Limited Link of Common Blood Parameters with Tinnitus
Abstract
1. Introduction
2. Materials and Methods
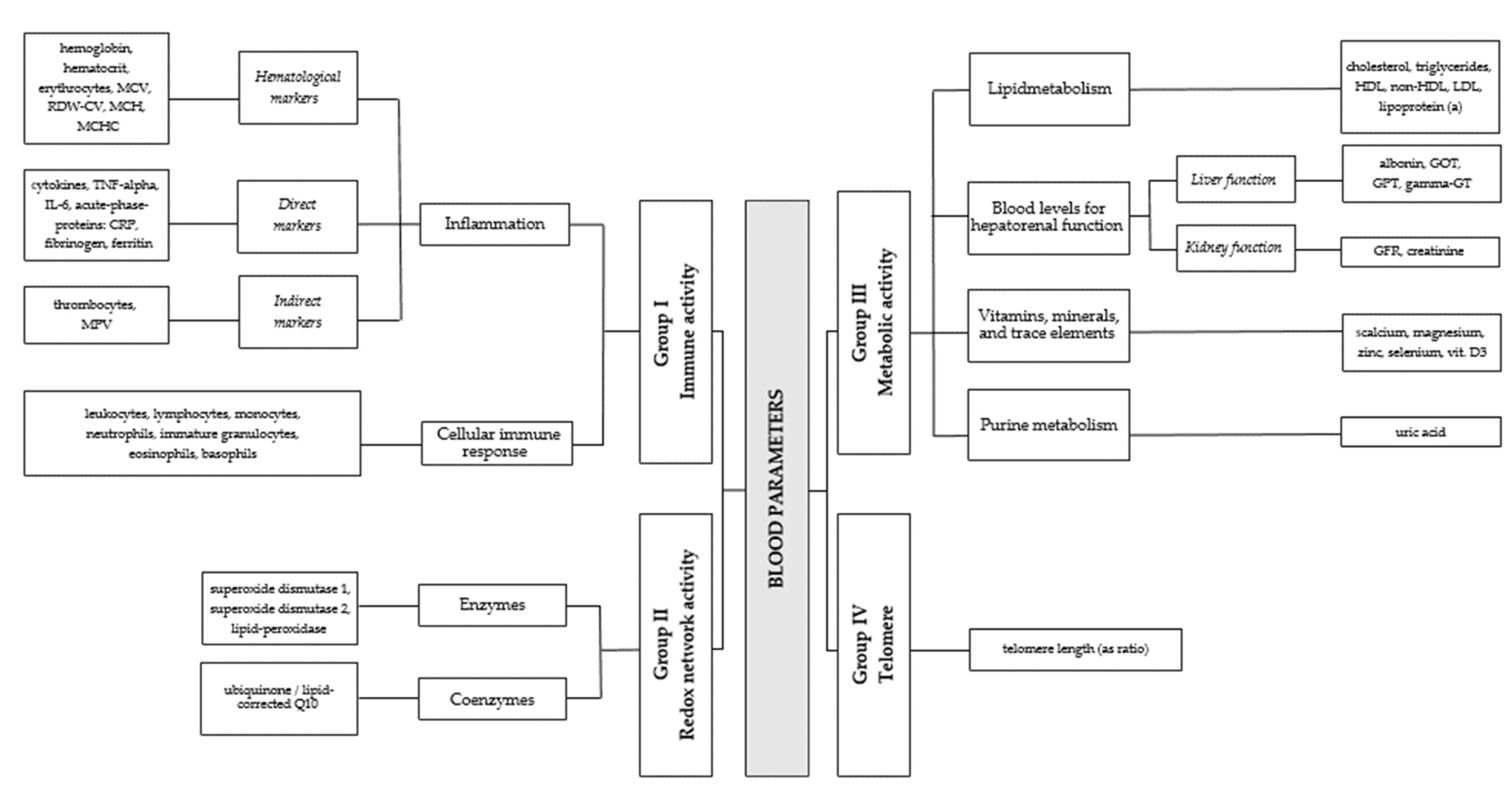
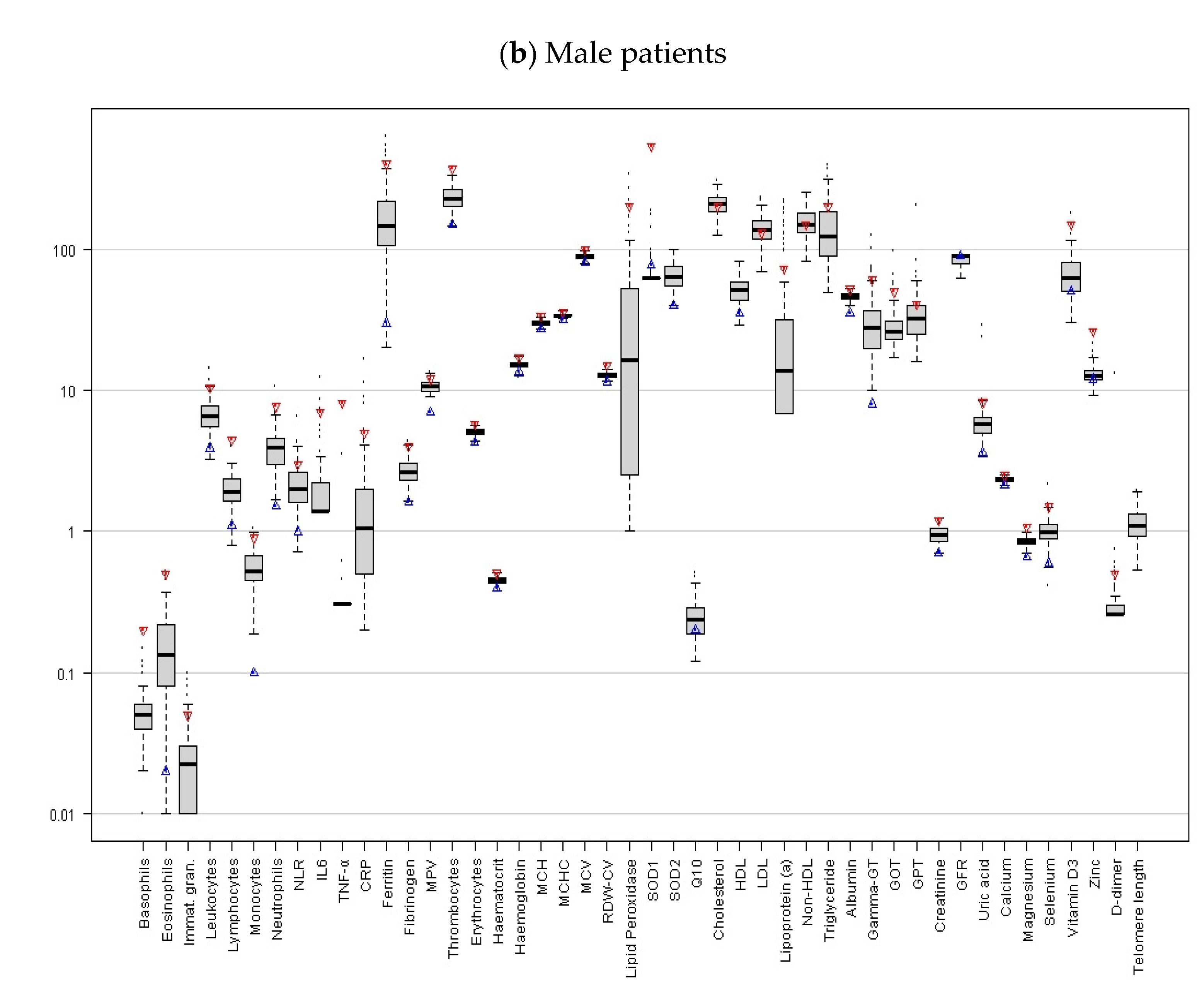
2.1. Sample and Blood Levels
2.2. Tinnitus Questionnaire and Audiological Measurements
2.3. Statistics
2.4. Ethical Approval
3. Results
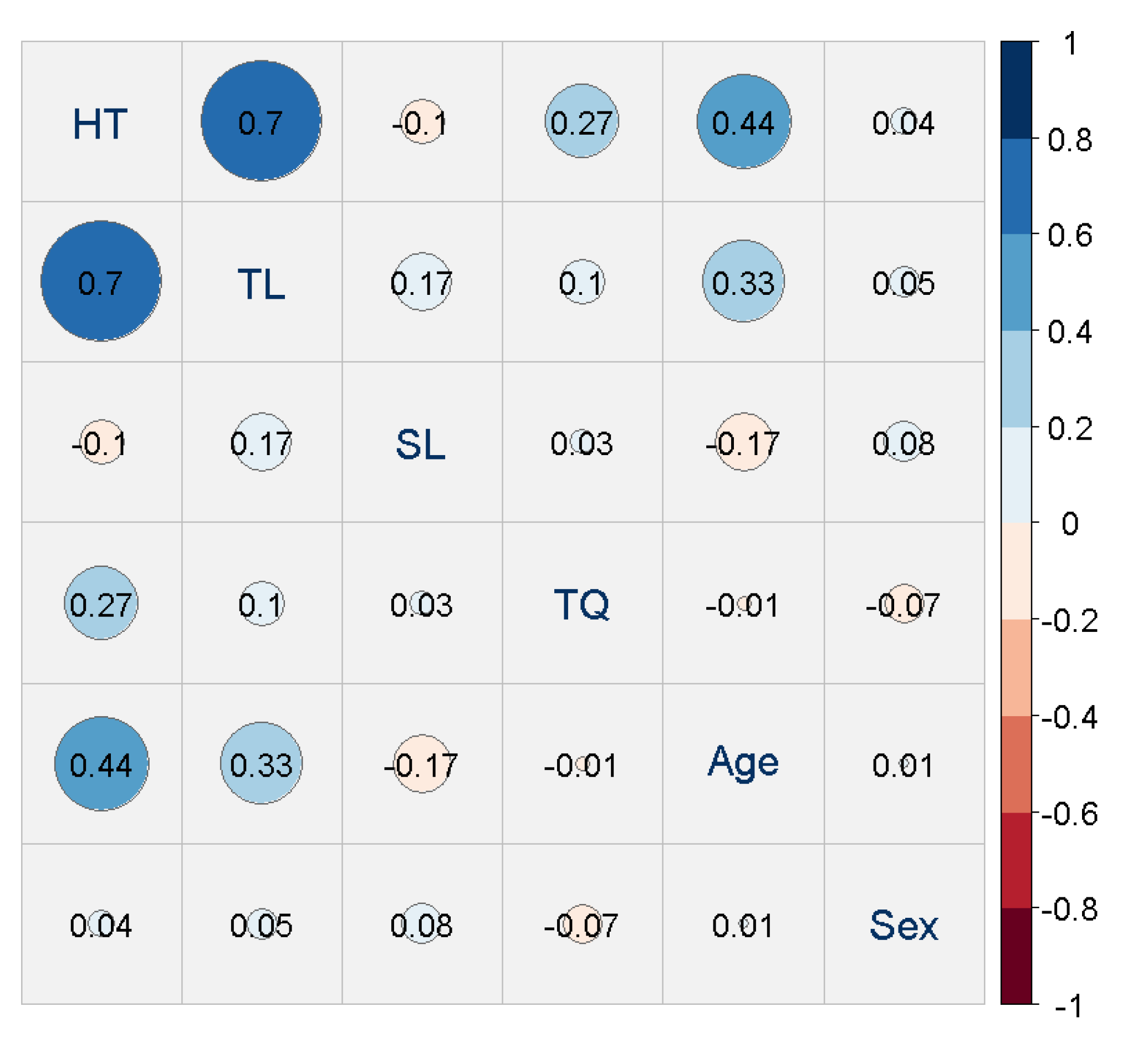
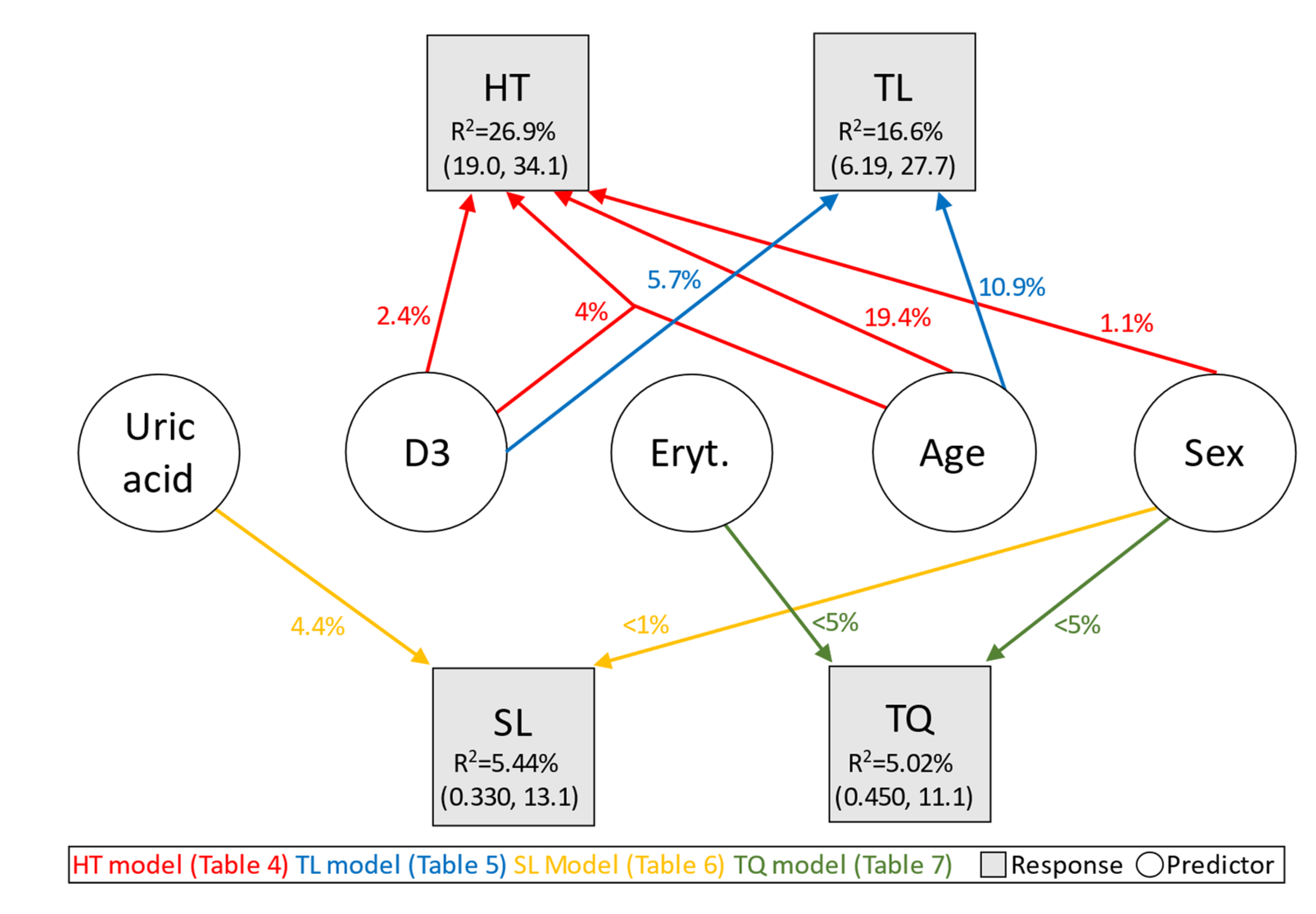
3.1. Link of Hearing Threshold (HT) and Blood Markers
3.2. Link of Tinnitus Loudness (TL) and Blood Markers
3.3. Link of Sensation Level (SL) and Blood Markers
3.4. Link of Tinnitus Distress (TQ) and Blood Markers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biswas, R.; Lugo, A.; Akeroyd, M.; Schlee, W.; Gallus, S.; Hall, D. Tinnitus prevalence in Europe: A multi-country cross-sectional population study. Lancet Reg. Health Eur. 2022, 12, 100250. [Google Scholar] [CrossRef]
- Trochidis, I.; Lugo, A.; Borroni, E.; Cederroth, C.R.; Cima, R.; Kikidis, D.; Langguth, B.; Schlee, W.; Gallus, S. Systematic Review on Healthcare and Societal Costs of Tinnitus. Int. J. Environ. Res. Public Health 2021, 18, 6881. [Google Scholar] [CrossRef]
- Brüggemann, P.; Szczepek, A.J.; Rose, M.; McKenna, L.; Olze, H.; Mazurek, B. Impact of Multiple Factors on the Degree of Tinnitus Distress. Front. Hum. Neurosci. 2016, 10, 341. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, B.; Böcking, B.; Dobel, C.; Rose, M.; Brüggemann, P. Tinnitus and Influencing Comorbidities. Laryngorhinootologie 2023, 102, 50–58. [Google Scholar]
- Deklerck, A.N.; Debacker, J.M.; Keppler, H.; Dhooge, I.J.M. Identifying non-otologic risk factors for tinnitus: A systematic review. Clin. Otolaryngol. 2020, 45, 775–787. [Google Scholar] [CrossRef] [PubMed]
- Cederroth, C.R.; Gallus, S.; Hall, D.A.; Kleinjung, T.; Langguth, B.; Maruotti, A.; Meyer, M.; Norena, A.; Probst, T.; Pryss, R.; et al. Editorial: Towards an Understanding of Tinnitus Heterogeneity. Front. Aging Neurosci. 2019, 11, 53. [Google Scholar] [CrossRef]
- De Ridder, D.; Schlee, W.; Vanneste, S.; Londero, A.; Weisz, N.; Kleinjung, T.; Shekhawat, G.S.; Elgoyhen, A.B.; Song, J.J.; Andersson, G.; et al. Chapter 1—Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). In Progress in Brain Research; Schlee, W., Langguth, B., Kleinjung, T., Vanneste, S., De Ridder, D., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; Volume 260, pp. 1–25. [Google Scholar]
- Hall, D.A.; Haider, H.; Szczepek, A.J.; Lau, P.; Rabau, S.; Jones-Diette, J.; Londero, A.; Edvall, N.K.; Cederroth, C.R.; Mielczarek, M.; et al. Systematic review of outcome domains and instruments used in clinical trials of tinnitus treatments in adults. Trials 2016, 17, 270. [Google Scholar] [CrossRef]
- Boecking, B.; Klasing, S.; Walter, M.; Brueggemann, P.; Nyamaa, A.; Rose, M.; Mazurek, B. Vascular-Metabolic Risk Factors and Psychological Stress in Patients with Chronic Tinnitus. Nutrients 2022, 14, 2256. [Google Scholar] [CrossRef]
- Goebel, G.; Hiller, W. The tinnitus questionnaire. A standard instrument for grading the degree of tinnitus. Results of a multicenter study with the tinnitus questionnaire. HNO 1994, 42, 166–172. [Google Scholar]
- Kang, D.-W.; Kim, S.-S.; Park, D.-C.; Kim, S.-H.; Yeo, S.-G. Objective and Measurable Biomarkers in Chronic Subjective Tinnitus. Int. J. Mol. Sci. 2021, 22, 6619. [Google Scholar] [CrossRef]
- Demir, M. Does inflammation play a role in the pathophysiology of tinnitus? Niger. J. Clin. Pract. 2021, 24, 199–204. [Google Scholar] [PubMed]
- Chrbolka, P.; Alusik, S.; Kalatova, D.; Paluch, Z. Increased platelet activity in tinnitus patients. Neuro Endocrinol. Lett. 2020, 41, 102–106. [Google Scholar] [PubMed]
- Szczepek, A.J.; Haupt, H.; Klapp, B.F.; Olze, H.; Mazurek, B. Biological correlates of tinnitus-related distress: An exploratory study. Hear. Res. 2014, 318, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Haider, H.F.; Ribeiro, S.F.; Martins, C.; Ribeiro, D.; Trigueiros, N.; Szczepek, A.J.; Caria, H.; Hoare, D.J.; Paço, J.; Borrego, L.-M. Tinnitus, hearing loss and inflammatory processes in an older Portuguese population. Int. J. Audiol. 2019, 59, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Savastano, M.; Aita, M.; Barlani, F. Psychological, neural, endocrine, and immune study of stress in tinnitus patients: Any correlation between psychometric and biochemical measures? Ann. Otol. Rhinol. Laryngol. 2007, 116, 100–106. [Google Scholar] [CrossRef]
- Gunes, A.; Karali, E.; Ural, A.; Ruzgar, F.; Bayatkara, T. The relationship of high-frequency distortion product otoacoustic emission (DPOAE) values with hematological parameters in tinnitus patients. Eur. Arch. Otorhinolaryngol. 2019, 276, 3013–3019. [Google Scholar] [CrossRef]
- Yüksel, F.; Karataş, D. Can Platelet Indices Be New Biomarkers for Subjective Tinnitus. J. Craniofacial Surg. 2016, 27, e420–e424. [Google Scholar] [CrossRef]
- Pawlak-Osińska, K.; Kaźmierczak, H.; Marzec, M.; Kupczyk, D.; Bilski, R.; Mikołajewska, E.; Mikołajewski, D.; Augustyńska, B. Assessment of the State of the Natural Antioxidant Barrier of a Body in Patients Complaining about the Presence of Tinnitus. Oxidative Med. Cell. Longev. 2018, 2018, 1439575. [Google Scholar] [CrossRef]
- Celik, M.; Koyuncu, I. A Comprehensive Study of Oxidative Stress in Tinnitus Patients. Indian J. Otolaryngol. Head Neck Surg. 2018, 70, 521–526. [Google Scholar] [CrossRef]
- Koç, S.; Akyüz, S.; Somuk, B.T.; Soyalic, H.; Yılmaz, B.; Taskin, A.; Bilinc, H.; Aksoy, N. Paraoxonase Activity and Oxidative Status in Patients with Tinnitus. J. Audiol. Otol. 2016, 20, 17–21. [Google Scholar] [CrossRef]
- Avcı, D. Increased Serum Lipid Levels in Patients with Subjective Tinnitus. Iran. J. Otorhinolaryngol. 2021, 33, 31–36. [Google Scholar]
- Ensari, N.; Gür, Ö.E.; Gür, N.; Selçuk, Ö.T.; Renda, L.; Yilmaz, M.D.; Öztürk, M.T.; Çekin, Y. Can apelin play a role in the etiology of tinnitus? Turk. J. Med. Sci. 2019, 49, 769–773. [Google Scholar] [CrossRef]
- Neuner, B.; Lenfers, A.; Kelsch, R.; Jäger, K.; Brüggmann, N.; Van Der Harst, P.; Walter, M. Telomere Length Is Not Related to Established Cardiovascular Risk Factors but Does Correlate with Red and White Blood Cell Counts in a German Blood Donor Population. PLoS ONE 2015, 10, e0139308. [Google Scholar] [CrossRef]
- Haider, H.F.; Hoare, D.J.; Ribeiro, S.F.; Ribeiro, D.; Caria, H.; Trigueiros, N.; Borrego, L.M.; Szczepek, A.J.; Papoila, A.L.; Elarbed, A.; et al. Evidence for biological markers of tinnitus: A systematic review. Prog. Brain Res. 2021, 262, 345–398. [Google Scholar] [PubMed]
- Liu, Y.W.; Wang, B.; Chen, B.; Galvin, J.J.; Fu, Q.-J. Tinnitus impairs segregation of competing speech in normal-hearing listeners. Sci. Rep. 2020, 10, 19851. [Google Scholar] [CrossRef]
- Mohamad, N.; Hoare, D.J.; Hall, D.A. The consequences of tinnitus and tinnitus severity on cognition: A review of the behavioural evidence. Hear. Res. 2016, 332, 199–209. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Walter, O.B.; Kocalevent, R.-D.; Weber, C.; Klapp, B.F. The Perceived Stress Questionnaire (PSQ) reconsidered: Validation and reference values from different clinical and healthy adult samples. Psychosom. Med. 2005, 67, 78–88. [Google Scholar] [CrossRef]
- Hotter, B.; Hoffmann, S.; Ulm, L.; Montaner, J.; Bustamante, A.; Meisel, C.; Meisel, A. Inflammatory and stress markers predicting pneumonia, outcome, and etiology in patients with stroke. Neurol. Neuroimmunol. Neuroinflammation 2020, 7, e692. [Google Scholar] [CrossRef]
- Basso, L.; Boecking, B.; Neff, P.; Brueggemann, P.; Mazurek, B.; Peters, E.M.J. Psychological Treatment Effects Unrelated to Hair-Cortisol and Hair-BDNF Levels in Chronic Tinnitus. Front. Psychiatry 2022, 13, 764368. [Google Scholar] [CrossRef]
- Boecking, B.; Rausch, L.; Psatha, S.; Nyamaa, A.; Dettling-Papargyris, J.; Funk, C.; Brueggemann, P.; Rose, M.; Mazurek, B. Hearing Therapy Improves Tinnitus-Related Distress in Mildly Distressed Patients with Chronic Tinnitus and Mild-to-Moderate Hearing Loss: A Randomized-Controlled Cross-Over Design. J. Clin. Med. 2022, 11, 1764. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Maechler, M.; Rousseeuw, P.; Croux, C.; Todorov, V.; Ruckstuhl, A.; Salibian-Barrera, M.; Verbeke, T.; Koller, M.; Conceicao, E.L.; di Palma, M.A. Robustbase: Basic Robust Statistics; Version 0.95-1; RDocumentation: New York, NY, USA, 2022. [Google Scholar]
- Koller, M.; Stahel, W.A. Nonsingular subsampling for regression S estimators with categorical predictors. Comput. Stat. 2017, 32, 631–646. [Google Scholar] [CrossRef]
- Davison, A.C.; Hinkley, D.V. Bootstrap Methods and Their Application; Cambridge University Press: Cambridge, UK, 1997. [Google Scholar]
- Canty, A.; Ripley, B. boot: Bootstrap R (S-Plus) Functions. 2021. Available online: https://cran.r-project.org/web/packages/boot/citation.html (accessed on 1 May 2023).
- Waechter, S. Association between hearing status and tinnitus distress. Acta Oto-Laryngol. 2021, 141, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Zenner, H.-P.; Delb, W.; Kröner-Herwig, B.; Jäger, B.; Peroz, I.; Hesse, G.; Mazurek, B.; Goebel, G.; Gerloff, C.; Trollmann, R.; et al. A multidisciplinary systematic review of the treatment for chronic idiopathic tinnitus. Eur. Arch. Otorhinolaryngol. 2017, 274, 2079–2091. [Google Scholar] [CrossRef]
- Dawes, P.; Cruickshanks, K.J.; Fischer, M.E.; Klein, B.E.; Klein, R.; Nondahl, D.M. Hearing-aid use and long-term health outcomes: Hearing handicap, mental health, social engagement, cognitive function, physical health, and mortality. Int. J. Audiol. 2015, 54, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Brueggemann, P.; Neff, P.K.; Meyer, M.; Riemer, N.; Rose, M.; Mazurek, B. Chapter 13—On the relationship between tinnitus distress, cognitive performance and aging. In Progress in Brain Research; Langguth, B., Kleinjung, T., De Ridder, D., Schlee, W., Vanneste, S., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; Volume 262, pp. 263–285. [Google Scholar]
- Neff, P.; Simões, J.; Psatha, S.; Nyamaa, A.; Boecking, B.; Rausch, L.; Dettling-Papargyris, J.; Funk, C.; Brueggemann, P.; Mazurek, B. The impact of tinnitus distress on cognition. Sci. Rep. 2021, 11, 2243. [Google Scholar] [CrossRef]
- Henry, J.A. “Measurement” of Tinnitus. Otol. Neurotol. 2016, 37, e276–e285. [Google Scholar] [CrossRef]
- Mazurek, B.; Szczepek, A.J.; Hebert, S. Stress and tinnitus. HNO 2015, 63, 258–265. [Google Scholar] [CrossRef]
- Paprocki, J.; Sutkowy, P.; Piechocki, J.; Woźniak, A. Association between Vitamin D Supplements, Oxidative Stress Biomarkers, and Hyperbaric Therapy in Patients with Sudden Sensorineural Hearing Loss. Oxidative Med. Cell. Longev. 2021, 2021, 8895323. [Google Scholar] [CrossRef]
- Atan, D.; Atan, T.; Özcan, K.M.; Ensari, S.; Dere, H. Relation of otosclerosis and osteoporosis: A bone mineral density study. Auris Nasus Larynx 2016, 43, 400–403. [Google Scholar] [CrossRef]
- Yamauchi, D.; Nakaya, K.; Raveendran, N.N.; Harbidge, D.G.; Singh, R.; Wangemann, P.; Marcus, D.C. Expression of epithelial calcium transport system in rat cochlea and vestibular labyrinth. BMC Physiol. 2010, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Brookler, K.H.; Hamid, M.A. An Approach to Tinnitus Management. Ear Nose Throat J. 2008, 87, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Dawes, P.; Cruickshanks, K.J.; Marsden, A.; Moore, D.R.; Munro, K.J. Relationship Between Diet, Tinnitus, and Hearing Difficulties. Ear Hear. 2020, 41, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.Y.; Kim, S.H.; Yeo, S.G. Association of Nutritional Factors with Hearing Loss. Nutrients 2019, 11, 307. [Google Scholar] [CrossRef] [PubMed]
- Marcinowska-Suchowierska, E.; Kupisz-Urbańska, M.; Łukaszkiewicz, J.; Płudowski, P.; Jones, G. Vitamin D Toxicity–A Clinical Perspective. Front. Endocrinol. 2018, 9, 550. [Google Scholar] [CrossRef] [PubMed]
- Abdelmawgoud, S.M. Vitamin D Level and its Relation to Tinnitus. Egypt. J. Ear Nose Throat Allied Sci. 2021, 22, 1–5. [Google Scholar] [CrossRef]
- Cotanche, D.A. Genetic and pharmacological intervention for treatment/prevention of hearing loss. J. Commun. Disord. 2008, 41, 421–443. [Google Scholar] [CrossRef]
- Le Prell, C.G.; Johnson, A.-C.; Lindblad, A.-C.; Skjönsberg, A.; Ulfendahl, M.; Guire, K.; Green, G.E.; Campbell, K.C.M.; Miller, J.M. Increased vitamin plasma levels in Swedish military personnel treated with nutrients prior to automatic weapon training. Noise Health 2011, 13, 432–443. [Google Scholar] [CrossRef]
- Nowaczewska, M.; Osiński, S.; Marzec, M.; Wiciński, M.; Bilicka, K.; Kaźmierczak, W. The role of vitamin D in subjective tinnitus-A case-control study. PLoS ONE 2021, 16, e0255482. [Google Scholar] [CrossRef]
- Kaźmierczak, H.; Doroszewska, G. Metabolic disorders in vertigo, tinnitus, and hearing loss. Int. Tinnitus J. 2001, 7, 54–58. [Google Scholar]
- Hamed, S.A.; El-Attar, A.M. Cochlear dysfunction in hyperuricemia: Otoacoustic emission analysis. Am. J. Otolaryngol. 2010, 31, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Moon, I.J.; Byun, H.; Woo, S.Y.; Gwak, G.Y.; Hong, S.H.; Chung, W.H.; Cho, Y.S. Factors Associated with Age-related Hearing Impairment: A Retrospective Cohort Study. Medicine 2015, 94, e1846. [Google Scholar] [CrossRef] [PubMed]
- Fasano, T.; Pertinhez, T.A.; Tribi, L.; Lasagni, D.; Pilia, A.; Vecchia, L.; Baricchi, R.; Bianchin, G. Laboratory assessment of sudden sensorineural hearing loss: A case-control study. Laryngoscope 2017, 127, 2375–2381. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Hong, D.; She, W.; Lu, W.; Xia, G. Relationship between Sudden Sensorineural Hearing Loss and Vascular Risk Factors. J. Otol. 2009, 4, 55–58. [Google Scholar]
- Yang, H.-F.; Kao, T.-W.; Peng, T.-C.; Sun, Y.-S.; Liaw, F.-Y.; Wang, C.-C.; Hsueh, J.-T.; Chen, W.-L. Serum Uric Acid Relation for Hearing Threshold Shift. Clin. Exp. Otorhinolaryngol. 2016, 10, 143–147. [Google Scholar] [CrossRef]
- Newman, P.E. Can idiopathic tinnitus be caused by hyperuricemia? Med. Hypotheses 1998, 50, 535–536. [Google Scholar] [CrossRef]
- Basso, L.; Boecking, B.; Neff, P.; Brueggemann, P.; Peters, E.M.J.; Mazurek, B. Hair-cortisol and hair-BDNF as biomarkers of tinnitus loudness and distress in chronic tinnitus. Sci. Rep. 2022, 12, 1934. [Google Scholar] [CrossRef]
- Chrousos, G.P.; Gold, P.W. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA 1992, 267, 1244–1252. [Google Scholar] [CrossRef]
- Resuli, A.S. Can the Determination of Salivary Cotinine Level Be a New Method in Diagnosis and Follow-up of Childhood Tinnitus? Iran. Red Crescent Med. J. 2020, 22, e95472. [Google Scholar]
- Lee, D.Y.; Kim, Y.H. Urine Cotinine Should Be Involved in Initial Evaluation of Tinnitus in Adolescents. Clin. Exp. Otorhinolaryngol. 2018, 11, 242–249. [Google Scholar] [CrossRef]
- Seydel, C.; Haupt, H.; Olze, H.; Szczepek, A.J.; Mazurek, B. Gender and Chronic Tinnitus: Differences in Tinnitus-Related Distress Depend on Age and Duration of Tinnitus. Ear Hear. 2013, 34, 661–672. [Google Scholar] [CrossRef]
- Cederroth, C.R.; Kähler, A.K.; Sullivan, P.F.; Lopez-Escamez, J.A. Genetics of Tinnitus: Time to Biobank Phantom Sounds. Front. Genet. 2017, 8, 110. [Google Scholar] [CrossRef]
- Cederroth, C.R.; Schlee, W. Editorial: Sex and Gender Differences in Tinnitus. Front. Neurosci. 2022, 16, 844267. [Google Scholar] [CrossRef]
- Basso, L.; Boecking, B.; Brueggemann, P.; Pedersen, N.L.; Canlon, B.; Cederroth, C.R.; Mazurek, B. Chapter 3—Subjective hearing ability, physical and mental comorbidities in individuals with bothersome tinnitus in a Swedish population sample. In Progress in Brain Research; Schlee, W., Langguth, B., Kleinjung, T., Vanneste, S., De Ridder, D., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; Volume 260, pp. 51–78. [Google Scholar]
- Boecking, B.; Rose, M.; Brueggemann, P.; Mazurek, B. Two birds with one stone.–Addressing depressive symptoms, emotional tension and worry improves tinnitus-related distress and affective pain perceptions in patients with chronic tinnitus. PLoS ONE 2021, 16, e0246747. [Google Scholar] [CrossRef] [PubMed]
- Brueggemann, P.; Mebus, W.; Boecking, B.; Amarjargal, N.; Niemann, U.; Spiliopoulou, M.; Dobel, C.; Rose, M.; Mazurek, B. Dimensions of Tinnitus-Related Distress. Brain Sci. 2022, 12, 275. [Google Scholar] [CrossRef] [PubMed]
- Niemann, U.; Brueggemann, P.; Boecking, B.; Mebus, W.; Rose, M.; Spiliopoulou, M.; Mazurek, B. Phenotyping chronic tinnitus patients using self-report questionnaire data: Cluster analysis and visual comparison. Sci. Rep. 2020, 10, 16411. [Google Scholar] [CrossRef] [PubMed]

| I. Immune activity | |
| Cellular immune response | Increase ↑: MPV (related to HFHL) [12], PDW, PC, 11-dTxB2 [13] |
Inflammation direct | Increase ↑: IL-1α (related to tonal tinnitus), IL-1, IL-2, TNF-α [14,15] Decrease ↓: IL-10, HSP-70, CD16NK, CD19 (related to ACTH) [16] |
| Inflammation indirect | Increase ↑: NLR (related to HFHL-TN), PLR, CRP, ESR [17,18] |
| II. Oxidative parameters | |
| Increase ↑: GST, GSH, MDA [19], TAS, TOS OSI [20,21] | |
| III. Metabolism | |
| Lipid metabolism | Increase ↑: TC, TG, or TRG, LDL [22] Decrease ↓: HDL [23] |
| Marker (Unit) | Female (N = 102) Mean (± St. Dev.) | Male (N = 98) Mean (± St. Dev.) | Total (N = 200) Mean (± St. Dev.) |
|---|---|---|---|
| Basophils (absolute/nL) | 0.0443 (±0.0204) | 0.0523 (±0.0242) | 0.0482 (±0.0226) |
| Eosinophils (absolute/nL) | 0.125 (±0.0875) | 0.158 (±0.111) | 0.141 (±0.101) |
| Immat. gran. (absolute/nL) | 0.0220 (±0.0134) | 0.0284 (±0.0196) | 0.0251 (±0.0170) |
| Leukocytes (absolute/nL) | 6.48 (±1.51) | 6.82 (±1.88) | 6.65 (±1.71) |
| Lymphocytes (absolute/nL) | 2.00 (±0.647) | 1.97 (±0.561) | 1.98 (±0.606) |
| Monocytes (absolute/nL) | 0.481 (±0.148) | 0.568 (±0.170) | 0.523 (±0.164) |
| Neutrophils (absolute/nL) | 3.83 (±1.22) | 4.02 (±1.47) | 3.93 (±1.34) |
| NLR (ratio) | 2.12 (±0.984) | 2.17 (±0.909) | 2.14 (±0.946) |
| IL6 (ng/L) | 2.88 (±11.8) | 2.12 (±1.69) | 2.51 (±8.53) |
| TNF-α (pg/mL) | 0.511 (±1.95) | 0.348 (±0.329) | 0.431 (±1.41) |
| CRP (mg/L) | 1.88 (±2.29) | 1.79 (±2.40) | 1.83 (±2.34) |
| Ferritin (μg/L) | 88.5 (±57.4) | 177 (±114) | 132 (±99.9) |
| Fibrinogen (g/L) | 2.72 (±0.581) | 2.72 (±0.568) | 2.72 (±0.573) |
| MPV (fl) | 10.6 (±0.899) | 10.7 (±1.09) | 10.7 (±0.998) |
| Thrombocytes (nL) | 256 (±58.9) | 232 (±46.5) | 244 (±54.3) |
| Erythrocytes (pL) | 4.56 (±0.331) | 5.10 (±0.361) | 4.83 (±0.439) |
| Haematocrit (L/L) | 0.404 (±0.0258) | 0.449 (±0.0279) | 0.426 (±0.0351) |
| Hemoglobin (g/dL) | 13.6 (±0.771) | 15.3 (±0.994) | 14.4 (±1.24) |
| MCH (pg) | 29.8 (±1.31) | 30.0 (±1.35) | 29.9 (±1.33) |
| MCHC (g/dL) | 33.6 (±0.930) | 34.0 (±0.915) | 33.8 (±0.944) |
| MCV (fL) | 88.6 (±3.49) | 88.1 (±3.70) | 88.3 (±3.60) |
| RDW-CV (%) | 12.9 (±0.904) | 12.8 (±0.590) | 12.8 (±0.768) |
| Lipid Peroxidase (μmol/L) | 110 (±158) | 40.8 (±59.2) | 75.8 (±125) |
| SOD1 (ng/mL) | 63.3 (±2.25) | 68.0 (±19.3) | 65.6 (±13.8) |
| SOD2 (ng/mL) | 52.7 (±13.6) | 65.4 (±14.8) | 58.9 (±15.5) |
| Q10 (μmol/mmol) | 0.220 (±0.0617) | 0.250 (±0.0793) | 0.235 (±0.0722) |
| Cholesterol (mg/dL) | 219 (±40.7) | 207 (±39.3) | 213 (±40.4) |
| HDL (mg/dL) | 73.2 (±18.0) | 52.8 (±11.8) | 63.2 (±18.3) |
| LDL (mg/dL) | 138 (±37.8) | 138 (±34.6) | 138 (±36.2) |
| Lipoprotein (a) (nmol/L) | 59.6 (±80.5) | 38.0 (±55.7) | 49.0 (±70.1) |
| Non-HDL (mg/dL) | 146 (±42.0) | 154 (±39.3) | 150 (±40.8) |
| Triglyceride (mg/dL) | 109 (±53.3) | 142 (±71.8) | 126 (±65.0) |
| Albumin (g/L) | 46.3 (±2.38) | 46.4 (±2.63) | 46.4 (±2.50) |
| Gamma-GT (U/L) | 19.8 (±11.2) | 32.0 (±18.4) | 25.8 (±16.3) |
| GOT (U/L) | 22.8 (±5.23) | 28.3 (±10.7) | 25.5 (±8.78) |
| GPT (U/L) | 22.8 (±10.1) | 35.4 (±21.0) | 29.0 (±17.6) |
| Creatinine (mg/dL) | 0.755 (±0.0967) | 0.954 (±0.136) | 0.852 (±0.154) |
| GFR (ml/min) | 84.9 (±7.94) | 83.9 (±8.99) | 84.4 (±8.46) |
| Uric acid (mg/dL) | 4.21 (±0.923) | 6.13 (±3.14) | 5.15 (±2.49) |
| Calcium (mmol/L) | 2.34 (±0.0985) | 2.34 (±0.0805) | 2.34 (±0.0899) |
| Magnesium (mmol/L) | 0.842 (±0.0543) | 0.849 (±0.0541) | 0.845 (±0.0542) |
| Selenium (μmol/L) | 1.02 (±0.220) | 1.01 (±0.239) | 1.01 (±0.229) |
| Vitamin D3 (nmol/L) | 67.6 (±25.8) | 66.9 (±24.0) | 67.2 (±24.9) |
| Zinc (μmol/L) | 12.4 (±1.67) | 13.0 (±2.03) | 12.7 (±1.88) |
| D-dimer (mg/L) | 0.386 (±0.502) | 0.435 (±1.31) | 0.410 (±0.985) |
| Telomere length (ratio) | 1.15 (±0.248) | 1.12 (±0.267) | 1.14 (±0.257) |
| Variable | Total (N = 200) Mean (± St. Dev.)/Freq. (Prop.) |
|---|---|
| HT (right) | 26.3 (±13.6) dB |
| HT (left) | 27.6 (±13.0) dB |
| TF (right) Not measured TF (left) Not measured TL | 6040 (±2260) Hz 99 (49.5%) 5760 (±2550) Hz 94 (47.0%) 47.3 (±20.4) dB |
| Not measured | 62 (31.0%) |
| SL | 6.59 (±5.71) dB |
| Not measured | 62 (31.0%) |
| TQ | 43.8 (±19.0) |
| Age | 54.7 (±8.44) years |
| Sex | |
| Female | 102 (51%) |
| Male | 98 (49%) |
| Term | Estimate | Std. Error | t-Statistic | p-Value |
|---|---|---|---|---|
| (Intercept) | −7.11 | 1.73 | −4.10 | <0.001 |
| Age | 0.17 | 0.03 | 5.38 | <0.001 |
| Log (Vitamin D3) | 2.14 | 0.42 | 5.06 | <0.001 |
| Sex | 0.13 | 0.05 | 2.86 | 0.005 |
| Age:log (Vitamin D3) | −0.04 | 0.01 | −4.57 | <0.001 |
| Term | Estimate | Std. Error | t-Statistic | p-Value |
|---|---|---|---|---|
| (Intercept) | −48.44 | 20.15 | −2.40 | 0.018 |
| Age | 0.74 | 0.20 | 3.79 | <0.001 |
| Log (Vitamin D3) | 13.52 | 4.47 | 3.02 | 0.003 |
| Term | Estimate | Std. Error | t-Statistic | p-Value |
|---|---|---|---|---|
| (Intercept) | 11.95 | 2.67 | 4.47 | <0.001 |
| Sex | 2.65 | 1.14 | 2.32 | 0.022 |
| Log (Uric acid) | −4.46 | 1.80 | −2.48 | 0.014 |
| Term | Estimate | Std. Error | t-Statistic | p-Value |
|---|---|---|---|---|
| (Intercept) | −43.15 | 30.70 | −1.41 | 0.161 |
| Erythrocytes | 58.60 | 20.21 | 2.90 | 0.004 |
| Sex | −9.76 | 3.65 | −2.67 | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bulla, J.; Brueggemann, P.; Wrzosek, M.; Klasing, S.; Boecking, B.; Basso, L.; Nyamaa, A.; Psatha, S.; Rose, M.; Mazurek, B. Limited Link of Common Blood Parameters with Tinnitus. J. Clin. Med. 2023, 12, 3814. https://doi.org/10.3390/jcm12113814
Bulla J, Brueggemann P, Wrzosek M, Klasing S, Boecking B, Basso L, Nyamaa A, Psatha S, Rose M, Mazurek B. Limited Link of Common Blood Parameters with Tinnitus. Journal of Clinical Medicine. 2023; 12(11):3814. https://doi.org/10.3390/jcm12113814
Chicago/Turabian StyleBulla, Jan, Petra Brueggemann, Małgorzata Wrzosek, Sven Klasing, Benjamin Boecking, Laura Basso, Amarjargal Nyamaa, Stamatina Psatha, Matthias Rose, and Birgit Mazurek. 2023. "Limited Link of Common Blood Parameters with Tinnitus" Journal of Clinical Medicine 12, no. 11: 3814. https://doi.org/10.3390/jcm12113814
APA StyleBulla, J., Brueggemann, P., Wrzosek, M., Klasing, S., Boecking, B., Basso, L., Nyamaa, A., Psatha, S., Rose, M., & Mazurek, B. (2023). Limited Link of Common Blood Parameters with Tinnitus. Journal of Clinical Medicine, 12(11), 3814. https://doi.org/10.3390/jcm12113814







