Abstract
Objectives: The burden of postpartum depression (PPD) is significant because it remains unrecognized, and it not only affects the mother adversely but also has a negative consequence on the family life and the development of the infant. The aim of the study was to measure the prevalence of PPD and identify the risk factors of PPD among mothers attending the well-baby clinic of six Primary Health Care centers in Abha city, Southwest Saudi Arabia. Materials and Methods: A total of 228 Saudi women having a child aged between two weeks to one year were recruited in the study by using a consecutive sampling technique. The Arabic version of the Edinburgh Postnatal Depression Scale (EPDS) was used as a screening tool to measure the prevalence of PPD. The mothers were also inquired about their socio-demographic characteristics and risk factors. Results: The prevalence rate of postpartum depression was 43.4%. Family conflict, and lack of support by spouse and family during pregnancy were found to be the strongest predictors of developing PPD. Women who had reported family conflict were at six times higher risk for developing PPD compared to those who did not have a family conflict (aOR = 6.5, 95% CI = 2.3–18.4). Women who reported a lack of spousal support during pregnancy encountered 2.3 fold increased risk for PPD (aOR = 2.3, 95% CI = 1.0–4.8) and women who had not received family support during pregnancy period were more than three times (aOR = 3.5, 95 % CI 1.6–7.7) likely to experience PPD. Conclusion: The risk of PPD among Saudi postnatal women was high. PPD screening should be an integral part of postnatal care. Awareness of women, spouses and families about potential risk factors can be a preventive strategy. The early identification of high-risk women during the antenatal and post-natal period could help to prevent this condition.
1. Introduction
Pregnancy is an enormous change in a woman’s life. Having a baby can be a very exciting time, at the same time, the emotional, hormonal, and physical changes a woman bears during this process can be hard and stressful, causing her to feel sad, anxious, afraid, and confused. Most women who experience these emotional changes are able to recover quickly. For some women, however, these feelings do not go away and may get worse.
In the Diagnostic and Statistical Manual of Mental Disorders (DSM–5), postpartum depression is considered when a patient has a major depressive episode along with the peripartum onset. By definition, it is defined as a major depressive episode with the onset of pregnancy or within four weeks of delivery [1]. Three types of illness have been classified based on the symptoms; baby blues, postpartum depression, and postpartum psychosis [1]. Baby blues that begins within the firstweek post-delivery is the least severe form of depression affecting between 13.7% to 76.0% of postpartum women [2]. Baby blues are described by symptoms, such as mood changes, dysphoria, anxiety, sleep disturbance, lack of appetite, irritability, tearfulness, agitation, lack of confidence, and feelings of being overwhelmed. Persisting for more than two weeks indicates that the woman may have advanced into postpartum depression [1].
The global prevalence of PPD varies between 10 and 33% [2,3,4,5,6], while in the middle-east region, it ranges from 17.6% to 51% [7,8,9,10,11,12]. Within Saudi Arabia, PPD affects 14–38.5% women in their post-partum period [13,14,15,16]. PPD usually occurs from four to twelve weeks after birth but can happen up to a year after delivery. Untreated PPD can lead to chronic depression and other complications, such as anxiety, poor quality of life, poor social and sexual relationships, risky behaviors, and suicidal ideation [17]. In addition to directly influencing the emotional well-being of mothers, postpartum depression has also been shown to affect mother–infant bonding and infant behavior. Children’s cognitive and emotional development can be significantly affected by postpartum depression [18,19,20].
A large body of evidence has consolidated the factors that can place mothers at risk for post-partum depression. These include prior history of depression, family history of depression, unemployment, low level of education, preterm birth, cesarean delivery, unplanned pregnancy, hormonal changes during pregnancy, lack of spousal support and insufficient family support, marital conflicts, stressful life events, such as involvement in violent relationships, and traumatic experiences [6,12,21,22].
Most pregnant women do not know about PPD and do not seek help, even when having experienced similar problems in previous pregnancies [18,23]. Postpartum women need early screening and quick access to mental healthcare [24,25]. Very limited studies have been carried out on this issue in Saudi Arabia. Particularly in the Southern region, no such study has been conducted. Hence a study on postpartum depression and associated risk factors was urgently needed to inform the current situation to health care providers and policymakers. Therefore, the aim of this study was to estimate the prevalence of postpartum depression and to identify the risk factors associated with PPD which would improve our understanding of the picture of PPD and also inform prevention and intervention strategies.
2. Methods
2.1. Study Place and Population
This cross sectional study was conducted in Abha city, the capital of Aseer Region in Saudi Arabia. The study period was from August to December 2019. The study participants comprised of post-partum Saudi women between 18–48 years of age with a child between 2 weeks to one year of age. Non-Saudi mothers and mothers having a child less than two weeks of age and more than one year of age were excluded from the study. The women were recruited from well-baby clinics at six primary health care centers randomly chosen from twelve primary health care centers in Abha city.
2.2. Sample Size and Sampling Technique
The sample size was calculated by using the statistical formula n = Z2pq/d2 [26]. Here, Z is the confidence limit (1.96) at a 95% level. “p” is the prevalence rate of postpartum depression (33.2%) in a Saudi Arabia study [21], “q” is (1 − p) that is the proportion of women who did not have postpartum depression, and “d” is the acceptable standard error (6%). The calculated sample size was 236. Consecutive sampling technique, that is participants were recruited on a first come basis, continuously till the desired sample size was reached. A total of 236 participants were approached. Due to incomplete information, eight questionnaires were excluded and as a result, the final sample size remained at 228.
2.3. Data Collection Tool
Arabic version of the Edinburgh Postnatal Depression Scale [27] was used as a screening tool to identify post-partum depression among the study subjects. The EPDS is a 10-item self-report questionnaire designed specifically for the detection of depression in the postpartum period [28]. It has been validated and translated into more than 20 languages, including Arabic. It is proven to be an effective screening tool and has been shown to have a sensitivity of 95% and specificity of 93%. Responses are scored 0–3 indicating the severity of manifestations with a minimum score of 0 and a maximum score of 30. The EPDS has a cutoff of 10 to signify probable depression [27]. Mothers with EPDS scores of more than 10 were classed as having depression. An increased score indicates the increasing severity of depression. A questionnaire covering the socio-demographic information and risk factors for PPD was developed and included with EPDS.
2.4. Study Procedure
The researcher provided a brief explanation about the objective of the study to the participants before the interview. The participants were assured of the confidentiality of all information. Voluntary verbal consent was obtained from participants before the interview. The study proposal was approved by the King Khalid University research ethical committee. (Reference #: REC: 2016/05/14). At the end of the study, mothers identified with high EPDS scores were advised to consult a psychiatrist for confirming the diagnosis and treatment.
2.5. Data Analysis
Data entry and analysis were conducted by using statistical software package SPSS version 22.0 [29]. Categorical data were presented as frequency and percentages and continuous data were presented as mean ± standard deviation. Univariate analysis was initially performed using Chi-square test or Fisher exact test to find the association of various risk factors with postpartum depression. Multiple logistic regression analysis was conducted using only the independent variables that were significant in the univariate analysis. A p-value less than 0.05 was considered statistically significant. Adjusted odds ratios in multiple logistic regression were measured with a 95% Confidence Interval.
2.6. Findings
The study participants comprised post-partum women between 18–48 years of age with a mean age of 30.9 ± 7.0 years. One hundred and ten women (48.2%) were less than 30 years of age, while 118 (51.8%) women were more than thirty years of age. The monthly income of 42.5% of women was between SR. 5000–10,000 and 37.7% was more than SR. 10,000. Almost all women (98.2%) were non-smokers. The pregnancy-related characteristics of the study group revealed that three in four were multi-gravid. More than half of the women (54.8%) reported that their last pregnancy was planned. No complication in last pregnancy was reported by 82.5% of women. Gestational diabetes was reported by 22 (9.6%). Most of women (about 90%) did not report any complications during or after delivery for themselves or the neonate. Sex of last child revealed an almost equal sex ratio. Few mothers delivered twins (3.5%). Current psychiatric illness was reported by 12 respondents (5.3%), while 11.8% reported a positive family history of psychiatric disease. Existing family conflict was reported by 1 in 6 respondents, while the past family conflict was reported by almost a third of the women. Three out of every four women reported support from their husband during pregnancy, and a little higher (76.8%) reported support by family in pregnancy.
Figure 1 presents the proportion of post-partum depression among the respondents. Based on the Edinburgh screening (EPDS) instrument, 99 (43.4%) mothers had depressive symptoms. Regarding the time since delivery for women with depressive symptoms, almost 46% of women were within 2 months of delivery, 40% were within 2–5 months of delivery, 9.5% between 6–9 months, and only about 4 % of cases between 10–12 months of delivery (Figure 2).
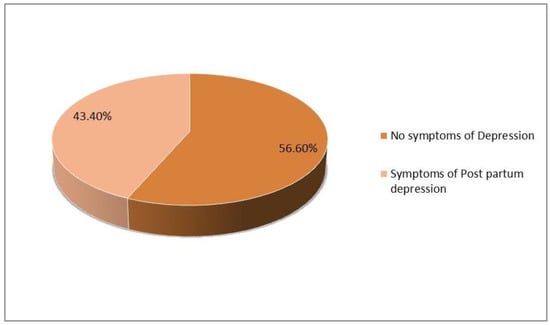
Figure 1.
Proportion of respondents with post-partum depression.
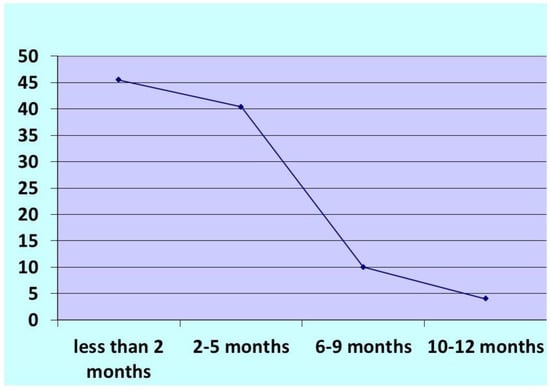
Figure 2.
Percentage distribution of postpartum depression cases by time since delivery.
Table 1 presents the association of postpartum depression with socio-demographic factors. A larger proportion of women with depression belongs to older ages (57.6%) and had a higher education (87.9%). Postpartum depression was more common in non-working women (59.6%), lower family income group (68.7%) and married women. However, none of these factors showed any significant association with postpartum depression.

Table 1.
Association of socio-demographic variables with postpartum depression.
Table 2 demonstrates the association of obstetric factors with postpartum depression. Multi-gravid women had significantly more postpartum depression than primigravid women (cOR = 2.0, 95%CI 1.1,3.8; p = 0.03). All other factors, such as planned pregnancy, outcome of pregnancy, sex of child, time, and mode of delivery, complication during or after delivery, twins or gestational diabetes did not show any significant association with postpartum depression.

Table 2.
Association of obstetric factors with postpartum depression.
The association of psychosocial characteristics with postpartum depression is presented in Table 3. Women with existing psychiatric illness (cOR = 4.2, 95% CI 1.1,5.9; p = 0.024) and those with family history of psychiatric illness (cOR = 3.5, 95% CI 1.5,8.6; p = 0.003) had significantly more postpartum depression than those without. Significant association was also observed for those women who reported existing (cOR = 8.3, 95% CI 3.5, 19.8; p < 0.001) or past family conflict (cOR = 2.6, 95%CI 1.4,4.6; p = 0.001), and lack of support from spouse (cOR = 4.4, 95% CI 2.3,8.5; p < 0.001) and family during pregnancy (cOR = 5.3, 95% CI 2.6,10.6; p < 0.001).

Table 3.
Association of psychosocial characteristics with postpartum depression.
Multivariate regression analysis was performed using only those variables that were found significant in univariate analysis shown in Table 4. Existing family conflict, lack of support by spouse, and lack of family support during pregnancy were identified as predictors for PPD. Women who had reported existing family conflict were at six times higher risk for developing postpartum depression compared to those women who did not (aOR = 6.5, 95% CI = 2.3,18.4). Women who did not receive care or support from their spouse during pregnancy faced more than two-fold increased risk for postpartum depression (aOR = 2.3, 95% CI 1.0,4.8) compared to those who were supported by their spouses. Women who had not received family support during the pregnancy period were more than three times more (aOR = 3.5, 95 % CI 1.6–7.7) likely to experience postpartum depression.

Table 4.
Multivariate logistic regression analysis for the predictors of PPD.
3. Discussion
Postpartum depression (PPD) is a major depressive disorder and is recognized as an important public health problem for women of reproductive age. It has long-term implications for the mother and infant. Untreated PPD causes maternal distress that affects parenting, maternal bonding, and also the infant’s emotional, cognitive, and behavioral development [20,28,29]. It has been repeatedly reported that early diagnosis would help in implementing preventive strategies to prevent the worsening of the problem. As is evident from studies, mothers fail to recognize the symptoms and it is imperative that healthcare providers detect early any symptoms of depression in recently delivered mothers [18]. Hence, this study on postpartum depression among Saudi women would help in informing the current situation to the community and health care providers.
The worldwide prevalence of PPD ranges from 10–33% [3,4,5,6] while the prevalence of PPD in the middle-east region ranges from 17.6% to 51% [7,8,9,10,11,12]. Prevalence rates differ due to cross-cultural and social factors [21,30]. In a study from India, factors in India, such as poor living conditions, family disputes, crises, financial issues, more children to take care of, and fewer work opportunities, are the factors influencing postpartum depression [31]. Urban, low-income, and married mothers have different risk factors and higher rates of PPD than their more affluent counterparts in Midwest, North America [32].
Within Saudi Arabia, wide differences are reported in the prevalence of PPD ranging from 14–38.5% [13,14,15,16]. The current study observed a higher prevalence (43.4%). This difference can be explained by the difference in study method used, diagnostic criteria, the cutoff point for screening, and time of screening and location of the study. The cutoff point for screening was 2–6 months in the study by Al-Asoom [13] and 2–3 months by Al-Harbi [15], whereas it was 2 weeks–1 year in our study. Similarly, in the study by Al-Mudayfar [14], the sample size was 1200, and cutoff point was also different from our study.
A considerable body of research has examined multiple risk factors to be associated with postpartum depression. These include socio-demographic, obstetric, and psychosocial factors. In the current study, no associations were observed with any of the socio-demographic factors. This is in resonance with other studies in Saudi Arabia [13,14,15,16].
Maternal health during pregnancy and some obstetric factors increase the risk of development of post-partum depression [33]. Studies in Saudi Arabia reported that mothers who have poor health during pregnancy premature delivery, unplanned pregnancy, and delivery by cesarean section have a significant risk for subsequently developing postnatal depression [13,14,15,16]. Surprisingly, no such association was observed in the current study except multigravidity. Association with gravidity could be due to stress related to successive pregnancies and caring for many children at the same time.
The psychosocial factors that increase mothers’ risk for postpartum depression include prior history of depression, family history of depression, lack of family support, marital conflict, stressful life events, such as involvement in violent relationships, and traumatic experiences [6,12,21,22]. Research from the region consistently reported stressful life events and traumatic experiences, such as current family conflict, a non-supportive spouse, and a non-supportive family during pregnancy, as predictors of PPD [15,34,35]. This is also reflected in the current study. We identified family conflict, non-supportive spouse, and non-supportive family as predictors of PPD in our study group. Many women experience stress during pregnancy and motherhood. This stress is compounded by a lack of support from a spouse and family. Support provided by the partner as well as by family acts as a buffer against the difficulties in the transition to motherhood and helps to safeguard women’s mental health [33].
Screening for depression in the early postpartum period helps in early detection and prompt treatment of PPD. In Ref. [24], it is recommended that patients who screen positive and meet diagnostic criteria for PPD should receive prompt treatment [25]. A majority of women do not recognize the symptoms of depression and fail to seek help for PPD [18,23]. Therefore, primary care physicians should screen for depression at every opportunity early in the postpartum period. It is expected that the findings of the study can motivate health care providers who work with pregnant women to include assessments of these factors in their routine examinations and to improve the early identification and management of this condition.
4. Strengths and Limitations of the Study
Our study is the first of its kind to examine postpartum depression in this region of Saudi Arabia. It provides a picture of the prevailing situation in this area and shows the size of the problem and the main priorities to be focused on maternal health programs for this population of Saudi Arabia. Despite this, the study has also a number of limitations. Firstly, this study sample selected six urban PHCCs and consecutive sampling was adopted. Thus, the results of this study cannot be generalized to all women from Saudi Arabia. Secondly, the recall bias could not be avoided due to self-reported questionnaire, and all data were extracted from maternal recall. Finally, although this study explored a vast number of factors associated with PPD, there are many other factors, such as hormonal effect, post-natal anemia, marital discord, intimate partner violence, and lack of social support, cultural factors, and other physical health problems that may affect the associations and need exploration.
5. Conclusions
Our study provides evidence that a substantial proportion of Saudi women experience post-partum depression. Family conflict, non-supportive spouses, and non-supportive families act as precursors of PPD. Increasing the awareness of women, men and family members about potential risk factors of PPD can be a preventive strategy. Healthcare providers need to be aware of and receive appropriate training on dealing with the psychosocial aspects of women’s health. PPD screening should be an integral part of postnatal care as early identification of high-risk women could help to prevent post-partum depression and its complications.
Author Contributions
Conceptualization, N.F.A.-S.; Methodology, N.F.A.-S., A.F.S. and S.N.K.; Software, M.A.A. and H.A.A.; Formal analysis, A.F.S. and S.N.K.; Investigation, S.A.S.A.-S.A., N.F.A.-S. and M.A.A.; Resources, S.A.S.A.-S.A., M.A.A., H.A.A., S.A.A.-Q. and A.A.A.; Data curation, N.F.A.-S. and H.A.A.; Writing—original draft, A.F.S. and S.N.K.; Writing—review & editing, A.F.S., S.N.K., M.A.A., S.A.A.-Q. and A.A.A.; Visualization, S.A.A.-Q. and A.A.A.; Supervision, S.N.K.; Project administration, S.A.S.A.-S.A. and N.F.A.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional ethics committee of King Khalid University, Abha, Saudi Arabia, with approval number REC: 2016/05/14.
Informed Consent Statement
Written informed consent was taken.
Data Availability Statement
The data is available with the first author.
Conflicts of Interest
All authors declare no conflict of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Rezaie-Keikhaie, K.; Arbabshastan, M.E.; Rafiemanesh, H.; Amirshahi, M.; Mogharabi, S.; Sarjou, A.A. Prevalence of the Maternity Blues in the Postpartum Period. J. Obstet. Gynecol. Neonatal Nurs. 2020, 49, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Earls, M.F.; Yogman, M.W.; Mattson, G.; Rafferty, J.; Committee on Psychosocial Aspects of Child And Family Health. Incorporating Recognition and Management of Perinatal Depression Into Pediatric Practice. Pediatrics 2019, 143, e20183259. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Maternal Mental Health. Available online: http://www.who.int/mental_health/maternal-child/maternal_mental_health/en/ (accessed on 15 March 2018).
- Fisher, J.; Cabral de Mello, M.; Patel, V.; Rahman, A.; Tran, T.; Holton, S.; Holmes, W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull. World Health Organ. 2012, 90, 139G–149G. [Google Scholar] [CrossRef] [PubMed]
- Kerie, S.; Menberu, M.; Niguse, W. Prevalence and associated factors of postpartum depression in Southwest, Ethiopia, 2017: A cross-sectional study. BMC Res. Notes 2018, 11, 623. [Google Scholar] [CrossRef]
- Bener, A.; Burgut, F.T.; Ghuloum, S.; Sheikh, J.A. Study of Postpartum Depression in a Fast Developing Country: Prevalence and Related Factors. In Proceedings of the 12th International Mental Health Conference: Personality Disorders: Out of the Darkness, GoldCoast, Australia, 24–26 August 2011. [Google Scholar]
- Hanach, N.; Radwan, H.; Fakhry, R.; Dennis, C.L.; Issa, W.B.; Faris, M.E.; Obaid, R.S.; Al Marzooqi, S.; Tabet, C.; De Vries, N. Prevalence and risk factors of postpartum depression among women living in the United Arab Emirates. Soc. Psychiatry. Psychiatr. Epidemiol. 2023, 58, 395–407. [Google Scholar] [CrossRef]
- Al-Hinai, F.I. Prospective study on prevalence and risk factors of postpartum depression in Al Dakhliya Governorate in Oman. Oman Med. J. 2014, 29, 198–202. [Google Scholar] [CrossRef]
- Mohamed, N.A.; Mahmoud, G.A.; Said, N.A.; Abdelhafez, H.A.; Maklof, A.M.A. Postpartum depression: Prevalence and predictors among women at El Eman’s Specialized Hospital. J. Am. Sci. 2011, 7, 122–128. [Google Scholar]
- Mohammad, K.I.; Gamble, J.; Creedy, D.K. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. J. Midwifery Womens Health 2011, 27, e238–e245. [Google Scholar] [CrossRef]
- Vaezi, A.; Soojoodi, F.; Banihashemi, A.T.; Nojomi, M. The association between social support and postpartum depression in women: A cross sectional study. Women Birth. 2019, 32, e238–e242. [Google Scholar] [CrossRef]
- Alasoom, L.I.; Koura, M.R. Predictors of postpartum depression in the eastern province capital of saudi arabia. J. Family Med. Prim. Care 2014, 3, 146–150. [Google Scholar] [CrossRef]
- Al-Modayfer, O.; Alatiq, Y.; Khair, O.; Abdelkawi, S. Postpartum depression and related risk factors among Saudi females. Int. J. Cult. Ment. Health 2015, 8, 316–324. [Google Scholar] [CrossRef]
- Al Nasr, R.S.; Altharwi, K.; Derbah, M.S.; Gharibo, S.O.; Fallatah, S.A.; Alotaibi, S.G.; Almutairi, K.A.; Asdaq, S.M.B. Prevalence and predictors of postpartum depression in Riyadh, Saudi Arabia: A cross sectional study. PLoS ONE 2020, 15, e0228666. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.A.; Abdulghani, H.M. Risk factors associated with postpartum depression in the Saudi population. Neuropsychiatr. Dis. Treat. 2014, 10, 311–316. [Google Scholar] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, C.P.; Kwasky, A.N.; Groh, C.J. Social Support, Postpartum Depression, and Professional Assistance: A Survey of Mothers in the Midwestern United States. J. Perinat. Educ. 2015, 24, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Kingston, D.; Tough, S.; Whitfield, H. Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child. Psychiatry Hum. Dev. 2012, 43, 683–714. [Google Scholar] [CrossRef]
- Mirhosseini, H.; Moosavipoor, S.A.; Nazari, M.A.; Dehghan, A.; Mirhosseini, S.; Bidaki, R.; Yazdian-Anari, P. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron. Physician. 2015, 7, 1673–1679. [Google Scholar] [CrossRef] [PubMed]
- Evagorou, O.; Arvaniti, A.; Samakouri, M. Cross-Cultural Approach of Postpartum Depression: Manifestation, Practices Applied, Risk Factors and Therapeutic Interventions. Psychiatr. Q. 2016, 87, 129–154. [Google Scholar] [CrossRef]
- Escribà-Agüir, V.; Artazcoz, L. Gender differences in postpartum depression: A longitudinal cohort study. J. Epidemiol. Community Health 2011, 65, 320–326. [Google Scholar] [CrossRef]
- Almutairi, A.F.; Salam, M.; Alanazi, S.; Alweldawi, M.; Alsomali, N.; Alotaibi, N. Impact of help-seeking behavior and partner support on postpartum depression among Saudi women. Neuropsychiatr. Dis. Treat. 2017, 13, 1929–1936. [Google Scholar] [CrossRef]
- Liberto, T.L. Screening for Depression and Help-Seeking in Postpartum Women During Well-Baby Pediatric Visits: An Integrated Review. J. Pediatr. Health Care 2012, 26, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Bobo, W.V.; Yawn, B.P. Concise Review for Physicians and other Clinicians: Postpartum Depression. Mayo ClinProc. 2014, 89, 835–844. [Google Scholar] [CrossRef]
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Ghubash, R.; Abou-Saleh, M.; Daradkeh, T.K. The validity of the Arabic Edinburgh Postnatal Depression Scale. Soc. Psychiatry Psychiatr. Epidemiol. 1997, 32, 474–476. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.; Holden, J.; Sagovsky, R. Detection of postnatal depression: Development of the 10 item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- IBM Corp. Released. IBM SPSS Statistics for Windows; Version 22.0; IBM Corp: Armonk, NY, USA, 2013. [Google Scholar]
- Abdollahi, F.; Lye, M.S.; Md Zain, A.; Shariff Ghazali, S.; Zarghami, M. Postnatal depression and its associated factors in women from different cultures. Iran J. Psychiatry Behav. Sci. 2011, 5, 5–11. [Google Scholar]
- Shelke, A.; Chakole, S. A Review on Risk Factors of Postpartum Depression in India and Its Management. Cureus 2022, 14, e29150. [Google Scholar] [CrossRef]
- Garfield, L.; Holditch-Davis, D.; Carter, C.S.; McFarlin, B.L.; Schwertz, D.; Seng, J.S.; Giurgescu, C.; White-Traut, R. Risk factors for postpartum depressive symptoms in low-income women with very low-birth-weight infants. Adv. Neonatal Care 2015, 15, E3–E8. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Ghaedrahmati, M.; Kazemi, A.; Kheirabadi, G.; Ebrahimi, A.; Bahrami, M. Postpartum depression risk factors: A narrative review. J. Educ. Health Promot. 2017, 6, 60. [Google Scholar] [CrossRef]
- Haque, A.; Namawar, A.; Breene, K.A. Prevalence and Risk Factors of Postpartum Depression in Middle Eastern/Arab Women. J. Muslim Ment. Health 2015, 9, 65–84. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).