Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches
Abstract
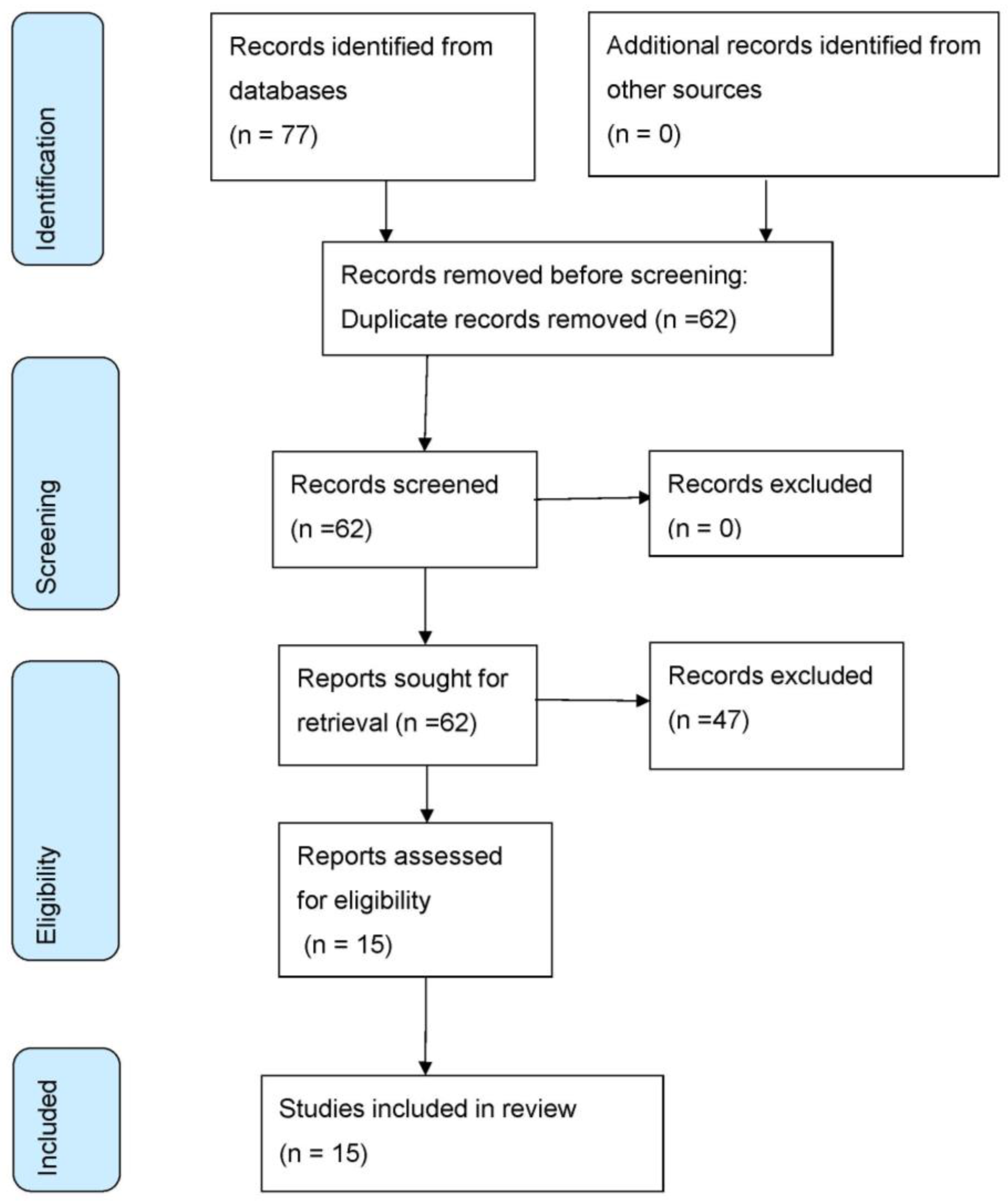
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
- -
- Studies published in Spanish or English.
- -
- Studies published between 2010 and the present (June 2022).
- -
- Clinical trial studies.
- -
- Studies conducted in patients diagnosed with temporomandibular disorders who have undergone treatment.
- -
- Duplicated studies.
- -
- Studies in which no type of treatment was studied.
2.4. Study Selection
2.5. Methodological Quality Analysis
3. Results
Methodological Quality Assessment
4. Discussion
4.1. Clinical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lomas, J.; Gurgenci, T.; Jackson, C.; Campbell, D. Temporomandibular dysfunction. Aust. J. Gen. Pract. 2018, 47, 212–215. [Google Scholar] [CrossRef]
- Ingawalé, S.; Goswami, T. Temporomandibular joint: Disorders, treatments, and biomechanics. Ann. Biomed. Eng. 2009, 37, 976–996. [Google Scholar] [CrossRef] [PubMed]
- Oral, K.; Bal Küçük, B.; Ebeoğlu, B.; Dinçer, S. Etiology of temporomandibular disorder pain. AGRI 2009, 21, 89–94. [Google Scholar]
- Peñón Vivas, P.Á.; Grau León, I.B.; Sarracent Pérez, H. Síndrome de disfunción temporomandibular y factores asociados. Rev. Habanera Cienc. Médicas 2011, 10, 448–457. [Google Scholar]
- Pasinato, F.; Souza, J.A.; Corrêa, E.C.R.; Silva, A.M.T. Temporomandibular disorder and generalized joint hypermobility: Application of diagnostic criteria. Braz. J. Otorhinolaryngol. 2011, 77, 418–425. [Google Scholar] [CrossRef]
- Liarte Pedreño, A.; Escobar Velando, G.; Rodríguez Saura, P.; Jiménez Cervantes, A. La fisioterapia en el tratamiento interdisciplinar de la disfunción de la articulación temporomandibular. Fisioterapia 2002, 24, 2–9. [Google Scholar]
- Peck, C.C.; Goulet, J.P.; Lobbezoo, F.; Schiffman, E.F.; Alstergren, P.; Anderson, G.C.; De Leeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R.; et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2–23. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Truelove, E.; Look, J.; Anderson, G.; Ceusters, W.; Smith, B. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician 2015, 91, 378–386. [Google Scholar]
- Wieckiewicz, M.; Boening, K.; Wiland, P.; Shiau, Y.Y.; Paradowska-Stolarz, A. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J. Headache Pain 2015, 16, 106. [Google Scholar] [CrossRef]
- Liébana, S.; Codina, B. Tratamiento fisioterápico en la disfunción temporomandibular. Fisioterapia 2011, 33, 203–209. [Google Scholar] [CrossRef]
- Hutton, B. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Med. Clín. 2016, 147, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Conesa, A.; Suárez-Serrano, C.M.; Catalan, D.; López-López, J. The Spanish translation and adaptation of the Pedro scale. Physiotherapy 2015, 101, E463–E464. [Google Scholar] [CrossRef]
- Brochado, F.T.; Jesus, L.H.; Carrard, V.C.; Freddo, A.L.; Chaves, K.D.; Martins, M.D. Comparative effectiveness of photobiomodulation and manual therapy alone or combined in TMD patients: A randomized clinical trial. Braz. Oral Res. 2018, 32, 50. [Google Scholar] [CrossRef]
- Delgado de la Serna, P.; Plaza-Manzano, G.; Cleland, J.; Fernández-de-Las-Peñas, C.; Martín-Casas, P.; Díaz-Arribas, M.J. Effects of Cervico-Mandibular Manual Therapy in Patients with Temporomandibular Pain Disorders and Associated Somatic Tinnitus: A Randomized Clinical Trial. Pain Med. Malden Mass. 2020, 21, 613–624. [Google Scholar] [CrossRef]
- Abboud, W.A.; Yarom, N.; Yahalom, R.; Joachim, M.; Reiter, S.; Koren, O.; Elishoov, H. Comparison of two physiotherapy programmes for rehabilitation after temporomandibular joint arthroscopy. Int. J. Oral Maxillofac. Surg. 2018, 47, 755–761. [Google Scholar] [CrossRef]
- Calixtre, L.B.; Grüninger, B.L.; Haik, M.N.; Alburquerque-Sendín, F.; Oliveira, A.B. Effects of cervical mobilization and exercise on pain, movement and function in subjects with temporomandibular disorders: A single group pre- post test. J. Appl. Oral Sci. 2016, 24, 188–197. [Google Scholar] [CrossRef]
- Craane, B.; Dijkstra, P.U.; Stappaerts, K.; De Laat, A. Randomized controlled trial on physical therapy for TMJ closed lock. J. Dent. Res. 2012, 91, 364–369. [Google Scholar] [CrossRef]
- Madani, A.S.; Mirmortazavi, A. Comparison of three treatment options for painful temporomandibular joint clicking. J. Oral Sci. 2011, 53, 349–354. [Google Scholar] [CrossRef]
- Dalewski, B.; Kamińska, A.; Szydłowski, M.; Kozak, M.; Sobolewska, E. Comparison of Early Effectiveness of Three Different Intervention Methods in Treatment of Temporomandibular Joint Disorders by Ultrashort Wave and Extracorporeal Shock Wave: A Comparative Study. Med. Sci. Monit. 2020, 26, e923461. [Google Scholar]
- Dib-Zakkour, J.; Flores-Fraile, J.; Montero-Martin, J.; Dib-Zakkour, S.; Dib-Zaitun, I. Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders. Medicina 2022, 58, 256. [Google Scholar] [CrossRef]
- Nambi, G.; Abdelbasset, W.K.; Soliman, G.S.; Alessi, A.A.; Alsalem, I.N.; Ali, Z.A. Clinical and functional efficacy of gallium-arsenide super pulsed laser therapy on temporo mandibular joint pain with orofacial myalgia following healed unilateral cervicofacial burn—A randomized trial. Burns 2022, 48, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Chellappa, D.; Thirupathy, M. Comparative efficacy of low-Level laser and TENS in the symptomatic relief of temporomandibular joint disorders: A randomized clinical trial. Indian J. Dent. Res. 2020, 31, 42–47. [Google Scholar] [CrossRef]
- Li, W.; Wu, J.; Catalá, F.; Moher, D. Patients with Chronic Orofacial Pain: A Randomized, Controlled Clinical Trial. Pain Res. Manag. 2019, 2019, 7954291. [Google Scholar] [CrossRef]
- Jo, J.H.; Jang, Y.; Chung, G.; Chung, J.W.; Park, J.W. Long-term efficacy and patient satisfaction of pulsed radiofrequency therapy in temporomandibular disorders: A randomized controlled trial. Medicine 2021, 100, e28441. [Google Scholar] [CrossRef] [PubMed]
- Brandão, R.A.F.S.; Mendes, C.M.C. Temporomandibular Joint Pain With Orofacial Myalgia Following Post Healed Unilateral Cervicofacial Burn. Acupunct. Electro-Ther. Res. 2021, 46, 123–134. [Google Scholar]
- Urbański, P.; Trybulec, B.; Pihut, M. The Application of Manual Techniques in Masticatory Muscles Relaxation as Adjunctive Therapy in the Treatment of Temporomandibular Joint Disorders. Int. J. Environ. Res. Public Health 2021, 18, 12970. [Google Scholar] [CrossRef]
- Shandilya, S.; Mohanty, S.; Sharma, P.; Chaudhary, Z.; Kohli, S.; Kumar, R.D. Effect of Preoperative Intramuscular Injection of Botulinum Toxin A on Pain and Mouth Opening After Surgical Intervention in Temporomandibular Joint Ankylosis Cases: A Controlled Clinical Trial. J. Oral Maxillofac. Surg. 2020, 78, 916–926. [Google Scholar] [CrossRef]
- Şenbursa, G.; Baltaci, G.; Atay, Ö.A. The effectiveness of manual therapy in supraspinatus tendinopathy. Acta Orthop. Traumatol. Turc. 2011, 45, 162–167. [Google Scholar] [CrossRef]
- Nejati, P.; Safarcherati, A.; Karimi, F. Effectiveness of Exercise Therapy and Manipulation on Sacroiliac Joint Dysfunction: A Randomized Controlled Trial. Pain Physician 2019, 22, 53–61. [Google Scholar] [CrossRef]
- Wójcik, M.; Goździewicz, T.; Hudáková, Z.; Siatkowski, I. Endometriosis and the Temporomandibular Joint—Preliminary Observations. J. Clin. Med. 2023, 12, 2862. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, J.; Malo-Urriés, M.; Corral-de-Toro, J.; López-de-Celis, C.; Lucha-López, M.O.; Tricás-Moreno, J.M.; Lorente, A.I.; Hidalgo-García, C. Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 6601. [Google Scholar] [CrossRef] [PubMed]
- Ziaeifar, M.; Arab, A.M.; Mosallanezhad, Z.; Nourbakhsh, M.R. Dry needling versus trigger point compression of the upper trapezius: A randomized clinical trial with two-week and three-month follow-up. J. Man. Manip. Ther. 2019, 27, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Lo, M.Y.; Wu, C.H.; Luh, J.J.; Wang, T.G.; Fu, L.C.; Lin, J.G.; Lai, J.S. The effect of electroacupuncture merged with rehabilitation for frozen shoulder syndrome: A single-blind randomized sham-acupuncture controlled study. J. Formos. Med. Assoc. 2020, 119 Pt 1, 81–88. [Google Scholar] [CrossRef]
- Manfredini, D.; Guarda-Nardini, L.; Winocur, E.; Piccotti, F.; Ahlberg, J.; Lobbezoo, F. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2011, 112, 453–462. [Google Scholar] [CrossRef]
- Van Grootel, R.J.; Buchner, R.; Wismeijer, D.; van der Glas, H.W. Towards an optimal therapy strategy for myogenous TMD, physiotherapy compared with occlusal splint therapy in an RCT with therapy-and-patient-specific treatment durations. BMC Musculoskelet. Disord. 2017, 18, 76. [Google Scholar] [CrossRef]
- Kucukguven, A.; Demiryurek, M.D.; Vargel, I. Temporomandibular joint innervation: Anatomical study and clinical implications. Ann. Anat. 2022, 240, 151882. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; De Almeida, A.M.; Manfredini, D. Arthrocentesis of the Temporomandibular Joint: Systematic Review and Clinical Implications of Research Findings. J. Oral Facial Pain Headache 2021, 35, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016, 147, 438–445. [Google Scholar] [CrossRef] [PubMed]
| Data Bases | Searching Strategies |
|---|---|
| PubMed | Temporomandibular joint AND physiotherapy Temporomandibular joint disorders AND physiotherapy Temporomandibular dysfunction syndrome AND physiotherapy |
| ScienceDirect | Temporomandibular joint AND physiotherapy Temporomandibular joint disorders AND physiotherapy Temporomandibular dysfunction syndrome AND physiotherapy |
| Dialnet | Articulation temporomandibular AND physiotherapy Trastornos de la articulación temporomandibular AND fisioterapia Síndrome de disfunción temporomandibular AND fisioterapia |
| PEDro | Temporomandibular joint AND physiotherapy Temporomandibular joint disorders AND physiotherapy Temporomandibular dysfunction syndrome AND physiotherapy |
| Study | Objective | Diagnosed Disorder [8] | Sample/Age | Intervention | Duration | Assessment Tool | Results |
|---|---|---|---|---|---|---|---|
| Brochado et al., 2018 [14] | To investigate the efficacy of manual therapy and photobiomodulation, separately or in combination, with regard to pain intensity, mandibular movements, psychosocial aspects, and anxiety in patients with TMDs. | TMD (Myogenic and arthrogenic) | 51 patients 21 years old or more. | G1: 18 patients. Photobiomodulation application. G2: 16 patients. Manual therapy G3: 17 patients. Both techniques. | 12 sessions. Duration unspecified. | Visual Analog Scale (VAS). Beck Anxiety Inventory (BAI). Research Diagnostic Criteria for TMJ Disorders (RDC/TMD). | All protocols demonstrated changes in the reduction of pain (p < 0.001) and anxiety symptoms (p ≤ 0.05). The combination of both methods does not prove to be more effective than both separately. |
| Delgado de la Serna et al., 2020 [15] | To investigate the effects of adding cervical-mandibular manual therapies to an educational and exercise program in individuals with tinnitus associated with TMDs. | TMD with associated tinnitus | 61 patients. 18–65 years. | Cranio-cervical treatment, TMJ treatment, self-massages exercises and patient education. | Six 30 min sessions during a month. | Intensity of TMJ pain. Tinnitus disability inventory. Disability related to TMJ disorders. Beck depression inventory (BDI-II) Mandibular joint range. | Cervico-mandibular manual therapies in combination with exercise/education produced better results than the application of exercise/education alone in people with TMJ-attributed tinnitus (p < 0.001). |
| Abboud et al., 2018 [16] | To compare two physiotherapy programs, progressive versus immediate, after TMJ arthroscopy. | TMD (TMJ arthroscopy) | 137 patients Mean age 27.5 gradual group mean age 28.5 immediate group | G1: 68 patients gradual exercise program. G2: 69 patients immediate exercise program. | 10 months post-op rehabilitation. Sessions unspecified. | VAS Maximum Mandibular Opening Range (MMO) | Group 2 showed better results, in terms of pain and MMO, compared to group 1. |
| Calixtre et al., 2016 [17] | To investigate the effects of a program based on cervical mobilization and therapeutic exercise in patients with TMDs. | TMD | 12 patients. Mean age = 22.08 (SD ± 2.23) | Subjects were evaluated 3 times: twice pre-intervention and once post-intervention 3–5 days after the last session. | 10 physiotherapy sessions for 5 weeks. Duration unspecified | Cohen coefficient. Mandibular Functional Impairment Questionnaire. MMO Pressure pain threshold in both masseter and temporalis. | The protocol demonstrates significant changes in pain after MMO (32.3–8.8 mm to 38–8.8 mm), referred pain and joint functionality in such patients. |
| Craane et al., 2012 [18] | To evaluate the effects of physiotherapy on pain and mandibular dysfunction associated with anterior disc displacement without reduction of the joint space. | TMD with Anterior disc displacement without reduction of the temporomandibular joint (closed lock) | 49 patients Mean age 34.7 control group, mean age 38.5 experimental group. | G1: 23 patients. Therapeutic exercise. G2: 26 patients control group. | 1 year. Number and duration of sessions unspecified. | No use of quantitative scales | Physical therapy had no significant additional effect in patients with anterior disc displacement, without reduction, of the TMJ. |
| Madani et al., 2011 [19] | To evaluate the efficacy of three treatment methods in patients with painful TMJ clicking. | TMD (joint pain) | 60 patients Mean Age 27.2 G1 23.15 G2 22.43 G3 | G1: anterior positioning splint. G2: physical therapy. G3: physical treatment and splinting. Group ratio 1:1:1. | 4 weeks 35 min per session. | RDC/TMD VAS Bilateral palpation of TMJ muscles. | Subjective pain decreased in all three groups (p < 0.05). Changes between group 1 and 2 (p < 0.05). Group 2 and 3 no change. The anterior positioning splint proved to be the best treatment to reduce mandibular pain and sounds in patients with TMJ problems. |
| Dalewski et al., 2019 [20] | To compare the early effectiveness of routine intervention methods in patients with chronic orofacial pain. | TMD (joint pain) | 90 patients. 18–65 years. | G1: Occlusal appliance (OA) + NSAIDs. G2: OA + dry needling (DN). G3: OA (control group). | 3 weeks. Number and duration of sessions unspecified. | VAS Sleep Activity and Pain Questionnaire (SPAQ). | OA + NSAIDs showed better relief of orofacial pain, compared with the use of OA alone or together with DN. No differences between pain perception and quality of life between the OA + DN and OA groups. |
| Dib-Zakkour et al., 2022 [21] | To determine the effectiveness of deep dry needling as the first step in the treatment of TMDs. | TMD | 36 patients. 18–40 years. | Experimental group: bilateral dry needling of the masseter muscle. Control group: simulation of the technique. | 15 days. Evaluated pre-puncture, 10 min post puncture and after 15 days. | VAS Bilateral muscle palpation. T-Scans. Electromyography. | Facial pain is significantly reduced and is accompanied by a marked reduction in muscle activity after the puncture of its trigger points. |
| Nambi et al., 2022 [22] | To investigate the clinical and functional efficacy of electroacupuncture therapy on TMJ pain with orofacial myalgia after healing in patients with cervicofacial burns. | TMD with a cervico-facial burn | 30 patients. Age unspecified | Active group: 15 patients underwent electroacupuncture. Placebo group: 15 patients | 4 sessions/week for 1 month. | Pain intensity/threshold/frequency and mouth opening, disability level, and quality of life were measured at baseline, after week 4, week 8, and 6-month follow-up | Electroacupuncture therapy has an ideal treatment protocol for TMJ pain with orofacial myalgia after a healed cervicofacial burn (p < 0.001). |
| Chellappa et al., 2020 [23] | To compare the therapeutic efficacy of transcutaneous electrical nerve stimulation (TENS) and low-level laser in patients with TMDs | TMD | 60 patients Age unspecified. | All patients underwent both treatment methods. | 6 weeks. Low level laser: 2 sessions/3 weeks. TENS: 2 sessions/3 weeks, 15 min/session | VAS Numerical Rating Scale (NRS) Palpation of the bilateral masticatory musculature | The results of low-level laser therapy were significantly superior to those obtained with TENS (p < 0.01). |
| Li et al., 2020 [24] | To compare the therapeutic efficacy of extracorporeal shock waves (ESW) and ultrashort waves (UW) for TMDs. | TMD | 80 patients. >18 years. | G1: ESW. G2: UW | 1 month. Sessions unspecified | VAS MMO | ESW presents better results than UW (p < 0.05). |
| Jo et al., 2021 [25] | To evaluate the long-term efficacy and patient satisfaction with pulsed-radiofrequency therapy (PRF) in TMDs. | TMD | 86 + 23 women 18–65 years old | G1: PRF G2: placebo. | 12 weeks. 1 session/week 10min duration. | VAS MMO Baseline, after 4, 8, and 12 weeks. | PRF significantly reduced TMD pain. The effect was long-lasting after completion of treatment relative to the placebo group. |
| Brandão et al., 2021 [26] | To investigate the electroneurophysiological aspects of volunteers with TMDs before and after performing isotonic exercises for pain relief. | TMD with or without opening limitations | 23 patients 18–60 years old | Experimental: 12 patients Control: 11 patients. | 4 weeks 2 session/week | Electroencephalography RDC/TMD | Isotonic exercises performed to reduce pain provided a small increase in alpha power density in the left temporal, parietal, and occipital regions. |
| Urbański et al., 2021 [27] | To compare the degree of relaxation of the anterior part of the temporal muscles and the masseter muscles achieved through the use of post-isometric relaxation and myofascial release methods in patients requiring prosthetic treatment due to TMDs with a dominant muscular component. | TMD with a dominant muscular component | 60 patients 19–40 years old. | G1: post-isometric relaxation treatment. G2: myofascial release treatment. | 2 weekly sessions. 30 min duration. | EMG masticatory musculature. VAS | No significant changes were found between the two groups. |
| Shandilya et al., 2020 [28] | To determine the efficacy of intramuscularly infiltrating botulinum toxin into the masticatory muscles in patients with TMJ ankylosis. | TMD (TMJ ankylosis) | 20 patients. 18–45 years old. | Intervention group: botulinum toxin infiltration prior to surgery. Control group: saline solution. | 6 months. Evaluated after 1 week, 1, 3, and 6 months. | EMG. | Botulinum toxin infiltrations showed better results in terms of pain during mandibular opening exercises compared to the control group. |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Points |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brochado et al., 2018 [14] | N | Y | N | Y | N | N | Y | N | Y | Y | Y | 6/10 |
| Delgado de la Serna et al., 2020 [15] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Abboud et al., 2018 [16] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Calixtre et al., 2016 [17] | Y | N | N | Y | N | S | Y | N | Y | Y | Y | 7/10 |
| Craane et al., 2012 [18] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Madani et al., 2011 [19] | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 6/10 |
| Dalewski et al., 2019 [20] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Dib-Zakkour et al., 2022 [21] | Y | N | N | N | N | N | N | Y | Y | Y | Y | 5/10 |
| Nambi et al., 2022 [22] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9/10 |
| Chellappa et al., 2020 [23] | Y | Y | N | Y | N | N | N | N | N | Y | N | 4/10 |
| Li et al., 2020 [24] | Y | Y | N | N | N | N | N | N | Y | Y | Y | 5/10 |
| Jo et al., 2021 [25] | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 8/10 |
| Brandão et al., 2021 [26] | Y | Y | N | N | N | N | N | N | N | Y | N | 3/10 |
| Urbański et al., 2021 [27] | Y | N | N | Y | N | N | N | N | N | N | Y | 3/10 |
| Shandilya et al., 2020 [28] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Sánchez, B.; García Monterey, P.; Ramírez-Durán, M.d.V.; Garrido-Ardila, E.M.; Rodríguez-Mansilla, J.; Jiménez-Palomares, M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. J. Clin. Med. 2023, 12, 4156. https://doi.org/10.3390/jcm12124156
González-Sánchez B, García Monterey P, Ramírez-Durán MdV, Garrido-Ardila EM, Rodríguez-Mansilla J, Jiménez-Palomares M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. Journal of Clinical Medicine. 2023; 12(12):4156. https://doi.org/10.3390/jcm12124156
Chicago/Turabian StyleGonzález-Sánchez, Blanca, Pablo García Monterey, María del Valle Ramírez-Durán, Elisa Mª Garrido-Ardila, Juan Rodríguez-Mansilla, and María Jiménez-Palomares. 2023. "Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches" Journal of Clinical Medicine 12, no. 12: 4156. https://doi.org/10.3390/jcm12124156
APA StyleGonzález-Sánchez, B., García Monterey, P., Ramírez-Durán, M. d. V., Garrido-Ardila, E. M., Rodríguez-Mansilla, J., & Jiménez-Palomares, M. (2023). Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. Journal of Clinical Medicine, 12(12), 4156. https://doi.org/10.3390/jcm12124156









