RETRACTED: Clinical Effect of Arthroscopic Resection of Extra-Articular Knee Osteochondroma
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Patient Selection
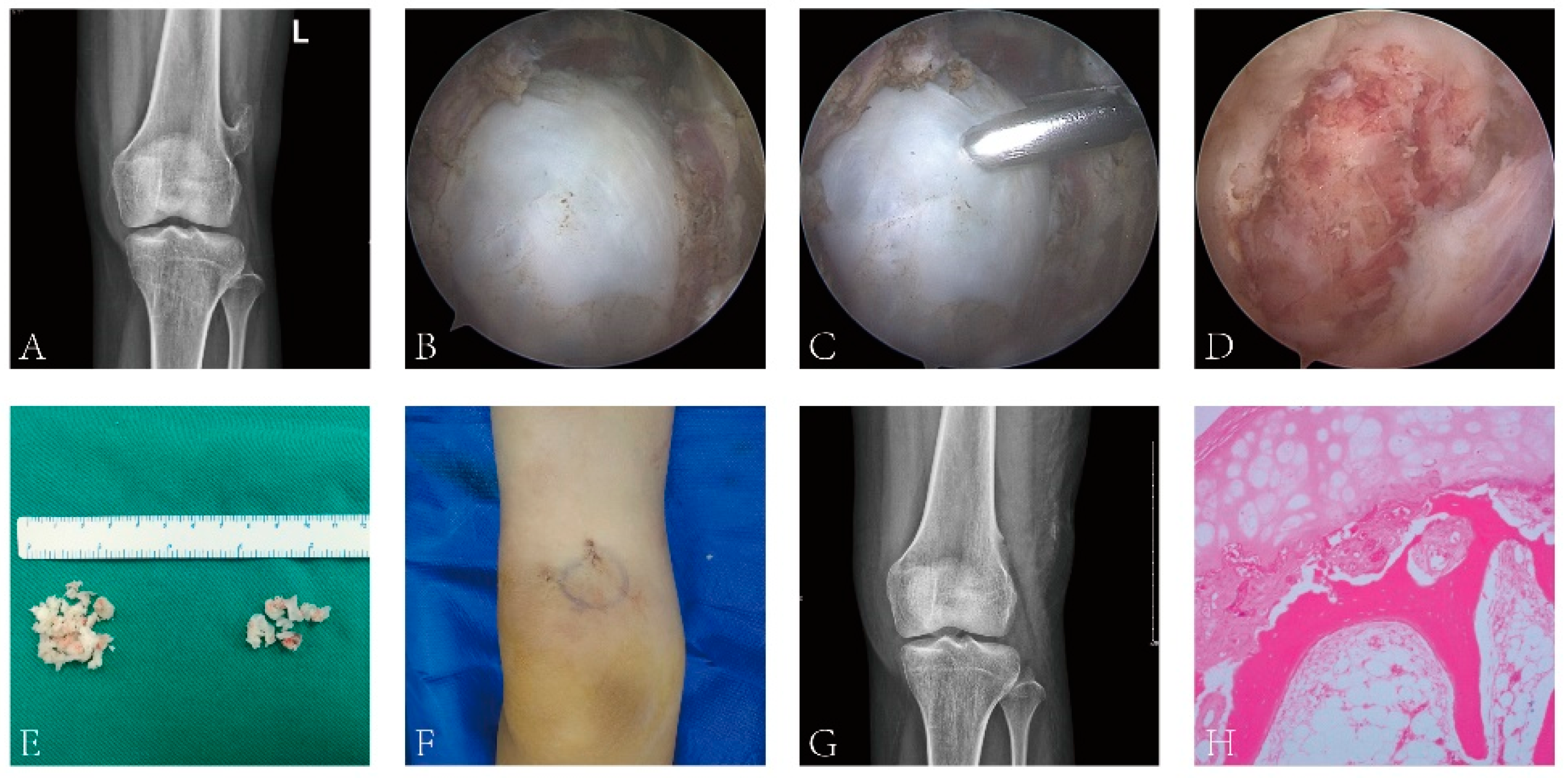
2.3. Surgical Technique
2.4. Clinical Assessment
2.5. Statistical Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hakim, D.N.; Pelly, T.; Kulendran, M.; Caris, J.A. Benign tumours of the bone: A review. J. Bone Oncol. 2015, 4, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.R.; Tan, T.-S.; Unni, K.K.; Collins, M.S.; Wenger, D.E.; Sim, F.H. Secondary Chondrosarcoma in Osteochondroma: Report of 107 Patients. Clin. Orthop. Relat. Res. 2003, 411, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Bottner, F.; Rodl, R.; Kordish, I.; Winkelmann, W.; Gosheger, G.; Lindner, N. Surgical treatment of symptomatic osteochon-droma. A three- to eight-year follow-up study. J. Bone. Jt. Surg. Br. 2003, 85, 1161–1165. [Google Scholar] [CrossRef]
- Sakamoto, A.; Okamoto, T.; Matsuda, S. Subvastus approach for resection of subvastus osteochondroma in the distal femur. Asian J. Surg. 2019, 42, 842–843. [Google Scholar] [CrossRef] [PubMed]
- Wirganowicz, P.Z.; Watts, H.G. Surgical Risk for Elective Excision of Benign Exostoses. J. Pediatr. Orthop. 1997, 17, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Bigony, L. Arthroscopic surgery: A historical perspective. Orthop. Nurs. 2008, 27, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Konstantinos, M.; Georgios, K.; Konstantinos, S.; Konstantinos, S.; Georgios, T. The Evolution of the Surgical Treatment of Sports Injuries in the 20th Century: A Historical Perspective. Surg. Innov. 2016, 23, 538–542. [Google Scholar] [CrossRef]
- Bohnsack, M. Arthroscopic decompression of extra-articular subspinal hip impingement. Oper. Orthop. Traumatol. 2018, 30, 87–97. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, P.-Y.; Ku, M.-C.; Wu, N.-Y.; Lo, C.-S. Extra-articular endoscopic excision of symptomatic popliteal cyst with failed initial conservative treatment: A novel technique. Orthop. Traumatol. Surg. Res. 2019, 105, 125–128. [Google Scholar] [CrossRef]
- Zhang, X.; Jiang, X.; He, F.; Liang, Z.; You, T.; Jin, D.; Zhang, W. Arthroscopic revision release of gluteal muscle contracture after failed primary open surgery. Int. Orthop. 2016, 41, 1521–1526. [Google Scholar] [CrossRef]
- Ruan, W.; Cao, L.; Chen, Z.; Kong, M.; Bi, Q. Novel exostosin-2 mutation identified in a Chinese family with hereditary multiple oste-ochon-droma. Oncol. Lett. 2018, 15, 4383–4389. [Google Scholar]
- Takahashi, M.; Nishihara, A.; Ohishi, T.; Shiga, K.; Yamamoto, K.; Nagano, A. Arthroscopic resection of an intra-articular osteochondroma of the knee in the patient with multiple osteochondromatosis. Arthroscopy 2004, 20 (Suppl. 2), 28–31. [Google Scholar] [CrossRef] [PubMed]
- Porter, D.E.; Lonie, L.; Fraser, M.; Porter, A.P.D.-S.; Monaco, A.H.R.W. Severity of disease and risk of malignant change in hereditary multiple exostoses. A gen-otype-phenotype study. J. Bone. Jt. Surg. Br. 2004, 86, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, J.; Wang, Z.; Tang, J.; Yu, T. A genotype-phenotype study of hereditary multiple exostoses in forty-six Chinese patients. BMC Med. Genet. 2017, 18, 126. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Kwon, J.H.; Park, Y.J.; D'Almeida, V.R.; Soni, S.M.; Wook, K. Arthroscopic Excision of Solitary Intra-articular Osteochondroma of the Knee. Knee. Surg. Relat. Res. 2013, 25, 36–39. [Google Scholar] [CrossRef]
- Ayerza, M.A.; Abalo, E.; Aponte-Tinao, L.; Muscolo, D.L. Endoscopic resection of symptomatic osteochondroma of the distal femur. Clin. Orthop. Relat. Res. 2007, 459, 150–153. [Google Scholar] [CrossRef]
- Diaz, A.A.; Miguel, A. Endoscopic resection of a distal femoral osteochondroma: Description of the technique and case report. Arthroscopy 2002, 18, 23E. [Google Scholar] [CrossRef]
- Kim, C.H.; Kekatpure, A.L.; Kashikar, A.; Suk, C.J.; Yeon, J.M.; Whan, Y.P. Arthroscopic Excision of a Solitary Acetabular Osteochondroma in an Adult: A Case Report. JBJS. Case. Connect. 2016, 6, e101. [Google Scholar] [CrossRef]
- Masquefa, T.; Dunet, B.; Verdier, N.; Pallar, T. Arthroscopic resection of benign tumors of the knee posterior compartment: A report of 15 cases. Orthop. Traumatol. Surg. Res. 2015, 101, 543–546. [Google Scholar] [CrossRef]
- Padua, R.; Castagna, A.; Ceccarelli, E.; Bondì, R.; Alviti, F.; Padua, L. Intracapsular osteochondroma of the humeral head in an adult causing restriction of motion: A case report. J. Shoulder. Elb. Surg. 2009, 18, e30–e31. [Google Scholar] [CrossRef]
- Kim, J.R.; Lee, J.H.; Wang, S.I. Arthroscopic management of lesser tuberosity osteochondroma causing impingement and sub-scapularis tear of the shoulder. Knee. Surg. Sport. Traumatol. Arthrosc. 2017, 25, 2225–2229. [Google Scholar] [CrossRef] [PubMed]
- Aalderink, K.; Wolf, B. Scapular osteochondroma treated with arthroscopic excision using prone positioning. Am. J. Orthop. Belle Mead. NJ. 2010, 39, E11–E14. [Google Scholar] [PubMed]
- Fukunaga, S.; Futani, H.; Yoshiya, S. Endoscopically assisted resection of a scapular osteochondroma causing snapping scapula syndrome. World J. Surg. Oncol. 2007, 5, 37. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.; Cano, J.R.; Caballero, J.; López, L. Minimally-invasive resection of a scapular osteochondroma. Interact. Cardiovasc. Thorac. Surg. 2011, 13, 468–470. [Google Scholar] [CrossRef]
- van Riet, R.P.; Van Glabbeek, F. Arthroscopic resection of a symptomatic snapping subscapular osteochondroma. Acta. Orthop. Belg. 2007, 73, 252–254. [Google Scholar]
- Gudas, R.; Pocius, A. Endoscopic removal of the osteochondroma of the fibular head. Medicina 2013, 49, 191–194. [Google Scholar] [CrossRef]
- Khosla, A.; Parry, R.L. Costal osteochondroma causing pneumothorax in an adolescent: A case report and review of the literature. J. Pediatr. Surg. 2010, 45, 2250–2253. [Google Scholar] [CrossRef]
- Tsakotos, G.; Tokis, A.; Vlasis, K.; Demesticha, T.; Skandalakis, P.; Filippou, D.; Piagkou, M. Arthroscopic resection of extra-articular knee osteochondroma: Report of two cases. J. Surg. Case Rep. 2019, 2019, z167. [Google Scholar] [CrossRef]
- You, T.; Zhang, X.T.; Zha, Z.G.; Zhang, W.T. Congenital heart disease in adolescents with gluteal muscle contracture. Medicine 2015, 94, e488. [Google Scholar] [CrossRef]
- Morbidi, M.; Ventura, A.; Della, R.C. Arthroscopic assisted resection of juxta-articular osteoid osteoma. J. Foot. Ankle. Surg. 2007, 46, 470–473. [Google Scholar] [CrossRef]
- Tamam, C.; Howse, E.A.; Tamam, M.; Barnes, R.H.; Kelsey, T.J.; Perry, B.; Stubbs, A.J. Arthroscopic Excision of Acetabular Osteoid Osteoma: Computer Tomography-Guided Approach. Arthrosc. Tech. 2015, 4, e101–e105. [Google Scholar] [CrossRef] [PubMed]
- Goyal, T.; Pandita, N.; Paul, S. Arthroscopic excision of intraarticular subperiosteal osteoid osteoma of elbow: A case report. SICOT J. 2018, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Tong, K.; Liu, H.; Wang, X.; Zhong, Z.; Cao, S.; Zhong, C.; Wang, G. Osteochondroma: Review of 431 patients from one medical institution in South China. J. Bone. Oncol. 2017, 8, 23–29. [Google Scholar] [CrossRef] [PubMed]
| Preoperative | 3 Months after Surgery | 6 Months after Surgery | 12 Months after Surgery | ≥24 Months after Surgery | p-Value | |
|---|---|---|---|---|---|---|
| VAS | 3.6 ± 1.1 | 1.3 ± 0.6 * | 0.5 ± 0.1 */** | 0.3 ± 0.06 */** | 0.1 ± 0.02 */** | <0.001 |
| Lysholm | 44.5 ± 2.3 | 70.1 ± 3.6 * | 87.9 ± 4.2 */** | 90.2 ± 4.7 */** | 91.3 ± 4.9 */** | <0.001 |
| IKDC | 53.7 ± 2.6 | 82.1 ± 3.7 * | 88.9 ± 4.1 */** | 92.4 ± 4.6 */** | 94.2 ± 5.1 */** | <0.001 |
| Tegner | 4.6 ± 1.2 | 6.5 ± 1.4 * | 8.0 ± 1.6 * | 8.9 ± 2.0 */** | 9.4 ± 1.4 */** | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.; Shen, L.; Long, Q.; Dai, W.; Jiang, X.; Li, C.; Zuo, J.; Guo, J.; Zhang, X. RETRACTED: Clinical Effect of Arthroscopic Resection of Extra-Articular Knee Osteochondroma. J. Clin. Med. 2023, 12, 52. https://doi.org/10.3390/jcm12010052
Chen P, Shen L, Long Q, Dai W, Jiang X, Li C, Zuo J, Guo J, Zhang X. RETRACTED: Clinical Effect of Arthroscopic Resection of Extra-Articular Knee Osteochondroma. Journal of Clinical Medicine. 2023; 12(1):52. https://doi.org/10.3390/jcm12010052
Chicago/Turabian StyleChen, Peng, Li Shen, Qiong Long, Wei Dai, Xiaocheng Jiang, Canfeng Li, Jianwei Zuo, Jiang Guo, and Xintao Zhang. 2023. "RETRACTED: Clinical Effect of Arthroscopic Resection of Extra-Articular Knee Osteochondroma" Journal of Clinical Medicine 12, no. 1: 52. https://doi.org/10.3390/jcm12010052
APA StyleChen, P., Shen, L., Long, Q., Dai, W., Jiang, X., Li, C., Zuo, J., Guo, J., & Zhang, X. (2023). RETRACTED: Clinical Effect of Arthroscopic Resection of Extra-Articular Knee Osteochondroma. Journal of Clinical Medicine, 12(1), 52. https://doi.org/10.3390/jcm12010052





