Dry Needling in Physical Therapy Treatment of Chronic Neck Pain: Systematic Review
Abstract
:1. Introduction
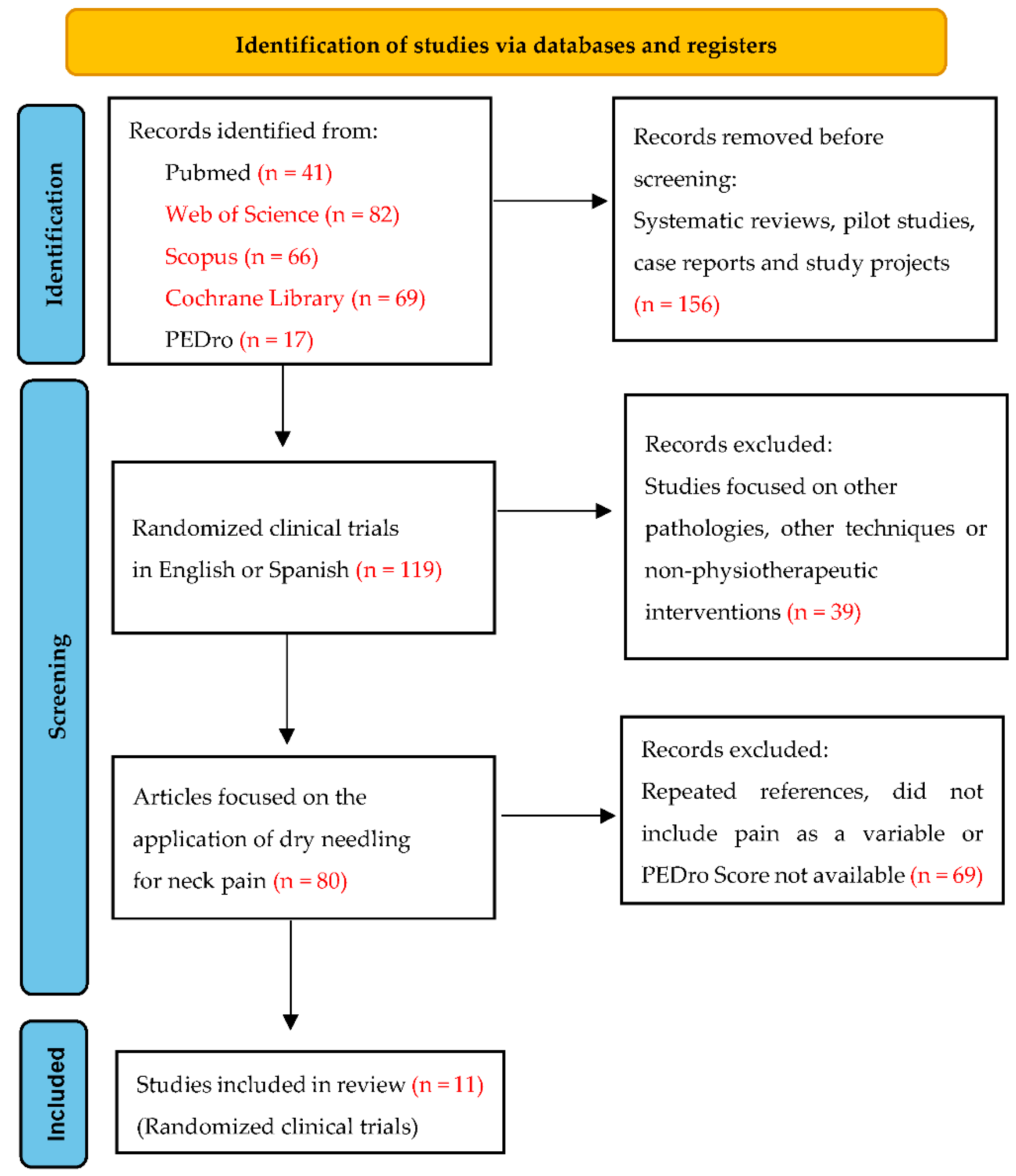
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Author (Year) | PEDro Scale Score Details |
|---|---|
| Irnich et al. (2002) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: No; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: No; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Llamas-Ramos et al. (2014) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Cerezo-Téllez et al. (2016) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: No; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Sobhani et al. (2017) | Eligibility criteria: No; Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: No; Intention-to-treat analysis: No; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Manafnezhad et al. (2019) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: No; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Gallego-Sendarrubias et al. (2020) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: Yes; Blind therapists: No; Blind assessors: No; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: No; Point estimates and variability: Yes. |
| Stieven et al. (2020) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Gattie et al. (2021) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: No; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Leon-Hernandez et al. (2021) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: No; Baseline comparability: Yes; Blind subjects: Yes; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: No; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Stieven et al. (2021) | Eligibility criteria: No; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: Yes; Point estimates and variability: Yes. |
| Valiente-Castrillo et al. (2021) | Eligibility criteria: Yes; Random allocation: Yes; Concealed allocation: Yes; Baseline comparability: Yes; Blind subjects: No; Blind therapists: No; Blind assessors: Yes; Adequate follow-up: Yes; Intention-to-treat analysis: Yes; Between-group comparisons: Yes; Point estimates and variability: Yes. |
Appendix B
| Author (Year) | Country and Clinical Center |
|---|---|
| Irnich et al. (2002) | Germany—Department of Physical Medicine and Rehabilitation and the Interdisciplinary Pain Unit at the University of Munich |
| Llamas-Ramos et al. (2014) | Spain—Alcalá de Henares University |
| Cerezo-Téllez et al. (2016) | Spain—Primary Health Care Centers at Alcalá de Henares Health Area |
| Sobhani et al. (2017) | Iran—Baqiyatallah University of Medical Sciences |
| Manafnezhad et al. (2019) | Iran—Tabriz University of Medical Sciences |
| Gallego-Sendarrubias et al. (2020) | Spain—San Carlos Clinic Hospital |
| Stieven et al. (2020) | Brazil—Physiotherapy private clinic in Porto Alegre |
| Gattie et al. (2021) | United States—Concord Hospital and Franciscan Health physical therapy clinics |
| Leon-Hernandez et al. (2021) | Spain—La Salle University, Madrid |
| Stieven et al. (2021) | Brazil—Physiotherapy private clinic in Porto Alegre |
| Valiente-Castrillo et al. (2021) | Spain—Infanta Sofía University Hospital |
References
- Bier, J.D.; Scholten-Peeters, W.G.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients With Nonspecific Neck Pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Climent, J.M.; Bagó, J.; García-López, A. Patología dolorosa de columna: Cervicalgia, dorsalgia y lumbalgia. FMC Form. Médica Contin. Atención Primaria 2014, 21, 9–35. [Google Scholar] [CrossRef]
- Cohen, S.P. Epidemiology, diagnosis, and treatment of neck pain. In Mayo Clinic Proceedings; Elsevier Ltd.: Amsterdam, The Netherland, 2015; Volume 90, pp. 284–299. [Google Scholar]
- Cohen, S.P.; Hooten, W.M. Advances in the diagnosis and management of neck pain. BMJ 2017, 358, j3221. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, R.; Kurihara, C.; Tsai, H.T.; Silvestri, P.J.; Bennett, M.I.; Pasquina, P.F.; Cohen, S.P. Classification and treatment of chronic Neck pain: A longitudinal cohort study. Reg. Anesth. Pain Med. 2017, 42, 52–61. [Google Scholar] [CrossRef]
- George, S.Z.; Lentz, T.A.; Goertz, C.M. Back and neck pain: In support of routine delivery of non-pharmacologic treatments as a way to improve individual and population health. Transl. Res. 2021, 234, 129–140. [Google Scholar] [CrossRef]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003. [Google Scholar] [CrossRef] [Green Version]
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 783–792. [Google Scholar] [CrossRef]
- Lin, I.H.; Chang, K.H.; Liou, T.H.; Tsou, C.M.; Huang, Y.C. Progressive shoulder-neck exercise on cervical muscle functions in middle-aged and senior patients with chronic neck pain. Eur. J. Phys. Rehabil. Med. 2018, 54, 13–21. [Google Scholar] [CrossRef]
- Ye, S.; Jing, Q.; Wei, C.; Lu, J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: A cross-sectional study. BMJ Open 2017, 7, e014914. [Google Scholar] [CrossRef] [Green Version]
- Kim, R.; Wiest, C.; Clark, K.; Cook, C.; Horn, M. Identifying risk factors for first-episode neck pain: A systematic review. Musculoskelet. Sci. Pract. 2018, 33, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Côté, P.; Yu, H.; Shearer, H.M.; Randhawa, K.; Wong, J.J.; Mior, S.; Ameis, A.; Carroll, L.J.; Nordin, M.; Varatharajan, S.; et al. Non-pharmacological management of persistent headaches associated with neck pain: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. Eur. J. Pain 2019, 23, 1051–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrade Ortega, J.A.; Martínez, A.D.D.; Ruiz, R.A. Validación de una versión Española del Índice de Discapacidad Cervical. Med. Clin. 2008, 130, 85–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riew, K.D. Variations in cervical myotomes and dermatomes. Spine J. 2019, 19, 1143–1145. [Google Scholar] [CrossRef]
- Furukawa, Y.; Miyaji, Y.; Kadoya, A.; Kamiya, H.; Chiba, T.; Hokkoku, K.I.; Hatanaka, Y.; Imafuku, I.; Miyoshi, K.; Sonoo, M. Determining C5, C6 and C7 myotomes through comparative analyses of clinical, MRI and EMG findings in cervical radiculopathy. Clin. Neurophysiol. Pract. 2021, 6, 88–92. [Google Scholar] [CrossRef]
- Hakimi, K.; Spanier, D. Electrodiagnosis of cervical radiculopathy. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 1–12. [Google Scholar] [CrossRef]
- Malfliet, A.; Coppieters, I.; Van Wilgen, P.; Kregel, J.; De Pauw, R.; Dolphens, M.; Ickmans, K. Brain changes associated with cognitive and emotional factors in chronic pain: A systematic review. Eur. J. Pain 2017, 21, 769–786. [Google Scholar] [CrossRef]
- Yavuz, B.G.; Aydinlar, E.I.; Dikmen, P.Y.; Incesu, C. Association between somatic amplification, anxiety, depression, stress and migraine. J. Headache Pain 2013, 14, 53. [Google Scholar] [CrossRef] [Green Version]
- Yalinay Dikmen, P.; Yavuz, B.G.; Aydinlar, E.I. The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Acta Neurol. Belg. 2015, 115, 117–122. [Google Scholar] [CrossRef]
- Peres, M.F.P.; Mercante, J.P.P.; Tobo, P.R.; Kamei, H.; Bigal, M.E. Anxiety and depression symptoms and migraine: A symptom-based approach research. J. Headache Pain 2017, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Seidel, S.; Beisteiner, R.; Manecke, M.; Aslan, T.S.; Wöber, C. Psychiatric comorbidities and photophobia in patients with migraine. J. Headache Pain 2017, 18, 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martimbianco, A.L.C.; Porfírio, G.J.M.; Pacheco, R.L.; Torloni, M.R.; Riera, R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck pain. Cochrane Database Syst. Rev. 2019, 2019, 1465–1858. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, G.S.; Mohanty, P.; Pattnaik, M.; Mishra, C. Effectiveness of mobilization therapy and exercises in mechanical neck pain. Physiother. Theory Pract. 2015, 31, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Mayoral-del-Moral, O.; Torres-Lacomba, M. Fisioterapia invasiva y punción seca. Informe sobre la eficacia de la punción seca en el tratamiento del síndrome de dolor miofascial y sobre su uso en Fisioterapia. Cuest. Fisioter. 2009, 38, 206–217. [Google Scholar]
- Capó-Juan, M.A. Síndrome de dolor miofascial cervical. Revisión narrativa del tratamiento fisioterápico. An. Sist. Sanit. Navar. 2015, 38, 105–116. [Google Scholar] [CrossRef]
- Mayoral-del-Moral, O.; Salvat-Salvat, I. Punción seca de los puntos gatillo miofasciales. In Fisioterapia Invasiva; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, Spain, 2017; pp. 297–312. ISBN 978-84-9113-099-4. [Google Scholar]
- Li, X.; Wang, R.; Xing, X.; Shi, X.; Tian, J.; Zhang, J.; Ge, L.; Zhang, J.; Li, L.; Yang, K. Acupuncture for Myofascial Pain Syndrome: A Network Meta-Analysis of 33 Randomized Controlled Trials. Pain Physician 2017, 20, E883–E902. [Google Scholar]
- Irnich, D.; Behrens, N.; Gleditsch, J.M.; Stör, W.; Schreiber, M.A.; Schöps, P.; Vickers, A.J.; Beyer, A. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: Results of a randomized, double-blind, sham-controlled crossover trial. Pain 2002, 99, 83–89. [Google Scholar] [CrossRef]
- Mayoral-del-Moral, O. Fisioterapia invasiva del síndrome de dolor miofascial. Fisioterapia 2005, 27, 69–75. [Google Scholar] [CrossRef]
- Perreault, T.; Dunning, J.; Butts, R. The local twitch response during trigger point dry needling: Is it necessary for successful outcomes? J. Bodyw. Mov. Ther. 2017, 21, 940–947. [Google Scholar] [CrossRef] [Green Version]
- Dommerholt, J.; Mayoral-del-Moral, O.; Gröbli, C. Trigger Point Dry Needling. J. Man. Manip. Ther. 2006, 14, 70–87. [Google Scholar] [CrossRef]
- Shah, J.P.; Thaker, N. Punción seca segmentaria en el dolor musculoesquelético. In Fisioterapia Invasiva; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, Spain, 2017; pp. 335–356. ISBN 978-84-9113-099-4. [Google Scholar]
- Lim, C.Y.; In, J. Randomization in clinical studies. Korean J. Anesthesiol. 2019, 72, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, W.F.; Uschner, D.; Wang, Y. Randomization: The forgotten component of the randomized clinical trial. Stat. Med. 2019, 38, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llamas-Ramos, R.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Llamas-Ramos, I.; Plaza-Manzano, G.; Ortega-Santiago, R.; Cleland, J.; Fernández-de-las-Peñas, C. Comparison of the short-term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2014, 44, 852–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valiente-Castrillo, P.; Martín-Pintado-Zugasti, A.; Calvo-Lobo, C.; Beltran-Alacreu, H.; Fernández-Carnero, J. Effects of pain neuroscience education and dry needling for the management of patients with chronic myofascial neck pain: A randomized clinical trial. Acupunct. Med. 2021, 39, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Cerezo-Téllez, E.; Torres-Lacomba, M.; Fuentes-Gallardo, I.; Perez-Muñoz, M.; Mayoral-Del-Moral, O.; Lluch-Girbés, E.; Prieto-Valiente, L.; Falla, D. Effectiveness of dry needling for chronic nonspecific neck pain: A randomized, single-blinded, clinical trial. Pain 2016, 157, 1905–1917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sobhani, V.; Shamsoddini, A.; Khatibi-Aghda, A.; Mazloum, V.; Kia, H.H.; Emami Meybodi, M.K. Effectiveness of dry needling, manual therapy, and Kinesio Taping for patients with chronic myofascial neck pain: A single-blind clinical trial. Trauma Mon. 2017, 22. [Google Scholar] [CrossRef]
- Manafnezhad, J.; Salahzadeh, Z.; Salimi, M.; Ghaderi, F.; Ghojazadeh, M. The effects of shock wave and dry needling on active trigger points of upper trapezius muscle in patients with non-specific neck pain: A randomized clinical trial. J. Back Musculoskelet. Rehabil. 2019, 32, 811–818. [Google Scholar] [CrossRef]
- Gallego-Sendarrubias, G.M.; Rodríguez-Sanz, D.; Calvo-Lobo, C.; Martín, J.L. Efficacy of dry needling as an adjunct to manual therapy for patients with chronic mechanical neck pain: A randomised clinical trial. Acupunct. Med. 2020, 38, 244–254. [Google Scholar] [CrossRef]
- Stieven, F.; Ferreira, G.; Wiebusch, M.; de Araújo, F.; da Rosa, L.; Silva, M. Dry Needling Combined With Guideline-Based Physical Therapy Provides No Added Benefit in the Management of Chronic Neck Pain: A Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2020, 50, 447–454. [Google Scholar] [CrossRef]
- Gattie, E.; Cleland, J.A.; Pandya, J.; Snodgrass, S. Dry Needling Adds No Benefit to the Treatment of Neck Pain: A Sham-Controlled Randomized Clinical Trial With 1-Year Follow-up. J. Orthop. Sports Phys. Ther. 2021, 51, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Leon-Hernandez, J.V.; Calvo-Lobo, C.; Martin-Pinado-Zugasti, A.; Fernandez-Carnero, J.; Beltran-Alacreu, H. Effectiveness of Dry Needling with Percutaneous Electrical Nerve Stimulation of High Frequency Versus Low Frequency in Patients with Myofascial Neck Pain. Pain Physician 2021, 24, 135–143. [Google Scholar]
- Stieven, F.; Ferreira, G.; de Araújo, F.; Angellos, R.; Silva, M.; da Rosa, L. Immediate Effects of Dry Needling and Myofascial Release on Local and Widespread Pressure Pain Threshold in Individuals With Active Upper Trapezius Trigger Points: A Randomized Clinical Trial. J. Manipulative Physiol. Ther. 2021, 44, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Abohashrh, M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet. Disord. 2019, 20, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iqbal, Z.A.; Alghadir, A.H.; Anwer, S. Efficacy of Deep Cervical Flexor Muscle Training on Neck Pain, Functional Disability, and Muscle Endurance in School Teachers: A Clinical Trial. Biomed Res. Int. 2021, 2021, 7190808. [Google Scholar] [CrossRef] [PubMed]
- Iversen, V.M.; Vasseljen, O.; Mork, P.J.; Fimland, M.S. Resistance training vs general physical exercise in multidisciplinary rehabilitation of chronic neck pain: A randomized controlled trial. J. Rehabil. Med. 2018, 50, 743–750. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.; Kim, J. Effects of Acupressure on Pain, Flexibility, and Substance P in Middle-Age Women with Chronic Neck Pain. J. Altern. Complement. Med. 2021, 27, 160–167. [Google Scholar] [CrossRef]
- Callejas-Marcos, I.; Torrijos-Bravo, A.; Torres-Chica, B.; Ortiz-Gutiérrez, R.M. Eficacia de la punción seca en la cervicalgia en comparación con otras técnicas de fisioterapia: Una revisión sistemática. Rehabilitación 2019, 53, 189–197. [Google Scholar] [CrossRef]
- Gildir, S.; Tüzün, E.H.; Eroğlu, G.; Eker, L. A randomized trial of trigger point dry needling versus sham needling for chronic tension-type headache. Medicine 2019, 98, e14520. [Google Scholar] [CrossRef]
- Pourahmadi, M.; Mohseni-Bandpei, M.A.; Keshtkar, A.; Koes, B.W.; Fernández-De-Las-Peñas, C.; Dommerholt, J.; Bahramian, M. Effectiveness of dry needling for improving pain and disability in adults with tension-type, cervicogenic, or migraine headaches: Protocol for a systematic review. Chiropr. Man. Therap. 2019, 27, 1–11. [Google Scholar] [CrossRef]
| Author (Year) | Participants and Groups | PEDro Score | Outcomes Measurements | Assessment Time |
|---|---|---|---|---|
| Irnich et al. (2002) | N = 36 | 6/10 | Pain ROM | Immediate post-intervention (15–30 min after treatment) |
| Llamas-Ramos et al. (2014) | N = 94 (47/47) | 8/10 | Pain PPT ROM Disability | 3 post-intervention evaluations: 1 day, 1 week, and 2 weeks after the last treatment session |
| Cerezo-Téllez et al. (2016) | N = 130 (65/65) | 6/10 | Pain PPT ROM Strength NDI | 6 post intervention evaluations: After 2 sessions; after full treatment; 15, 30, 90, and 180 days |
| Sobhani et al. (2017) | N = 39 (13/13/13) | 5/10 | Pain Catastrophism ROM NDI | 1 post-intervention evaluation |
| Manafnezhad et al. (2019) | N = 70 (35/35) | 6/10 | Pain NDI PPT | Evaluation prior to each session and final evaluation 1 week after the last session |
| Gallego- Sendarrubias et al. (2020) | N = 101 (47/54) | 7/10 | Pain PPT ROM NDI | 3 post-intervention evaluations: an evaluation after each session and one month after completion |
| Stieven et al. (2020) | N = 116 (58/58) | 8/10 | Pain NDI Perceived effects Catastrophism Sleep quality Self-efficacy | 3 post-intervention evaluations: at 1, 3, and 6 months |
| Gattie et al. (2021) | N = 77 (37/40) | 7/10 | NDI Pain Perceived effects | 3 post-intervention evaluations: 4 weeks, at 6 months, and 1 year |
| Leon-Hernandez et al. (2021) | N = 40 (20/20) | 7/10 | Pain PPT NDI Kinesiophobia | 2 post-intervention evaluations: 1 week and 1 month |
| Stieven et al. (2021) | N = 44 (15/14/15) | 8/10 | PPT Pain | Immediate post-intervention evaluation and at 10 min |
| Valiente-Castrillo et al. (2021) | N = 60 (21/20/19) | 8/10 | Pain NDI Kinesiophobia Catastrophism Depression Anxiety Fear Pain Pain Attitudes | 3 post-intervention evaluations: at the end of the full treatment, at 1 month, and at 3 months |
| Author (Year) | DN Interventions Protocols | Alternative Treatment | Results |
|---|---|---|---|
| Irnich et al. (2002) | 1 session DN trapezius, splenius, levator scapula, semispinalis, sternocleidomastoid, scalenus, and paravertebral muscles (LTR: Yes) | 1 session: needle acupuncture at distant point/sham laser acupuncture | There are no differences between DN and sham laser acupuncture |
| Llamas-Ramos et al. (2014) | 2 sessions in 2 weeks: DN upper trapezius (LTR: Yes) | 2 sessions in 2 weeks: trigger point manual therapy (compression, stretching, and friction massage) | ↓ Pain ↑ PPT ↑ ROM ↓ Disability |
| Cerezo-Téllez et al. (2016) | 4 sessions in 2 weeks: DN multifidus, splenius, upper trapezius, and levator scapula (LTR: Yes) + passive stretching | 4 sessions in 2 weeks: Passive stretching | ↓ Pain ↑ PPT ↑ ROM ↑ Strength ↓ NDI |
| Sobhani et al. (2017) | 5 sessions in 10 days: bilateral DN upper trapezius and levator scapulae (LTR: not specified) + passive stretching | 5 sessions in 10 days: manual therapy (ischemic trigger point compression)/kinesiotaping on trigger points | ↓ Pain ↓ Catastrophism ↑ ROM ↓ NDI |
| Manafnezhad et al. (2019) | 3 sessions, 1 per week: DN upper trapezius (LTR: Yes) | 3 sessions, 1 per week: Shock waves in upper trapezius | ↓ Pain ↓ NDI ↑ PPT |
| Gallego- Sendarrubias et al. (2020) | 2 sessions with 1 week interval: DN trapezius and levator scapulae (LTR: Yes) + manual therapy | 2 sessions with 1 week interval: sham DN + manual therapy | ↓ Pain ↑ PPT ↑ ROM ↓ NDI |
| Stieven et al. (2020) | 4–6 sessions in 4 weeks: DN upper trapezius, middle trapezius, multifidus, splenius, and levator scapulae (LTR: Yes) + manual therapy (cervical and thoracic mobilization) and exercise | 4–6 sessions in 4 weeks: manual therapy (cervical and thoracic mobilization) and exercise | ↓ Pain |
| Gattie et al. (2021) | 7 sessions in 4 weeks: DN trapezius, levator scapulae, splenius capitis, semispinalis, spinalis capitis, multifidus, and suboccipital muscles (LTR: Yes) + manual therapy + exercise | 7 sessions in 4 weeks: sham DN + manual therapy + exercise | There are no differences between DN and sham DN |
| Leon-Hernandez et al. (2021) | 2 sessions, 1 per week: DN upper trapezius (LTR: Yes) + 15 min of percutaneous needle electrical stimulation (low frequency versus high frequency) | ↓ Pain (There are no differences between DN modalities) | |
| Stieven et al. (2021) | 1 session unilateral DN upper trapezius (LTR: Yes) | 1 session: myofascial release or sham DN | ↑ PPT ↓ Pain |
| Valiente-Castrillo et al. (2021) | 6 sessions in 2 weeks: DN upper trapezius, levator scapulae, splenius, and multifidus (LTR: Yes) + self-stretching + 3 sessions 30′ therapy education for one of the experimental groups | 10 sessions in 2 weeks: 15 min TENS and 15 min Microwave + self-stretching | ↓ Pain ↓ NDI ↓ Kinesiophobia ↓ Catastrophism ↓ Depression ↓ Anxiety ↓ Fear Pain ↑ Pain Attitudes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Huguet, M.; Vinolo-Gil, M.J.; Góngora-Rodríguez, J. Dry Needling in Physical Therapy Treatment of Chronic Neck Pain: Systematic Review. J. Clin. Med. 2022, 11, 2370. https://doi.org/10.3390/jcm11092370
Rodríguez-Huguet M, Vinolo-Gil MJ, Góngora-Rodríguez J. Dry Needling in Physical Therapy Treatment of Chronic Neck Pain: Systematic Review. Journal of Clinical Medicine. 2022; 11(9):2370. https://doi.org/10.3390/jcm11092370
Chicago/Turabian StyleRodríguez-Huguet, Manuel, Maria Jesus Vinolo-Gil, and Jorge Góngora-Rodríguez. 2022. "Dry Needling in Physical Therapy Treatment of Chronic Neck Pain: Systematic Review" Journal of Clinical Medicine 11, no. 9: 2370. https://doi.org/10.3390/jcm11092370
APA StyleRodríguez-Huguet, M., Vinolo-Gil, M. J., & Góngora-Rodríguez, J. (2022). Dry Needling in Physical Therapy Treatment of Chronic Neck Pain: Systematic Review. Journal of Clinical Medicine, 11(9), 2370. https://doi.org/10.3390/jcm11092370








