The Effect of Symptom-Provocation on Inhibitory Control in Obsessive-Compulsive Disorder Patients Is Contingent upon Chronotype and Time of Day
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Clinical Assessments
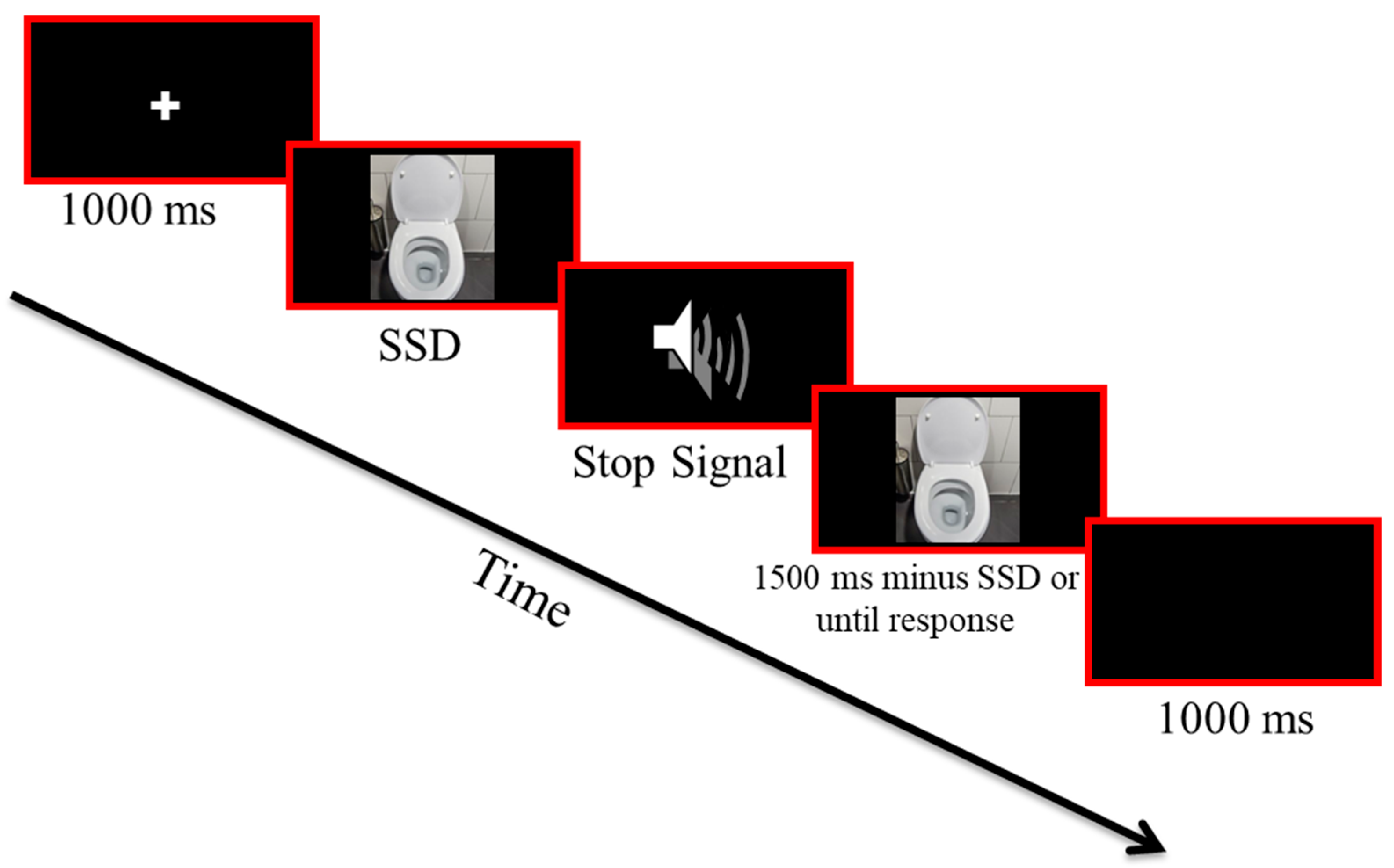
2.4. The Symptom-Provocation Stop Signal Task (SP-SST)
2.5. The Morningness–Eveningness Questionnaire (MEQ)
2.6. Statistical Analysis
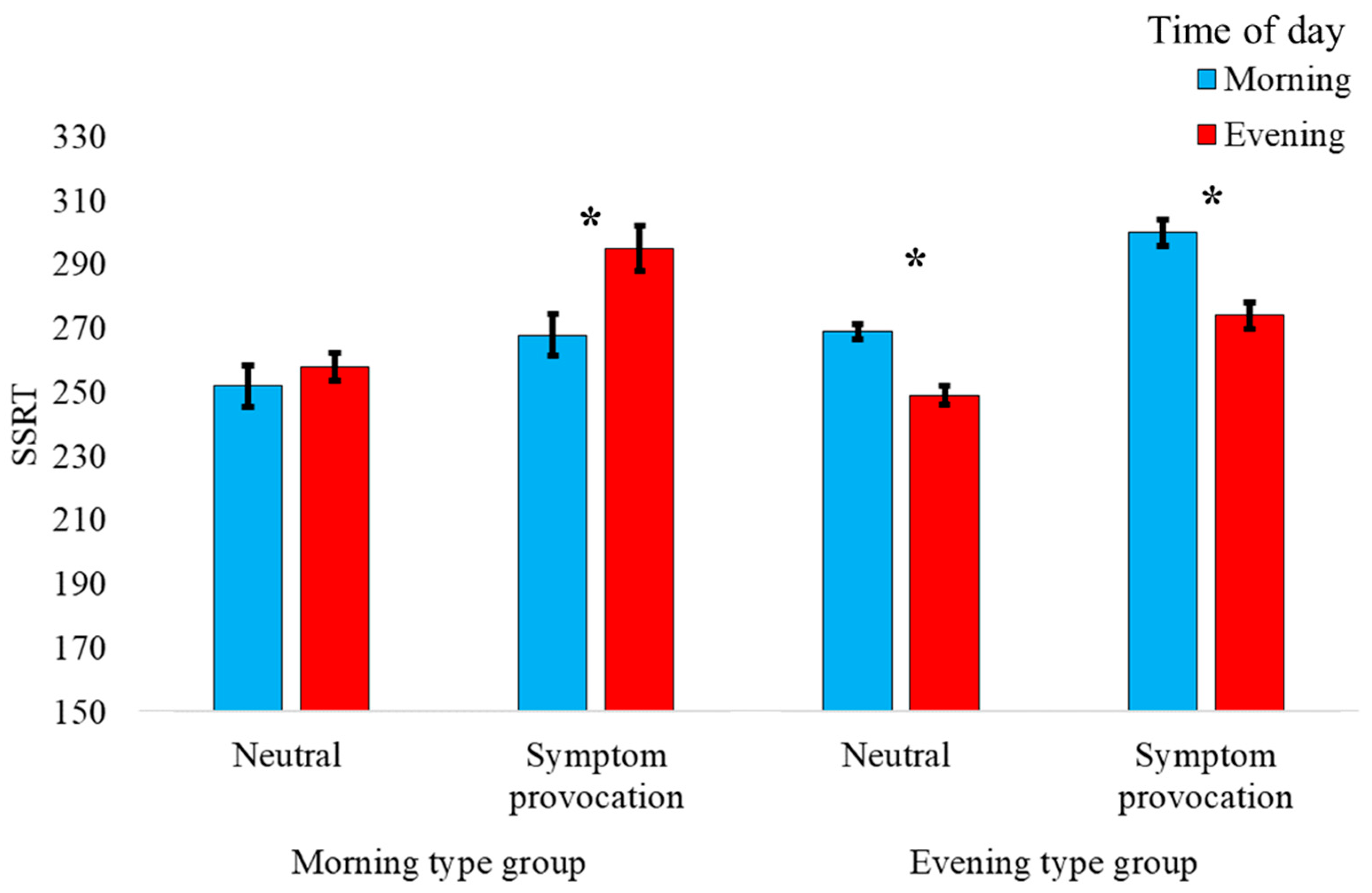
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- Abramovitch, A.; Abramowitz, J.S.; Mittelman, A. The Neuropsychology of Adult Obsessive–Compulsive Disorder: A Meta-Analysis. Clin. Psychol. Rev. 2013, 33, 1163–1171. [Google Scholar] [CrossRef]
- Anholt, G.E.; Linkovski, O.; Kalanthroff, E. If I Do It, It Must Be Important: Integrating Basic Cognitive Research Findings with Cognitive Behavior Theory of Obsessive-Compulsive Disorder. Psicoter. Cogn. Comport. 2012, 18, 69–78. [Google Scholar]
- Gillan, C.M.; Kalanthroff, E.; Evans, M.; Weingarden, H.M.; Jacoby, R.J.; Gershkovich, M.; Snorrason, I.; Campeas, R.; Cervoni, C.; Crimarco, N.C.; et al. Comparison of the Association Between Goal-Directed Planning and Self-Reported Compulsivity vs. Obsessive-Compulsive Disorder Diagnosis. JAMA Psychiatry 2020, 77, 77–85. [Google Scholar] [CrossRef] [Green Version]
- Linkovski, O.; Kalanthroff, E.; Henik, A.; Anholt, G.E. Did I Turn off the Stove? Good Inhibitory Control Can Protect from Influences of Repeated Checking. J. Behav. Ther. Exp. Psychiatry 2013, 44, 30–36. [Google Scholar] [CrossRef]
- Linkovski, O.; Kalanthroff, E.; Henik, A.; Anholt, G.E. Stop Checking: Repeated Checking and Its Effects on Response Inhibition and Doubt. J. Behav. Ther. Exp. Psychiatry 2016, 53, 84–91. [Google Scholar] [CrossRef]
- Robbins, T.W.; Vaghi, M.M.; Banca, P. Obsessive-Compulsive Disorder: Puzzles and Prospects. Neuron 2019, 102, 27–47. [Google Scholar] [CrossRef]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef]
- Logan, G.D.; Cowan, W.B. On the Ability to Inhibit Thought and Action: A Theory of an Act of Control. Psychol. Rev. 1984, 91, 295–327. [Google Scholar] [CrossRef]
- Verbruggen, F.; De Houwer, J. Do Emotional Stimuli Interfere with Response Inhibition? Evidence from the Stop Signal Paradigm. Cogn. Emot. 2007, 21, 391–403. [Google Scholar] [CrossRef]
- Verbruggen, F.; Aron, A.R.; Band, G.P.; Beste, C.; Bissett, P.G.; Brockett, A.T.; Brown, J.W.; Chamberlain, S.R.; Chambers, C.D.; Colonius, H.; et al. A Consensus Guide to Capturing the Ability to Inhibit Actions and Impulsive Behaviors in the Stop-Signal Task. eLife 2019, 8, e46323. [Google Scholar] [CrossRef] [PubMed]
- van Velzen, L.S.; Vriend, C.; de Wit, S.J.; van den Heuvel, O.A. Response Inhibition and Interference Control in Obsessive Compulsive Spectrum Disorders. Front. Hum. Neurosci. 2014, 8, 419. [Google Scholar] [CrossRef] [PubMed]
- Abramovitch, A.; Cooperman, A. The Cognitive Neuropsychology of Obsessive-Compulsive Disorder: A Critical Review. J. Obs. Compuls. Relat. Disord. 2015, 5, 24–36. [Google Scholar] [CrossRef]
- Kalanthroff, E.; Teichert, T.; Wheaton, M.G.; Kimeldorf, M.B.; Linkovski, O.; Ahmari, S.E.; Fyer, A.J.; Schneier, F.R.; Anholt, G.E.; Simpson, H.B. The Role of Response Inhibition in Medicated and Unmedicated Obsessive-Compulsive Disorder Patients: Evidence from the Stop-Signal Task. Depress. Anxiety 2017, 34, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.C.; Hulbert, J.C. Active Forgetting: Adaptation of Memory by Prefrontal Control. Annu. Rev. Psychol. 2021, 72, 1–36. [Google Scholar] [CrossRef]
- Bartholomew, M.E.; Heller, W.; Miller, G.A. Inhibitory Control of Emotional Processing: Theoretical and Empirical Considerations. Int. J. Psychophysiol. 2021, 163, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Akerman, A.; Naftalovich, H.; Akiva-Kabiri, L.; Kalanthroff, E. Inhibiting the Emergence of Involuntary Musical Imagery: Implications for Improving Our Understanding of Intrusive Thoughts. Cogn. Ther. Res. 2020, 44, 885–891. [Google Scholar] [CrossRef]
- Kalanthroff, E.; Cohen, N.; Henik, A. Stop Feeling: Inhibition of Emotional Interference Following Stop-Signal Trials. Front. Hum. Neurosci. 2013, 7, 78. [Google Scholar] [CrossRef]
- Linkovski, O.; Rodriguez, C.I.; Wheaton, M.G.; Henik, A.; Anholt, G.E. Momentary Induction of Inhibitory Control and Its Effects on Uncertainty. J. Cogn. 2021, 4, 10. [Google Scholar] [CrossRef]
- Kalanthroff, E.; Linkovski, O.; Henik, A.; Wheaton, M.G.; Anholt, G.E. Inhibiting Uncertainty: Priming Inhibition Promotes Reduction of Uncertainty. Neuropsychologia 2016, 92, 142–146. [Google Scholar] [CrossRef]
- Petersen, S.E.; Posner, M.I. The Attention System of the Human Brain: 20 Years After. Annu. Rev. Neurosci. 2012, 35, 73–89. [Google Scholar] [CrossRef]
- Posner, M.I.; Petersen, S.E. The Attention System of the Human Brain. Annu. Rev. Neurosci. 1990, 13, 25–42. [Google Scholar] [CrossRef]
- Posner, M.I.; Rothbart, M.K. Attentional Mechanisms and Conscious Experience. In The Neuropsychology of Consciousness; Elsevier: Amsterdam, The Netherlands, 1992; pp. 91–111. ISBN 978-0-12-498045-7. [Google Scholar]
- Hayat, H.; Regev, N.; Matosevich, N.; Sales, A.; Paredes-Rodriguez, E.; Krom, A.J.; Bergman, L.; Li, Y.; Lavigne, M.; Kremer, E.J.; et al. Locus Coeruleus Norepinephrine Activity Mediates Sensory-Evoked Awakenings from Sleep. Sci. Adv. 2020, 6, eaaz4232. [Google Scholar] [CrossRef] [PubMed]
- Aston-Jones, G.; Cohen, J.D. An Integrative Theory of Locus Coeruleus-Norepinephrine Function: Adaptive Gain and Optimal Performance. Annu. Rev. Neurosci. 2005, 28, 403–450. [Google Scholar] [CrossRef]
- Aston-Jones, G.; Waterhouse, B. Locus Coeruleus: From Global Projection System to Adaptive Regulation of Behavior. Brain Res. 2016, 1645, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Altena, E.; Nombela, C.; Housden, C.R.; Maxwell, H.; Rittman, T.; Huddleston, C.; Rae, C.L.; Regenthal, R.; Sahakian, B.J.; et al. Improving Response Inhibition in Parkinson’s Disease with Atomoxetine. Biol. Psychiatry 2015, 77, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Zhukovsky, P.; Morein-Zamir, S.; Ziauddeen, H.; Fernandez-Egea, E.; Meng, C.; Regenthal, R.; Sahakian, B.J.; Bullmore, E.T.; Robbins, T.W.; Dalley, J.W.; et al. Prefrontal Cortex Activation and Stopping Performance Underlie the Beneficial Effects of Atomoxetine on Response Inhibition in Healthy Volunteers and Those with Cocaine Use Disorder. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2022, 7, 1116–1126. [Google Scholar] [CrossRef]
- Weinbach, N.; Kalanthroff, E.; Avnit, A.; Henik, A. Can Arousal Modulate Response Inhibition? J. Exp. Psychol. Learn. Mem. Cogn. 2015, 41, 1873–1877. [Google Scholar] [CrossRef]
- Kalanthroff, E.; Linkovski, O.; Weinbach, N.; Pascucci, O.; Anholt, G.E.; Simpson, H.B. What Underlies the Effect of Sleep Disruption? The Role of Alertness in Obsessive-Compulsive Disorder (OCD). J. Behav. Ther. Exp. Psychiatry 2017, 57, 212–213. [Google Scholar] [CrossRef]
- Nota, J.A.; Schubert, J.R.; Coles, M.E. Sleep Disruption Is Related to Poor Response Inhibition in Individuals with Obsessive–Compulsive and Repetitive Negative Thought Symptoms. J. Behav. Ther. Exp. Psychiatry 2016, 50, 23–32. [Google Scholar] [CrossRef]
- Naftalovich, H.; Tauber, N.; Kalanthroff, E. But First, Coffee: The Roles of Arousal and Inhibition in the Resistance of Compulsive Cleansing in Individuals with High Contamination Fears. J. Anxiety Disord. 2020, 76, 102316. [Google Scholar] [CrossRef]
- Coles, M.E.; Stewart, E. Circadian Zeitgebers and Treatment Outcome in Inpatient Programs for Obsessive Compulsive Disorder (OCD): A Pilot Study. Chronobiol. Int. 2019, 36, 1190–1193. [Google Scholar] [CrossRef] [PubMed]
- Dijk, D.-J.; Duffy, J.F.; Czeisler, C.A. Circadian and Sleep/Wake Dependent Aspects of Subjective Alertness and Cognitive Performance. J. Sleep Res. 1992, 1, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Scheiermann, C.; Kunisaki, Y.; Frenette, P.S. Circadian Control of the Immune System. Nat. Rev. Immunol. 2013, 13, 190–198. [Google Scholar] [CrossRef]
- Tonetti, L.; Natale, V.; Randler, C. Association between Circadian Preference and Academic Achievement: A Systematic Review and Meta-Analysis. Chronobiol. Int. 2015, 32, 792–801. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A Self-Assessment Questionnaire to Determine Morningness-Eveningness in Human Circadian Rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Matchock, R.L.; Mordkoff, T.J. Chronotype and Time-of-Day Influences on the Alerting, Orienting, and Executive Components of Attention. Exp. Brain Res. 2009, 192, 189–198. [Google Scholar] [CrossRef]
- Bailey, S.L.; Heitkemper, M.M. Circadian Rhythmicity of Cortisol and Body Temperature: Morningness-Eveningness Effects. Chronobiol. Int. 2001, 18, 249–261. [Google Scholar] [CrossRef]
- Carasso, S.; Fishman, B.; Lask, L.S.; Shochat, T.; Geva-Zatorsky, N.; Tauber, E. Metagenomic Analysis Reveals the Signature of Gut Microbiota Associated with Human Chronotypes. FASEB J. 2021, 35, e22011. [Google Scholar] [CrossRef]
- Natale, V.; Cicogna, P. Morningness-Eveningness Dimension: Is It Really a Continuum? Personal. Individ. Differ. 2002, 32, 809–816. [Google Scholar] [CrossRef]
- Kerkhof, G.A.; Korving, H.J.; Willemse-vd Geest, H.M.; Rietveld, W.J. Diurnal Differences between Morning-Type and Evening-Type Subjects in Self-Rated Alertness, Body Temperature and the Visual and Auditory Evoked Potential. Neurosci. Lett. 1980, 16, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.; Collette, F.; Leclercq, Y.; Sterpenich, V.; Vandewalle, G.; Berthomier, P.; Berthomier, C.; Phillips, C.; Tinguely, G.; Darsaud, A.; et al. Homeostatic Sleep Pressure and Responses to Sustained Attention in the Suprachiasmatic Area. Science 2009, 324, 516–519. [Google Scholar] [CrossRef] [PubMed]
- Koran, L.M.; Aboujaoude, E.; Gamel, N.N. Double-Blind Study of Dextroamphetamine versus Caffeine Augmentation for Treatment-Resistant Obsessive-Compulsive Disorder. J. Clin. Psychiatry 2009, 70, 1530–1535. [Google Scholar] [CrossRef]
- Naftalovich, H.; Anholt, G.E.; Keren, R.; Ben Arush, O.; Kalanthroff, E. Waxing and Waning: The Roles of Chronotype and Time of Day in Predicting Symptom Fluctuations in Obsessive-Compulsive Disorder Using a Daily-Monitoring Design. J. Psychiatr. Res. 2021, 143, 91–97. [Google Scholar] [CrossRef]
- Nota, J.A.; Gibb, B.E.; Coles, M.E. Obsessions and Time of Day: A Self-Monitoring Study in Individuals with Obsessive-Compulsive Disorder. J. Cogn. Psychother. 2014, 28, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Goodman, W.K.; Price, L.H.; Rasmussen, S.A.; Mazure, C.; Fleischmann, R.L.; Hill, C.L.; Heninger, G.R.; Charney, D.S. The Yale-Brown Obsessive Compulsive Scale: I. Development, Use, and Reliability. Arch. Gen. Psychiatry 1989, 46, 1006–1011. [Google Scholar] [CrossRef]
- First, M.B.; Williams, J.B.W.; Karg, R.S.; Spitzer, R.L. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV); American Psychiatric Association: Arlington, VA, USA, 2015. [Google Scholar]
- Foa, E.B.; Huppert, J.D.; Leiberg, S.; Langner, R.; Kichic, R.; Hajcak, G.; Salkovskis, P.M. The Obsessive-Compulsive Inventory: Development and Validation of a Short Version. Psychol. Assess. 2002, 14, 485–496. [Google Scholar] [CrossRef]
- Hajcak, G.; Huppert, J.D.; Simons, R.F.; Foa, E.B. Psychometric Properties of the OCI-R in a College Sample. Behav. Res. Ther. 2004, 42, 115–123. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G. Manual for the Beck Depression Inventory—II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Dozois, D.J.A.; Dobson, K.S.; Ahnberg, J.L. A Psychometric Evaluation of the Beck Depression Inventory–II. Psychol. Assess. 1998, 10, 83–89. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, S.J.; Lee, S.Y.; Jang, K.H.; Kim, I.S.; Duffy, J.F. Reliability and Validity of the Korean Version of Morningness–Eveningness Questionnaire in Adults Aged 20–39 Years. Chronobiol. Int. 2014, 31, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Thun, E.; Bjorvatn, B.; Osland, T.; Steen, V.M.; Sivertsen, B.; Johansen, T.; Lilleholt, T.H.; Udnes, I.; Nordhus, I.H.; Pallesen, S. An Actigraphic Validation Study of Seven Morningness-Eveningness Inventories. Eur. Psychol. 2012, 17, 222–230. [Google Scholar] [CrossRef]
- Verbruggen, F.; Chambers, C.D.; Logan, G.D. Fictitious Inhibitory Differences: How Skewness and Slowing Distort the Estimation of Stopping Latencies. Psychol Sci 2013, 24, 352–362. [Google Scholar] [CrossRef]
- Diggle, P. Analysis of Longitudinal Data; Oxford Univ. Press: Oxford, UK, 2002; ISBN 978-0-19-852484-7. [Google Scholar]
- Adams, T.G. Exposure to Emotionally Arousing, Contamination-Relevant Pictorial Stimuli Interferes with Response Inhibition: Implication for Obsessive–Compulsive Disorder. J. Obs. Compuls. Relat. Disord. 2015, 6, 66–71. [Google Scholar] [CrossRef]
- Hudiburgh, S.E.; Reese, H.E.; Carver, C.S.; Çek, D.; Timpano, K.R. A Multi-method Examination of the Link between Obsessive-compulsive Symptomatology and Emotion-related Impulsivity. Br. J. Clin. Psychol. 2021, 60, 293–311. [Google Scholar] [CrossRef]
- Paul, S.; Beucke, J.C.; Kaufmann, C.; Mersov, A.; Heinzel, S.; Kathmann, N.; Simon, D. Amygdala–Prefrontal Connectivity during Appraisal of Symptom-Related Stimuli in Obsessive–Compulsive Disorder. Psychol. Med. 2019, 49, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Simon, D.; Adler, N.; Kaufmann, C.; Kathmann, N. Amygdala Hyperactivation during Symptom Provocation in Obsessive–Compulsive Disorder and Its Modulation by Distraction. NeuroImage Clin. 2014, 4, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Kalanthroff, E.; Wheaton, M.G. An Integrative Model for Understanding Obsessive-Compulsive Disorder: Merging Cognitive Behavioral Theory with Insights from Clinical Neuroscience. J. Clin. Med. 2022, 11, 7379. [Google Scholar] [CrossRef] [PubMed]
- Abramovitch, A.; Dar, R.; Hermesh, H.; Schweiger, A. Comparative Neuropsychology of Adult Obsessive-Compulsive Disorder and Attention Deficit/Hyperactivity Disorder: Implications for a Novel Executive Overload Model of OCD: Comparative Neuropsychology of OCD and ADHD. J. Neuropsychol. 2012, 6, 161–191. [Google Scholar] [CrossRef]
- Fornaro, S.; Vallesi, A. Functional Connectivity Abnormalities of Brain Networks in Obsessive–Compulsive Disorder: A Systematic Review. Curr. Psychol. 2023. [Google Scholar] [CrossRef]
- Posner, J.; Song, I.; Lee, S.; Rodriguez, C.I.; Moore, H.; Marsh, R.; Simpson, H.B. Increased Functional Connectivity between the Default Mode and Salience Networks in Unmedicated Adults with Obsessive-Compulsive Disorder. Hum. Brain Mapp. 2017, 38, 678–687. [Google Scholar] [CrossRef]
- Sonuga-Barke, E.J.S.; Castellanos, F.X. Spontaneous Attentional Fluctuations in Impaired States and Pathological Conditions: A Neurobiological Hypothesis. Neurosci. Biobehav. Rev. 2007, 31, 977–986. [Google Scholar] [CrossRef]
- Fontaine, J.R.J.; Scherer, K.R.; Roesch, E.B.; Ellsworth, P.C. The World of Emotions Is Not Two-Dimensional. Psychol. Sci. 2007, 18, 1050–1057. [Google Scholar] [CrossRef]
- Frijda, N.H. Emotion, Cognitive Structure, and Action Tendency. Cogn. Emot. 1987, 1, 115–143. [Google Scholar] [CrossRef]
- Rinck, M.; Becker, E.S. Approach and Avoidance in Fear of Spiders. J. Behav. Ther. Exp. Psychiatry 2007, 38, 105–120. [Google Scholar] [CrossRef]
- Dayan-Riva, A.; Berger, A.; Anholt, G.E. Early Cognitive Processes in OCD: An ERP Study. J. Affect. Disord. 2019, 246, 429–436. [Google Scholar] [CrossRef]
- Lara, T.; Madrid, J.A.; Correa, Á. The Vigilance Decrement in Executive Function Is Attenuated When Individual Chronotypes Perform at Their Optimal Time of Day. PLoS ONE 2014, 9, e88820. [Google Scholar] [CrossRef]
- Song, J.; Feng, P.; Zhao, X.; Xu, W.; Xiao, L.; Zhou, J.; Zheng, Y. Chronotype Regulates the Neural Basis of Response Inhibition during the Daytime. Chronobiol. Int. 2018, 35, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Feng, P.; Wu, X.; Li, B.; Su, Y.; Liu, Y.; Zheng, Y. Individual Differences in the Neural Basis of Response Inhibition after Sleep Deprivation Are Mediated by Chronotype. Front. Neurol. 2019, 10, 514. [Google Scholar] [CrossRef] [PubMed]
- Linkovski, O.; Weinbach, N.; Edelman, S.; Feldman, M.W.; Lotem, A.; Kolodny, O. Beyond Uncertainty: A Broader Scope for “Incentive Hope” Mechanisms and Its Implications. Behav. Brain. Sci. 2019, 42, e44. [Google Scholar] [CrossRef] [PubMed]
| Morning Type Group (N = 10) | Evening Type Group (N = 15) | |||
|---|---|---|---|---|
| Demographics | ||||
| Age (years; mean, SD) | 35.3 | (13.6) | 27.7 | (9.6) |
| Education (years; mean, SD) | 14.5 | (2.9) | 13.5 | (1.5) |
| Sex (n, % female/male) | 3/7 | (30/70%) | 5/10 | (33/66%) |
| Current SRI (n, % on SRI) | 4 | (40%) | 9 | (60%) |
| Clinical Characteristics | ||||
| Y-BOCS Total (mean, SD) | 28.6 | (5.5) | 30.8 | (3.6) |
| MEQ | 50.3 | (3.7) | 36 | (6.6) |
| OCI-R (mean, SD) | 29.8 | (11.8) | 31.7 | (14.4) |
| BDI-II | 20.1 | (10.2) | 21.4 | (11.9) |
| Current comorbid disorders (N) | Depression (4), Dysthymia (1), ADHD (2), Social anxiety (2), GAD (1), Specific phobia (3), BDD (1), EA (1). | Depression (6), Dysthymia (2), ADHD (4), Social anxiety (2), GAD (3), Specific phobia (5), BDD (3). | ||
| Morning Type Group (N = 10) | Evening Type Group (N = 15) | ||||
|---|---|---|---|---|---|
| Session | Morning | Evening | Morning | Evening | |
| nsRT | Neutral | 564 (18) | 574 (30) | 594 (10) | 564 (21) |
| Symptom provocation | 600 (13) | 615 (12) | 596 (10) | 586 (15) | |
| SSRT | Neutral | 252 (13) | 258 (9) | 269 (5) | 249 (6) |
| Symptom provocation | 268 (13) | 295 (14) | 300 (8) | 274 (8) | |
| p(r|s) | Neutral | 0.52 | 0.55 | 0.53 | 0.56 |
| Symptom provocation | 0.53 | 0.55 | 0.51 | 0.53 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Linkovski, O.; Naftalovich, H.; David, M.; Seror, Y.; Kalanthroff, E. The Effect of Symptom-Provocation on Inhibitory Control in Obsessive-Compulsive Disorder Patients Is Contingent upon Chronotype and Time of Day. J. Clin. Med. 2023, 12, 4075. https://doi.org/10.3390/jcm12124075
Linkovski O, Naftalovich H, David M, Seror Y, Kalanthroff E. The Effect of Symptom-Provocation on Inhibitory Control in Obsessive-Compulsive Disorder Patients Is Contingent upon Chronotype and Time of Day. Journal of Clinical Medicine. 2023; 12(12):4075. https://doi.org/10.3390/jcm12124075
Chicago/Turabian StyleLinkovski, Omer, Hadar Naftalovich, Mor David, Yuval Seror, and Eyal Kalanthroff. 2023. "The Effect of Symptom-Provocation on Inhibitory Control in Obsessive-Compulsive Disorder Patients Is Contingent upon Chronotype and Time of Day" Journal of Clinical Medicine 12, no. 12: 4075. https://doi.org/10.3390/jcm12124075
APA StyleLinkovski, O., Naftalovich, H., David, M., Seror, Y., & Kalanthroff, E. (2023). The Effect of Symptom-Provocation on Inhibitory Control in Obsessive-Compulsive Disorder Patients Is Contingent upon Chronotype and Time of Day. Journal of Clinical Medicine, 12(12), 4075. https://doi.org/10.3390/jcm12124075






