The Incidence and Risk Factors of Medial and Inferior Orbital Wall Fractures in Korea: A Nationwide Cohort Study
Abstract
:1. Introduction
2. Methods
2.1. Dataset and Study Population
2.2. Definition and Classification of Orbital Wall Fractures
2.3. Sociodemographic Risk Factors of Orbital Wall Fractures
2.4. Statistical Analysis
3. Results
3.1. Incidence of Orbital Wall Fractures
3.2. Types of Orbital Wall Fractures
3.3. Sociodemographic Risk Factors of Orbital Wall Fractures
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Joseph, J.M.; Glavas, I.P. Orbital fractures: A review. Clin. Ophthalmol. 2011, 5, 95–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iftikhar, M.; Canner, J.K.; Hall, L.; Ahmad, M.; Srikumaran, D.; Woreta, F.A. Characteristics of Orbital Floor Fractures in the United States from 2006 to 2017. Ophthalmology 2020, 128, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Noh, H.; Chung, J.K.; Woo, K.I.; Kim, Y.D. Occurrence of ocular injury and orbital fracture in orbital blunt trauma patients at tertiary care center emergency room. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Khojastepour, L.; Moannaei, M.; Eftekharian, H.R.; Khaghaninejad, M.S.; Mahjoori-Ghasrodashti, M.; Tavanafar, S. Prevalence and severity of orbital blowout fractures. Br. J. Oral Maxillofac. Surg. 2020, 58, e93–e97. [Google Scholar] [CrossRef] [PubMed]
- Chi, M.J.; Ku, M.; Shin, K.H.; Baek, S. An analysis of 733 surgically treated blowout fractures. Int. J. Ophthalmol. 2010, 224, 167–175. [Google Scholar] [CrossRef]
- Ko, M.J.; Morris, C.K.; Kim, J.W.; Lad, S.P.; Arrigo, R.T.; Lad, E.M. Orbital fractures: National inpatient trends and complications. Ophthalmic Plast. Reconstr. Surg. 2013, 29, 298–303. [Google Scholar] [CrossRef] [Green Version]
- Park, C.H.; Chung, K.J.; Kim, T.G.; Lee, J.H.; Kim, I.K.; Kim, Y.H. Big Data Statistical Analysis of Facial Fractures in Korea. J. Korean Med. Sci. 2020, 35, e57. [Google Scholar] [CrossRef]
- Lalloo, R.; Lucchesi, L.R.; Bisignano, C.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Roberts, N.L.S.; Sylte, D.O.; et al. Epidemiology of facial fractures: Incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. J. Int. Soc. Child Adolesc. Inj. Prev. 2020, 26, i27–i35. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef]
- Jung, E.H.; Kim, S.J.; Lee, J.Y.; Cho, B.J. The incidence and presumed aetiologies of fourth cranial nerve palsy in Korea: A 10-year nationwide cohort study. Eye 2021, 35, 3012–3019. [Google Scholar] [CrossRef]
- Rim, T.H.; Kim, H.S.; Kwak, J.; Lee, J.S.; Kim, D.W.; Kim, S.S. Association of Corticosteroid Use With Incidence of Central Serous Chorioretinopathy in South Korea. JAMA Ophthalmol. 2018, 136, 1164–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rim, T.H.; Kim, S.S.; Ham, D.I.; Yu, S.Y.; Chung, E.J.; Lee, S.C. Incidence and prevalence of uveitis in South Korea: A nationwide cohort study. Br. J. Ophthalmol. 2018, 102, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.U.; Roh, S.; Kim, Y.E.; Park, J.I.; Jeon, B.; Oh, I.H. Impact of disability status on suicide risks in South Korea: Analysis of National Health Insurance cohort data from 2003 to 2013. Disabil. Health J. 2017, 10, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.; You, S.H.; Sohn, I.A. Analysis of orbital bone fractures: A 12-year study of 391 patients. J. Craniofacial Surg. 2009, 20, 1218–1223. [Google Scholar] [CrossRef]
- Kwon, J.W.; Choi, M.Y.; Bae, J.M. Incidence and seasonality of major ocular trauma: A nationwide population-based study. Sci. Rep. 2020, 10, 10020. [Google Scholar] [CrossRef]
- Shin, J.W.; Lim, J.S.; Yoo, G.; Byeon, J.H. An analysis of pure blowout fractures and associated ocular symptoms. J. Craniofacial Surg. 2013, 24, 703–707. [Google Scholar] [CrossRef]
- Moffatt, J.; Hughes, D.; Bhatti, N.; Holmes, S. Orbital Bone Fractures in a Central London Trauma Center: A Retrospective Study of 582 Patients. J. Craniofacial Surg. 2021; Publish Ahead of Print. [Google Scholar] [CrossRef]
- Lee, W.S.; McNamara, P.; English, J.; Meusemann, R. Ocular trauma associated with falls in older people: A 10-year review from a state trauma service. Injury 2020, 51, 2009–2015. [Google Scholar] [CrossRef]
- de Silva, D.J.; Rose, G.E. Orbital blowout fractures and race. Ophthalmology 2011, 118, 1677–1680. [Google Scholar] [CrossRef]
- Sun, M.T.; Wu, W.; Watanabe, A.; Kakizaki, H.; Chen, B.; Ueda, K.; Katori, N.; Takahashi, Y.; Selva, D. Orbital blowout fracture location in Japanese and Chinese patients. Jpn. J. Ophthalmol. 2015, 59, 65–69. [Google Scholar] [CrossRef]
- Manson, P.N. Pure orbital blowout fracture: New concepts and importance of the medial orbital blowout fracture. Plast. Reconstr. Surg. 1999, 104, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Song, W.K.; Lew, H.; Yoon, J.S.; Oh, M.J.; Lee, S.Y. Role of medial orbital wall morphologic properties in orbital blow-out fractures. Investig. Ophthalmol. Vis. Sci. 2009, 50, 495–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jo, A.; Rizen, V.; Nikolić, V.; Banović, B. The role of orbital wall morphological properties and their supporting structures in the etiology of “blow-out” fractures. Surg. Radiol. Anat. 1989, 11, 241–248. [Google Scholar] [CrossRef]
- Choi, K.E.; Lee, J.; Lee, H.; Chang, M.; Park, M.; Baek, S. The Paradoxical Predominance of Medial Wall Injuries in Blowout Fracture. J. Craniofacial Surg. 2015, 26, e752–e755. [Google Scholar] [CrossRef]
- Yano, H.; Nakano, M.; Anraku, K.; Suzuki, Y.; Ishida, H.; Murakami, R.; Hirano, A. A consecutive case review of orbital blowout fractures and recommendations for comprehensive management. Plast. Reconstr. Surg. 2009, 124, 602–611. [Google Scholar] [CrossRef] [PubMed]
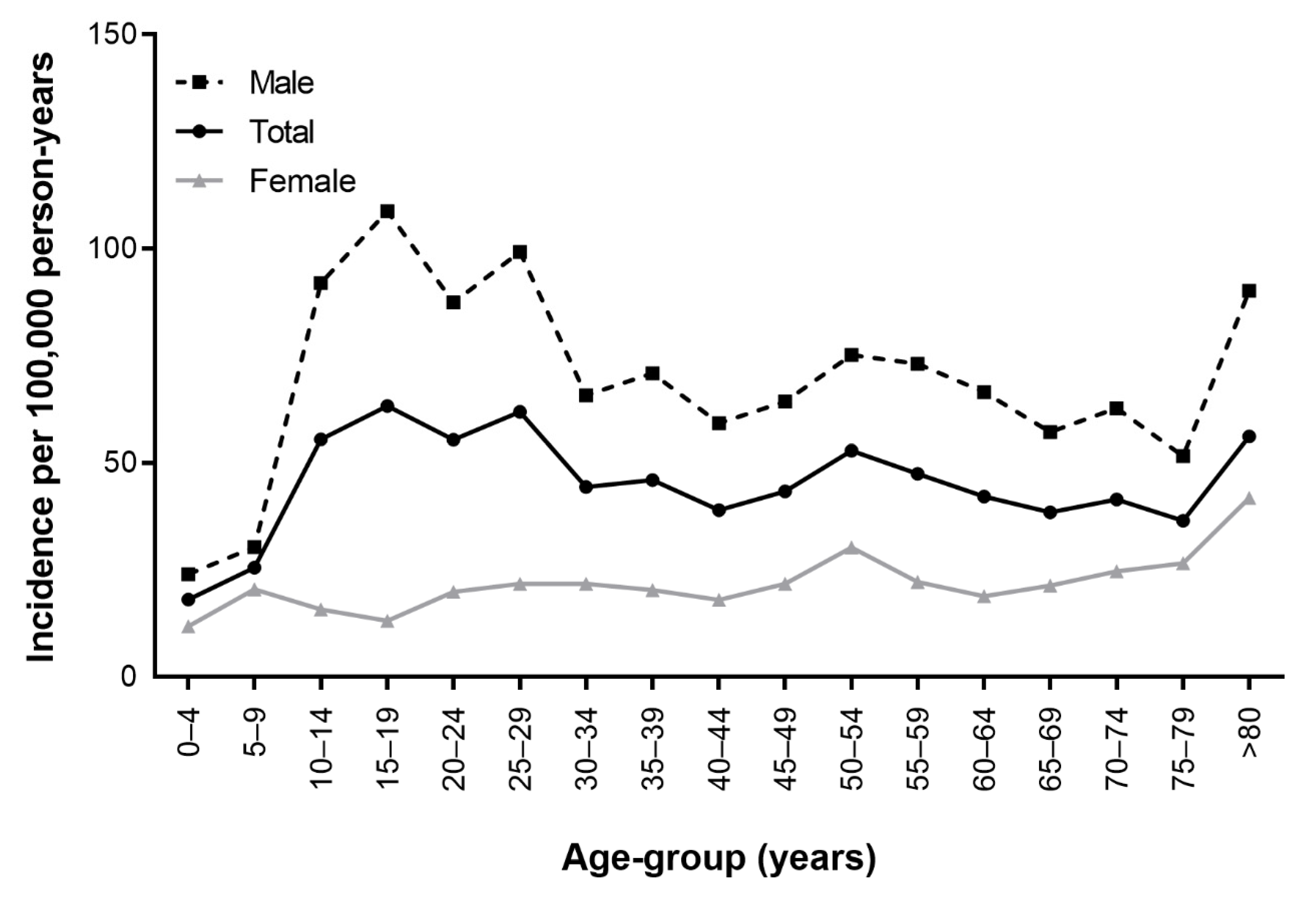
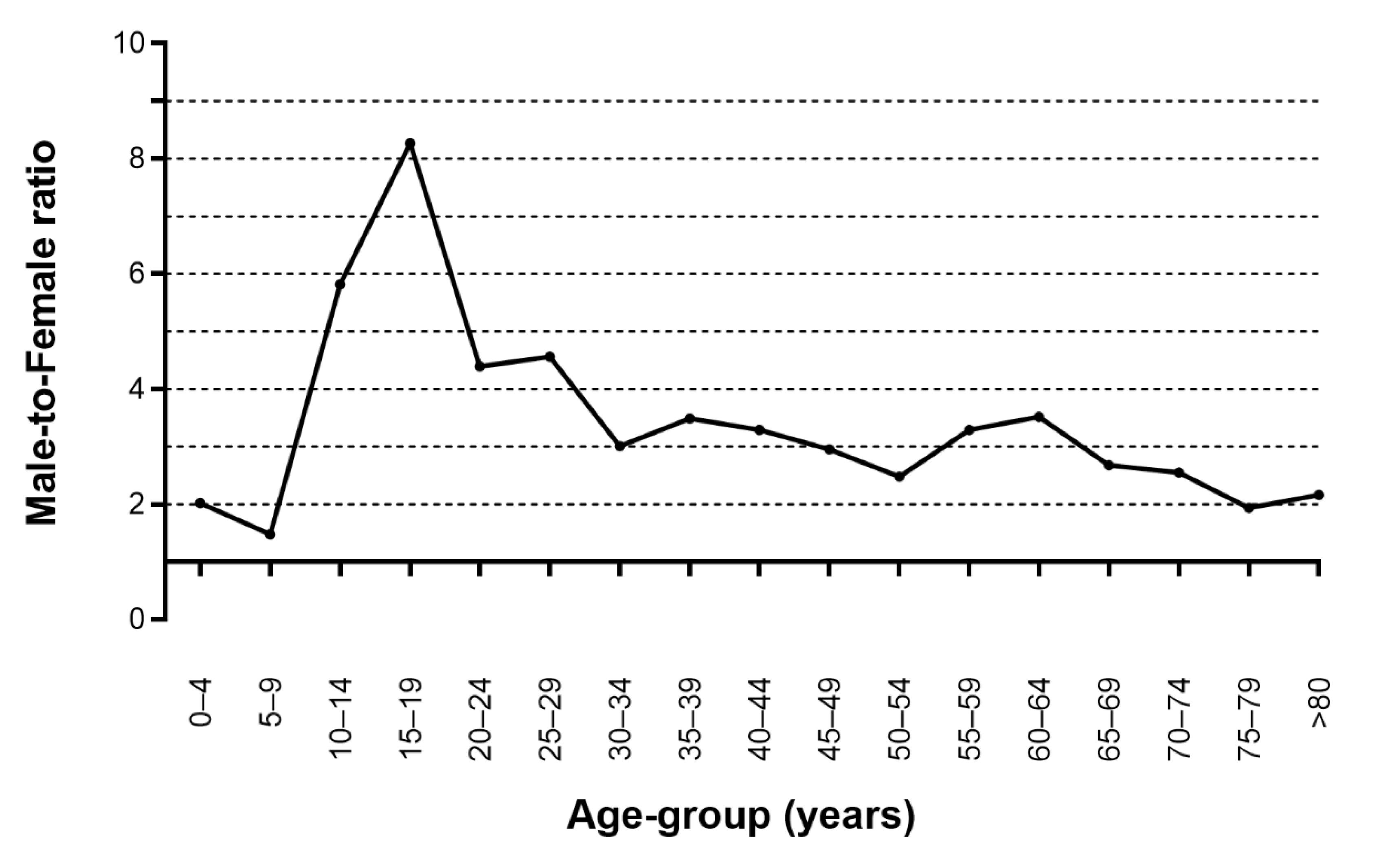
| Age (Years) | Total | Male | Female | MF Ratio | Surgery | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Person Years | N | Incidence | 95% CI | Person Years | N | Incidence | 95% CI | Person Years | N | Incidence | 95% CI | N | ||
| 0–4 | 242,563 | 44 | 18.14 | 13.29, 24.04 | 124,724 | 30 | 24.05 | 16.44, 33.72 | 117,839 | 14 | 11.88 | 6.69, 19.23 | 2.02 | 2 |
| 5–9 | 242,428 | 62 | 25.57 | 19.73, 32.48 | 125,175 | 38 | 30.36 | 21.70, 41.06 | 117,253 | 24 | 20.47 | 13.33, 29.78 | 1.48 | 8 |
| 10–14 | 290,061 | 161 | 55.51 | 47.37, 64.53 | 151,045 | 139 | 92.03 | 77.56, 108.18 | 139,016 | 22 | 15.83 | 10.10, 23.39 | 5.82 | 31 |
| 15–19 | 351,996 | 223 | 63.35 | 55.40, 72.04 | 184,809 | 201 | 108.76 | 94.41, 124.50 | 167,186 | 22 | 13.16 | 8.40, 19.45 | 8.27 | 74 |
| 20–24 | 349,817 | 194 | 55.46 | 48.02, 63.63 | 184,148 | 161 | 87.43 | 74.61, 101.64 | 165,669 | 33 | 19.92 | 13.87, 27.51 | 4.39 | 79 |
| 25–29 | 334,257 | 207 | 61.93 | 53.87, 70.75 | 173,322 | 172 | 99.24 | 85.14, 114.82 | 160,935 | 35 | 21.75 | 15.32, 29.77 | 4.56 | 77 |
| 30–34 | 403,632 | 179 | 44.35 | 38.16, 51.16 | 206,657 | 136 | 65.81 | 55.36, 77.50 | 196,976 | 43 | 21.83 | 15.94, 29.02 | 3.01 | 67 |
| 35–39 | 408,812 | 188 | 45.99 | 39.72, 52.88 | 207,303 | 147 | 70.91 | 60.06, 83.00 | 201,509 | 41 | 20.35 | 14.74, 27.23 | 3.49 | 72 |
| 40–44 | 461,802 | 180 | 38.98 | 33.56, 44.95 | 234,447 | 139 | 59.29 | 49.97, 69.70 | 227,355 | 41 | 18.03 | 13.06, 24.13 | 3.29 | 56 |
| 45–49 | 435,864 | 189 | 43.36 | 37.47, 49.84 | 220,613 | 142 | 64.37 | 54.35, 75.54 | 215,252 | 47 | 21.83 | 16.17, 28.69 | 2.95 | 47 |
| 50–54 | 438,524 | 232 | 52.9 | 46.39, 60.01 | 220,699 | 166 | 75.22 | 64.35, 87.24 | 217,826 | 66 | 30.3 | 23.57, 38.21 | 2.48 | 54 |
| 55–59 | 366,242 | 174 | 47.51 | 40.80, 54.92 | 181,771 | 133 | 73.17 | 61.43, 86.32 | 184,471 | 41 | 22.23 | 16.10, 29.74 | 3.29 | 34 |
| 60–64 | 258,453 | 109 | 42.17 | 34.74, 50.59 | 126,238 | 84 | 66.54 | 53.31, 81.80 | 132,215 | 25 | 18.91 | 12.43, 27.32 | 3.52 | 24 |
| 65–69 | 205,457 | 79 | 38.45 | 30.58, 47.56 | 97,855 | 56 | 57.23 | 43.52, 73.55 | 107,602 | 23 | 21.38 | 13.79, 31.34 | 2.68 | 10 |
| 70–74 | 180,909 | 75 | 41.46 | 32.77, 51.56 | 79,602 | 50 | 62.81 | 46.97, 81.87 | 101,307 | 25 | 24.68 | 16.22, 35.65 | 2.55 | 9 |
| 75–79 | 131,376 | 48 | 36.54 | 27.15, 47.87 | 52,304 | 27 | 51.62 | 34.52, 73.61 | 79,072 | 21 | 26.56 | 16.76, 39.59 | 1.94 | 2 |
| >80 | 126,253 | 71 | 56.24 | 44.15, 70.35 | 37,710 | 34 | 90.16 | 63.15, 123.95 | 88,543 | 37 | 41.79 | 29.73, 56.74 | 2.16 | 2 |
| Overall | 5,228,446 | 2415 | 46.19 | 44.37, 48.06 | 2,608,422 | 1855 | 71.12 | 67.93, 74.40 | 2,620,026 | 560 | 21.37 | 19.65, 23.19 | 3.33 | 648 |
| Year | Incidence | |||
|---|---|---|---|---|
| Person Years | No. | Incidence | 95% CI | |
| 2011 | 1,038,607 | 518 | 49.87 | 45.70, 54.29 |
| 2012 | 1,045,182 | 493 | 47.17 | 43.13, 51.46 |
| 2013 | 1,045,101 | 492 | 47.08 | 43.04, 51.36 |
| 2014 | 1,048,204 | 442 | 42.17 | 38.36, 46.22 |
| 2015 | 1,051,352 | 470 | 44.70 | 40.78, 48.87 |
| Fracture Sites | N (%) |
|---|---|
| Inferior orbital wall | 1435 (59.4) |
| Medial orbital wall | 572 (23.7) |
| Le Fort II or III | 8 (0.3) |
| Naso-orbito-ethmoid | 37 (1.5) |
| Combination | 363 (15.0) |
| Total | 2415 |
| HR | 95% CI | p-Value | |
|---|---|---|---|
| Age Group(Year) | |||
| 0–9 | 0.52 | 0.42, 0.65 | <0.001 |
| 10–19 | 1.43 | 1.24, 1.65 | <0.001 |
| 20–29 | 1.37 | 1.19, 1.58 | <0.001 |
| 30–39 | 1.1 | 0.95, 1.27 | 0.198 |
| 40–49 | 1 (ref) | ||
| 50–59 | 1.22 | 1.06, 1.41 | 0.005 |
| 60–69 | 1.01 | 0.85, 1.21 | 0.9 |
| 70–79 | 1.06 | 0.86, 1.30 | 0.596 |
| >80 | 1.75 | 1.35, 2.26 | <0.001 |
| Sex | |||
| Male | 3.38 | 3.07, 3.72 | <0.001 |
| Female | 1 (ref) | ||
| Residence | |||
| Province | 1.17 | 1.05, 1.30 | 0.005 |
| Metropolitan city | 1.1 | 0.97, 1.24 | 0.138 |
| Seoul | 1 (ref) | ||
| Income | |||
| Low | 1.31 | 1.18, 1.45 | <0.001 |
| Middle | 1.15 | 1.05, 1.26 | 0.004 |
| High | 1 (ref) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, E.H.; Lee, M.J.; Cho, B.-J. The Incidence and Risk Factors of Medial and Inferior Orbital Wall Fractures in Korea: A Nationwide Cohort Study. J. Clin. Med. 2022, 11, 2306. https://doi.org/10.3390/jcm11092306
Jung EH, Lee MJ, Cho B-J. The Incidence and Risk Factors of Medial and Inferior Orbital Wall Fractures in Korea: A Nationwide Cohort Study. Journal of Clinical Medicine. 2022; 11(9):2306. https://doi.org/10.3390/jcm11092306
Chicago/Turabian StyleJung, Eun Hye, Min Joung Lee, and Bum-Joo Cho. 2022. "The Incidence and Risk Factors of Medial and Inferior Orbital Wall Fractures in Korea: A Nationwide Cohort Study" Journal of Clinical Medicine 11, no. 9: 2306. https://doi.org/10.3390/jcm11092306
APA StyleJung, E. H., Lee, M. J., & Cho, B.-J. (2022). The Incidence and Risk Factors of Medial and Inferior Orbital Wall Fractures in Korea: A Nationwide Cohort Study. Journal of Clinical Medicine, 11(9), 2306. https://doi.org/10.3390/jcm11092306






