The Prevalence and Characteristics of Chronic Ankle Instability in Elite Athletes of Different Sports: A Cross-Sectional Study
Abstract
1. Introduction
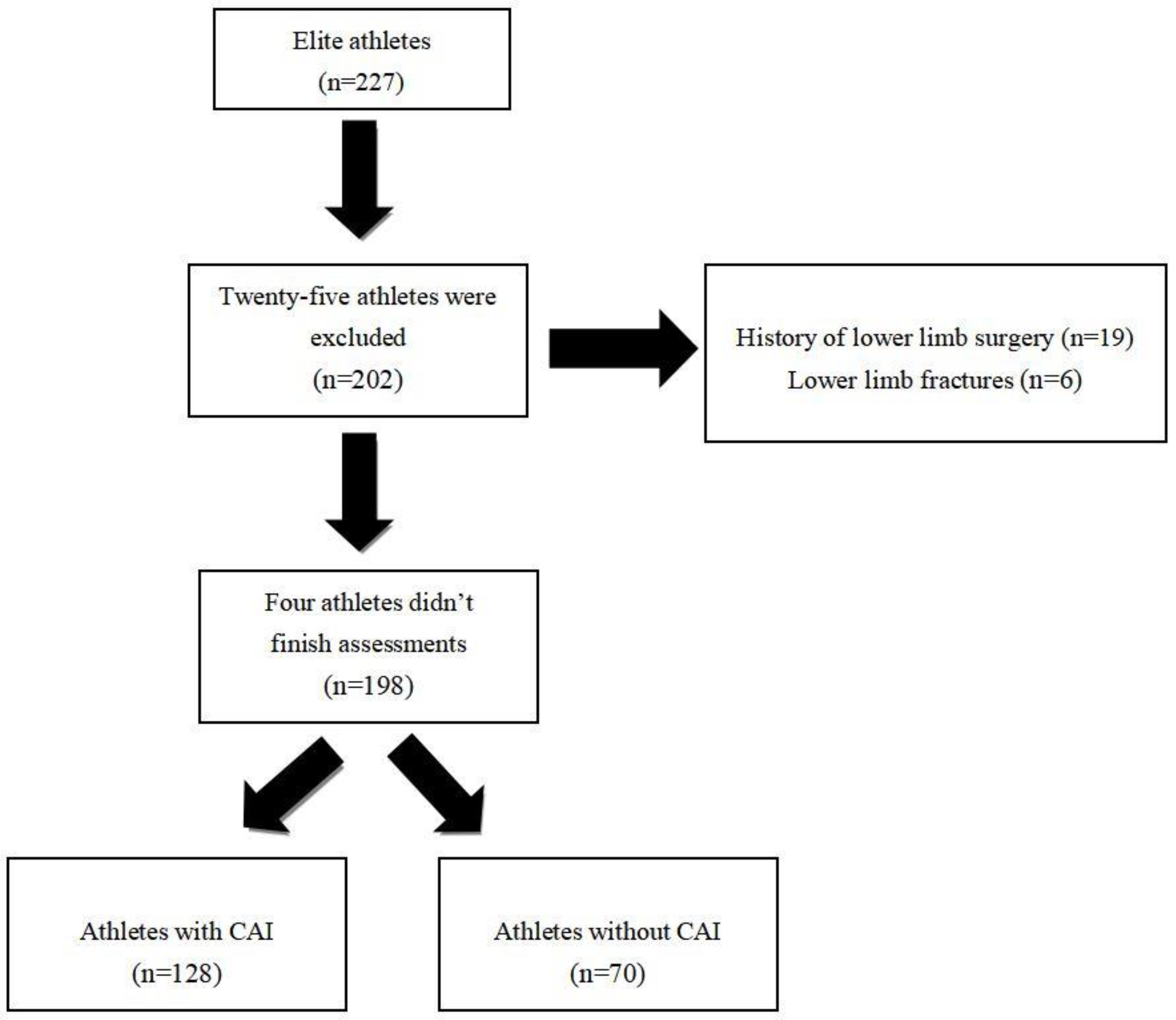
2. Materials and Methods
2.1. Study Design
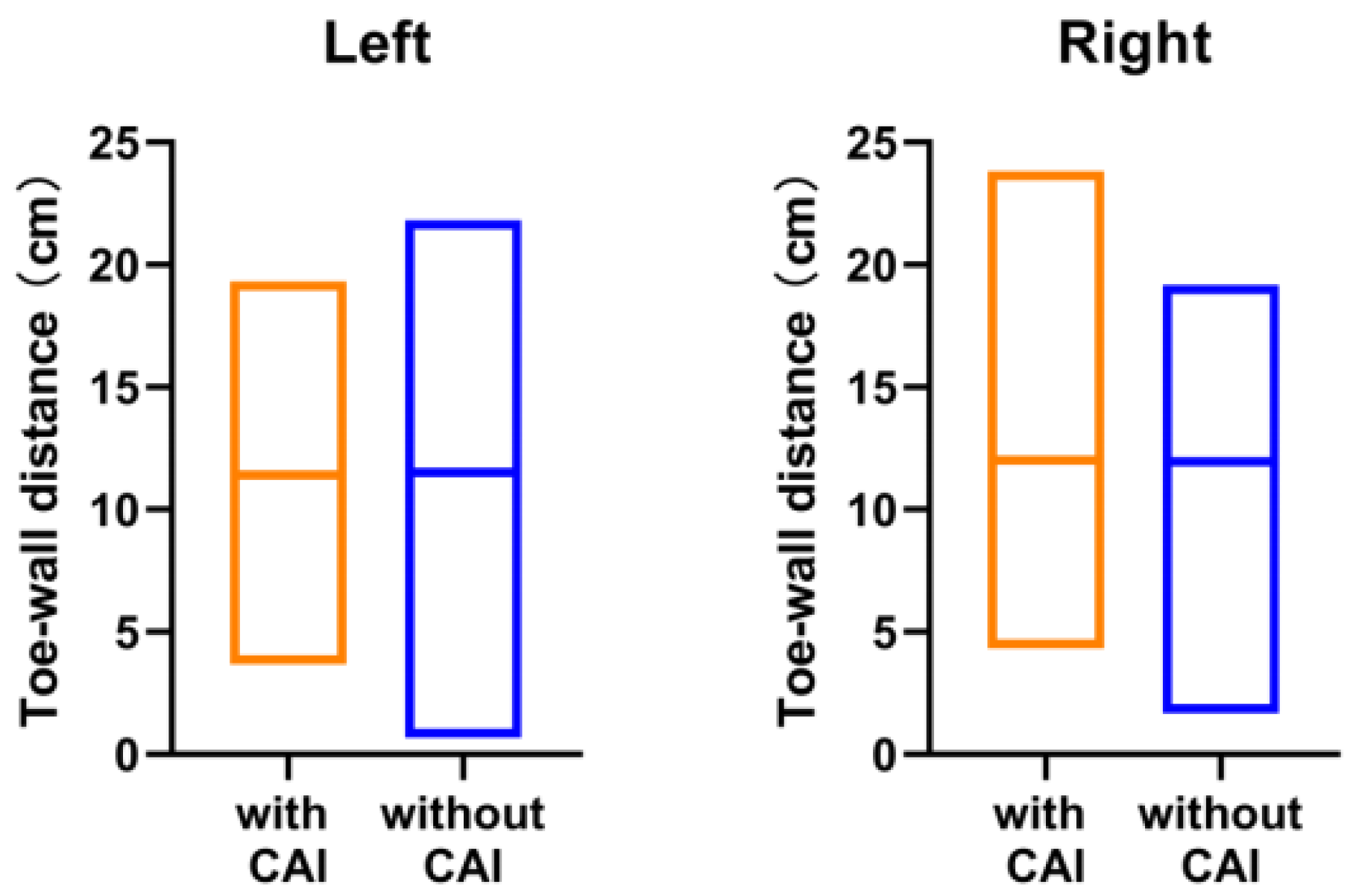
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The Incidence and Prevalence of Ankle Sprain Injury: A Systematic Review and Meta-Analysis of Prospective Epidemiological Studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Roos, K.G.; Kerr, Z.Y.; Mauntel, T.C.; Djoko, A.; Dompier, T.P.; Wikstrom, E. The Epidemiology of Lateral Ligament Complex Ankle Sprains in National Collegiate Athletic Association Sports. Am. J. Sports Med. 2017, 45, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. Br. J. Sports Med. 2014, 48, 1014–1018. [Google Scholar] [CrossRef]
- Lin, C.-I.; Mayer, F.; Wippert, P.-M. The prevalence of chronic ankle instability in basketball athletes: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 2022, 14, 27. [Google Scholar] [CrossRef]
- Valderrabano, V.; Hintermann, B.; Horisberger, M.; Fung, T.S. Ligamentous Posttraumatic Ankle Osteoarthritis. Am. J. Sports Med. 2006, 34, 612–620. [Google Scholar] [CrossRef]
- Valderrabano, V.; Horisberger, M.; Russell, I.; Dougall, H.; Hintermann, B. Etiology of Ankle Osteoarthritis. Clin. Orthop. Relat. Res. 2008, 467, 1800–1806. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1496–1505. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic Ankle Instability: Evolution of the Model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef]
- Hertel, J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Bleakley, C.; Wagemans, J.; Netterström-Wedin, F. Understanding chronic ankle instability: Model rich, data poor. Br. J. Sports Med. 2021, 55, 463–464. [Google Scholar] [CrossRef]
- Donovan, L.; Hetzel, S.; Laufenberg, C.R.; McGuine, T.A. Prevalence and Impact of Chronic Ankle Instability in Adolescent Athletes. Orthop. J. Sports Med. 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Koshino, Y.; Samukawa, M.; Murata, H.; Osuka, S.; Kasahara, S.; Yamanaka, M.; Tohyama, H. Prevalence and characteristics of chronic ankle instability and copers identified by the criteria for research and clinical practice in collegiate athletes. Phys. Ther. Sport 2020, 45, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Attenborough, A.S.; Hiller, C.E.; Smith, R.M.; Stuelcken, M.; Greene, A.; Sinclair, P.J. Chronic Ankle Instability in Sporting Populations. Sports Med. 2014, 44, 1545–1556. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland Ankle Instability Tool: A Report of Validity and Reliability Testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- McPoil, T.G.; Cornwall, M.W.; Medoff, L.; Vicenzino, B.; Forsberg, K.; Hilz, D. Arch height change during sit-to-stand: An alternative for the navicular drop test. J. Foot Ankle Res. 2008, 1, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Langarika-Rocafort, A.; Emparanza, J.I.; Aramendi, J.F.; Castellano, J.; Calleja-González, J. Intra-rater reliability and agreement of various methods of measurement to assess dorsiflexion in the Weight Bearing Dorsiflexion Lunge Test (WBLT) among female athletes. Phys. Ther. Sport 2017, 23, 37–44. [Google Scholar] [CrossRef]
- Anandacoomarasamy, A.; Barnsley, L.; Grujic, L. Long term outcomes of inversion ankle injuries * Commentary. Br. J. Sports Med. 2005, 39, e14; discussion e14. [Google Scholar] [CrossRef]
- Gerber, J.P.; Williams, G.N.; Scoville, C.R.; Arciero, R.C.; Taylor, D.C. Persistent disability associated with ankle sprains: A prospective examination of an athletic population. Foot Ankle Int. 1998, 19, 653–660. [Google Scholar] [CrossRef]
- Tanen, L.; Docherty, C.L.; Van Der Pol, B.; Simon, J.; Schrader, J. Prevalence of Chronic Ankle Instability in High School and Division I Athletes. Foot Ankle Spéc. 2014, 7, 37–44. [Google Scholar] [CrossRef]
- Baldwin, J.N.; McKay, M.; Hiller, C.E.; Nightingale, E.J.; Moloney, N.; Burns, J.; Chard, A.; Ferreira, P.; Yan, A.F.; Hawke, F.; et al. Correlates of Perceived Ankle Instability in Healthy Individuals Aged 8 to 101 Years. Arch. Phys. Med. Rehabil. 2017, 98, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Takabayashi, T.; Kudo, S.; Edama, M. The prevalence of chronic ankle instability and its relationship to foot arch characteristics in female collegiate athletes. Phys. Ther. Sport 2020, 46, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Attenborough, A.S.; Sinclair, P.; Sharp, T.; Greene, A.; Stuelcken, M.; Smith, R.M.; Hiller, C.E. A snapshot of chronic ankle instability in a cohort of netball players. J. Sci. Med. Sport 2015, 19, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Khowailed, I.A.; Lee, H. Neuromuscular Control of Ankle-stabilizing Muscles-specific Effects of Sex and Menstrual Cycle. Int. J. Sports Med. 2021, 42, 270–276. [Google Scholar] [CrossRef]
- Wilkerson, R.D.; Mason, M.A. Differences in men’s and women’s mean ankle ligamentous laxity. Iowa Orthop. J. 2000, 20, 46–48. [Google Scholar]
- Ericksen, H.; Gribble, P.A. Sex differences, hormone fluctuations, ankle stability, and dynamic postural control. J. Athl. Train. 2012, 47, 143–148. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Renström, P.A.; Alosa, D.M.; Baumhauer, J.F.; Vacek, P.M. Ankle ligament injury risk factors: A prospective study of college athletes. J. Orthop. Res. 2001, 19, 213–220. [Google Scholar] [CrossRef]
- Eiling, E.; Bryant, A.L.; Petersen, W.; Murphy, A.; Hohmann, E. Effects of menstrual-cycle hormone fluctuations on musculotendinous stiffness and knee joint laxity. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 126–132. [Google Scholar] [CrossRef]
- Zuil-Escobar, J.C.; Martínez-Cepa, C.B.; Martín-Urrialde, J.A.; Gómez-Conesa, A. Medial Longitudinal Arch: Accuracy, Reliability, and Correlation Between Navicular Drop Test and Footprint Parameters. J. Manip. Physiol. Ther. 2018, 41, 672–679. [Google Scholar] [CrossRef]
- Ashraf, T.; Asif, M.; Abdul, S.; Khalfe, H.; Mehmood; Hafiza, A.; Muhammad, H.; Farrag; Muhammad, F.; Qureshi, M.F.; et al. Prevalence of Flat Foot and High Arch Foot among undergraduate Physical Therapy students by using Navicular Drop Test. IJART 2017, 6, 21–28. [Google Scholar]
- Martin, R.L.; Davenport, T.E.; Paulseth, S.; Wukich, D.K.; Godges, J.J. Ankle Stability and Movement Coordination Impairments: Ankle Ligament Sprains. J. Orthop. Sports Phys. Ther. 2013, 43, A1–A40. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.; Chang, G.; Alaia, M.; Jazrawi, L.; Gonzalez-Lomas, G. Lower extremity injuries in U.S. national fencing team members and U.S. fencing Olympians. Physician Sport. 2022, 50, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.-P.; Hong, Y.; Chan, L.K.; Yung, P.S.-H.; Chan, K.-M. A Systematic Review on Ankle Injury and Ankle Sprain in Sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Benouaich, L.; Rouch, P.; Natta, F.; Thoreux, P. Spring jumpers vs power jumpers: Ankle joint behavior in elite wushu athletes and implications for performance and injury risk. Comput. Methods Biomech. Biomed. Eng. 2015, 18 (Suppl. 1), 1886–1887. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tsang, R.C.-C.; Liu, D.; Ruan, B.; Yu, Y.; Gao, Q. Applicability of cutoff scores of Chinese Cumberland Ankle Instability Tool and Foot and Ankle Ability Measure as inclusion criteria for study of chronic ankle instability in Chinese individuals. Phys. Ther. Sport 2021, 48, 116–120. [Google Scholar] [CrossRef]
- Wang, W.; Liao, D.; Kang, X.; Zheng, W.; Xu, W.; Chen, S.; Xie, Q. Development of a valid Chinese version of the Cumberland Ankle Instability Tool in Chinese-speaking patients with chronic ankle instability disorders. Sci. Rep. 2021, 11, 9747. [Google Scholar] [CrossRef]
- Sesma, A.R.; Mattacola, C.G.; Uhl, T.L.; Nitz, A.J.; McKeon, P.Q. Effect of foot orthotics on single- and double-limb dynamic balance tasks in patients with chronic ankle instability. Foot Ankle Spec 2008, 1, 330–337. [Google Scholar] [CrossRef]
- Sawkins, K.; Refshauge, K.; Kilbreath, S.; Raymond, J. The Placebo Effect of Ankle Taping in Ankle Instability. Med. Sci. Sports Exerc. 2007, 39, 781–787. [Google Scholar] [CrossRef]
- Malliaropoulos, N.; Papacostas, E.; Papalada, A.; Maffulli, N. Acute Lateral Ankle Sprains in Track and Field Athletes: An Expanded Classification. Foot Ankle Clin. 2006, 11, 497–507. [Google Scholar] [CrossRef]
- Tohyama, H.; Yasuda, K.; Ohkoshi, Y.; Beynnon, B.D.; Renstrom, P.A. Anterior Drawer Test for Acute Anterior Talofibular Ligament Injuries of the Ankle: How Much Load Should be Applied during the Test? Am. J. Sport. Med. 2003, 31, 226–232. [Google Scholar] [CrossRef]
- Bahr, R.; Pena, F.; Shine, J.; Lew, W.D.; Lindquist, C.; Tyrdal, S.; Engebretsen, L. Mechanics of the anterior drawer and talar tilt tests: A cadaveric study of lateral ligament injuries of the ankle. Acta Orthop. Scand. 1997, 68, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Luo, Z.-P.; Kitaoka, H.B.; An, K.-N. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin. Biomech. 2000, 15, 619–623. [Google Scholar] [CrossRef] [PubMed]


| CAI (n = 128) | without CAI (n = 70) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p | |
| Age (year) | 21.33 (3.91) | 20.97 ± 3.76 | 0.584 |
| Height (cm) | 172.72 (15.73) | 175.24 ± 15.22 | 0.966 |
| Weight (kg) | 65.55 (17.45) | 67.36 ± 15.76 | 0.636 |
| BMI (kg/m2) | 21.63 (3.24) | 21.75 (3.44) | 0.806 |
| CAIT score | |||
| Left ankle | 20.78 (5.27) | 27.80 (1.83) | <0.001 |
| Right ankle | 19.64 (5.93) | 27.80 (1.82) | <0.001 |
| Female (n = 69) | Male (n = 129) | ||
|---|---|---|---|
| n (%) | n (%) | p | |
| Ankle sprain history | |||
| Previous ankle sprain | 62 (89.86) | 108 (83.72) | 0.238 |
| No ankle sprain | 7 (10.14) | 21 (16.28) | |
| CAI prevalence | |||
| No CAI | 15 (21.74) | 55 (42.64) | 0.010 |
| Unilateral CAI | 19 (27.54) | 31 (24.03) | |
| Bilateral CAI | 35 (50.72) | 43 (33.33) |
| Sport | Total | Ankle Sprain History | CAI Prevalence | |||
|---|---|---|---|---|---|---|
| Previous Ankle Sprain | No Ankle Sprain | No CAI | Unilateral CAI | Bilateral CAI | ||
| n | n (%) | n (%) | n (%) | n (%) | n (%) | |
| All | 198 | 170 (85.9) | 28 (14.1) | 70 (35.4) | 50 (25.3) | 78 (39.4) |
| Diving | 24 | 22 (91.7) | 2 (8.3) | 6 (25.0) | 8 (33.3) | 10 (41.7) |
| Basketball | 40 | 34 (85.0) | 6 (15.0) | 13 (32.5) | 9 (22.5) | 18 (45.0) |
| Weightlifting | 19 | 16 (84.2) | 3 (15.8) | 6 (31.6) | 3 (15.8) | 10 (52.6) |
| Badminton | 20 | 15 (75.0) | 5 (25.0) | 7 (35.0) | 5 (25.0) | 8 (40.0) |
| Track and field | 20 | 17 (85.0) | 3 (15.0) | 8 (40.0) | 5 (25.0) | 7 (35.0) |
| Fencing | 23 | 17 (73.9) | 6 (26.1) | 15 (65.2) | 3 (13.0) | 5 (21.7) |
| Sanda | 12 | 10 (83.3) | 2 (16.7) | 4 (33.3) | 3 (25.0) | 5 (41.7) |
| Trampolining | 20 | 19 (95.0) | 1 (5.0) | 5 (25.0) | 8 (40.0) | 7 (35.0) |
| Gymnastics | 20 | 20 (100.0) | 0 (0.0) | 6 (30.0) | 6 (30.0) | 8 (40.0) |
| Sport | Total | Acrobatics (n = 54) | Contact (n = 52) | Non-Contact (n = 82) | Differences between Groups | |||
|---|---|---|---|---|---|---|---|---|
| without CAI | with CAI | without CAI | with CAI | without CAI | with CAI | |||
| n | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| All | 198 | 17 (26.6%) | 47 (73.4%) | 17 (32.7 %) | 35 (67.3%) | 36 (43.9%) | 46 (56.1%) | X2(2) = 4.947, p = 0.08 |
| Female | 69 | 2 (7.1%) | 26 (92.9%) | 3 (23.1%) | 10 (76.9%) | 10 (35.7%) | 18 (64.3%) | X2(2) = 6.734, p = 0.03 |
| Male | 129 | 15 (41.7%) | 21 (58.3%) | 14 (35.9%) | 25 (64.1%) | 26 (48.1%) | 28 (51.9%) | X2(2) = 1.409, p = 0.49 |
| Sport | Total | Left Ankle | Right Ankle | ||||
|---|---|---|---|---|---|---|---|
| CAI | ADT(+) in CAI | TTT(+) in CAI | CAI | ADT(+) in CAI | TTT(+) in CAI | ||
| n | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| All | 198 | 100 (50.5) | 72 (72.0) | 46 (46.0) | 106 (53.5) | 79 (74.5) | 45 (42.5) |
| Diving | 24 | 12 (50.0) | 8 (66.7) | 8 (66.7) | 16 (66.7) | 13 (81.3) | 4 (25.0) |
| Basketball | 40 | 21 (52.5) | 17 (81.0) | 12 (57.1) | 24 (60.0) | 15 (62.5) | 9 (37.5) |
| Weightlifting | 19 | 10 (52.6) | 6 (60.0) | 4 (40.0) | 13 (68.4) | 10 (76.9) | 6 (46.2) |
| Badminton | 20 | 10 (50.0) | 8 (80.0) | 7 (70.0) | 11 (55.0) | 7 (63.6) | 5 (45.5) |
| Track and field | 20 | 11 (55.0) | 10 (90.9) | 4 (36.4) | 8 (40.0) | 7 (87.5) | 3 (37.5) |
| Fencing | 23 | 5 (21.7) | 5 (100.0) | 3 (60.0) | 8 (34.8) | 8 (100.0) | 4 (50.0) |
| Sanda | 12 | 6 (50.0) | 4 (66.7) | 2 (33.3) | 7 (58.3) | 6 (85.7) | 4 (57.1) |
| Trampolining | 20 | 13 (65.0) | 8 (61.5) | 4 (30.8) | 9 (45.0) | 9 (100.0) | 6 (66.7) |
| Gymnastics | 20 | 12 (60.0) | 6 (50.0) | 2 (16.7) | 10 (50.0) | 4 (40.0) | 4 (40.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Chen, N.; Wang, J.; Zhang, Z.; Jiang, C.; Chen, Z.; Fang, J.; Peng, J.; Li, W.; Song, B. The Prevalence and Characteristics of Chronic Ankle Instability in Elite Athletes of Different Sports: A Cross-Sectional Study. J. Clin. Med. 2022, 11, 7478. https://doi.org/10.3390/jcm11247478
Zhang C, Chen N, Wang J, Zhang Z, Jiang C, Chen Z, Fang J, Peng J, Li W, Song B. The Prevalence and Characteristics of Chronic Ankle Instability in Elite Athletes of Different Sports: A Cross-Sectional Study. Journal of Clinical Medicine. 2022; 11(24):7478. https://doi.org/10.3390/jcm11247478
Chicago/Turabian StyleZhang, Congda, Na Chen, Jingsong Wang, Zhengzheng Zhang, Chuan Jiang, Zhong Chen, Jianhui Fang, Juhua Peng, Weiping Li, and Bin Song. 2022. "The Prevalence and Characteristics of Chronic Ankle Instability in Elite Athletes of Different Sports: A Cross-Sectional Study" Journal of Clinical Medicine 11, no. 24: 7478. https://doi.org/10.3390/jcm11247478
APA StyleZhang, C., Chen, N., Wang, J., Zhang, Z., Jiang, C., Chen, Z., Fang, J., Peng, J., Li, W., & Song, B. (2022). The Prevalence and Characteristics of Chronic Ankle Instability in Elite Athletes of Different Sports: A Cross-Sectional Study. Journal of Clinical Medicine, 11(24), 7478. https://doi.org/10.3390/jcm11247478









