Locoregional Flaps for the Reconstruction of Midface Skin Defects: A Collection of Key Surgical Techniques
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Review
2.2. Study Selection
2.3. Surgical Techniques Data Extraction
3. Results
Surgical Techniques Collection
- Bilobed flap: the bilobed flap (BF) is a single pedicle random pattern cutaneous transposition flap composed of two lobes. Its applications are various, including the hand, scalp, foot, and eyelids, but its main adoption is in nasal reconstruction for its excellent color and texture match with adjacent skin. The BF is used for small nasal defects (1.5 cm). Nasal ala defects are approached with a medially based flap, while tip defects are approached with a laterally based one. The surgical technique requires precise measurements: the first measure is the diameter of the defect (D), then the pivot point is placed at least 0.5 D from the defect; from the pivot point, the outer flap edge is obtained by rotating a suture around the pivot point; an inner arch is marked 0.5 D inside the outer arch; and the first lobe is demarcated with a diameter equal to D, while the second lobe is marked with a width 0.5 higher than D (Figure 1). The dissection is performed above the periosteum and perichondrium. The first lobe covers the excision gap and the second lobe will replace the first lobe, while the gap of the second lobe is closed by direct suture [11].
- 2.
- Rhomboid flap: the rhomboid flap (RF), also known as the Limberg flap, is a transposing rhomboid-shaped flap, used typically for medium-sized defects of the cheek (2–2.5 cm). It can be designed in every direction. The main advantage is that, being adjacent to the defect, it matches the skin color and texture. Its plan is geometrical: the defect is surrounded by a rhomboid with 60° and 120° angles; then, the flap is designed on the short axis (120°), as shown in Figure 2. The Dufourmentel flap is a modification of the Limberg flap and uses angles from 60° to 90° [11,13,14].
- 3.
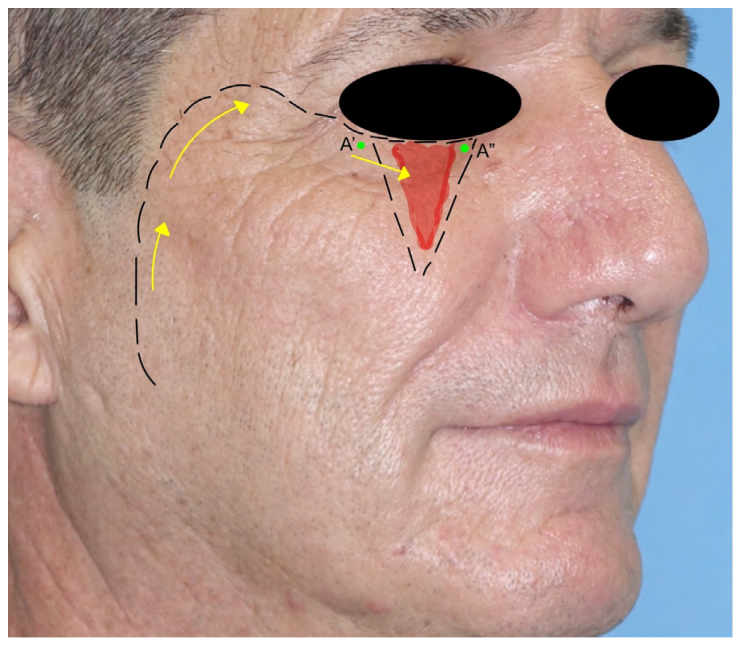
- Facial-artery-based flaps: The nasolabial flap (NLF) is the most adopted advancement flap in the reconstruction of the nasal side wall and ala defects and also cheek and upper lip regions. The NLF is used to cover medium defects close to the flap. It is based on the branches of the facial artery, most commonly on the angular artery. It is triangular-shaped, with the base of the triangle direct to the defect, while the apex is directed toward the pedicle. Once the flap is mobilized, the surgical wound is closed in a V-Y fashion [2,15] (Figure 3A).
- 4.
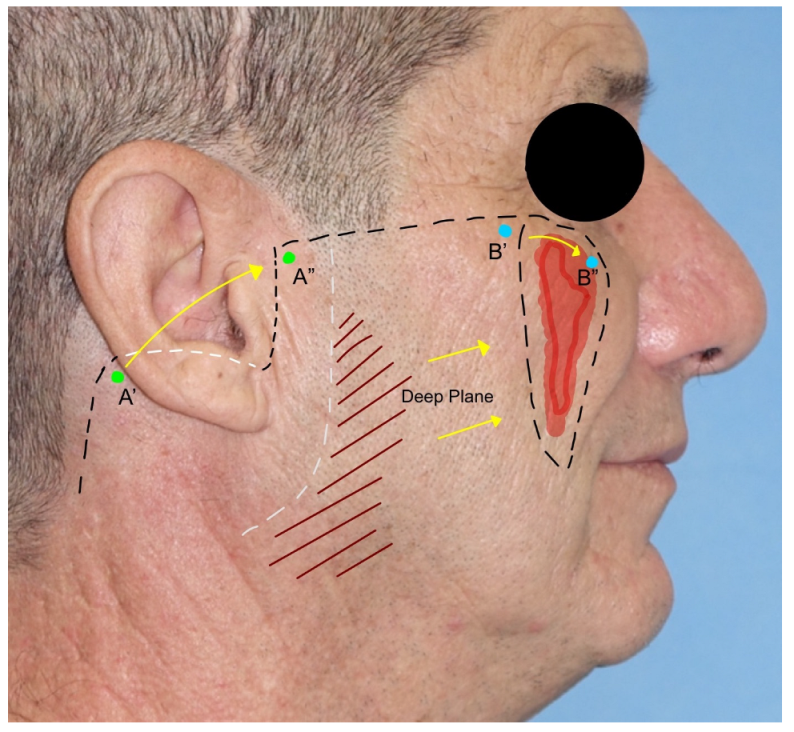
- Cervicofacial flap: the cervicofacial flap is suited for moderate and large (>3 cm) defects of the cheek and is extendible to the periorbital and neck regions. It represents a combination of an advancement and rotational flap that can be moved anteriorly or posteriorly and anteriorly. The incision is a variant of the rhytidectomy approach but continues through the zygomatic arch, the lateral cantus, and the lower eyelid line until the nasolabial groove is reached in its most inferior part. The incision can be prolonged posteriorly, as in a parotidectomy with a horizontal limb. The flap is elevated superficially to the superficial musculoaponeurotic system (SMAS) and the masseteric fascia to avoid facial nerve branch injuries. After rotation and advancement, the donor site is closed by direct suture. Due to the great dimension of the flap, anchoring the flap to the orbital–zygomatic periosteum is necessary [11,17] (Figure 4).
- 5.
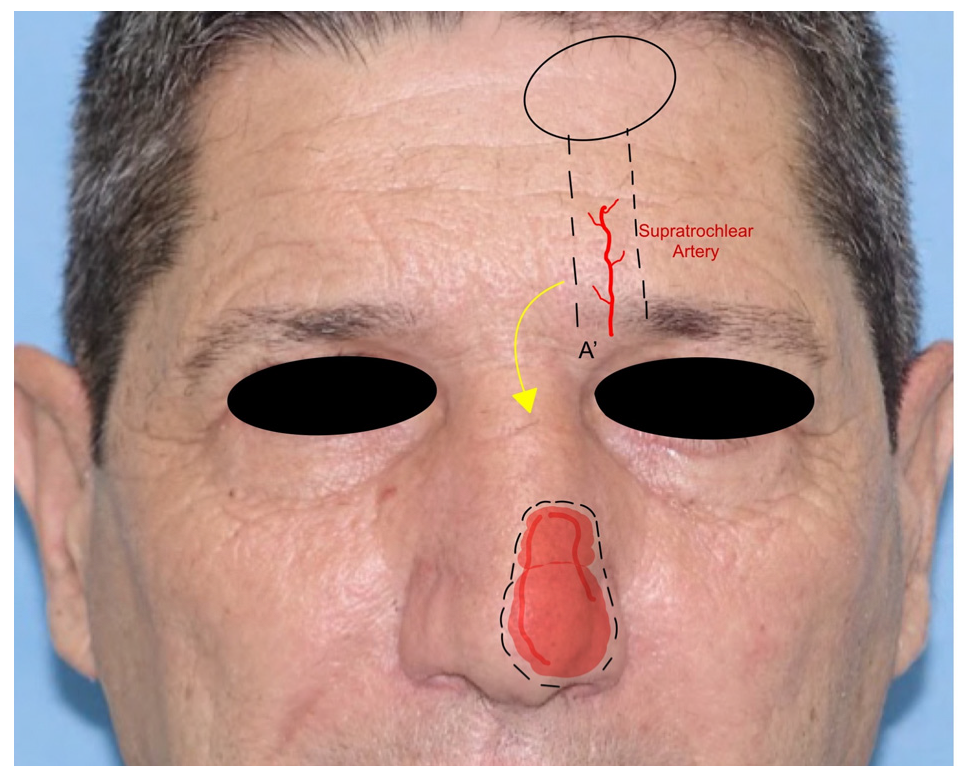
- Paramedian forehead flap: the paramedian forehead flap (PMFF) is an interpolated rotational flap harvested from the forehead and used for reconstructing large and complex defects of the nose. It is harvested based on the blood supply of the supratrochlear artery. The PMFF requires an accurate template of the defect to fill due to the complex three-dimensionality of the nasal region (Figure 4). After the identification of the supratrochlear pedicle by Doppler, the flap is harvested through the skin and subcutaneous muscle in a subfascial plan just above the periosteum. The key to the mobility of the flap is represented by the release of the corrugator muscle. The flap is rotated and then inset in the defect. The PMFF can be associated with cartilage grafting for composite reconstructions. In some variations of the technique, the pedicle is separated in a second stage debulking the flap excess [18] (Figure 5).
- 6.
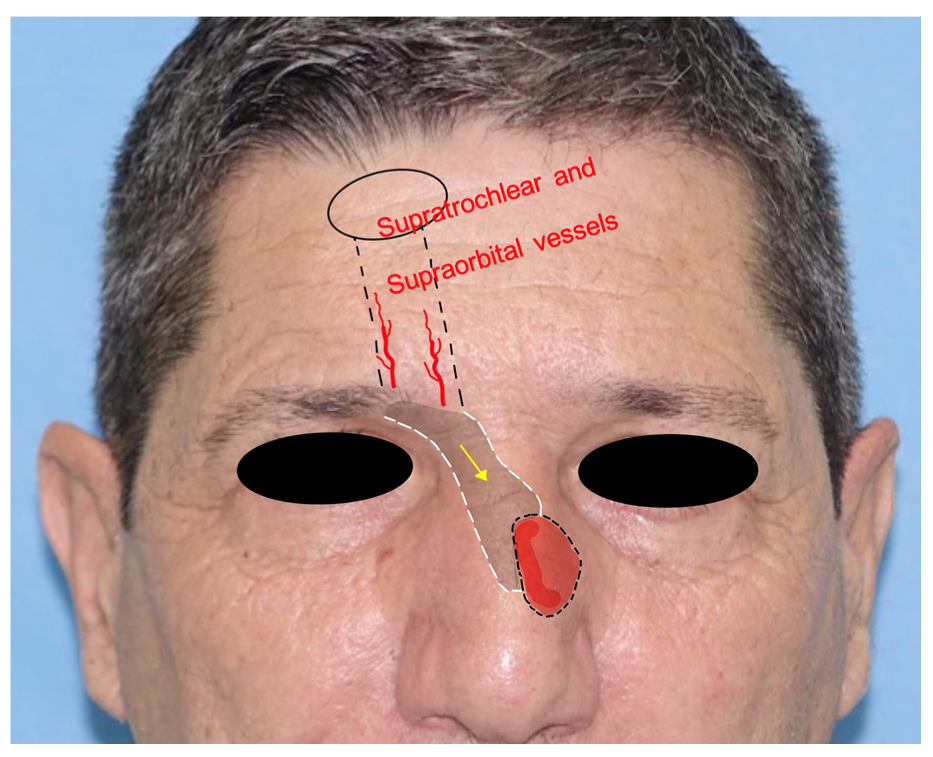
- Frontal hairline island flap: the frontal hairline island flap (FHiF) is a transpositional tunneled island flap harvested from the forehead and nourished by the supraorbital and supratrochlear arteries. It is used for medial canthal, upper nasal dorsum, and nasolabial small–medium defects. The FHiH is harvested in an elliptical shape at the level of the frontal hairline. Once the upper incision is made, the pedicle is dissected subperiosteally toward the orbital rim. The flap is transposed subcutaneously in a tunneled passage to the gap and sutured to the adjacent skin. The donor site is closed by direct suture. This flap represents a tunneled version of the paramedian flap but with indications for smaller skin defects [19] (Figure 6).
- 7.
- Keystone flap: the keystone area flap (KSAF) is a random-pattern multi-perforator advancement flap applicable to all defect dimensions, as it can be performed in all facial subunits. After tumor excision, the flap is islanded to the subcutaneous tissue with the shape of a Roman arch or vault keystone. The ratio between the width of the defect and the flap should be 1:1. The flap should not be undermined to not injure the multiple perforator vessels. It is important to preserve the superficial venous system and to keep intact the deep fascia. It is divided into four categories: type I is the classic keystone flap, type II includes skin grafting, type III is a double classic keystone, and type IV is based on undermining the skin around the keystone flap. The flap is then inserted into the gap and the closure starts with the edge closer to the defect. The longitudinal angles are closed in a V–Y fashion [8,20] (Figure 7).
- 8.
- Karapandzic flap: the Karapandzic flap (KF) is a rotation and advancement flap used in the upper lip and commissure reconstructions of full-thickness defects. It can fill medium and large defects. It is based on the facial artery branches. The KF is often harvested bilaterally with two “L-shaped” opposing flaps, eventually of different lengths. Once the upper lip skin defect has been created, a bull-horn skin excision is made in both alar sulci to increase the advancement of the flaps. The flap dissection is performed gently through the skin and subcutaneous tissue to preserve the vascular pedicle and the neural bundle. The two advancement flaps are moved until they meet centrally. Sutures are made by direct closure [21,22] (Figure 8).
- 9.
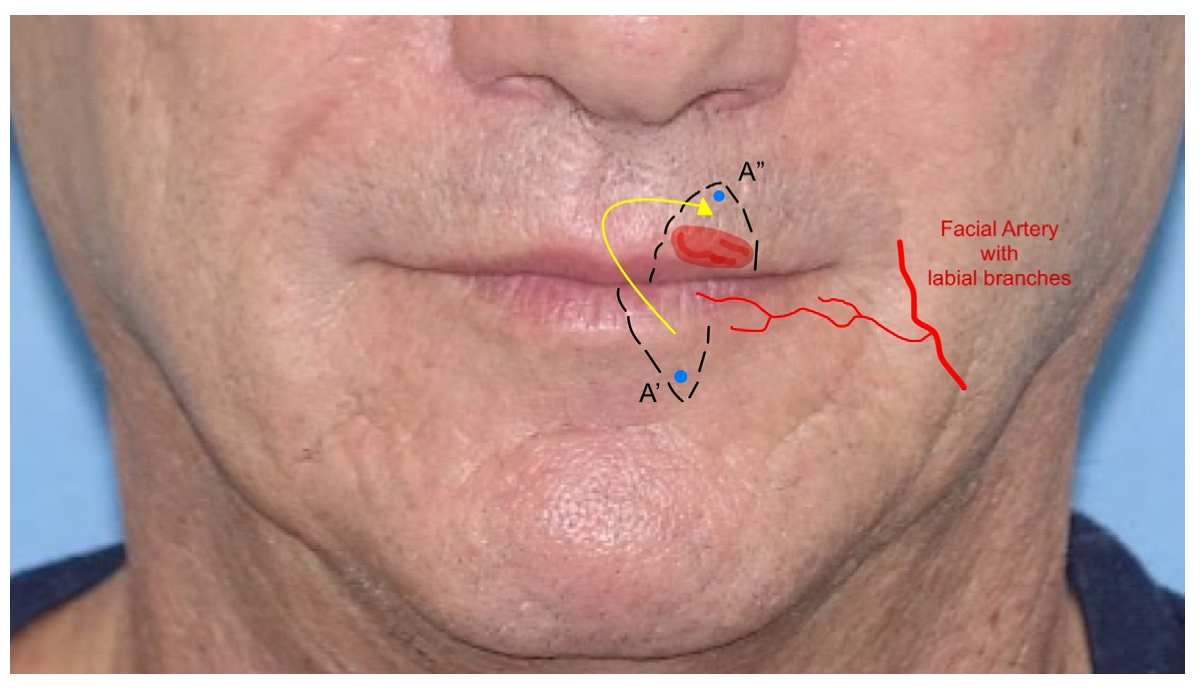
- Abbè flap: the Abbè flap (AF) is a rotational flap usually harvested for the reconstruction of the upper lip. Its indications are defects involving 50% or more of the philtrum and defects of the medial element of the lateral subunit greater than 1.5 cm. The AF is considered a cross-lip switch flap, where the donor site is represented by a quadrangular full-thickness portion of the lower lip, frequently in its center–lateral part. The flap is based on the labial artery, the pedicle of the region, which can be medial or lateral in the flap harvested. The AF amount is calculated based on the defect to fill and then transposed with markers on the lower lip. Once the defect in the upper lip is created, the flap is rotated to fill the gap, while the lower lip is closed primarily. This technique temporarily reduces lip movement and mouth-opening due to the closure. The flap requires a second stage of division where the pedicle is cut and the flap is inserted. The flap can also be harvested for defects in the lower lip [23,24] (Figure 9).
- 10.
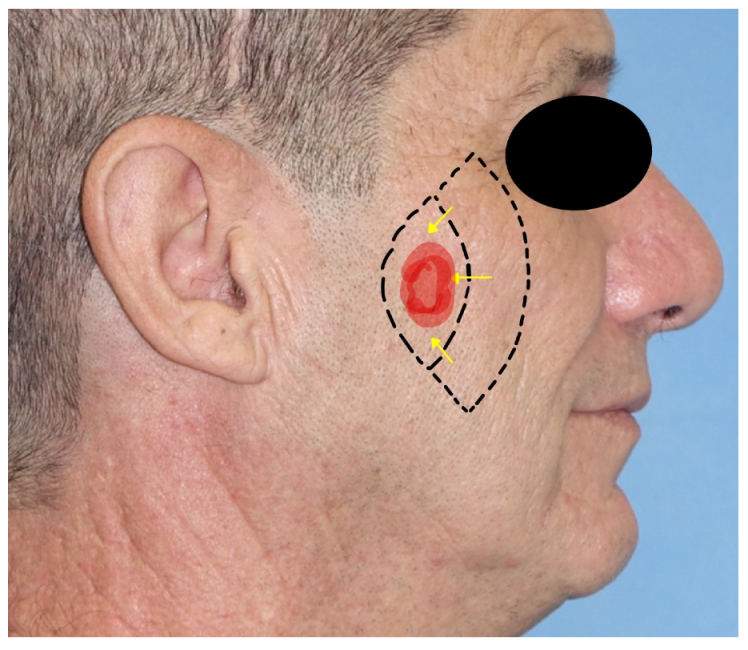
- Mustardè flap: the Mustardè flap is a rotational flap adopted for the reconstruction of large cheek defects, the lateral nose wall, and the lower eyelid region. Its harvesting begins from the edge of the excision defect and extends through the lower eyelid to the lateral canthus and ends with an incision superior and lateral to the temple region. The dissection is performed subcutaneously to not injure any facial nerve branches. As the MF is a flap of great dimensions, anchoring it to the zygomatic arch helps to avoid excessive tension on the flap’s insertion. The donor site is closed by direct suture, with the help of Burow’s triangles [25,26] (Figure 10).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rigby, M.H.; Hayden, R.E. Regional flaps: A move to simpler reconstructive options in the head and neck. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Ercan, A.; Ercan, L.D.; Demiroz, A. Nasolabial Perforator Flap: A Multi-Tool for Reconstruction of Facial Units. J. Craniofac. Surg. 2020, 31, 1042–1045. [Google Scholar] [CrossRef] [PubMed]
- Hammer, D.; Vincent, A.G.; Williams, F.; Ducic, Y. Considerations in Free Flap Reconstruction of the Midface. Facial Plast. Surg. 2021, 37, 759–770. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Ulloa, M. Restoration of the Face Covering by Means of. Br. J. Plast. Surg. 1956, 9, 212–221. [Google Scholar] [CrossRef]
- Nsaful, K.O. The Use of Rotation Flap to Cover a Facial Defect—A Case Study. Mod. Plast. Surg. 2020, 10, 101–107. [Google Scholar] [CrossRef]
- Orabona, G.D.; Maffia, F.; Audino, G.; Abbate, V.; Germano, C.; Bonavolontà, P.; Romano, A.; Villari, R.; Mormile, M.; Califano, L. The Use of Matriderm® for Scalp Full-Thickness Defects Reconstruction: A Case Series. J. Clin. Med. 2022, 11, 6041. [Google Scholar] [CrossRef]
- Gabrysz-Forget, F.; Tabet, P.; Rahal, A.; Bissada, E.; Christopoulos, A.; Ayad, T. Free versus pedicled flaps for reconstruction of head and neck cancer defects: A systematic review. J. Otolaryngol. Head Neck Surg. 2019, 48, 13. [Google Scholar] [CrossRef]
- Yoon, C.S.; Kim, H.B.; Kim, Y.K.; Kim, H.; Kim, K.N. Relaxed skin tension line-oriented keystone-designed perforator island flaps considering the facial aesthetic unit concept for the coverage of small to moderate facial defects. Medicine 2019, 98, e14167. [Google Scholar] [CrossRef]
- Lou, X.; Xue, C.; Molnar, J.A.; Bi, H. A Method to Reproduce Symmetry in Midfacial Reconstruction: A Report of 19 Cases. Adv. Ski. Wound Care 2020, 33, 383–388. [Google Scholar] [CrossRef]
- Seo, Y.-J.; Hwang, C.; Choi, S.; Oh, S.-H. Midface Reconstruction with Various Flaps Based on the Angular Artery. J. Oral Maxillofac. Surg. 2009, 67, 1226–1233. [Google Scholar] [CrossRef]
- Chu, E.A.; Byrne, P.J. Local Flaps I: Bilobed, Rhombic, and Cervicofacial. Facial Plast. Surg. Clin. N. Am. 2009, 17, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Durgun, M.; Özakpinar, H.R.; Sari, E.; Selçuk, C.T.; Seven, E.; Tellioğlu, A.T. The Versatile Facial Artery Perforator-Based Nasolabial Flap in Midface Reconstruction. J. Craniofacial Surg. 2015, 26, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Hon, H.H.; Chandra, S.R. Rhomboid Flap. Atlas Oral Maxillofac. Surg. Clin. 2020, 28, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Limberg, A.A. Mathematical Principles of Local Plastic Procedures on the Surface of the Human Body; Medgis: Leningrad, Russia, 1946. [Google Scholar]
- Cook, T.A.; Israel, J.M.; Wang, T.D.; Murakami, C.S.; Brownrigg, P.J. Cervical rotation flaps for midface resurfacing. Arch. Otolaryngol. Head Neck Surg. 1991, 117, 77–82. [Google Scholar] [CrossRef]
- Pepper, J.-P.; Baker, S.R. Local Flaps: Cheek and Lip Reconstruction. JAMA Facial Plast. Surg. 2013, 15, 374–382. [Google Scholar] [CrossRef]
- Sakellariou, A.; Salama, A. The Use of Cervicofacial Flap in Maxillofacial Reconstruction. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 389–400. [Google Scholar] [CrossRef]
- Smart, R.J.; Yeoh, M.S.; Kim, D.D. Paramedian forehead flap. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 401–410. [Google Scholar] [CrossRef]
- Karṣdağ, S.; Sacak, B.; Bayraktaroglu, S.; Özcan, A.; Ugurlu, K.; Bas, L. A novel approach for the reconstruction of medial canthal and nasal dorsal defects: Frontal hairline Island flap. J. Craniofac. Surg. 2008, 19, 1653–1657. [Google Scholar] [CrossRef]
- Ettinger, K.S.; Fernandes, R.P.; Arce, K. Keystone Flap. Atlas Oral Maxillofac. Surg. Clin. 2019, 28, 29–42. [Google Scholar] [CrossRef]
- Teemul, T.A.; Telfer, A.; Singh, R.P.; Telfer, M.R. The versatility of the Karapandzic flap: A review of 65 cases with patient-reported outcomes. J. Cranio-Maxillofac. Surg. 2016, 45, 325–329. [Google Scholar] [CrossRef]
- Karapandzic, M. Reconstruction of lip defects by local arterial flaps. Br. J. Plast. Surg. 1974, 27, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Luce, E.A.; Jing, X.L.; Carlson, T. Abbe Flap Reconstruction of the Upper Lip. Plast. Reconstr. Surg. 2020, 145, 606e–607e. [Google Scholar] [CrossRef] [PubMed]
- Quick, B. The Estlander-Abbe operation. Aust N Z J. Surg. 1946, 16, 142–148. [Google Scholar] [CrossRef]
- Patel, S.B.; Buttars, B.R.; Roy, D.B. Mustardé flap for primary nasal sidewall defect post-Mohs micrographic surgery. JAAD Case Rep. 2022, 23, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Mustardé, J.C. The use of flaps in the orbital region. Plast. Reconstr. Surg. 1970, 45, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.W.; Lim, J.H.; Lee, J.H. Reconstruction of midface defects using local flaps. Medicine 2019, 98, e18021. [Google Scholar] [CrossRef]
- Neill, B.; Rickstrew, J.; Tolkachjov, S. Reconstructing the Glabella and Nasal Root. J. Drugs Dermatol. 2022, 21, 983–988. [Google Scholar] [CrossRef]
- Vozel, D.; Stritar, A. Cheek reconstruction with vy, cervicofacial and submental flap. Zdr. Vestn. 2019, 88, 143–155. [Google Scholar]
- Zhang, C.; Tang, X.; Wei, Z.; Wang, D.; Wang, B.; Zeng, X.; Jin, W. Nasolabial flap with Facial artery perforator for repairing defects after resection of midface tumor. Zhonghua Zheng Xing Wai Ke Za Zhi = Chin. J. Plast. Surg. 2016, 32, 342–346. [Google Scholar]
- Zarrabi, S.; Welch, M.; Neary, J.; Kim, B.-J. A Novel Approach for Total Nasal Reconstruction. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2019, 77, e1–e1073. [Google Scholar] [CrossRef]
- Weber, S.M.; Baker, S.R. Management of Cutaneous Nasal Defects. Facial Plast. Surg. Clin. N. Am. 2009, 17, 395–417. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Kim, Y.H.; Kim, J.T. Angular artery perforator-based transposition flap for the reconstruction of midface defect. Int. J. Dermatol. 2012, 51, 1366–1370. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.R.; Swanson, N.A. Reconstruction of Midfacial Defects Following Surgical Management of Skin Cancer. J. Dermatol. Surg. Oncol. 1994, 20, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Zito, P.M.; Mazzoni, T. Paramedian Forehead Flaps. In Stat Pearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Petersen, W.; Rahmanian-Schwarz, A.; Werner, J.-O.; Schiefer, J.; Rothenberger, J.; Hübner, G.; Schaller, H.-E.; Held, M. The use of collagen-based matrices in the treatment of full-thickness wounds. Burns 2016, 42, 1257–1264. [Google Scholar] [CrossRef] [PubMed]





| Technique Adopted | Type of Flap | Main Midface Region | Secondary Regions | Skin Defect Size |
|---|---|---|---|---|
| Abbè Flap | Rotational Flap | Upper Lip | - | Small–Medium |
| Bilobed Flap | Transpositional Flap | Nose | Eyelids | Small |
| Cervicofacial Flap | Rotational/Advancement Flap | Cheek | Periorbital Region, Preauricular, Neck | Large |
| Frontal Hairline Island Flap | Transpositional Flap | Nose | Canthal, Upper lip | Medium |
| Island Composite Nasal Flap | Transpositional Flap | Nose (Higher Portion) | - | Medium |
| Karapandzic Flap | Rotational Flap | Upper lip | Lower Lip | Medium–Large |
| Keystone Flap | Advancement Flap | Cheek | Nose, Upper Lip | Medium |
| Mustardè Flap | Rotational Flap | Cheek | Lateral Nose Wall, Lower Eyelid | Medium–Large |
| Nasolabial Flap | Advancement Flap | Nose | Periorbital Region, Cheek, Upper Lip | Medium |
| Paramedian Flap | Rotational Flap | Nose | - | Medium–Large |
| Retroangular Flap | Transpositional Flap | Cheek | Nose, Periorbital Region, Glabella | Medium |
| Rhomboidal Flap | Transpositional Flap | Cheek | Scalp, Neck, Nose, Eyelids | Medium |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salzano, G.; Maffìa, F.; Vaira, L.A.; Committeri, U.; Copelli, C.; Maglitto, F.; Manfuso, A.; Abbate, V.; Bonavolontà, P.; Scarpa, A.; et al. Locoregional Flaps for the Reconstruction of Midface Skin Defects: A Collection of Key Surgical Techniques. J. Clin. Med. 2023, 12, 3700. https://doi.org/10.3390/jcm12113700
Salzano G, Maffìa F, Vaira LA, Committeri U, Copelli C, Maglitto F, Manfuso A, Abbate V, Bonavolontà P, Scarpa A, et al. Locoregional Flaps for the Reconstruction of Midface Skin Defects: A Collection of Key Surgical Techniques. Journal of Clinical Medicine. 2023; 12(11):3700. https://doi.org/10.3390/jcm12113700
Chicago/Turabian StyleSalzano, Giovanni, Francesco Maffìa, Luigi Angelo Vaira, Umberto Committeri, Chiara Copelli, Fabio Maglitto, Alfonso Manfuso, Vincenzo Abbate, Paola Bonavolontà, Alfonso Scarpa, and et al. 2023. "Locoregional Flaps for the Reconstruction of Midface Skin Defects: A Collection of Key Surgical Techniques" Journal of Clinical Medicine 12, no. 11: 3700. https://doi.org/10.3390/jcm12113700
APA StyleSalzano, G., Maffìa, F., Vaira, L. A., Committeri, U., Copelli, C., Maglitto, F., Manfuso, A., Abbate, V., Bonavolontà, P., Scarpa, A., Califano, L., & Dell’Aversana Orabona, G. (2023). Locoregional Flaps for the Reconstruction of Midface Skin Defects: A Collection of Key Surgical Techniques. Journal of Clinical Medicine, 12(11), 3700. https://doi.org/10.3390/jcm12113700













