Cerebral Perfusion and Neuromonitoring during Complex Aortic Arch Surgery: A Narrative Review
Abstract
1. Introduction
2. Brain Damage after Ascending Aorta and Aortic Arch Surgery: General Considerations
3. Pathophysiology
4. Aetiology of Neurologic Injury during Aortic Surgery
- Type 1: including death from stroke and non-fatal stroke, transient ischemic attack (TIA), hypoxic encephalopathy, stupor and coma;
- Type 2: includes cognitive decline, delirium, memory loss and epilepsy without focal deficit [3].
- (a)
- The strategy for cerebral perfusion on top of hypothermic circulatory arrest.
- (b)
- Cerebral monitoring techniques associated with possible therapeutic interventions.
5. Strategy for Cerebral Perfusion on Top of Hypothermic Circulatory Arrest
- i.
- Deep hypothermic circulatory arrest (DHCA);
- ii.
- Retrograde cerebral perfusion (RCP) with DHCA;
- iii.
- Antegrade cerebral perfusion (ACP) with DHCA;
- iv.
- ACP with moderate hypothermic circulatory arrest.
5.1. Axillary Artery Cannulation (Table 1)
| Cannulation Site | PROs | CONs |
|---|---|---|
| Femoral Artery |
|
|
| Right Axillary Artery |
|
|
| Left Axillary Artery |
|
|
| Carotid Arteries |
|
|
| Innominate/Subclavian Artery |
|
|
| Ascending Aorta “true lumen” |
|
|
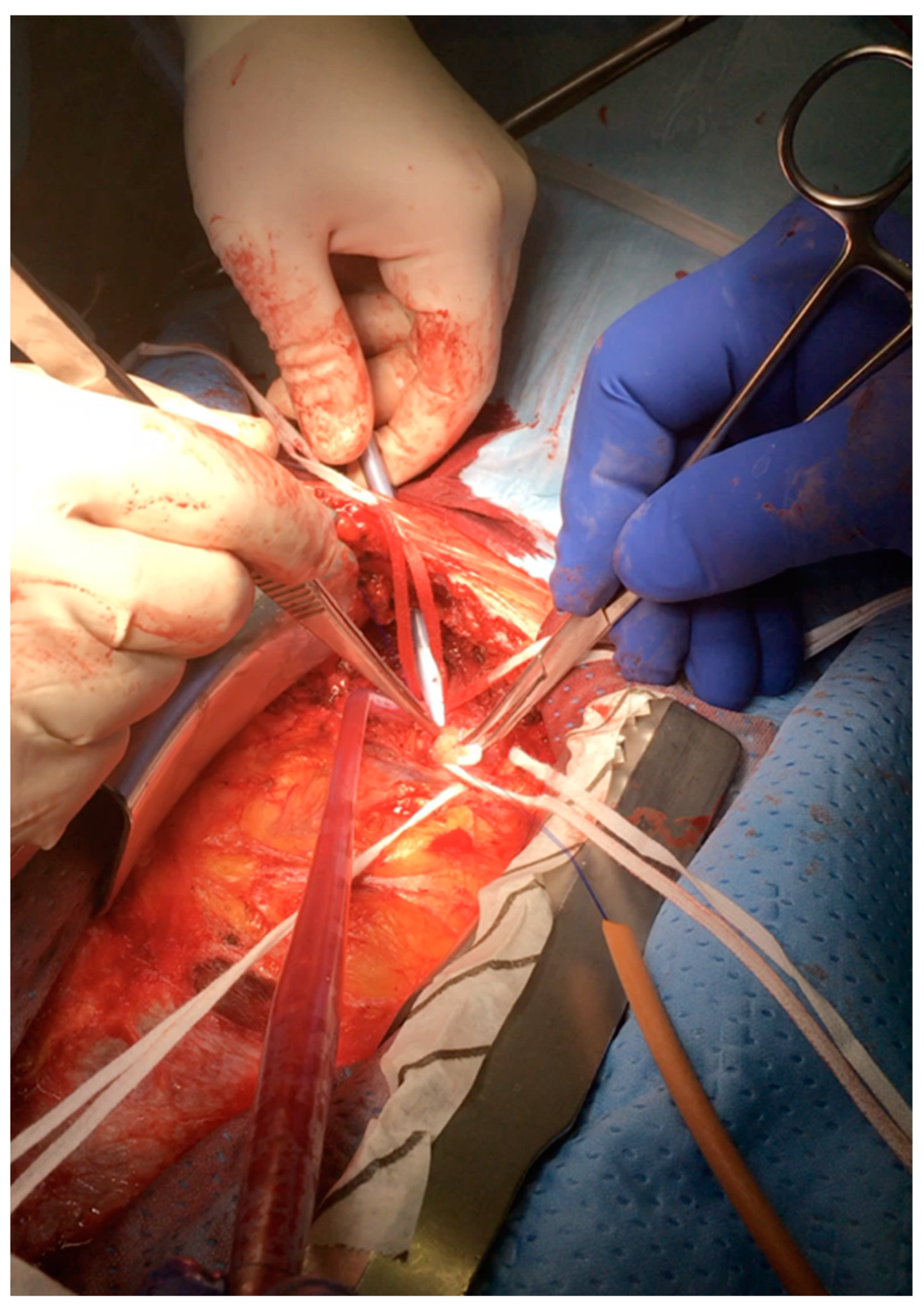
5.1.1. Direct Cannulation Technique
5.1.2. Side-Arm Graft Technique
5.1.3. Right Subclavian Artery Cannulation without Infraclavicular Incision (Table 1)
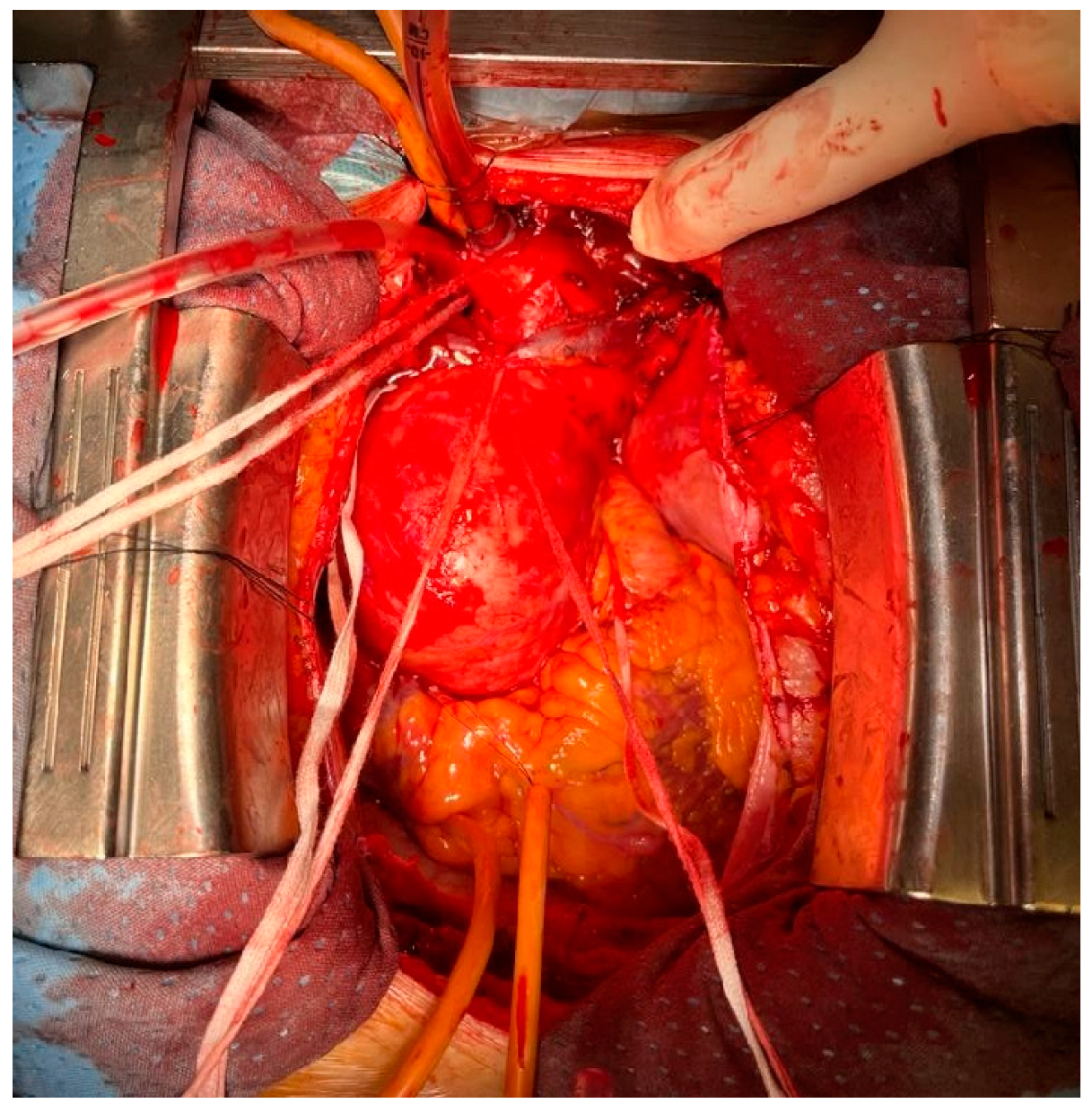
5.2. Innominate Artery Cannulation
Surgical Technique
5.3. Left Common Carotid Artery
5.4. Ascending Aorta
5.5. Femoral Artery Cannulation
6. Anterograde versus Retrograde Cerebral Perfusion
7. Monitoring Techniques Associated with Possible Therapeutic Strategies
- (a)
- A displaced cannula.
- (b)
- An arterial line obstruction.
- (c)
- An interrupted circle of Willis.
- (a)
- Preoperative central venous saturation (ScvO2) concentrations are reflective of baseline severity of cardiopulmonary dysfunction, associated with short- and long-term mortality and morbidity, and may add to preoperative risk stratification in patients undergoing cardiac surgery. However, patients with aortic dissection have different clinical presentations which might significantly affect their baseline ScvO2; therefore, the role of the preoperative status on the risk of postoperative neurological dysfunction, and the most appropriate CPB and ACP strategies to match these findings are still open questions.
- (b)
- rSO2 determined by NIRS is directly related to cerebral blood flow and jugular venous oxygen saturation (ScvO2); the innominate vein is sometimes interrupted during aortic surgery and this phenomenon might play a role in brain perfusion, especially in the left hemisphere during unilateral RCP [12,51].
- (a)
- NIRS is diagnosis, not therapy.
- (b)
- There is no consensus about normal and abnormal values; indeed, validated thresholds are urgently required in aortic surgery (less than 50% or reduction more than 20% from baseline).
- (c)
- There is no consensus about effective interventions.
- (d)
- NIRS does not measure all the cerebral brain oxygen saturation, but only a small portion of the frontal cortex (average depth 2.5 cm): cortical atrophy gets the cortex away from the skull (less reliable in high risk elderly patients), and postoperative neurologic damages are not exclusively related to the frontal cortex oxygen supply reduction/imbalance.
- (e)
- NIRS value can be influenced by non-brain sources (melanin, water).
- (f)
- Ice packs are placed around the head of patients until the start of rewarming, which might jeopardize the reliability and reproducibility of the data.
8. Cerebral Perfusion Monitoring: Integrative Strategies and Future Perspectives
8.1. Transcranial Doppler
8.2. Frequency-Domain Near-Infrared Spectroscopy (FDNIRS) and Diffuse Correlation Spectroscopy (DCS)
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abe, T.; Usui, A. The Cannulation Strategy in Surgery for Acute Type A Dissection. Gen. Thorac. Cardiovasc. Surg. 2017, 65, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bassin, L.; Bell, D. Temporary extracorporeal bypass modalities during aortic surgery. Best Pr. Res. Clin. Anaesthesiol. 2016, 30, 341–357. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.Y.; Safi, H.J.; Estrera, A.L. Cerebral perfusion in aortic arch surgery: Antegrade, retrograde, or both? Tex. Heart Inst. J. 2011, 38, 674–677. [Google Scholar] [PubMed]
- Oeveren, W.V. Neurological damage due to coagulation and fat release during cardiopulmonary bypass: Deutsche Forschungsgemeinschaft. BioMed Cent. 1999, 4, 1–2. [Google Scholar]
- Qu, J.Z.; Kao, L.W.; Smith, J.E.; Kuo, A.; Xue, A.; Iyer, M.H.; Essandoh, M.K.; Dalia, A.A. Brain Protection in Aortic Arch Surgery: An Evolving Field. J. Cardiothorac. Vasc. Anesth. 2021, 35, 1176–1188. [Google Scholar] [CrossRef] [PubMed]
- Czerny, M.; Fleck, T.; Zimpfer, D.; Dworschak, M.; Hofmann, W.; Hutschala, D.; Dunkler, D.; Ehrlich, M.; Wolner, E.; Grabenwoger, M. Risk factors of mortality and permanent neurologic injury in patients undergoing ascending aortic and arch repair. J. Thorac. Cardiovasc. Surg. 2003, 126, 1296–1301. [Google Scholar] [CrossRef] [PubMed]
- Payabyab, E.C.; Hemli, J.M.; Mattia, A.; Kremers, A.; Vatsia, S.K.; Scheinerman, S.J.; Mihelis, E.A.; Hartman, A.R.; Brinster, D.R. The use of innominate artery cannulation for antegrade cerebral perfusion in aortic dissection. J. Cardiothorac. Surg. 2020, 15, 205. [Google Scholar] [CrossRef]
- Berger, M.; Terrando, N.; Smith, S.K.; Browndyke, J.N.; Newman, M.F.; Mathew, J.P. Neurocognitive Function after Cardiac Surgery: From Phenotypes to Mechanisms. Anesthesiology 2018, 129, 829–851. [Google Scholar] [CrossRef]
- Motshabi-Chakane, P.; Mogane, P.; Moutlana, J.; Leballo-Mothibi, G.; Dingezweni, S.; Mpanya, D.; Tsabedze, N. Contemporary Neuroprotection Strategies during Cardiac Surgery: State of the Art Review. Int. J. Env. Res. Public Health 2021, 18, 12747. [Google Scholar] [CrossRef]
- Hage, A.; Stevens, L.-M.; Ouzounian, M.; Chung, J.; El-Hamamsy, I.; Chauvette, V.; Dagenais, F.; Cartier, A.; Peterson, M.D.; Boodhwani, M.; et al. Impact of brain protection strategies on mortality and stroke in patients undergoing aortic arch repair with hypothermic circulatory arrest: Evidence from the Canadian Thoracic Aortic Collaborative. Eur. J. Cardiothorac. Surg. 2020, 58, 95–103. [Google Scholar] [CrossRef]
- Xia, Q.; Cao, Y.; Xie, B.; Qiu, D.; Deng, L.; Wang, M.; Han, H. Cannulation strategies in type A aortic dissection: A novel insight narrative review. J. Thorac. Dis. 2021, 13, 2551–2562. [Google Scholar] [CrossRef] [PubMed]
- Luehr, M.; Bachet, J.; Mohr, F.-W.; Etz, C.D. Modern temperature management in aortic arch surgery: The dilemma of moderate hypothermia. Eur. J. Cardiothorac. Surg. 2014, 45, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Claassen, J.A.H.R.; Thijssen, D.H.J.; Panerai, R.B.; Faraci, F.M. Regulation of cerebral blood flow in humans: Physiology and clinical implications of autoregulation. Physiol. Rev. 2021, 101, 1487–1559. [Google Scholar] [CrossRef] [PubMed]
- Fantini, S.; Sassaroli, A.; Tgavalekos, K.T.; Kornbluth, J. Cerebral blood flow and autoregulation: Current measurement techniques and prospects for noninvasive optical methods. Neurophotonics 2016, 3, 031411. [Google Scholar] [CrossRef]
- Ergin, M.A.; Galla, J.D.; Lansman, S.L.; Quintana, C.; Bodian, C.; Griepp, R.B. Hypothermic circulatory arrest in operations on the thoracic aorta. Determinants of operative mortality and neurologic outcome. J. Thorac. Cardiovasc. Surg. 1994, 107, 788–797. [Google Scholar] [CrossRef]
- Ko, S.B. Perioperative stroke: Pathophysiology and management. Korean J. Anesth. 2018, 71, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kazui, T. Total arch replacement with separated graft technique and selective antegrade cerebral perfusion. Ann. Cardiothorac. Surg. 2013, 2, 353–357. [Google Scholar]
- Tian, D.H.; Wan, B.; Bannon, P.G.; Misfeld, M.; Lemaire, S.A.; Kazui, T.; Kouchoukos, N.T.; Elefteriades, J.A.; Bavaria, J.; Coselli, J.S.; et al. A meta-analysis of deep hypothermic circulatory arrest versus moderate hypothermic circulatory arrest with selective antegrade cerebral perfusion. Ann. Cardiothorac. Surg. 2013, 2, 148–158. [Google Scholar]
- Dong, S.-B.; Xiong, J.-X.; Zhang, K.; Zheng, J.; Xu, S.-D.; Liu, Y.-M.; Sun, L.-Z.; Pan, X.-D. Different hypothermic and cerebral perfusion strategies in extended arch replacement for acute type a aortic dissection: A retrospective comparative study. J. Cardiothorac. Surg. 2020, 15, 236. [Google Scholar] [CrossRef]
- Lee, T.C.; Kon, Z.; Cheema, F.H.; Grau-Sepulveda, M.V.; Englum, B.; Kim, S.; Chaudhuri, P.S.; Thourani, V.H.; Ailawadi, G.; Hughes, G.C.; et al. Contemporary management and outcomes of acute type A aortic dissection: An analysis of the STS adult cardiac surgery database. J. Card. Surg. 2018, 33, 7–18. [Google Scholar] [CrossRef]
- Okita, Y. Current surgical results of acute type A aortic dissection in Japan. Ann. Cardiothorac. Surg. 2016, 5, 368–376. [Google Scholar] [CrossRef]
- Mohamed, H.; Vitulli, P.; Petrou, M. Axillary versus femoral arterial cannulation in type A acute aortic dissection: Evidence from a meta-analysis of comparative studies and adjusted risk estimates. Eur. J. Cardiothorac. Surg. 2015, 48, 953–959. [Google Scholar]
- Kreibich, M.; Chen, Z.; Rylski, B.; Bavaria, J.E.; Brown, C.R.; Branchetti, E.; Vallabhajosyula, P.; Szeto, W.Y.; Desai, N.D. Outcome after aortic, axillary, or femoral cannulation for acute type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2019, 158, 27–34.e9. [Google Scholar] [CrossRef]
- Garg, V.; Peterson, M.D.; Chu, M.W.; Ouzounian, M.; MacArthur, R.G.; Bozinovski, J.; El-Hamamsy, I.; Chu, F.V.; Garg, A.; Hall, J.; et al. Axillary versus innominate artery cannulation for antegrade cerebral perfusion in aortic surgery: Design of the Aortic Surgery Cerebral Protection Evaluation (ACE) CardioLink-3 randomised trial. BMJ Open 2017, 7, e014491. [Google Scholar] [CrossRef] [PubMed]
- Tong, Z.; Gu, Y.; Guo, L.; Guo, J.; Gao, X.; Li, J.; Wang, Z.; Zhang, J. An Analysis of Complications of Brachial and Axillary Artery Punctures. Am. Surg. 2016, 82, 1250–1256. [Google Scholar] [CrossRef] [PubMed]
- Sabik, J.F.; Nemeh, H.; Lytle, B.W.; Blackstone, E.H.; Gillinov, A.; Rajeswaran, J.; Cosgrove, D.M. Cannulation of the axillary artery with a side graft reduces morbidity. Ann. Thorac. Surg. 2004, 77, 1315–1320. [Google Scholar] [CrossRef]
- Nishijima, S.; Nakamura, Y.; Yoshiyama, D.; Yasumoto, Y.; Kuroda, M.; Nakayama, T.; Tsuruta, R.; Ito, Y. Single direct right axillary artery cannulation using a modified Seldinger technique in minimally invasive cardiac surgery. Gen. Thorac. Cardiovasc. Surg. 2022, 70, 954–961. [Google Scholar] [CrossRef]
- Puiu, P.-C.; Pingpoh, C.; Beyersdorf, F.; Czerny, M.; Keyl, C.; Kreibich, M.; Kondov, S.; Rylski, B.; Zimmer, E.; Siepe, M. Direct Versus Side Graft Cannulation From the Right Axillary Artery in Thoracic Aortic Surgery. Ann. Thorac. Surg. 2021, 112, 1433–1440. [Google Scholar] [CrossRef]
- Regesta, T.; Cavozza, C.; Campanella, A.; Pellegrino, P.; Gherli, R.; Maj, G.; Audo, A. Direct proximal right subclavian artery cannulation during surgery of the thoracic aorta. JTCVS Tech. 2021, 8, 1–6. [Google Scholar] [CrossRef]
- Peterson, M.D.; Garg, V.; Mazer, C.D.; Chu, M.W.; Bozinovski, J.; Dagenais, F.; MacArthur, R.G.; Ouzounian, M.; Quan, A.; Jüni, M.P.; et al. A randomized trial comparing axillary versus innominate artery cannulation for aortic arch surgery. J. Thorac. Cardiovasc. Surg. 2020, 164, 1426–1438.e2. [Google Scholar] [CrossRef]
- Harky, A.; Wong, C.H.M.; Chan, J.S.K.; Zaki, S.; Froghi, S.; Bashir, M. Innominate artery cannulation in aortic surgery: A systematic review. J. Card. Surg. 2018, 33, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Chu, M.W.; Losenno, K.L.; Gelinas, J.J.; Garg, V.; Dickson, J.; Harrington, A.; Verma, S.; Peterson, M.D. Innominate and Axillary Cannulation in Aortic Arch Surgery Provide Similar Neuroprotection. Can. J. Cardiol. 2016, 32, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Eldeiry, M.; Ghincea, C.; Aftab, M.; Cleveland, J.C.; Fullerton, D.; Reece, T.B. Innominate Versus Axillary Artery Cannulation for the Hemiarch Repair. J. Surg. Res. 2018, 232, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Berretta, P.; Alfonsi, J.; Di Bartolomeo, R.; Di Eusanio, M. Innominate artery cannulation during aortic surgery. Multimed. Man. Cardiothorac. Surg. 2015, 2015, mmv030. [Google Scholar] [CrossRef] [PubMed]
- Cavozza, C.; Campanella, A.; Pellegrino, P.; Regesta, T.; Gherli, R.; Audo, A. Right subclavian artery cannulation for aortic dissection surgery, without infraclavicular incision. Multimed. Man. Cardiothorac. Surg. 2020, 2020. [Google Scholar] [CrossRef]
- Mochizuki, Y.; Iida, H.; Mori, H.; Yamada, Y.; Miyoshi, S. Left common carotid artery cannulation for type A aortic dissections. Tex. Heart Inst. J. 2003, 30, 128–129. [Google Scholar]
- Taguchi, S.; Mori, A.; Suzuki, R.; Ishida, O. Simplicity, skills, and pitfalls of ascending aortic cannulation for type A aortic dissection. J. Cardiothorac. Surg. 2013, 8, 161. [Google Scholar] [CrossRef]
- Kazui, T.; Inoue, N.; Komatsu, S. Surgical treatment ofaneurysms of the transverse aortic arch. J. Cardiovasc. Surg. 1989, 30, 402–406. [Google Scholar]
- Tan, M.E.S.H.; Dossche, J.M.E.; Morshuis, W.J.; Kelder, J.C.; Waanders, F.G.J.; Schepens, M.A.A.M. Is extended arch replacement for acute type a aortic dissection an additional risk factor for mortality? Ann. Thorac. Surg. 2003, 76, 1209–1214. [Google Scholar] [CrossRef]
- Di Eusanio, M.; Wesselink, R.M.J.; Morshuis, W.J.; Dossche, K.M.E.; Schepens, M.A.A.M. Deep hypothermic circulatory arrest and antegrade selective cerebral perfusion during ascending aorta-hemiarch replacement: A retrospective comparative study. J. Thorac. Cardiovasc. Surg. 2003, 125, 849–854. [Google Scholar] [CrossRef]
- Müller, D.; Fieguth, H.G.; Wimmer-Greinecker, G.; Wöhleke, T.; Kleine, P.; Moritz, A. Neurologic outcome after surgery of the aortic arch: Comparison of deep hypothermic arrest, antegrade and retrograde cerebral perfusion. Indian J. Thorac. Cardiovasc. Surg. 2004, 20, 72–76. [Google Scholar] [CrossRef]
- Harrington, D.K.; Walker, A.S.; Kaukuntla, H.; Bracewell, R.M.; Clutton-Brock, T.H.; Faroqui, M.; Pagano, D.; Bonser, R.S. Selective antegrade cerebral perfusion attenuates brain metabolic deficit in aortic arch surgery: A prospective randomized trial. Circulation 2004, 110 (Suppl. 1), II231-6. [Google Scholar] [CrossRef]
- Sundt III, T.M.; Orszulak, T.A.; Cook, D.J.; Schaff, H.V. Improving results of open arch replacement. Ann. Thorac. Surg. 2008, 86, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Halkos, M.E.; Kerendi, F.; Myung, R.; Kilgo, P.; Puskas, J.D.; Chen, E.P. Selective antegrade cerebral perfusion via right axillary artery cannulation reduces morbidity and mortality after proximal aortic surgery. J. Thorac. Cardiovasc. Surg. 2009, 138, 1081–1089. [Google Scholar] [CrossRef] [PubMed]
- Wiedemann, D.; Kocher, A.; Dorfmeister, M.; Vadehra, A.; Mahr, S.; Laufer, G.; Ehrlich, M. Effect of cerebral protection strategy on outcome of patients with Stanford type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2013, 146, 647–655.e1. [Google Scholar] [CrossRef]
- Misfeld, M.; Leontyev, S.; Borger, M.A.; Gindensperger, O.; Lehmann, S.; Legare, J.F.; Mohr, F.W. What is the best strategy for brain protection in patients undergoing aortic arch surgery? A single center experience of 636 patients. Ann. Thorac. Surg. 2012, 93, 1502–1508. [Google Scholar] [CrossRef]
- Zierer, A.; Risteski, P.; El-Sayed Ahmad, A.; Moritz, A.; Diegeler, A.; Urbanski, P.P. The impact of unilateral versus bilateral antegrade cerebral perfusion on surgical outcomes after aortic arch replacement: A propensity-matched analysis. J. Thorac. Cardiovasc. Surg. 2014, 147, 1212–1217; discussion 1217–1218. [Google Scholar] [CrossRef]
- Preventza, O.; Simpson, K.H.; Cooley, D.A.; Cornwell, L.; Bakaeen, F.G.; Omer, S.; Rodriguez, V.; de la Cruz, K.I.; Rosengart, T.; Coselli, J.S. Unilateral versus bilateral cerebral perfusion for acute type A aortic dissection. Ann. Thorac. Surg. 2015, 99, 80–87. [Google Scholar] [CrossRef]
- Urbanski, P.P.; Thamm, T.; Bougioukakis, P.; Irimie, V.; Prasad, P.; Diegeler, A.; Lenos, A. Efficacy of unilateral cerebral perfusion for brain protection in aortic arch surgery. J. Thorac. Cardiovasc. Surg. 2020, 159, 365–371.e1. [Google Scholar] [CrossRef]
- Angleitner, P.; Stelzmueller, M.; Mahr, S.; Kaider, A.; Laufer, G.; Ehrlich, M. Bilateral or unilateral antegrade cerebral perfusion during surgery for acute type A dissection. J. Thorac. Cardiovasc. Surg. 2020, 159, 2159–2167.e2. [Google Scholar] [CrossRef]
- Norton, E.L.; Wu, X.; Kim, K.M.; Patel, H.J.; Deeb, G.M.; Yang, B. Unilateral is comparable to bilateral antegrade cerebral perfusion in acute type A aortic dissection repair. J. Thorac. Cardiovasc. Surg. 2020, 160, 617–625.e5. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, O.; Morell, A.; Zemgulis, V.; Lundström, E.; Tovedal, T.; Einarsson, G.M.; Thelin, S.; Ahlström, H.; Björnerud, A.; Lennmyr, F. Minimal safe arterial blood flow during selective antegrade cerebral perfusion at 20° centigrade. Ann. Thorac. Surg. 2011, 91, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Haldenwang, P.L.; Bechtel, M.; Moustafine, V.; Buchwald, D.; Wippermann, J.; Wahlers, T.; Strauch, J.T. State of the art in neuroprotection during acute type A aortic dissection repair. Perfusion 2012, 27, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Ueda, Y.; Okita, Y.; Aomi, S.; Koyanagi, H.; Takamoto, S. Retrograde cerebral perfusion for aortic arch surgery: Analysis of risk factors. Ann. Thorac. Surg. 1999, 67, 1879–1882; discussion 1891–1894. [Google Scholar] [CrossRef]
- Usui, A.; Abe, T.; Murase, M. Early clinical results of retrograde cerebral perfusion for aortic arch operations in Japan. Ann. Thorac. Surg. 1996, 62, 94–103; discussion 103–104. [Google Scholar] [CrossRef]
- Sun, S.; Chien, C.-Y.; Fan, Y.-F.; Wu, S.-J.; Li, J.-Y.; Tan, Y.-H.; Hsu, K.-H. Retrograde cerebral perfusion for surgery of type A aortic dissection. Asian J. Surg. 2021, 44, 1529–1534. [Google Scholar] [CrossRef] [PubMed]
- Bavaria, J.E.; Pochettino, A. Retrograde cerebral perfusion (RCP) in aortic arch surgery: Efficacy and possible mechanisms of brain protection. Semin. Thorac. Cardiovasc. Surg. 1997, 9, 222–232. [Google Scholar]
- Okita, Y. Neuro-protection in open arch surgery. Ann. Cardiothorac. Surg. 2018, 7, 389–396. [Google Scholar] [CrossRef]
- Ziganshin, B.A.; Elefteriades, J.A. Deep hypothermic circulatory arrest. Ann. Cardiothorac. Surg. 2013, 2, 303–315. [Google Scholar]
- Agarwal, S.; Kendall, J.; Quarterman, C. Perioperative management of thoracic and thoracoabdominal aneurysms. BJA Educ. 2019, 19, 119–125. [Google Scholar] [CrossRef]
- Mosca, M.S.; Justison, G.; Reece, T.B. A Clinical Protocol for Goal Directed Cerebral Perfusion during Aortic Arch Surgery. Semin. Cardiothorac. Vasc. Anesth. 2016, 20, 289–297. [Google Scholar] [CrossRef]
- Zheng, F.; Sheinberg, R.; Yee, M.S.; Ono, M.; Zheng, Y.; Hogue, C.W. Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: A systematic review. Anesth. Analg. 2013, 116, 663–676. [Google Scholar] [CrossRef]
- Olsson, C.; Thelin, S. Regional cerebral saturation monitoring with near-infrared spectroscopy during selective antegrade cerebral perfusion: Diagnostic performance and relationship to postoperative stroke. J. Thorac. Cardiovasc. Surg. 2006, 131, 371–379. [Google Scholar] [CrossRef]
- Bennett, S.R.; Abukhodair, A.W.; Alqarni, M.S.; Fernandez, J.A.; Fernandez, A.J.; Bennett, M.R.; Fernandez, J.A.; Bennett, M. Outcomes in Cardiac Surgery Based on Preoperative, Mean Intraoperative and Stratified Cerebral Oximetry. Values Cureus 2021, 13, e17123. [Google Scholar] [CrossRef] [PubMed]
- Vretzakis, G.; Georgopoulou, S.; Stamoulis, K.; Stamatiou, G.; Tsakiridis, K.; Zarogoulidis, P.; Katsikogianis, N.; Kougioumtzi, I.; Machairiotis, N.; Tsiouda, T.; et al. Cerebral oximetry in cardiac anesthesia. J. Thorac. Dis. 2014, 6 (Suppl. 1), S60–S69. [Google Scholar]
- Rubio, A.; Hakami, L.; Münch, F.; Tandler, R.; Harig, F.; Weyand, M. Noninvasive control of adequate cerebral oxygenation during low-flow antegrade selective cerebral perfusion on adults and infants in the aortic arch surgery. J. Card. Surg. 2008, 23, 474–479. [Google Scholar] [CrossRef]
- Nenna, A.; Barbato, R.; Greco, S.M.; Pugliese, G.; Lusini, M.; Covino, E.; Chello, M. Near-infrared spectroscopy in adult cardiac surgery: Between conflicting results and unexpected uses. J. Geriatr. Cardiol. 2017, 14, 659–661. [Google Scholar]
- Siesjö, B.K. Lactic acidosis in the brain: Occurrence, triggering mechanisms and pathophysiological importance. Ciba. Found Symp. 1982, 87, 77–100. [Google Scholar]
- Wang, J.; Guo, L.; Holdefer, R.N.; Zhang, Y.; Liu, Q.; Gai, Q.; Zhang, W. Intraoperative Neurophysiology and Transcranial Doppler for Detection of Cerebral Ischemia and Hyperperfusion During Carotid Endarterectomy. World Neurosurg. 2021, 154, e245–e253. [Google Scholar] [CrossRef] [PubMed]
- Bouri, S.; Thapar, A.; Shalhoub, J.; Jayasooriya, G.; Fernando, A.; Franklin, I.; Davies, A. Hypertension and the post-carotid endarterectomy cerebral hyperperfusion syndrome. Eur. J. Vasc. Endovasc. Surg. 2011, 41, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Schoknecht, K.; Gabi, S.; Ifergane, G.; Friedman, A.; Shelef, I. Detection of cerebral hyperperfusion syndrome after carotid endarterectomy with CT perfusion. J. Neuroimaging 2014, 24, 295–297. [Google Scholar] [CrossRef]
- Ogasawara, K.; Yukawa, H.; Kobayashi, M.; Mikami, C.; Konno, H.; Terasaki, K.; Inoue, T.; Ogawa, A. Prediction and monitoring of cerebral hyperperfusion after carotid endarterectomy by using single-photon emission computerized tomography scanning. J. Neurosurg. 2003, 99, 504–510. [Google Scholar] [CrossRef]
- Baraka, A. Alpha-stat vs. pH-stat strategy during hypothermic cardiopulmonary bypass. Middle East J. Anaesthesiol. 2004, 17, 705–712. [Google Scholar] [PubMed]
- Ziya Apaydin, A. Antegrade cerebral perfusion: A review of its current application. Turk Gogus. Kalp. Damar. Cerrahisi. Derg. 2021, 29, 1–4. [Google Scholar] [CrossRef]
- Cesnjevar, R.A.; Purbojo, A.; Muench, F.; Juengert, J.; Rueffer, A. Goal-directed-perfusion in neonatal aortic arch surgery. Transl. Pediatr. 2016, 5, 134–141. [Google Scholar] [CrossRef]
- Murkin, J.M.; Arango, M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br. J. Anaesth. 2009, 103 (Suppl. 1), i3–i13. [Google Scholar] [CrossRef]
- Yu, Y.; Zhang, K.; Zhang, L.; Zong, H.; Meng, L.; Han, R. Cerebral near-infrared spectroscopy (NIRS) for perioperative monitoring of brain oxygenation in children and adults. Cochrane Database Syst. Rev. 2018, 1, CD010947. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.L.; Hyttel-Sørensen, S.; Jakobsen, J.C.; Gluud, C.; Kooi, E.M.W.; Mintzer, J.; de Boode, W.P.; Fumagalli, M.; Alarcon, A.; Alderliesten, T.; et al. The clinical effects of cerebral near-infrared spectroscopy monitoring (NIRS) versus no monitoring: A protocol for a systematic review with meta-analysis and trial sequential analysis. Syst. Rev. 2021, 10, 111. [Google Scholar] [CrossRef]
- Kane, J.M.; Steinhorn, D.M. Lack of irrefutable validation does not negate clinical utility of near-infrared spectroscopy monitoring: Learning to trust new technology. J. Crit. Care 2009, 24, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, A.; Conte, M.; Cavallaro, M.; Scarafile, R.; Riegler, L.; Cocchia, R.; Pezzullo, E.; Carbone, A.; Natale, F.; Santoro, G.; et al. Transcranial Doppler ultraso- nography: From methodology to major clinical applications. World J. Car 2016, 8, 383–400. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ji, B.; Yang, B.; Liu, G.; Miao, N.; Yang, J.; Liu, J.; Long, C. Real-time continuous neuromonitoring com- bines transcranial cerebral Doppler with near-infrared spectroscopy cere-bral oxygen saturation during total aortic arch replacement procedure: A pilot study. ASAIO J. 2012, 58, 122–126. [Google Scholar] [CrossRef]
- Ghazy, T.; Darwisch, A.; Schmidt, T.; Fajfrova, Z.; Zickmüller, C.; Mashhour, A.; Matschke, K.; Kappert, U. Transcranial Doppler sonography for optimization of cerebral perfusion in aortic arch operation. Ann. Thorac. Surg. 2016, 101, e15–e16. [Google Scholar] [CrossRef] [PubMed]
- Boas, D.A.; Yodh, A.G. Spatially varying dynamical properties of turbid media probed with diffusing temporal light correlation. J. Opt. Soc. Am. 1997, 14, 192–215. [Google Scholar] [CrossRef]
- Fantini, S.; Franceschini, M.A.; Maier, J.S.; Walker, S.A.; Barbieri, B.B.; Gratton, E. Frequency-domain multi-channel optical detector for noninvasive tissue spectroscopy and oxime- try. Opt. Eng. 1995, 34, 32–42. [Google Scholar] [CrossRef]
- Ferradal, S.L.; Yuki, K.; Vyas, R.; Ha, C.G.; Yi, F.; Stopp, C.; Wypij, D.; Cheng, H.H.; Newburger, J.W.; Kaza, A.K.; et al. Perioperative cerebral hemo-dynamics and oxygen metabolism in neonates with single-ventricle physi-ology. Biomed. Opt. Express 2015, 6, 4749–4767. [Google Scholar]
- Ferradal, S.L.; Yuki, K.; Vyas, R.; Ha, C.G.; Yi, F.; Stopp, C.; Wypij, D.; Cheng, H.H.; Newburger, J.W.; Kaza, A.K.; et al. Non-invasive assessment of cerebral blood flow and oxygen metabolism in neonates during hypothermic car-diopulmonary bypass: Feasibility and clinical implications. Sci. Rep. 2017, 7, 44117. [Google Scholar] [CrossRef]
| Author | Year | Etiology | Allocation | Cannulation Site | Flow | Temperature | Perfusate Temperature | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ATAAD (n.) | Aneurysm (n.) | Total (n.) | DHCA | MHCA + SACP | DHCA | MHCA | |||||
| Kazui [38] | 1989 | 16 | 5 | 21 | 10 | 11 | Innominate artery + left CCA | 600 mL/min | 15 °C | 25 °C | - |
| Tan [39] | 2003 | 32 | - | 32 | 19 | 13 | Innominate + LCCA | 10 mL/kg/min | 15.1 ± 3.1 °C | 25 °C | 25 °C |
| Di Eusanio [40] | 2003 | 122 | 167 | 289 | 128 | 161 | Innominate + LCCA | 10 mL/kg/min | 16.1 ± 2.8 °C | 23.2 ± 2.6 °C | - |
| Mulller [41] | 2004 | 28 | 14 | 42 | 12 | 30 | RSA | 400–700 mL/min | 20 ± 2 °C | 22 ± 2 °C | - |
| Harrington [42] | 2004 | 1 | 41 | 42 | 22 | 20 | Innominate + LCCA | 8–12 mL/kg/min | 15 °C | 25 °C | 15 °C |
| Sundt [43] | 2008 | 48 | 246 | 294 | 220 | 74 | RAA | 10–15 mL/kg/min | 16–18 °C (NP); 23 °C (Bldr) | 25 °C | 13 °C |
| Halkos [44] | 2009 | 105 | 166 | 271 | 66 | 205 | RAA | 10 mL/kg/min | 18 °C | 23.2 ± 4.2 °C | 18 °C |
| Wiedemann [45] | 2012 | 207 | - | 207 | 116 | 91 | uACP: R. subclavian/innominate bACP: subclavian/innominate + L. carotid | 10 mL/kg/min | 18 °C | 25 °C | 25 °C |
| Misfeld [46] | 2012 | 220 | 339 | 585 | 220 | 365 | uACP RCCA bACP uACP: Innominate + LCCA | 10–15 mL/kg/min | 22 ± 2 °C | UACP 24 ± 3 °C (NP) BACP 25 ± 4 °C | 24 °C |
| Author | Year | Postoperative Stroke DHCA | Postoperative Stroke MHCA + SCP | Postoperative Transient Neurological Dysfunction DHCA | Postoperative Transient Neurological Dysfunction MHCA + SCP | Postoperative Mortality DHCA | Postoperative Mortality MHCA + SCP |
|---|---|---|---|---|---|---|---|
| Kazui [38] | 1989 | 1% | 0% | - | - | 14.3% | 9% |
| Tan [39] | 2003 | 28.6% | 9.1% | - | - | - | - |
| Di Eusanio [40] | 2003 | 12.5% | 6% | 6.2% | 8% | 13.2% | 9.9% |
| Mulller [41] | 2004 | 0% | 10% | - | - | 17% | 23% |
| Harrington [42] | 2004 | 9.1% | 0% | 4.5% | 2.5% | 0% | 15% |
| Sundt [43] | 2008 | 9.1% | 5.4% | - | - | 7.2% | 8.1% |
| Halkos [44] | 2009 | 4.5% | 3.9% | 9% | 4.3% | 22.7% | 8.7% |
| Wiedemann [45] | 2012 | 23.2% | 12% | 0.9% | 2.1% | 25.8% | 13.1% |
| Misfeld [46] | 2013 | 14.1% | 9% | 12.7% | 15.9% | 11.3% | 11.7% |
| Author | Year | ATAAD | Chronic | Number of Patients | ACP | Flow | Temperature |
|---|---|---|---|---|---|---|---|
| Zierer [47] | 2012 | 655 | 347 | 1002 | u-ACP 673, b-ACP 329 | 1.6 ± 0.2 L/min; 1.7 L/min | 26–34 °C |
| Preventza [48] | 2015 | 157 | 0 | 153 | u-ACP 90 (58.8%), b-ACP 63 (41.2%) | 10–15 mL/kg/min | 22–24 °C |
| Urbanski [49] | 2020 | 0 | 1000 | 1000 | u-ACP | 1.4 ± 0.3 L/min | 31 °C |
| Angleitner [50] | 2020 | 184 | 0 | 184 | b-ACP: n = 91, 49.5%; u-ACP: n = 93 | 10–15 mL/kg/min | 20–28 °C |
| Norton [51] | 2020 | 307 | 0 | 307 | using uni-ACP (n = 140) and bi-ACP (n = 167). | 10 mL/kg/min | 24–28 °C |
| Author | Year | Stroke | Transient Neuro Dysfunction | Mortality |
|---|---|---|---|---|
| Preventza [48] | 2015 | 13 of 88 u-ACP patients (14.8%) and 8 of 62 b-ACP patients (12.9%) had a postoperative stroke (p = 0.75) | 10 pts u-ACP (11.4%) and 5 pts b-ACP (8.2%) patients (p = 0.53) | The operative mortality was 13.3% (n = 12) with u-ACP and 12.7% (n = 8) with b-ACP (p = 0.91) |
| Urbanski [49] | 2020 | u-ACP 1% | u-ACP 4.9% | 30 days 1.3%, in-hospital 2.1% |
| Angleitner [50] | 2020 | u-ACP:19.4% (18 pts), b-ACP 18.7% (17 pts) | u-ACP 9.7% (9 pts), b-ACP 7.7% (7 pts) | 30-day mortality u-ACP: 16.1%, b-ACP: 12.1% |
| Norton [51] | 2020 | u-ACP 2.8% (4 pts) vs. b-ACP 6.5% (11 pts) | u-ACP 3.5% (5 pts) vs. b-ACP 2.4% (4 pts) | 30-day mortality: uni-ACP 3.4% vs. bi-ACP 7.8%, p = 0.12) |
| Zierer [47] | 2012 | u-ACP 4% (14/673) vs. b-ACP 2% (14/329) | u-ACP 4% (30/673 pts), b-ACP 4% (12/329) | 30-day mortality u-ACP: 5% (32/673 pts), b-ACP 5% (15/329 PTS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montisci, A.; Maj, G.; Cavozza, C.; Audo, A.; Benussi, S.; Rosati, F.; Cattaneo, S.; Di Bacco, L.; Pappalardo, F. Cerebral Perfusion and Neuromonitoring during Complex Aortic Arch Surgery: A Narrative Review. J. Clin. Med. 2023, 12, 3470. https://doi.org/10.3390/jcm12103470
Montisci A, Maj G, Cavozza C, Audo A, Benussi S, Rosati F, Cattaneo S, Di Bacco L, Pappalardo F. Cerebral Perfusion and Neuromonitoring during Complex Aortic Arch Surgery: A Narrative Review. Journal of Clinical Medicine. 2023; 12(10):3470. https://doi.org/10.3390/jcm12103470
Chicago/Turabian StyleMontisci, Andrea, Giulia Maj, Corrado Cavozza, Andrea Audo, Stefano Benussi, Fabrizio Rosati, Sergio Cattaneo, Lorenzo Di Bacco, and Federico Pappalardo. 2023. "Cerebral Perfusion and Neuromonitoring during Complex Aortic Arch Surgery: A Narrative Review" Journal of Clinical Medicine 12, no. 10: 3470. https://doi.org/10.3390/jcm12103470
APA StyleMontisci, A., Maj, G., Cavozza, C., Audo, A., Benussi, S., Rosati, F., Cattaneo, S., Di Bacco, L., & Pappalardo, F. (2023). Cerebral Perfusion and Neuromonitoring during Complex Aortic Arch Surgery: A Narrative Review. Journal of Clinical Medicine, 12(10), 3470. https://doi.org/10.3390/jcm12103470








