Prevalence and Methods for Assessment of Oropharyngeal Dysphagia in Older Adults: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
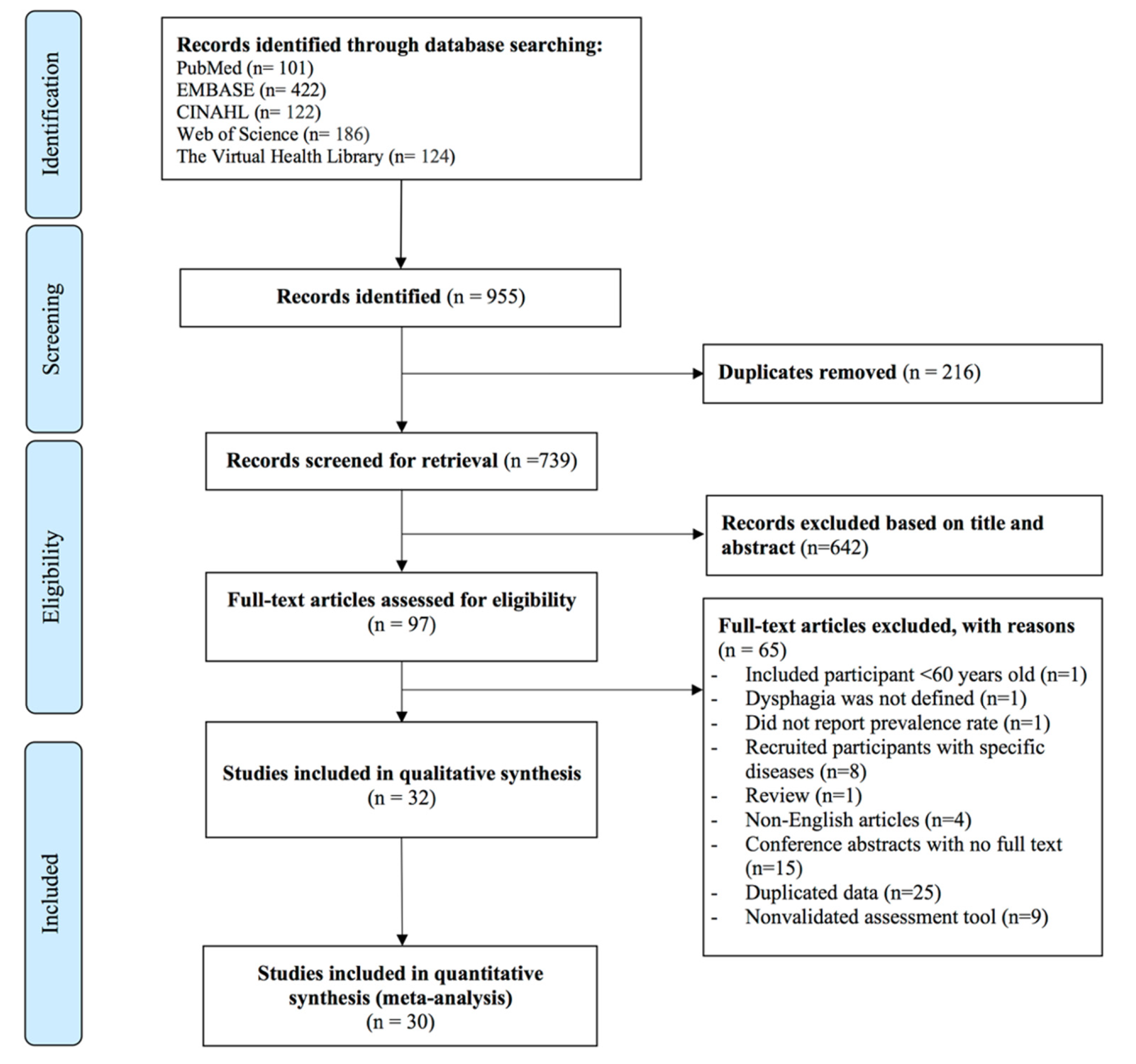
2.2. Search Strategy and Screening Process
2.3. Assessment of the Risk of Bias
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Characteristics of Studies
3.3. Study Methodology Evaluation
3.4. Prevalence of Dysphagia in the Elderly
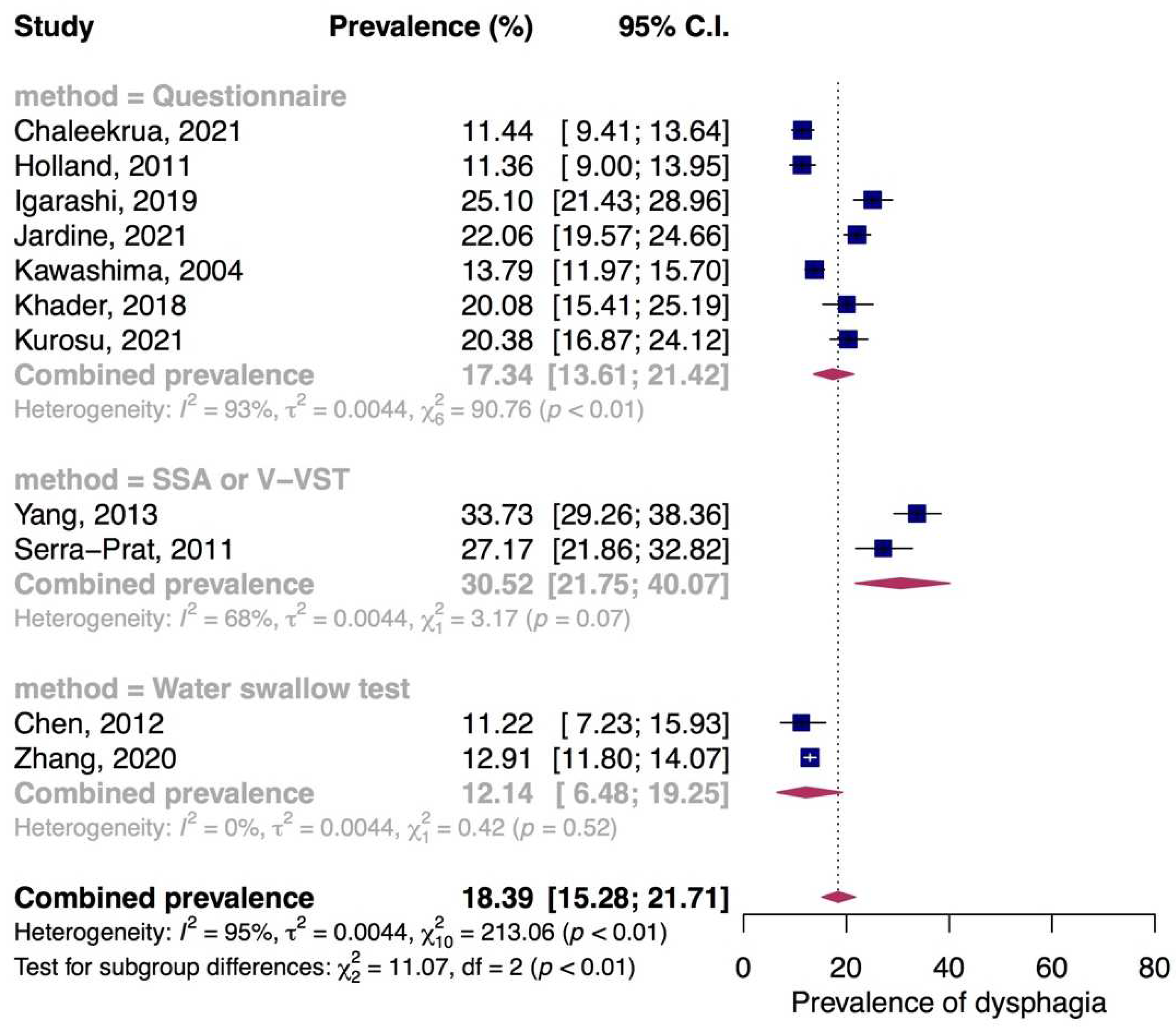
3.4.1. Prevalence of Dysphagia in Community-Dwelling Elderly
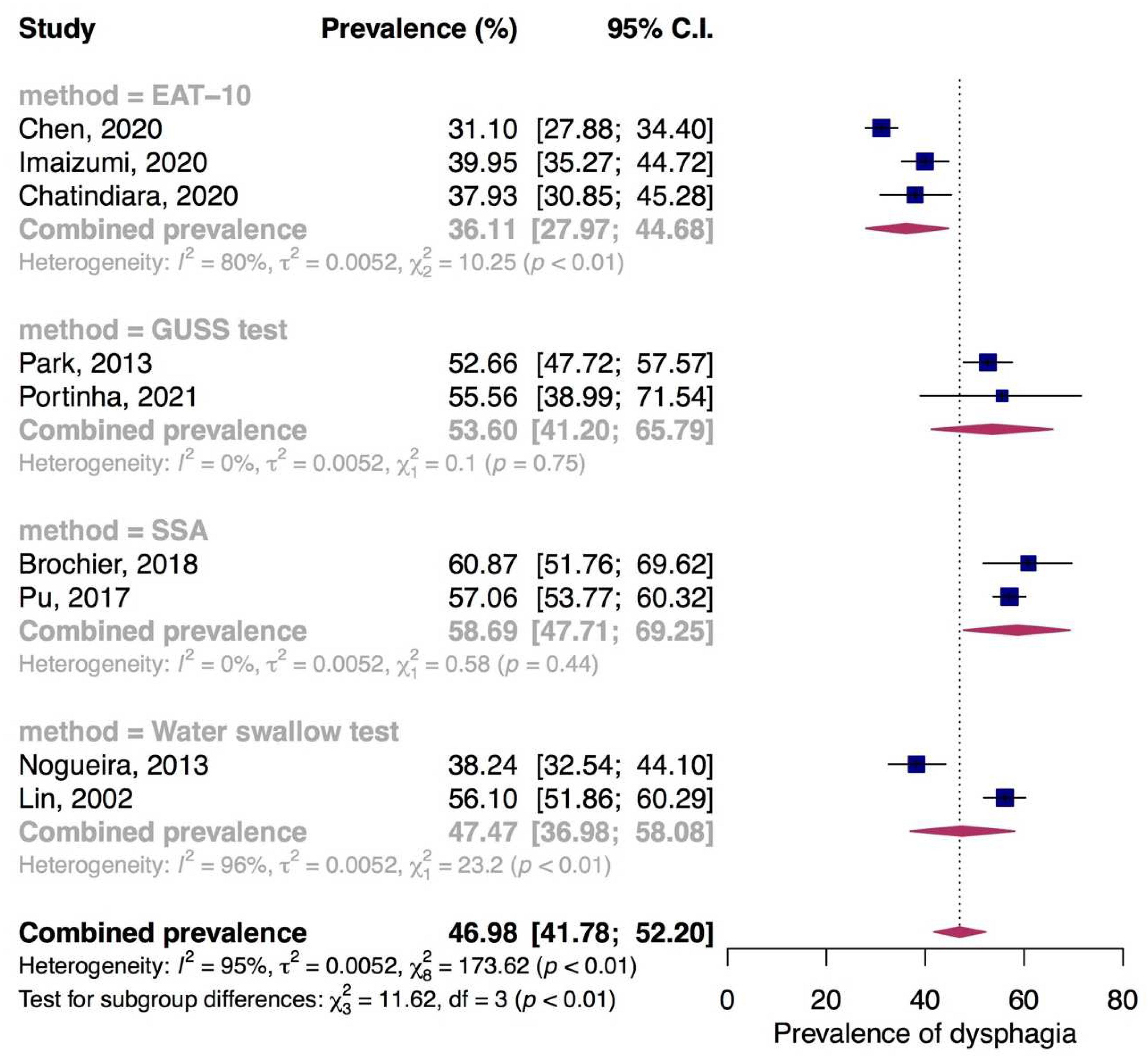
3.4.2. Prevalence of Dysphagia in Nursing Home Residents
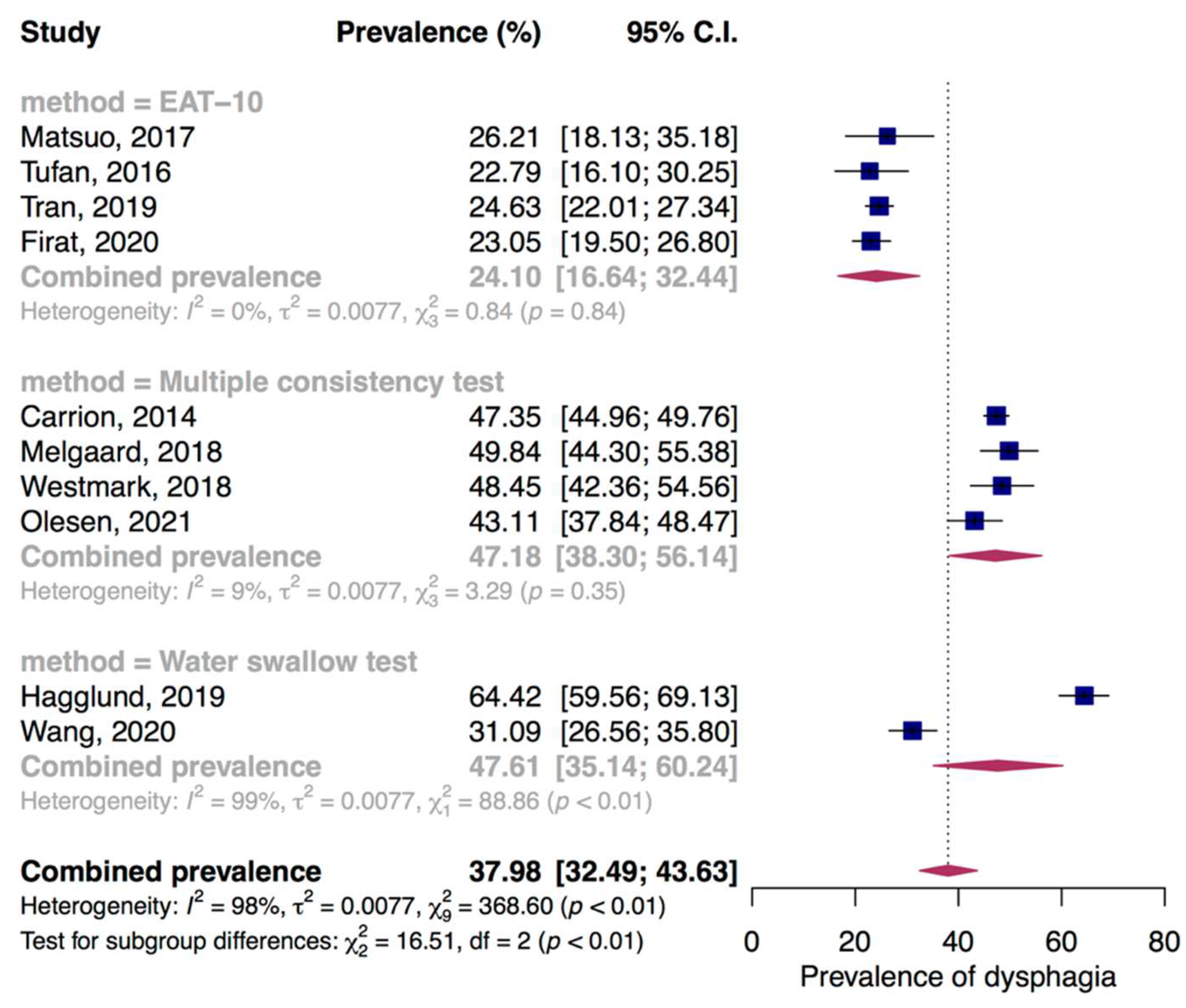
3.4.3. Prevalence of Dysphagia in Hospitalized Older Adults
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Life Expectancy and Healthy Life Expecancy—Data by Country; WHO: Geneva, Switzerland, 2020.
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430); United Nations: New York, NY, USA, 2019. [Google Scholar]
- Malagelada, J.R.; Bazzoli, F.; Boeckxstaens, G.; De Looze, D.; Fried, M.; Kahrilas, P.; Lindberg, G.; Malfertheiner, P.; Salis, G.; Sharma, P.; et al. World Gastroenterology Organisation Global Guidelines: Dysphagia—Global Guidelines and Cascades Update September 2014. J. Clin. Gastroenterol. 2015, 49, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Humbert, I.A.; Robbins, J. Dysphagia in the Elderly. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 853–866. [Google Scholar] [CrossRef] [PubMed]
- Malandraki, G.A.; Perlman, A.L.; Karampinos, D.C.; Sutton, B.P. Reduced Somatosensory Activations in Swallowing with Age. Hum. Brain Mapp. 2011, 32, 730–743. [Google Scholar] [CrossRef]
- Nicosia, M.A.; Hind, J.A.; Roecker, E.B.; Carnes, M.; Doyle, J.; Dengel, G.A.; Robbins, J. Age Effects on the Temporal Evolution of Isometric and Swallowing Pressure. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M634–M640. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, H.; Ekberg, O.; Olsson, R.; Hindfelt, B. Quantitative Aspects of Swallowing in an Elderly Nondysphagic Population. Dysphagia 1996, 11, 180–184. [Google Scholar] [CrossRef]
- Steele, C.M.; Van Lieshout, P. Tongue Movements during Water Swallowing in Healthy Young and Older Adults. J. Speech Lang. Hear. Res. 2009, 52, 1255–1267. [Google Scholar] [CrossRef]
- Logemann, J.A.; Pauloski, B.R.; Rademaker, A.W.; Colangelo, L.A.; Kahrilas, P.J.; Smith, C.H. Temporal and Biomechanical Characteristics of Oropharyngeal Swallow in Younger and Older Men. J. Speech Lang. Hear. Res. 2000, 43, 1264–1274. [Google Scholar] [CrossRef]
- Dejaeger, E.; Pelemans, W. Swallowing and the Duration of the Hyoid Movement in Normal Adults of Different Ages. Aging 1996, 8, 130–134. [Google Scholar] [CrossRef]
- Cook, I.J.; Weltman, M.D.; Wallace, K.; Shaw, D.W.; McKay, E.; Smart, R.C.; Butler, S.P. Influence of Aging on Oral-Pharyngeal Bolus Transit and Clearance during Swallowing: Scintigraphic Study. Am. J. Physiol. 1994, 266, G972–G977. [Google Scholar] [CrossRef]
- Aviv, J.E.; Martin, J.H.; Jones, M.E.; Wee, T.A.; Diamond, B.; Keen, M.S.; Blitzer, A. Age-Related Changes in Pharyngeal and Supraglottic Sensation. Ann. Otol. Rhinol. Laryngol. 1994, 103, 749–752. [Google Scholar] [CrossRef]
- Ebihara, S.; Sekiya, H.; Miyagi, M.; Ebihara, T.; Okazaki, T. Dysphagia, Dystussia, and Aspiration Pneumonia in Elderly People. J. Thorac. Dis. 2016, 8, 632–639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serra-Prat, M.; Palomera, M.; Gomez, C.; Sar-Shalom, D.; Saiz, A.; Montoya, J.G.; Navajas, M.; Palomera, E.; Clavé, P. Oropharyngeal Dysphagia as a Risk Factor for Malnutrition and Lower Respiratory Tract Infection in Independently Living Older Persons: A Population-Based Prospective Study. Age Ageing 2012, 41, 376–381. [Google Scholar] [CrossRef] [Green Version]
- Morley, J.E. Dysphagia and Aspiration. J. Am. Med. Dir. Assoc. 2015, 16, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Altman, K.W.; Yu, G.P.; Schaefer, S.D. Consequence of Dysphagia in the Hospitalized Patient: Impact on Prognosis and Hospital Resources. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 784–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hickson, M.; Frost, G. An Investigation into the Relationships between Quality of Life, Nutritional Status and Physical Function. Clin. Nutr. 2004, 23, 213–221. [Google Scholar] [CrossRef]
- Wirth, R.; Pourhassan, M.; Streicher, M.; Hiesmayr, M.; Schindler, K.; Sieber, C.C.; Volkert, D. The Impact of Dysphagia on Mortality of Nursing Home Residents: Results From the NutritionDay Project. J. Am. Med. Dir. Assoc. 2018, 19, 775–778. [Google Scholar] [CrossRef]
- Cook, I.J.; Kahrilas, P.J. AGA Technical Review on Management of Oropharyngeal Dysphagia. Gastroenterology 1999, 116, 455–478. [Google Scholar] [CrossRef]
- Belafsky, P.C.; Mouadeb, D.A.; Rees, C.J.; Pryor, J.C.; Postma, G.N.; Allen, J.; Leonard, R.J. Validity and Reliability of the Eating Assessment Tool (EAT-10). Ann. Otol. Rhinol. Laryngol. 2008, 117, 919–924. [Google Scholar] [CrossRef]
- McHorney, C.A.; Robbins, J.; Lomax, K.; Rosenbek, J.C.; Chignell, K.; Kramer, A.E.; Bricker, D.E. The SWAL-QOL and SWAL-CARE Outcomes Tool for Oropharyngeal Dysphagia in Adults: III. Documentation of Reliability and Validity. Dysphagia 2002, 17, 97–114. [Google Scholar] [CrossRef]
- DePippo, K.L.; Holas, M.A.; Reding, M.J. Validation of the 3-Oz Water Swallow Test for Aspiration Following Stroke. Arch. Neurol. 1992, 49, 1259–1261. [Google Scholar] [CrossRef]
- Clavé, P.; Arreola, V.; Romea, M.; Medina, L.; Palomera, E.; Serra-Prat, M. Accuracy of the Volume-Viscosity Swallow Test for Clinical Screening of Oropharyngeal Dysphagia and Aspiration. Clin. Nutr. 2008, 27, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Trapl, M.; Enderle, P.; Nowotny, M.; Teuschl, Y.; Matz, K.; Dachenhausen, A.; Brainin, M. Dysphagia Bedside Screening for Acute-Stroke Patients: The Gugging Swallowing Screen. Stroke 2007, 38, 2948–2952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry, L. Screening Swallowing Function of Patients with Acute Stroke. Part Two: Detailed Evaluation of the Tool Used by Nurses. J. Clin. Nurs. 2001, 10, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.-L.; Fu, S.-Y.; Wang, W.-H.; Ma, Y.-C. Validity and Reliability of Swallowing Screening Tools Used by Nurses for Dysphagia: A Systematic Review. Tzu Chi Med. J. 2016, 28, 41–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Speyer, R. Oropharyngeal Dysphagia: Screening and Assessment. Otolaryngol. Clin. N. Am. 2013, 46, 989–1008. [Google Scholar] [CrossRef] [PubMed]
- Langmore, S.E. Evaluation of Oropharyngeal Dysphagia: Which Diagnostic Tool Is Superior? Curr. Opin. Otolaryngol. Head Neck Surg. 2003, 11, 485–489. [Google Scholar] [CrossRef]
- Baijens, L.W.; Clavé, P.; Cras, P.; Ekberg, O.; Forster, A.; Kolb, G.F.; Leners, J.C.; Masiero, S.; Mateos-Nozal, J.; Ortega, O.; et al. European Society for Swallowing Disorders—European Union Geriatric Medicine Society White Paper: Oropharyngeal Dysphagia as a Geriatric Syndrome. Clin. Interv. Aging 2016, 11, 1403–1428. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019 (ST/ESA/SER.A/444); United Nations: New York, NY, USA, 2020. [Google Scholar]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological Quality of Case Series Studies: An Introduction to the JBI Critical Appraisal Tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- González-Fernández, M.; Humbert, I.; Winegrad, H.; Cappola, A.R.; Fried, L.P. Dysphagia in Old-Old Women: Prevalence as Determined According to Self-Report and the 3-Ounce Water Swallowing Test. J. Am. Geriatr. Soc. 2014, 62, 716–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holland, G.; Jayasekeran, V.; Pendleton, N.; Horan, M.; Jones, M.; Hamdy, S. Prevalence and Symptom Profiling of Oropharyngeal Dysphagia in a Communitydwelling Elderly Population: A Self-Reporting Questionnaire Survey. Gut 2009, 58, A109. [Google Scholar]
- Serra-Prat, M.; Hinojosa, G.; López, D.; Juan, M.; Fabré, E.; Voss, D.S.; Calvo, M.; Marta, V.; Ribó, L.; Palomera, E.; et al. Prevalence of Oropharyngeal Dysphagia and Impaired Safety and Efficacy of Swallow in Independently Living Older Persons. J. Am. Geriatr. Soc. 2011, 59, 186–187. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, D.; Reis, E. Swallowing Disorders in Nursing Home Residents: How Can the Problem Be Explained? Clin. Interv. Aging 2013, 8, 221–227. [Google Scholar] [CrossRef] [Green Version]
- Portinha, S.; Sa-Couto, P.; Matos, M.A. Cross-Sectional Study to Investigate the Presence of Sarcopenic Dysphagia in a Portuguese Geriatric Population. J. Stat. Health Decis. 2021, 3, 38–39. [Google Scholar]
- Hägglund, P.; Fält, A.; Hägg, M.; Wester, P.; Levring Jäghagen, E. Swallowing Dysfunction as Risk Factor for Undernutrition in Older People Admitted to Swedish Short-Term Care: A Cross-Sectional Study. Aging Clin. Exp. Res. 2019, 31, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Carríon, S.; Cabré, M.; Monteis, R.; Roca, M.; Palomera, E.; Clavé, P. Association between Oropharyngeal Dysphagia and Malnutrition in Elderly Patients with Acute Diseases Admitted to a General Hospital. Clin. Nutr. 2012, 7, 8. [Google Scholar] [CrossRef]
- Mateos-Nozal, J.; Montero-Errasquín, B.; Sánchez García, E.; Romero Rodríguez, E.; Cruz-Jentoft, A.J. High Prevalence of Oropharyngeal Dysphagia in Acutely Hospitalized Patients Aged 80 Years and Older. J. Am. Med. Dir. Assoc. 2020, 21, 2008–2011. [Google Scholar] [CrossRef]
- Westmark, S.; Melgaard, D.; Rethmeier, L.O.; Ehlers, L.H. The Cost of Dysphagia in Geriatric Patients. Clinicoecon. Outcomes Res. 2018, 10, 321–326. [Google Scholar] [CrossRef] [Green Version]
- Melgaard, D.; Rodrigo-Domingo, M.; Mørch, M.M. The Prevalence of Oropharyngeal Dysphagia in Acute Geriatric Patients. Geriatrics 2018, 3, 15. [Google Scholar] [CrossRef] [Green Version]
- Fırat Ozer, F.; Akın, S.; Soysal, T.; Gokcekuyu, B.M.; Erturk Zararsız, G. Relationship Between Dysphagia and Sarcopenia with Comprehensive Geriatric Evaluation. Dysphagia 2021, 36, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Olesen, M.D.; Modlinski, R.M.; Poulsen, S.H.; Rosenvinge, P.M.; Rasmussen, H.H.; Holst, M. Prevalence of Signs of Dysphagia and Associated Risk Factors in Geriatric Patients Admitted to an Acute Medical Unit. Clin. Nutr. ESPEN 2021, 41, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Chaleekrua, S.; Janpol, K.; Wattanapan, P. Swallowing Problems among Community-Dwelling Elderly in Northeastern Thailand. J. Prim. Care Community Health 2021, 12, 9596. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.Y.; Lin, L.C. Nonimaging Clinical Assessment of Impaired Swallowing in Community-Dwelling Older Adults in Taiwan. J. Nurs. Res. 2012, 20, 272–280. [Google Scholar] [CrossRef] [Green Version]
- Igarashi, K.; Kikutani, T.; Tamura, F. Survey of Suspected Dysphagia Prevalence in Home-Dwelling Older People Using the 10-Item Eating Assessment Tool (EAT-10). PLoS ONE 2019, 14, 211040. [Google Scholar] [CrossRef]
- Kawashima, K.; Motohashi, Y.; Fujishima, I. Prevalence of Dysphagia among Community-Dwelling Elderly Individuals as Estimated Using a Questionnaire for Dysphagia Screening. Dysphagia 2004, 19, 266–271. [Google Scholar] [CrossRef]
- Yang, E.J.; Kim, M.H.; Lim, J.-y.; Paik, N.-J. Oropharyngeal Dysphagia in a Community-Based Elderly Cohort: The Korean Longitudinal Study on Health and Aging. J. Korean Med. Sci. 2013, 28, 1534–1539. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.F.; Guo, F.; Tang, M.; Dai, H.; Sheng, J.; Chen, L.; Liu, S.; Wang, J.; Shi, Y.; Ye, C.; et al. Association between Skeletal Muscle Strength and Dysphagia among Chinese Community-Dwelling Elderly Adults. J. Nutr. Health Aging 2020, 24, 642–649. [Google Scholar] [CrossRef]
- Khader, F.A.; Mubeena, G.S. Swallowing Difficulties among Healthy Elderly: Prevalence and Aetiology. Int. J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 494–498. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Cui, Y.; Ding, Y.P.; Sun, C.X.; Xing, Y.; Zhou, R.; Liu, G.H. Prevalence and Risk Factors of Dysphagia among Nursing Home Residents in Eastern China: A Cross-Sectional Study. BMC Geriatr. 2020, 20, 352. [Google Scholar] [CrossRef]
- Park, Y.-H.; Han, H.-R.; Oh, B.-M.; Lee, J.; Park, J.-a.; Yu, S.J.; Chang, H. Prevalence and Associated Factors of Dysphagia in Nursing Home Residents. Geriatr. Nurs. 2013, 34, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.C.; Wu, S.C.; Chen, H.S.; Wang, T.G.; Chen, M.Y. Prevalence of Impaired Swallowing in Institutionalized Older People in Taiwan. J. Am. Geriatr. Soc. 2002, 50, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Imaizumi, M.; Suzuki, T.; Ikeda, M.; Matsuzuka, T.; Goto, A.; Omori, K. Implementing a Flexible Endoscopic Evaluation of Swallowing at Elderly Care Facilities to Reveal Characteristics of Elderly Subjects Who Screened Positive for a Swallowing Disorder. Auris Nasus Larynx 2020, 47, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Pu, D.; Murry, T.; Wong, M.C.M.; Yiu, E.M.L.; Chan, K.M.K. Indicators of Dysphagia in Aged Care Facilities. J. Speech Lang. Hear. Res. 2017, 60, 2416–2426. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zhao, Y.; Guo, A. Association of Swallowing Problems with Frailty in Chinese Hospitalized Older Patients. Int. J. Nurs. Sci. 2020, 7, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.P.; Nguyen, N.T.; Kayashita, J.; Shimura, F.; Yamamoto, S. Dysphagia Prevalence among Elderly in Some Vietnamese Hospitals. Asian J. Diet 2019, 1, 48–52. [Google Scholar]
- Matsuo, H.; Yoshimura, Y.; Ishizaki, N.; Ueno, T. Dysphagia Is Associated with Functional Decline during Acute-Care Hospitalization of Older Patients. Geriatr. Gerontol. Int. 2017, 17, 1610–1616. [Google Scholar] [CrossRef]
- Kurosu, A.; Osman, F.; Daggett, S.; Peña-Chávez, R.; Thompson, A.; Myers, S.M.; VanKampen, P.; Koenig, S.S.; Ciucci, M.; Mahoney, J.; et al. Factors Associated with Self-Reported Dysphagia in Older Adults Receiving Meal Support. J. Nutr. Health Aging 2021, 25, 1145–1153. [Google Scholar] [CrossRef]
- Tufan, A. Screening Oropharyngeal Dysphagia in Hospitalized Older Adults: A Prevalent Problem Associated with Mortality. Marmara Med. J. 2016, 29, 152–156. [Google Scholar] [CrossRef] [Green Version]
- Jardine, M.; Miles, A.; Allen, J. Self-reported Swallowing and Nutrition Status in Community-Living Older Adults. Dysphagia 2021, 36, 198–206. [Google Scholar] [CrossRef]
- Chatindiara, I.; Allen, J.; Hettige, D.; Senior, S.; Richter, M.; Kruger, M.; Wham, C. High Prevalence of Malnutrition and Frailty among Older Adults at Admission to Residential Aged Care. J. Prim. Health Care 2020, 12, 305–317. [Google Scholar] [CrossRef] [PubMed]
- Brochier, C.W.; Hugo, F.N.; Rech, R.S.; Baumgarten, A.; Hilgert, J.B. Influence of Dental Factors on Oropharyngeal Dysphagia among Recipients of Long-Term Care. Gerodontology 2018, 35, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, E.; Pongpipatpaiboon, K.; Inamoto, Y.; Kagaya, H. Dysphagia Evaluation and Treatment from the Perspective of Rehabilitation Medicine; Springer: Singapore, 2018; pp. 35–79. [Google Scholar]
- Perry, L. Screening Swallowing Function of Patients with Acute Stroke. Part One: Identification, Implementation and Initial Evaluation of a Screening Tool for Use by Nurses. J. Clin. Nurs. 2001, 10, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Umay, E.; Eyigor, S.; Karahan, A.Y.; Gezer, I.A.; Kurkcu, A.; Keskin, D.; Karaca, G.; Unlu, Z.; Tıkız, C.; Vural, M.; et al. The GUSS Test as a Good Indicator to Evaluate Dysphagia in Healthy Older People: A Multicenter Reliability and Validity Study. Eur. Geriatr. Med. 2019, 10, 879–887. [Google Scholar] [CrossRef]
- Rofes, L.; Arreola, V.; Mukherjee, R.; Clavé, P. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol. Motil. 2014, 26, 1256–1265. [Google Scholar] [CrossRef]
- Etges, C.L.; Scheeren, B.; Gomes, E.; Barbosa Lde, R. Screening Tools for Dysphagia: A Systematic Review. Codas 2014, 26, 343–349. [Google Scholar] [CrossRef] [Green Version]
- Wu, M.C.; Chang, Y.C.; Wang, T.G.; Lin, L.C. Evaluating Swallowing Dysfunction Using a 100-ML Water Swallowing Testa. Dysphagia 2004, 19, 43–47. [Google Scholar] [CrossRef]
- Smithard, D.; Westmark, S.; Melgaard, D. Evaluation of the Prevalence of Screening for Dysphagia among Older People Admitted to Medical Services—An International Survey. OBM Geriatr. 2019, 3, 8. [Google Scholar] [CrossRef] [Green Version]
- Schrock, J.W.; Lou, L.; Ball, B.A.W.; Van Etten, J. The Use of an Emergency Department Dysphagia Screen Is Associated with Decreased Pneumonia in Acute Strokes. Am. J. Emerg. Med. 2018, 36, 2152–2154. [Google Scholar] [CrossRef]
| No. | First Author, Year | Country/Region | Sample Size | Age and Mean Age (Years) | %Women | Specific Eligibility | Tool to Report Dysphagia | Strategy Criteria | Dysphagia Prevalence |
|---|---|---|---|---|---|---|---|---|---|
| Community (n = 12) | |||||||||
| 1 | Chaleekrua, 2021 [46] | Thailand | 874 | ≥60 (69.70 ± 6.79) | 66.2 | Excluded: individuals with neurological diseases, head and neck cancer | EAT-10 | Questionnaire | 11.4% |
| 2 | Chen, 2012 [47] | Taiwan | 216 | ≥65 (74.2 ± 6.33) | 72.2 | Excluded: neurological diseases, stroke < 3 months, cancer, chronic pulmonary diseases | 90 mL WST | Water swallow test | 11.2% |
| 3 | Fernandez, 2014 [34] | USA | 47 | 85 to 94 (89 ± 2.9) | 100 | 90 mL WST | Water swallow test | 72% | |
| 4 | Holland, 2011 [35] | UK | 634 | 69–98 (81 ± 5) | 76.5 | Excluded: individuals with history of neurological diseases | Sydney Swallow Questionnaire | Questionnaire | 11.4% |
| 5 | Igarashi, 2019 [48] | Japan | 510 | ≥65 (75.0 ± 7.2) | Independent older people | EAT-10 | Questionnaire | 25.1% | |
| 6 | Jardine, 2021 [63] | New Zealand | 1020 | ≥65 (75.22 ± 6.24) | 61 | EAT-10 | Questionnaire | 22.1% | |
| 7 | Kawashima, 2004 [49] | Japan | 1313 | ≥65 (74.1 ± 6.9) | 56.2 | Dysphagia Screening Questionnaire | Questionnaire | 13.8% | |
| 8 | Yang, 2013 [50] | South Korea | 415 | ≥65 74 (65–95) | 53.1 | Standardized Swallowing Assessment | Standardized Swallowing Assessment | 33.7% | |
| 9 | Zhang, 2020 [51] | China | 3361 | ≥65 (72.64 ± 6.10) | 51.8 | Excluded: bed-ridden, hearing disorders, serious physiological or psychological illness | 30 mL WST | Water swallow test | 12.9% |
| 10 | Khader, 2018 [52] | India | 259 | ≥60 (66.2 ± 6.2) | 32.8 | Excluded: patients with aspiration risk, neurological diseases, upper GI malignancy, oropharyngeal diseases | Swallowing Disturbance Questionnaire | Questionnaire | 20.1% |
| 11 | Serra-Prat, 2011 [36] | Spain | 254 | ≥70 (78.2 ± 5.6) | 46.5 | Excluded: persons with a life expectancy of less than 3 months | V-VST | Multiple consistency test | 27.2% |
| 12 | Kurosu, 2021 [61] | Japan | 476 | ≥65 (78.5 ± 11.12) | 64.4 | EAT-10 | Questionnaire | 20.4% | |
| Nursing homes (n = 9) | |||||||||
| 13 | Brochier, 2018 [65] | Brazil | 115 | ≥60 | 67 | Standardized Swallowing Assessment | Standardized Swallowing Assessment | 60.9% | |
| 14 | Chen, 2020 [53] | China | 775 | ≥60 (81.3 ± 9.3) | 60.6 | Excluded: intellectual disabilities | EAT-10 | Questionnaire | 31.1% |
| 15 | Nogueira, 2013 [37] | Portugal | 272 | ≥65 (82 ± 10) | 75 | Excluded: low level of consciousness | 90 mL WST | Water swallow test | 38.2% |
| 16 | Park, 2013 [54] | South Korea | 395 | ≥65 (80.7 ± 8.0) | 76.5 | GUSS | Multiple consistency test | 52.7% | |
| 17 | Lin, 2002 [55] | Taiwan | 611 | ≥65 (77 ± 10.8) | 48.1 | 90-mL timed swallowing test | Water swallow test | 56.1% | |
| 18 | Imaizumi, 2020 [56] | Japan | 413 | ≥65 (84.4) | 73.1 | EAT-10 | Questionnaire | 40% | |
| 19 | Pu, 2017 [57] | Hong Kong | 878 | ≥60 (84.5 ± 7.9) | 70.1 | Excluded: not cognizant enough or unfit to be assessed on the day of examination | Standardized Swallowing Assessment | Standardized Swallowing Assessment | 57.1% |
| 20 | Portinha, 2021 [38] | Portugal | 36 | ≥65 (88.0 ± 5.6) | 63.8 | GUSS | Multiple consistency test | 55.6% | |
| 21 | Chatindiara, 2020 [64] | New Zealand | 174 | ≥65 (85.5 ± 7.5) | Excluded: palliative care, dementia, previoulsy diagnosis with swallow disorders, cancer of the larynx or psychiatric eating disorders | EAT-10 | Questionnaire | 37.9% | |
| Hospital (n = 11) | |||||||||
| 22 | Carrion, 2014 [40] | Spain | 1662 | ≥70 (85.1 ± 6.23) | 61.7 | Excluded: terminal patients | V-VST | Multiple consistency test | 47.4% |
| 23 | Mateos, 2020 [41] | Spain | 329 | ≥80 (93.5 ± 4.1) | 68.4 | Excluded: end-of life situations, low level of consciousness, enteral nutrition | V-VST | Multiple consistency test | 82.4% |
| 24 | Matsuo, 2017 [60] | Japan | 103 | ≥65 (80.5 ± 7.9) | 56.3 | Excluded: neurological diseases, head and neck cancer | EAT-10 | Questionnaire | 26.2% |
| 25 | Westmark, 2018 [42] | Denmark | 258 | ≥60 (83.1 ± 7.7) | 54 | Excluded: delirium, severe dementia, terminal patients | V-VST | Multiple consistency test | 48.5% |
| 26 | Tufan, 2016 [62] | Turkey | 136 | ≥65 (74.6 ± 6.6) | 54.4 | EAT-10 | Questionnaire | 23% | |
| 27 | Wang, 2020 [58] | China | 386 | ≥65 (74.76 ± 6.19) | 51.6 | Excluded: Parkinson’s disease, stroke, dementia, myasthenia gravis, head and neck cancer, gastric tubes, tracheal intubation, diagnosed swallowing dysfunction, disorder of consciousness | 30 mL WST | Water swallow test | 31.1% |
| 28 | Hagglund, 2019 [39] | Sweden | 385 | ≥65 81 (65–98) | 53.4 | Excluded: People with end-of-life care, insufficient cognitive capacity | 150-mL timed swallowing test | Water swallow test | 64% |
| 29 | Tran, 2019 [59] | Vietnam | 1007 | ≥65 (75.5) | 58.3 | Excluded: patients with mute, deaf, psychosis, on ventilator, coma, dementia, trauma | EAT-10 | Questionnaire | 24.6% |
| 30 | Melgaard, 2018 [43] | Denmark | 313 | ≥60 (83.1 ± 7.8) | 56 | Excluded: terminal illness, dementia, delirium, hospitalized for less than 24 h | V-VST | Multiple consistency test | 50% |
| 31 | Fırat, 2020 [44] | Turkey | 512 | ≥60 72.1 ± 7.3 | Excluded: severe dementia, head and neck cancer, or acute diseases with clinical deterioration | EAT-10 | Questionnaire | 23% | |
| 32 | Olesen, 2021 [45] | Denmark | 334 | ≥65 78.5 (73–85) | 47.7 | WST + GUSS | Multiple consistency test | 43.1% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doan, T.-N.; Ho, W.-C.; Wang, L.-H.; Chang, F.-C.; Nhu, N.T.; Chou, L.-W. Prevalence and Methods for Assessment of Oropharyngeal Dysphagia in Older Adults: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 2605. https://doi.org/10.3390/jcm11092605
Doan T-N, Ho W-C, Wang L-H, Chang F-C, Nhu NT, Chou L-W. Prevalence and Methods for Assessment of Oropharyngeal Dysphagia in Older Adults: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(9):2605. https://doi.org/10.3390/jcm11092605
Chicago/Turabian StyleDoan, Thanh-Nhan, Wen-Chao Ho, Liang-Hui Wang, Fei-Chun Chang, Nguyen Thanh Nhu, and Li-Wei Chou. 2022. "Prevalence and Methods for Assessment of Oropharyngeal Dysphagia in Older Adults: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 9: 2605. https://doi.org/10.3390/jcm11092605
APA StyleDoan, T.-N., Ho, W.-C., Wang, L.-H., Chang, F.-C., Nhu, N. T., & Chou, L.-W. (2022). Prevalence and Methods for Assessment of Oropharyngeal Dysphagia in Older Adults: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(9), 2605. https://doi.org/10.3390/jcm11092605







