Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of Study Subjects
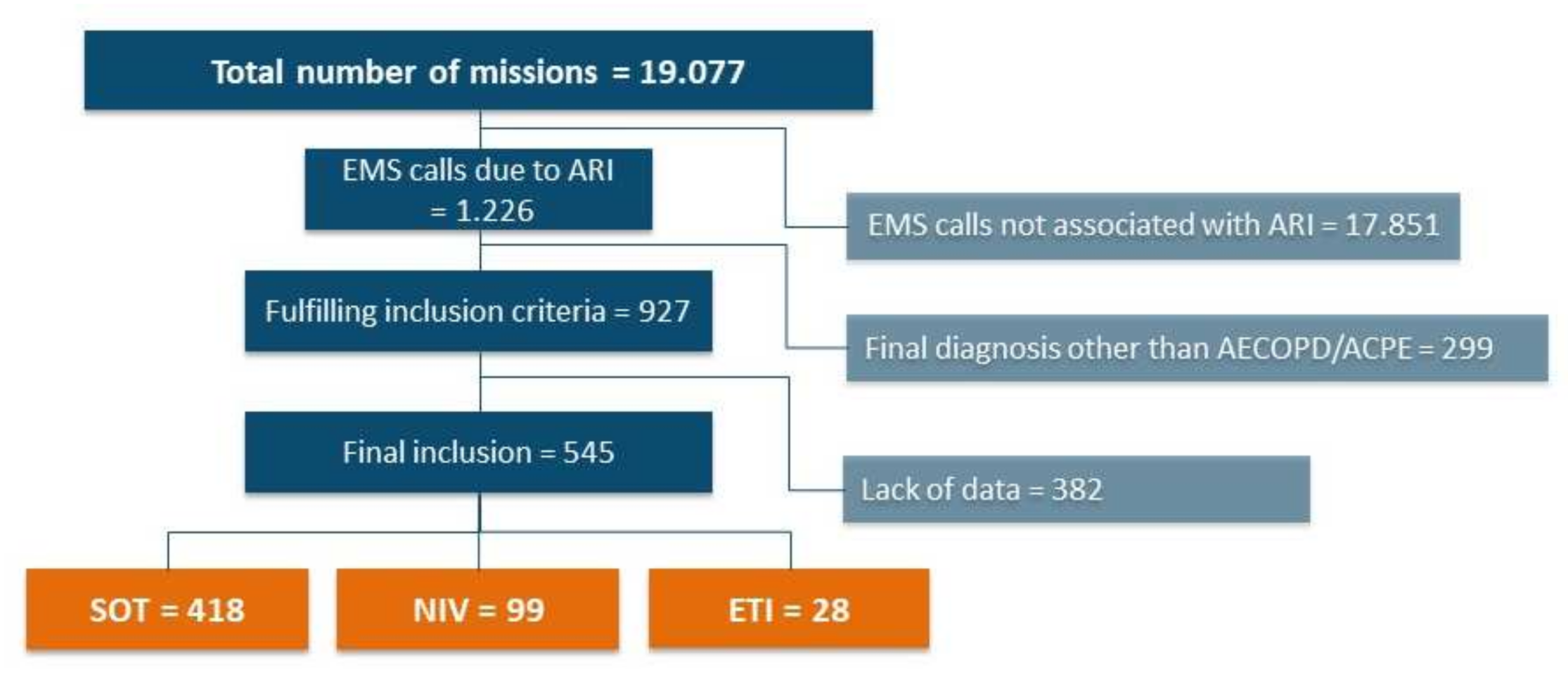
3.1.1. Recruitment and Inclusion
3.1.2. Demographic Data
3.1.3. Initial Clinical Data
3.2. Primary Outcomes
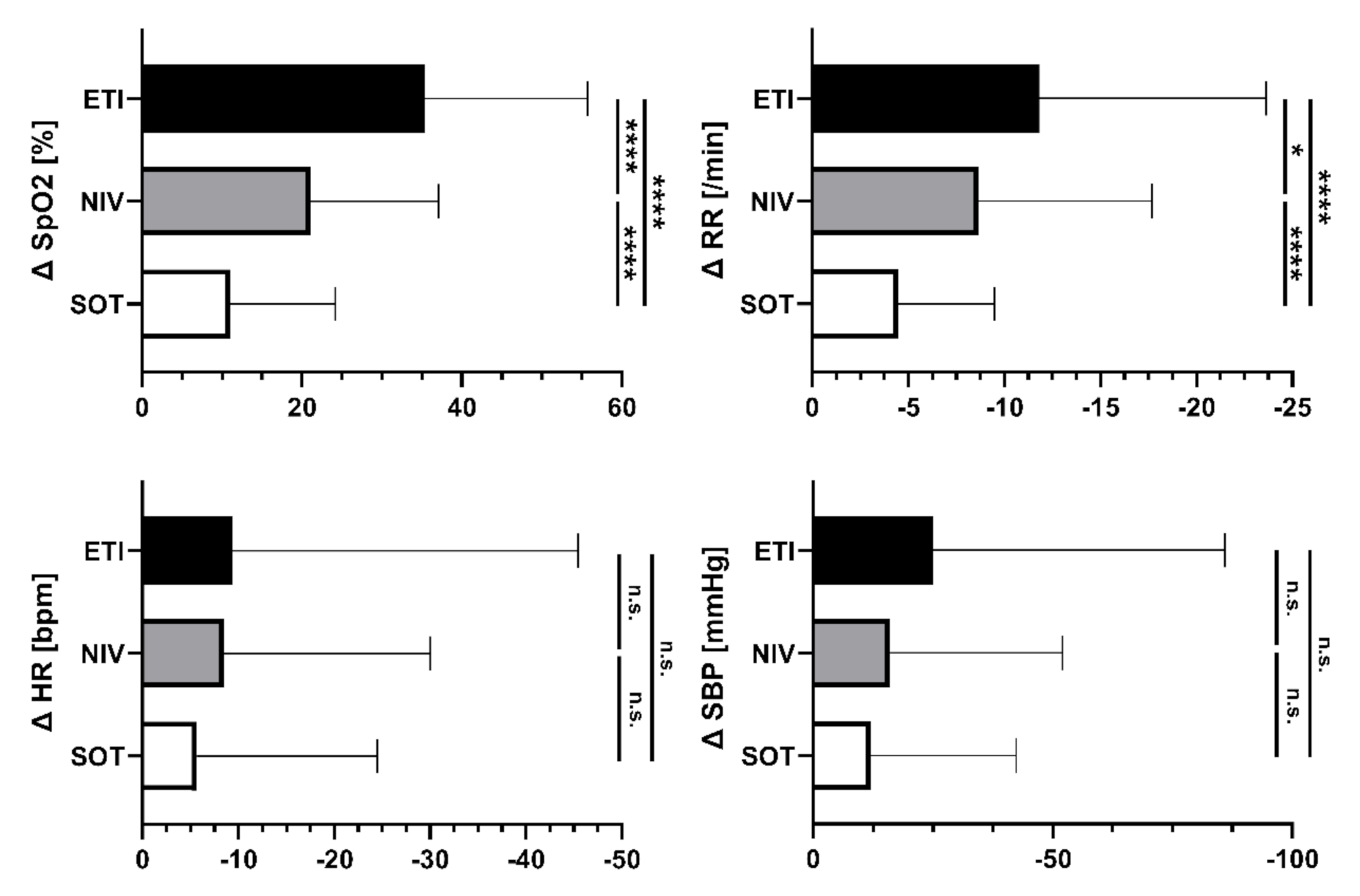
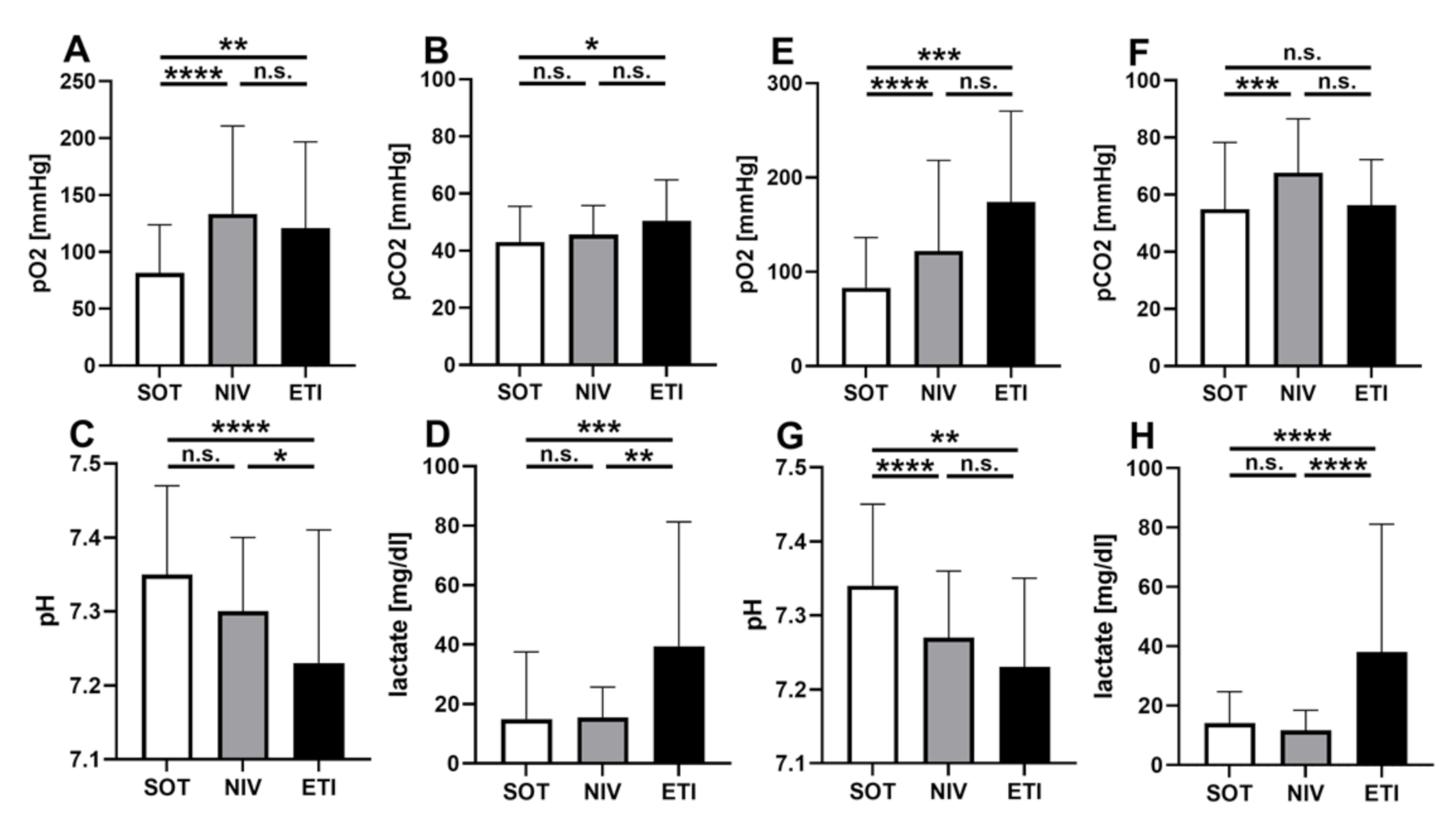
3.2.1. Handover Clinical Data
3.2.2. Clinical Course
3.3. Secondary Outcomes
3.3.1. Hemodynamic Parameters, Vigilance and Sedation
3.3.2. Time Efficiency
3.3.3. Complication Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mas, A.; Masip, J. Noninvasive ventilation in acute respiratory failure. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 837–852. [Google Scholar] [CrossRef]
- Berbenetz, N.; Wang, Y.; Brown, J.; Godfrey, C.; Ahmad, M.; Vital, F.M.; Lambiase, P.; Banerjee, A.; Bakhai, A.; Chong, M. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst. Rev. 2019, 4, CD005351. [Google Scholar] [CrossRef] [PubMed]
- Lemyze, M.; Bury, Q.; Guiot, A.; Jonard, M.; Mohammad, U.; Van Grunderbeeck, N.; Gasan, G.; Thevenin, D.; Mallat, J. Delayed but successful response to noninvasive ventilation in COPD patients with acute hypercapnic respiratory failure. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 1539–1547. [Google Scholar] [CrossRef]
- Hess, D.R. Noninvasive ventilation for acute respiratory failure. Respir. Care 2013, 58, 950–972. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.P.; Zhang, X.C.; Hu, S.L.; Xu, J.-Y.; Xie, J.-F.; Liu, S.-Q.; Liu, L.; Huang, Y.-Z.; Guo, F.-M.; Yang, Y.; et al. Noninvasive Ventilation in Acute Hypoxemic Nonhypercapnic Respiratory Failure: A Systematic Review and Meta-Analysis. Crit. Care Med. 2017, 45, e727–e733. [Google Scholar] [CrossRef] [PubMed]
- Cabrini, L.; Landoni, G.; Oriani, A.; Plumari, V.P.; Nobile, L.; Greco, M.; Pasin, L.; Beretta, L.; Zangrillo, A. Noninvasive ventilation and survival in acute care settings: A comprehensive systematic review and metaanalysis of randomized controlled trials. Crit. Care Med. 2015, 43, 880–888. [Google Scholar] [CrossRef]
- Jayadev, A.; Stone, R.; Steiner, M.C.; McMillan, V.; Roberts, C.M. Time to NIV and mortality in AECOPD hospital admissions: An observational study into real world insights from National COPD Audits. BMJ Open Respir. Res. 2019, 6, e000444. [Google Scholar] [CrossRef]
- Roessler, M.S.; Schmid, D.S.; Michels, P.; Schmid, O.; Jung, K.; Stöber, J.; Neumann, P.; Quintel, M.; Moerer, O. Early out-of-hospital non-invasive ventilation is superior to standard medical treatment in patients with acute respiratory failure: A pilot study. Emerg. Med. J. 2012, 29, 409–414. [Google Scholar] [CrossRef]
- Plaisance, P.; Pirracchio, R.; Berton, C.; Vicaut, E.; Payen, D. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: Physiological and clinical effects. Eur. Heart J. 2007, 28, 2895–2901. [Google Scholar] [CrossRef]
- Schmidbauer, W.; Ahlers, O.; Spies, C.; Dreyer, A.; Mager, G.; Kerner, T. Early prehospital use of non-invasive ventilation improves acute respiratory failure in acute exacerbation of chronic obstructive pulmonary disease. Emerg. Med. J. 2011, 28, 626–627. [Google Scholar] [CrossRef]
- Tsakiridou, E.; Mega, A.-M.; Zakynthinos, E.; Melissopoulou, T.; Stamos, G.; Argyriou, K.; Pangrati, S.; Deliolanis, I.; Floros, I. Pre-intensive care unit intubation and subsequent delayed intensive care unit admission is independently associated with increased occurrence of ventilator-associated pneumonia. Clin. Respir. J. 2018, 12, 2497–2504. [Google Scholar] [CrossRef] [PubMed]
- Fagon, J.Y.; Chastre, J.; Hance, A.J.; Montravers, P.; Novara, A.; Gibert, C. Nosocomial pneumonia in ventilated patients: A cohort study evaluating attributable mortality and hospital stay. Am. J. Med. 1993, 94, 281–288. [Google Scholar] [CrossRef]
- Kollef, M.H. Prevention of hospital-associated pneumonia and ventilator-associated pneumonia. Crit. Care Med. 2004, 32, 1396–1405. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Rosti, V.D.; Travierso, C.; Brambilla, A.M.; Piffer, F.; Petrelli, G.; Minelli, C.; Camisa, D.; Voza, A. A real life evaluation of non invasive ventilation in acute cardiogenic pulmonary edema: A multicenter, perspective, observational study for the ACPE SIMEU study group. BMC Emerg. Med. 2018, 18, 61. [Google Scholar] [CrossRef] [PubMed]
- Hongisto, M.; Lassus, J.; Tarvasmaki, T.; Sionis, A.; Tolppanen, H.; Lindholm, M.G.; Banaszewski, M.; Parissis, J.; Spinar, J.; Silva-Cardoso, J.; et al. Use of noninvasive and invasive mechanical ventilation in cardiogenic shock: A prospective multicenter study. Int. J. Cardiol. 2017, 230, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Gartner, B.A.; Fehlmann, C.; Suppan, L.; Niquille, M.; Rutschmann, O.T.; Sarasin, F. Effect of noninvasive ventilation on intubation risk in prehospital patients with acute cardiogenic pulmonary edema: A retrospective study. Eur. J. Emerg. Med. 2019, 27, 54–58. [Google Scholar] [CrossRef]
- Hensel, M.; Strunden, M.S.; Tank, S.; Gagelmann, N.; Wirtz, S.; Kerner, T. Prehospital non-invasive ventilation in acute respiratory failure is justified even if the distance to hospital is short. Am. J. Emerg. Med. 2019, 37, 651–656. [Google Scholar] [CrossRef]
- Craven, R.A.; Singletary, N.; Bosken, L.; Sewell, E.; Payne, M.; Lipsey, R. Use of bilevel positive airway pressure in out-of-hospital patients. Acad. Emerg. Med. 2000, 7, 1065–1068. [Google Scholar] [CrossRef][Green Version]
- Weitz, G.; Struck, J.; Zonak, A.; Balnus, S.; Perras, B.; Dodt, C. Prehospital noninvasive pressure support ventilation for acute cardiogenic pulmonary edema. Eur. J. Emerg. Med. 2007, 14, 276–279. [Google Scholar] [CrossRef]
- Taylor, D.M.; Bernard, S.A.; Masci, K.; MacBean, C.E.; Kennedy, M.P.; Zalstein, S. Prehospital noninvasive ventilation: A viable treatment option in the urban setting. Prehosp. Emerg. Care 2008, 12, 42–45. [Google Scholar] [CrossRef]
- Lapinsky, S.E. Endotracheal intubation in the ICU. Crit. Care 2015, 19, 258. [Google Scholar] [CrossRef] [PubMed]
- Brochard, L.; Mancebo, J.; Wysocki, M.; Lofaso, F.; Conti, G.; Rauss, A.; Simonneau, G.; Benito, S.; Gasparetto, A.; Lemaire, F.; et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N. Engl. J. Med. 1995, 333, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Conti, G.; Antonelli, M.; Navalesi, P.; Rocco, M.; Bufi, M.; Spadetta, G.; Meduri, G.U. Noninvasive vs. conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: A randomized trial. Intensive Care Med. 2002, 28, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Gil-Perotin, S.; Ramirez, P.; Marti, V.; Sahuquillo, J.M.; Gonzalez, E.; Calleja, I.; Menendez, R.; Bonastre, J. Implications of endotracheal tube biofilm in ventilator-associated pneumonia response: A state of concept. Crit. Care 2012, 16, R93. [Google Scholar] [CrossRef]
- Jaber, S.; Amraoui, J.; Lefrant, J.-Y.; Arich, C.; Cohendy, R.; Landreau, L.; Calvet, Y.; Capdevila, X.; Mahamat, A.; Eledjam, J.-J. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit. Care Med. 2006, 34, 2355–2361. [Google Scholar] [CrossRef]
- Squadrone, E.; Frigerio, P.; Fogliati, C.; Gregoretti, C.; Conti, G.; Antonelli, M.; Costa, R.; Baiardi, P.; Navalesi, P. Noninvasive vs invasive ventilation in COPD patients with severe acute respiratory failure deemed to require ventilatory assistance. Intensive Care Med. 2004, 30, 1303–1310. [Google Scholar] [CrossRef]
- Scala, R.; Heunks, L. Highlights in acute respiratory failure. Eur. Respir. Rev. 2018, 27, 147. [Google Scholar] [CrossRef]
- Duan, J.; Wang, S.; Liu, P.; Han, X.; Tian, Y.; Gao, F.; Zhou, J.; Mou, J.; Qin, Q.; Yu, J.; et al. Early prediction of noninvasive ventilation failure in COPD patients: Derivation, internal validation, and external validation of a simple risk score. Ann. Intensive Care 2019, 9, 108. [Google Scholar] [CrossRef]
- Westhoff, M.; Schönhofer, B.; Neumann, P.; Bickenbach, J.; Barchfeld, T.; Becker, H.; Dubb, R.; Fuchs, H.; Heppner, H.J.; Janssens, U.; et al. [Noninvasive Mechanical Ventilation in Acute Respiratory Failure]. Pneumologie 2015, 69, 719–756. [Google Scholar] [CrossRef]
- Iurilli, C.M.; Brunetti, N.D.; Di Corato, P.R.; Salvemini, G.; Di Biase, M.; Ciccone, M.M.; Procacci, V. Hyperacute Hemodynamic Effects of BiPAP Noninvasive Ventilation in Patients With Acute Heart Failure and Left Ventricular Systolic Dysfunction in Emergency Department. J. Intensive Care Med. 2018, 33, 128–133. [Google Scholar] [CrossRef]
- Sellmann, T.; Conty, C.; Treschan, T.; Kindgen-Milles, D. [Prehospital non-invasive ventilation in Germany: Results of a nationwide survey of ground-based emergency medical services]. Anaesthesist 2014, 63, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, A.; Richard, J.C.; Wysocki, M.; Lepage, E.; Brochard, L. Ventilation SCGoM. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am. J. Respir. Crit. Care Med. 2001, 163, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Schnell, D.; Timsit, J.F.; Darmon, M.; Vesin, A.; Goldgran-Toledano, D.; Dumenil, A.-S.; Garrouste-Orgeas, M.; Adrie, C.; Bouadma, L.; Planquette, B.; et al. Noninvasive mechanical ventilation in acute respiratory failure: Trends in use and outcomes. Intensive Care Med. 2014, 40, 582–591. [Google Scholar] [CrossRef]
- Cammarota, G.; Vaschetto, R.; Azzolina, D.; De Vita, N.; Olivieri, C.; Ronco, C.; Longhini, F.; Bruni, A.; Colombo, D.; Pissaia, C.; et al. Early extubation with immediate non-invasive ventilation versus standard weaning in intubated patients for coronavirus disease 2019: A retrospective multicenter study. Sci. Rep. 2021, 11, 13418. [Google Scholar] [CrossRef] [PubMed]
- Bertaina, M.; Nuñez-Gil, I.J.; Franchin, L.; Rozas, I.F.; Arroyo-Espliguero, R.; Viana-Llamas, M.C.; Romero, R.; Eid, C.M.; Uribarri, A.; Becerra-Muñoz, V.M.; et al. Non-invasive ventilation for SARS-CoV-2 acute respiratory failure: A subanalysis from the HOPE COVID-19 registry. Emerg. Med. J. 2021, 38, 359–365. [Google Scholar] [CrossRef]
- Fischer, M.; Kamp, J.; Riesgo, L.G.-C.; Robertson-Steel, I.; Overton, J.; Ziemann, A.; Krafft, T. Comparing emergency medical service systems—A project of the European Emergency Data (EED) Project. Resuscitation 2011, 82, 285–293. [Google Scholar] [CrossRef]
- Tjelmeland, I.B.M.; Masterson, S.; Herlitz, J.; Wnent, J.; Bossaert, L.; Rosell-Ortiz, F.; Alm-Kruse, K.; Bein, B.; Lilja, G.; Gräsner, J.-T.; et al. Description of Emergency Medical Services, treatment of cardiac arrest patients and cardiac arrest registries in Europe. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 103. [Google Scholar] [CrossRef]

| Total | SOT | NIV | ETI | p-Value | |
|---|---|---|---|---|---|
| Sex (female/male), n (%) | 227/318 (42/58) | 174/244 (42/58) | 41/58(41/59) | 12/16(43/57) | p = 0.99 |
| Age (years) | 75.1 ± 10.7 | 75.5 ± 10.6 | 73.8 ± 11.3 | 74.1 ± 10.0 | p = 0.28 |
| LTOT | 167 (30.6%) | 126 (30.1%) | 37 (37.4%) | 4 (14.3%) | p = 0.06 |
| OSAS | 34 (6.2%) | 25 (6.0%) | 7 (7.1%) | 2 (7.1%) | p = 0.97 |
| Asthma | 18 (3.3%) | 12 (2.9%) | 5 (5.0%) | 1 (3.6%) | p = 0.83 |
| Arterial hypertension | 468 (85.9%) | 357 (85.4%) | 86 (86.9%) | 25 (89.3%) | p = 0.95 |
| s/p myocardial infarction | 141 (25.9%) | 114 (27.3%) | 21 (21.2%) | 6 (21.4%) | p = 0.42 |
| PAOD | 62 (11.4%) | 51 (12.2%) | 8 (8.1%) | 3 (10.7%) | p = 0.51 |
| Renal failure | 134 (24.6%) | 110 (26.3%) | 18 (18.2%) | 6 (21.4%) | p = 0.22 |
| Initial Clinical Data | |||||
|---|---|---|---|---|---|
| Total | SOT | NIV | ETI | p-Value | |
| Respiratory rate (/min) | 24 ± 9 | 23 ± 7 | 29 ± 11 | 28 ± 11 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p = 0.002 NIV vs. ETI: p = 0.56 |
| SpO2 (%) | 81 ± 14 | 84 ± 12 | 76 ± 16 | 62 ± 19 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p < 0.001 NIV vs. ETI: p < 0.001 |
| Heart rate (/min) | 105 ± 28 | 103 ± 28 | 114 ± 23 | 110 ± 43 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p = 0.24 NIV vs. ETI: p = 0.47 |
| SBP (mmHg) | 149 ± 38 | 148 ± 36 | 156 ± 40 | 134 ± 53 | SOT vs. NIV: p = 0.06 SOT vs. ETI: p = 0.08 NIV vs. ETI: p = 0.01 |
| GCS | 15 (15, 15) | 15 (15, 15) | 15 (13, 15) | 12 (8, 14) | SOT vs. NIV: p < 0.001 SOT vs. ETI: p < 0.001 NIV vs. ETI: p = 0.001 |
| Handover clinical data | |||||
| Total | SOT | NIV | ETI | p-Value | |
| Respiratory rate (/min) | 19 ± 6 | 18 ± 6 | 21 ± 6 | 16 ± 3 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p = 0.03 NIV vs. ETI: p < 0.001 |
| SpO2 (%) | 95 ± 6 | 95 ± 7 | 97 ± 3 | 96 ± 5 | SOT vs. NIV: p = 0.01 SOT vs. ETI: p = 0.53 NIV vs. ETI: p = 0.52 |
| Heart rate (/min) | 99 ± 20 | 98 ± 21 | 105 ± 17 | 98 ± 22 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p = 0.93 NIV vs. ETI: p = 0.11 |
| SBP (mmHg) | 135 ± 24 | 135 ± 23 | 140 ± 24 | 112 ± 22 | SOT vs. NIV: p = 0.06 SOT vs. ETI: p < 0.001 NIV vs. ETI: p < 0.001 |
| GCS | 15 (14, 15) | 15 (15, 15) | 14 (12, 15) | 3 (3, 3) | SOT vs. NIV: p < 0.001 SOT vs. ETI: p < 0.001 NIV vs. ETI: p < 0.001 |
| Total | SOT | NIV | ETI | p Value | |
|---|---|---|---|---|---|
| On-scene time (min) | 29 ± 13 | 27 ± 11 | 32 ± 12 | 53 ± 15 | SOT vs. NIV: p < 0.001 SOT vs. ETI: p < 0.001 NIV vs. ETI: p < 0.001 |
| Transportation time (min) | 17 ± 9 | 16 ± 8 | 16 ± 8 | 22 ±13 | SOT vs. NIV: p = 0.82 SOT vs. ETI: p < 0.001 NIV vs. ETI: p = 0.001 |
| CPR (n) | 8 (1.5%) | 5 (1.2%) | 1 (0.9%) | 2 (13.3%) | SOT vs. NIV: p = 0.83 SOT vs. ETI: p = 0.17 NIV vs. ETI: p = 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmitt, F.C.F.; Gruneberg, D.; Schneider, N.R.E.; Fögeling, J.-O.; Leucht, M.; Herth, F.; Preusch, M.R.; Schmidt, W.; Bopp, C.; Bruckner, T.; et al. Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services. J. Clin. Med. 2022, 11, 2504. https://doi.org/10.3390/jcm11092504
Schmitt FCF, Gruneberg D, Schneider NRE, Fögeling J-O, Leucht M, Herth F, Preusch MR, Schmidt W, Bopp C, Bruckner T, et al. Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services. Journal of Clinical Medicine. 2022; 11(9):2504. https://doi.org/10.3390/jcm11092504
Chicago/Turabian StyleSchmitt, Felix C. F., Daniel Gruneberg, Niko R. E. Schneider, Jan-Ole Fögeling, Moritz Leucht, Felix Herth, Michael R. Preusch, Werner Schmidt, Christian Bopp, Thomas Bruckner, and et al. 2022. "Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services" Journal of Clinical Medicine 11, no. 9: 2504. https://doi.org/10.3390/jcm11092504
APA StyleSchmitt, F. C. F., Gruneberg, D., Schneider, N. R. E., Fögeling, J.-O., Leucht, M., Herth, F., Preusch, M. R., Schmidt, W., Bopp, C., Bruckner, T., Weigand, M. A., Hofer, S., & Popp, E. (2022). Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services. Journal of Clinical Medicine, 11(9), 2504. https://doi.org/10.3390/jcm11092504









