Mental Fatigue in Patients with Hearing Loss and/or Tinnitus Undergoing Audiological Rehabilitation—A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. A Self-Assessment Questionnaire for Mental Fatigue—MFS
2.3. Tinnitus Handicap Inventory (THI)
2.4. Statistical Analysis
3. Results
3.1. Demographic Data of All Included Subjects Stratified by Gender
3.2. Hearing Aids and Cochlear Implants (CIs)
3.3. Demographic Data Stratified by MFS Level: 10.5–15, 15.5–20, and ≥20.5
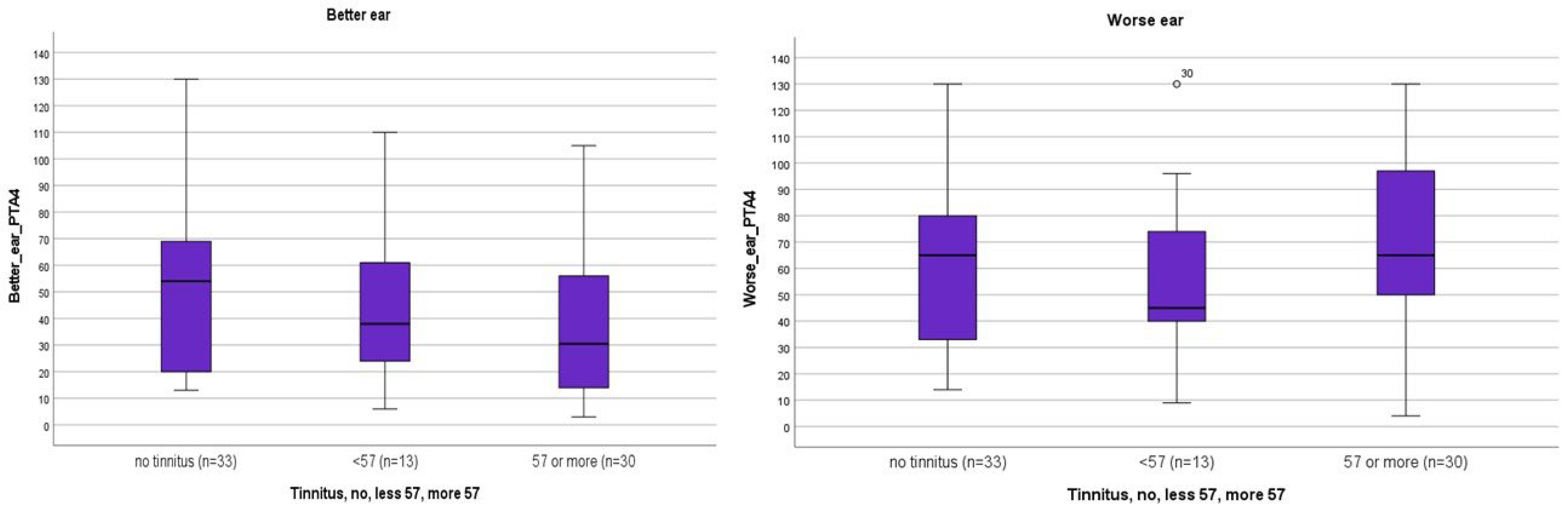
3.4. Hearing Thresholds for the Entire Study Group in the Better and Worse Ear, with or without Tinnitus
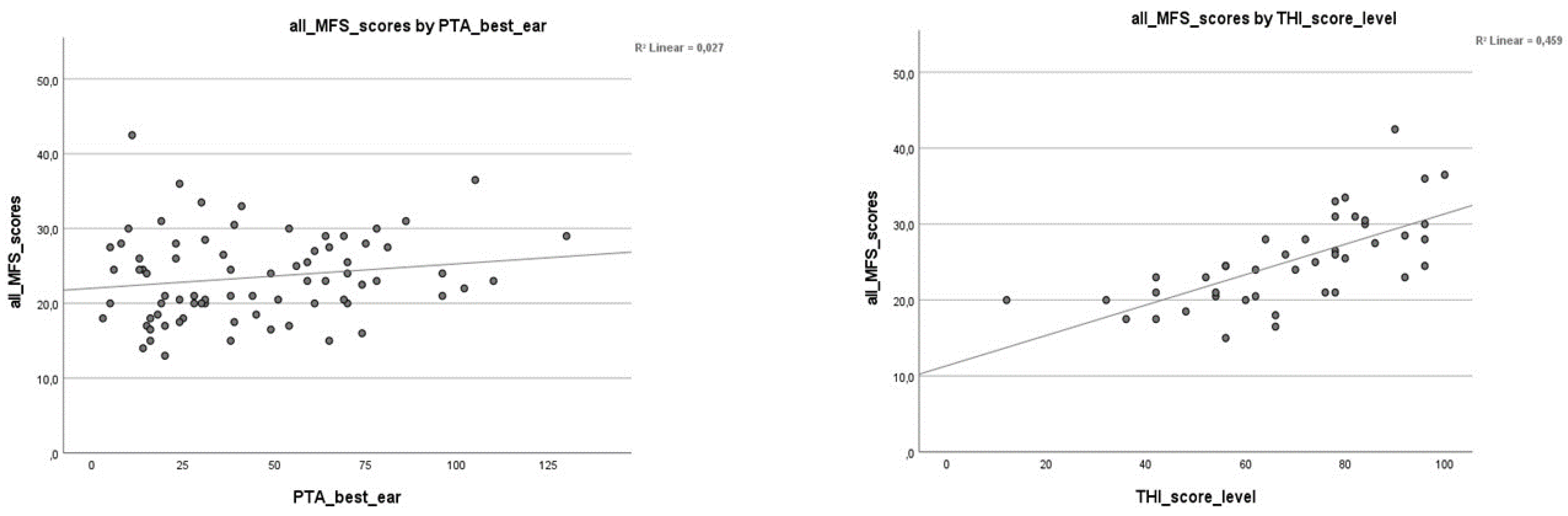
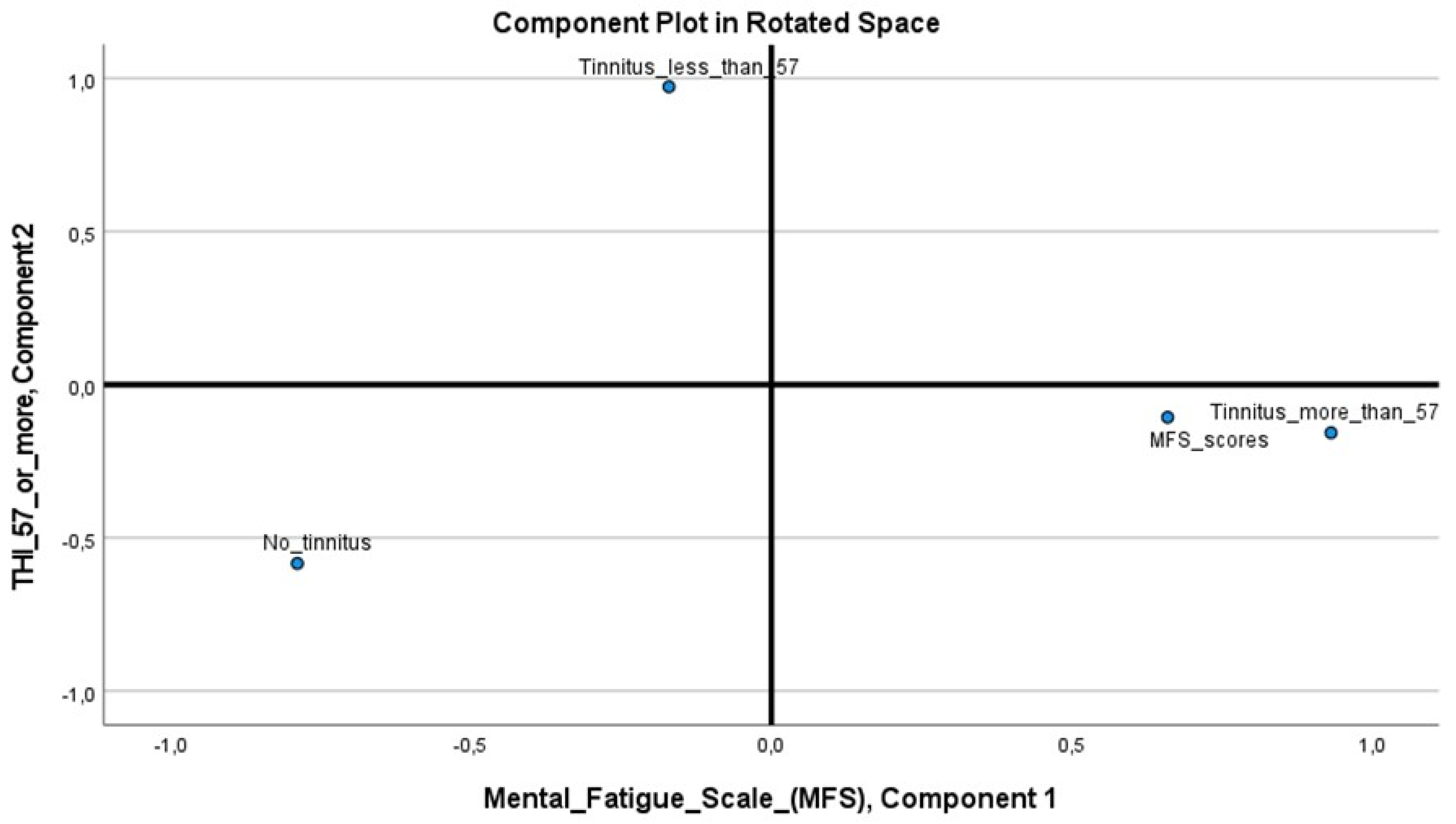
3.5. Correlation Analysis on Variables MFS, PTA4, and THI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD. Hearing loss prevalence and years lived with disability, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet 2021, 397, 996–1009. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Hearing. 2021. Available online: https://www.who.int/publications/i/item/world-report-on-hearing (accessed on 15 April 2020).
- Mick, P.; Kawachi, I.; Lin, F.R. The association between hearing loss and social isolation in older adults. Otolaryngol.–Head Neck Surg. 2014, 150, 378–384. [Google Scholar] [CrossRef]
- Carlsson, P.-I.; Hall, M.; Lind, K.-J.; Danermark, B. Quality of life, psychosocial consequences, and audiological rehabilitation after sudden sensorineural hearing loss. Int. J. Audiol. 2011, 50, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Li, C.M.; Zhang, X.; Hoffman, H.J.; Cotch, M.F.; Themann, C.L.; Wilson, M.R. Hearing impairment associated with depression in US adults, National Health and Nu-trition Examination Survey 2005–2010. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 293–302. [Google Scholar] [CrossRef]
- Andersson, G.; McKenna, L. The role of cognition in tinnitus. Acta Oto-Laryngol. 2006, 126, 39–43. [Google Scholar] [CrossRef]
- Nondahl, D.M.; Cruickshanks, K.J.; Dalton, D.S.; Klein, B.E.; Klein, R.; Schubert, C.R.; Tweed, T.S.; Wiley, T.L. The Impact of Tinnitus on Quality of Life in Older Adults. J. Am. Acad. Audiol. 2007, 18, 257–266. [Google Scholar] [CrossRef]
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- McCormack, A.; Edmondson-Jones, M.; Somerset, S.; Hall, D. A systematic review of the reporting of tinnitus prevalence and severity. Hear. Res. 2016, 337, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, B.; Böcking, B.; Dobel, C.; Rose, M.; Brüggemann, P. Tinnitus and Influencing Comorbidities. Laryngo-Rhino-Otologie 2023, 102, S50–S58. [Google Scholar] [PubMed]
- Staub, F.; Bogousslavsky, J. Fatigue after Stroke: A Major but Neglected Issue. Cerebrovasc. Dis. 2001, 12, 75–81. [Google Scholar] [CrossRef]
- Johansson, B.; Starmark, A.; Berglund, P.; Rödholm, M.; Rönnbäck, L. A self-assessment questionnaire for mental fatigue and related symptoms after neurological disorders and injuries. Brain Inj. 2010, 24, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Johansson, B.; Rönnbäck, L. Mental Fatigue and Cognitive Impairment after an Almost Neurological Recovered Stroke. ISRN Psychiatry 2012, 2012, 686425. [Google Scholar] [CrossRef] [PubMed]
- Moore, T.M.; Key, A.P.; Thelen, A.; Hornsby, B.W. Neural mechanisms of mental fatigue elicited by sustained auditory processing. Neuropsychologia 2017, 106, 371–382. [Google Scholar] [CrossRef]
- Hornsby, B.W.Y. The Effects of Hearing Aid Use on Listening Effort and Mental Fatigue Associated With Sustained Speech Processing Demands. Ear Hear. 2013, 34, 523–534. [Google Scholar] [CrossRef]
- Hornsby, B.W.Y.; Kipp, A.M. Subjective Ratings of Fatigue and Vigor in Adults with Hearing Loss Are Driven by Perceived Hearing Difficulties Not Degree of Hearing Loss. Ear Hear. 2016, 37, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.C. Speech processing for the hearing-impaired: Successes, failures, and implications for speech mechanisms. Speech Commun. 2003, 41, 81–91. [Google Scholar] [CrossRef]
- Jahncke, H.; Halin, N. Performance, fatigue and stress in open-plan offices: The effects of noise and restoration on hearing im-paired and normal hearing individuals. Noise Health 2012, 14, 260–272. [Google Scholar] [CrossRef]
- Rödholm, M.; Starmark, J.-E.; Svensson, E.; Von Essen, C. Astheno-emotional disorder after aneurysmal SAH: Reliability, symptomatology and relation to outcome. Acta Neurol. Scand. 2001, 103, 379–385. [Google Scholar] [CrossRef]
- Turunen-Taheri, S.; Carlsson, P.I.; Johnson, A.C.; Hellström, S. Severe-to-profound hearing impairment: Demographic data, gender dif-ferences and benefits of audiological rehabilitation. Disabil. Rehabil. 2019, 41, 2766–2774. [Google Scholar] [CrossRef]
- Johansson, B.; Rönnbäck, L. Long-Lasting Mental Fatigue After Traumatic Brain Injury—A Major Problem Most Often Neglected Diagnostic Criteria, Assessment, Relation to Emotional and Cognitive Problems, Cellular Background, and Aspects on Treatment. In Traumatic Brain Injury; Intech Open: London, UK, 2014. [Google Scholar]
- Johansson, B.; Rönnbäck, L. Evaluation of the Mental Fatigue Scale and its relation to Cognitive and Emotional Functioning after Traumatic Brain Injury or Stroke. Int. J. Phys. Med. Rehabil. 2014, 2, 182. [Google Scholar]
- Johansson, B.; Rönnbäck, L. När Hjärnan Inte Orkar: Om Hjärntrötthet; Recito Förlag: Sundered, Sweden, 2014. [Google Scholar]
- Newman, C.W.; Jacobson, G.P.; Spitzer, J.B. Development of the Tinnitus Handicap Inventory. Arch. Otolaryngol. Head Neck Surg. 1996, 122, 143–148. [Google Scholar] [CrossRef]
- McCombe, A.; Baguley, D.; Coles, R.; McKenna, L.; McKinney, C.; Windle-Taylor, P. Guidelines for the grading of tinnitus severity: The results of a working group commis-sioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999. Clin. Otolaryngol. Allied Sci. 2001, 26, 388–393. [Google Scholar] [CrossRef]
- Austin, P.C.; Steyerberg, E.W. The number of subjects per variable required in linear regression analyses. J. Clin. Epidemiol. 2015, 68, 627–636. [Google Scholar] [CrossRef]
- Hornsby, B.W.Y.; Camarata, S.; Cho, S.-J.; Davis, H.; McGarrigle, R.; Bess, F.H. Development and validation of the Vanderbilt Fatigue Scale for Adults (VFS-A). Psychol. Assess. 2021, 33, 777–788. [Google Scholar] [CrossRef]
- Holman, J.A.; Drummond, A.; Naylor, G. The Effect of Hearing Loss and Hearing Device Fitting on Fatigue in Adults: A Systematic Review. Ear Hear. 2020, 42, 1–11. [Google Scholar] [CrossRef]
- Hornsby, B.W.Y.; Naylor, G.; Bess, F.H. A Taxonomy of Fatigue Concepts and Their Relation to Hearing Loss. Ear Hear. 2016, 37 (Suppl. 1), 136S–144S. [Google Scholar] [CrossRef]
- Backenroth, G.A.M.; Ahlner, B.H. Quality of life of hearing-impaired persons who have participated in audiological rehabilitation counselling. Int. J. Adv. Couns. 2000, 22, 225–240. [Google Scholar] [CrossRef]
- Nachtegaal, J.; Smit, J.H.; Smits, C.; Bezemer, P.D.; van Beek, J.H.M.; Festen, J.M.; Kramer, S.E. The Association Between Hearing Status and Psychosocial Health Before the Age of 70 Years: Results From an Internet-Based National Survey on Hearing. Ear Hear. 2009, 30, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Hétu, R.; Riverin, L.; Lalande, N.; Getty, L.; St-Cyr, C. Qualitative analysis of the handicap associated with occupational hearing loss. Br. J. Audiol. 1988, 22, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.; Schlundt, D.; Bonnet, K.; Camarata, S.; Bess, F.H.; Hornsby, B. Understanding Listening-Related Fatigue: Perspectives of Adults with Hearing Loss. Int. J. Audiol. 2021, 60, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, P.-I.; Hjaldahl, J.; Magnuson, A.; Ternevall, E.; Edén, M.; Skagerstrand, J.R. Severe to profound hearing impairment: Quality of life, psychosocial consequences and audiological rehabilitation. Disabil. Rehabil. 2015, 37, 1849–1856. [Google Scholar] [CrossRef] [PubMed]

| Total | Male | Female | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Gender; total | 76 (100) | 23 (30.5) | 53 (69.5) |
| Age (years), | 52.55 | 52.09 | 52.75 |
| Mean (±SD) | (6.06) | (6.09) | (6.10) |
| Range (years) | 38–65 | 43–65 | 38–63 |
| Civil status, living alone a | 18 (23.5) | 6 (33.3) | 12 (66.7) |
| Age groups (years) | |||
| 19–30 | 0 (0) | 0 (0) | 0 (0) |
| 31–40 | 3 (4) | 0 (0) | 3 (6) |
| 41–50 | 25 (33) | 9 (39) | 16 (30) |
| 51–60 | 37 (48.5) | 11 (48) | 26 (49) |
| 61–70 | 11(14.5) | 3 (13) | 8 (15) |
| Degree of hearing loss, better ear | |||
| 0–25 dB HL b | 28 (37) | 6 (26) | 22 (41.5) |
| 26–40 dB HL | 13 (17) | 3 (13) | 10 (19) |
| 41–70 dB HL | 22 (29) | 8 (35) | 14 (26.5) |
| 71–90 dB HL | 7 (9) | 4 (17.5) | 3 (5.5) |
| 91–130 dB HL | 6 (8) | 2 (8.5) | 4 (7.5) |
| Tinnitus; THI c < 57 | 13 (17) | 7 (30) | 6 (11.5) |
| Tinnitus; THI c ≥ 57 | 30 (39.5) | 8 (35) | 22 (41.5) |
| No tinnitus | 33 (43.5) | 8 (35) | 25 (47) |
| Extended audiological rehabilitation d | 68 (89.5) | 22 (32.5) | 46 (67.5) |
| Total | MFS Score | MFS Score | MFS Score | |
|---|---|---|---|---|
| 10.5–15 | 15.5–20 | ≥20.5 | ||
| n (%) | n (%) | n (%) | n (%) | |
| Gender; total | 76 | 5 (6.5) | 20 (26.5) | 51 (67) a |
| Female | 53 (69.5) | 4 (7.5) | 13 (24.5) | 36 (68) |
| Male | 23 (30.5) | 1 (4.5) | 7 (30.5) | 15 (65) |
| Age (years) | ||||
| Mean (±SD) | 52.55 (6.06) | 53.80 (4.76) | 53.65 (6.18) | 52.00 (6.15) |
| Range (years) | 38–65 | 49–60 | 38–63 | 38–65 |
| Civil status, living alone b | 18 (23.5) | 2 (11) | 4 (22) | 12 (67) |
| Age groups | ||||
| (years) | ||||
| 19–30 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 31–40 | 3 (4) | 0 (0) | 1 (5) | 2 (4) |
| 41–50 | 25 (33) | 2 (40) | 3 (15) | 20 (39) |
| 51–60 | 37 (48.5) | 3 (60) | 12 (60) | 22 (43) |
| 61–70 | 11 (14.5) | 0 (0) | 4 (20) | 7 (14) |
| Degree of hearing loss, better ear c | ||||
| 0–25 dB HL | 28 (37) | 2 (40) | 9 (45) | 17 (33.5) |
| 26–40 dB HL | 13 (17) | 1 (20) | 1 (5) | 11 (21.5) |
| 41–70 dB HL | 22 (29) | 1 (20) | 5 (25) | 16 (31.5) |
| 71–90 dB HL | 7 (9) | 1 (20) | 2 (10) | 4 (7.5) |
| 91–130 dB HL | 6 (8) | 0 (0) | 3 (15) | 3 (6) |
| Occupation | ||||
| Unemployed | 7 (9) | 1 (20) | 1 (5) | 5 (10) |
| Working | 68 (89.5) | 4 (80) | 19 (95) | 45 (88) |
| Sick leave permanent | 1 (1.5) | 0 (0) | 0 (0) | 1 (2) |
| Sick leave d | 44 (58) | 2 (4.5) | 14 (32) | 28 (63.5) |
| Sick leave e | 73 (96) | 4 (5.5) | 20 (27.5) | 49 (67) |
| Tinnitus; THI f < 57 | 13 (17) | 1 (20) | 5 (25) | 7 (13.5) |
| Tinnitus; THI f ≥ 57 | 30 (39.5) | 0 (0) | 3 (15) | 27 (53) |
| No tinnitus | 33 (43.5) | 4 (80) | 12 (60) | 17 (33.5) |
| Extended audiological rehabilitation g | 68 (89.5) | 4 (6) | 17 (25) | 47 (69) |
| PTA4 a Better Ear | Tinnitus b | |
|---|---|---|
| (THI) | ||
| n = 76 | n = 76 | |
| MFS all scores | ||
| Pearson’s R | 0.165 | 0.677 ** |
| 95% CI | (−0.091–0.389) | (0.564–0.790) |
| p-value | 0.153 | 0.000 ** |
| MFS mild (10.5–15) | ||
| Pearson’s R | −0.155 | −0.222 |
| 95% CI | (−0.296–0.009) | (−0.367—0.079) |
| p-value | 0.182 | 0.054 |
| MFS moderate (15.5–20) | ||
| Pearson’s R | −0.231 * | −0.270 * |
| 95% CI | (−0.396−0.032) | (−0.480—0.065) |
| p-value | 0.045 * | 0.018 * |
| MFS severe (20.5 or more) | ||
| Pearson’s R | 0.298 ** | 0.370 ** |
| 95% CI | (0.116–0.460) | (0.164–0.559) |
| p-value | 0.009 ** | 0.001 ** |
| THI ≥ 57 n = 30 | THI < 57 n = 13 | No Tinnitus n = 33 | |
|---|---|---|---|
| MFS scores a | |||
| 10.5–15 mean rank (n = 5) | 23.50 | 39.60 | 52.40 |
| 15.5–20 mean rank (n = 20) | 29.20 | 41.50 | 44.80 |
| 20.5 > mean rank (n = 51) | 43.62 | 37.22 | 34.67 |
| p-value b | 0.002 ** | 0.521 | 0.030 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turunen-Taheri, S.; Carlsson, P.-I.; Ternevall, E.; Hellström, S. Mental Fatigue in Patients with Hearing Loss and/or Tinnitus Undergoing Audiological Rehabilitation—A Pilot Study. J. Clin. Med. 2023, 12, 6756. https://doi.org/10.3390/jcm12216756
Turunen-Taheri S, Carlsson P-I, Ternevall E, Hellström S. Mental Fatigue in Patients with Hearing Loss and/or Tinnitus Undergoing Audiological Rehabilitation—A Pilot Study. Journal of Clinical Medicine. 2023; 12(21):6756. https://doi.org/10.3390/jcm12216756
Chicago/Turabian StyleTurunen-Taheri, Satu, Per-Inge Carlsson, Elisabeth Ternevall, and Sten Hellström. 2023. "Mental Fatigue in Patients with Hearing Loss and/or Tinnitus Undergoing Audiological Rehabilitation—A Pilot Study" Journal of Clinical Medicine 12, no. 21: 6756. https://doi.org/10.3390/jcm12216756
APA StyleTurunen-Taheri, S., Carlsson, P.-I., Ternevall, E., & Hellström, S. (2023). Mental Fatigue in Patients with Hearing Loss and/or Tinnitus Undergoing Audiological Rehabilitation—A Pilot Study. Journal of Clinical Medicine, 12(21), 6756. https://doi.org/10.3390/jcm12216756







