 14 (10) | 6 (25) | 8 (7) | 0.019 * |
| Sepsis | 18 (13) | 4 (17) | 14 (13) | 0.527 |
| Outcome | ||||
| ICU length of stay (days) | 7 (IQR 3–16) | 15 (IQR 6–16) | 6 (IQR 2–15) | 0.018 * |
| Hospital length of stay (days) | 12 (IQR 9–22) | 21 (IQR 10–23) | 12 (IQR 9–20) | 0.174 |
| 30-day mortality | 23 (17) | 8 (33) | 15 (14) | 0.032 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omran, S.; Schawe, L.; Konietschke, F.; Angermair, S.; Weixler, B.; Treskatsch, S.; Greiner, A.; Berger, C. Identification of Perioperative Procedural and Hemodynamic Risk Factors for Developing Colonic Ischemia after Ruptured Infrarenal Abdominal Aortic Aneurysm Surgery: A Single-Centre Retrospective Cohort Study. J. Clin. Med. 2023, 12, 4159. https://doi.org/10.3390/jcm12124159
Omran S, Schawe L, Konietschke F, Angermair S, Weixler B, Treskatsch S, Greiner A, Berger C. Identification of Perioperative Procedural and Hemodynamic Risk Factors for Developing Colonic Ischemia after Ruptured Infrarenal Abdominal Aortic Aneurysm Surgery: A Single-Centre Retrospective Cohort Study. Journal of Clinical Medicine. 2023; 12(12):4159. https://doi.org/10.3390/jcm12124159
Chicago/Turabian StyleOmran, Safwan, Larissa Schawe, Frank Konietschke, Stefan Angermair, Benjamin Weixler, Sascha Treskatsch, Andreas Greiner, and Christian Berger. 2023. "Identification of Perioperative Procedural and Hemodynamic Risk Factors for Developing Colonic Ischemia after Ruptured Infrarenal Abdominal Aortic Aneurysm Surgery: A Single-Centre Retrospective Cohort Study" Journal of Clinical Medicine 12, no. 12: 4159. https://doi.org/10.3390/jcm12124159
APA StyleOmran, S., Schawe, L., Konietschke, F., Angermair, S., Weixler, B., Treskatsch, S., Greiner, A., & Berger, C. (2023). Identification of Perioperative Procedural and Hemodynamic Risk Factors for Developing Colonic Ischemia after Ruptured Infrarenal Abdominal Aortic Aneurysm Surgery: A Single-Centre Retrospective Cohort Study. Journal of Clinical Medicine, 12(12), 4159. https://doi.org/10.3390/jcm12124159






