Patient Visits and Prescribing Patterns Associated with Rosacea in Korea: A Real-World Retrospective Study Based on Electronic Medical Records
Abstract
:1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population and Study Design
2.3. Statistical Analysis
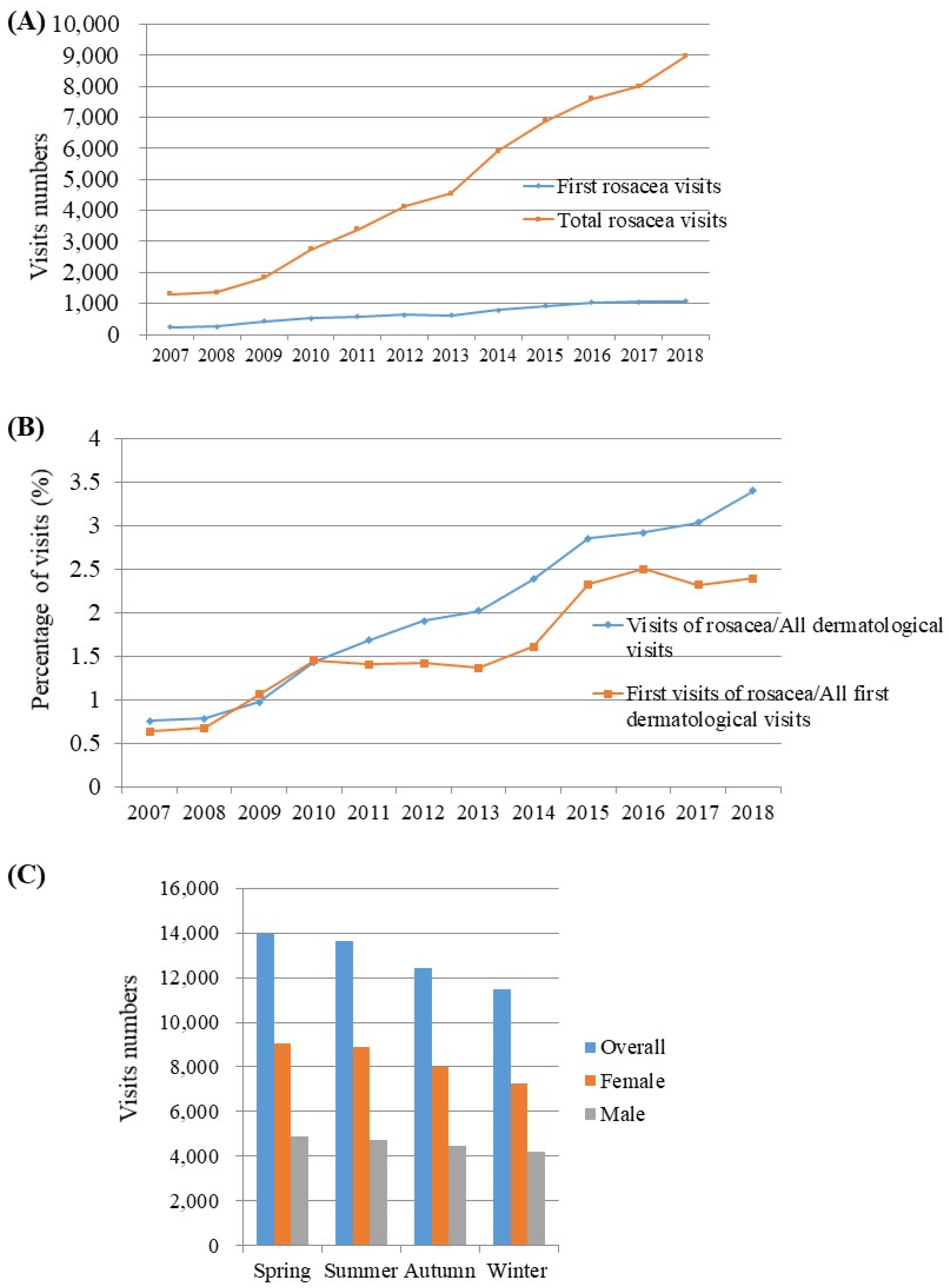
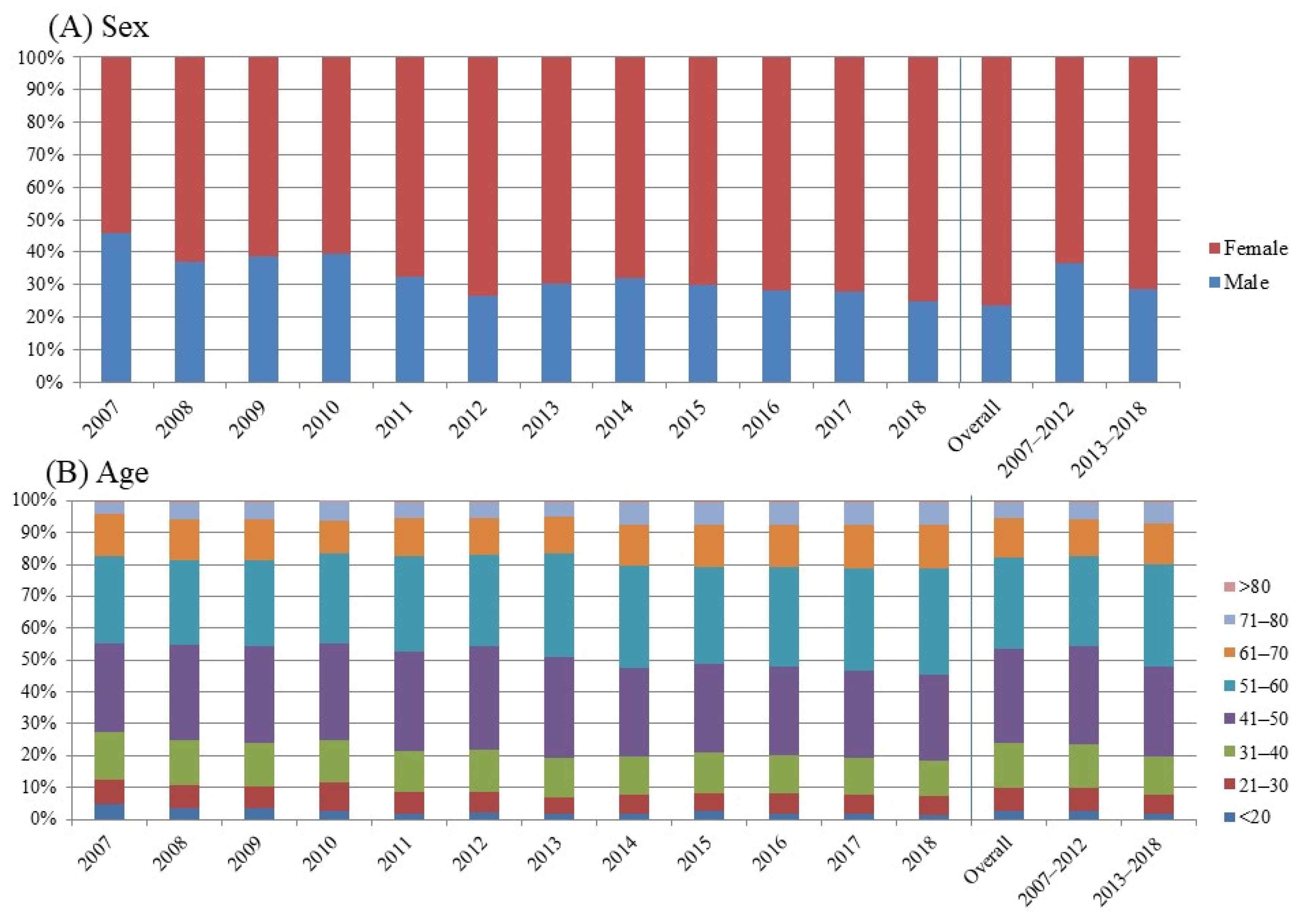
3. Results
3.1. Patients’ Demographic Characteristics
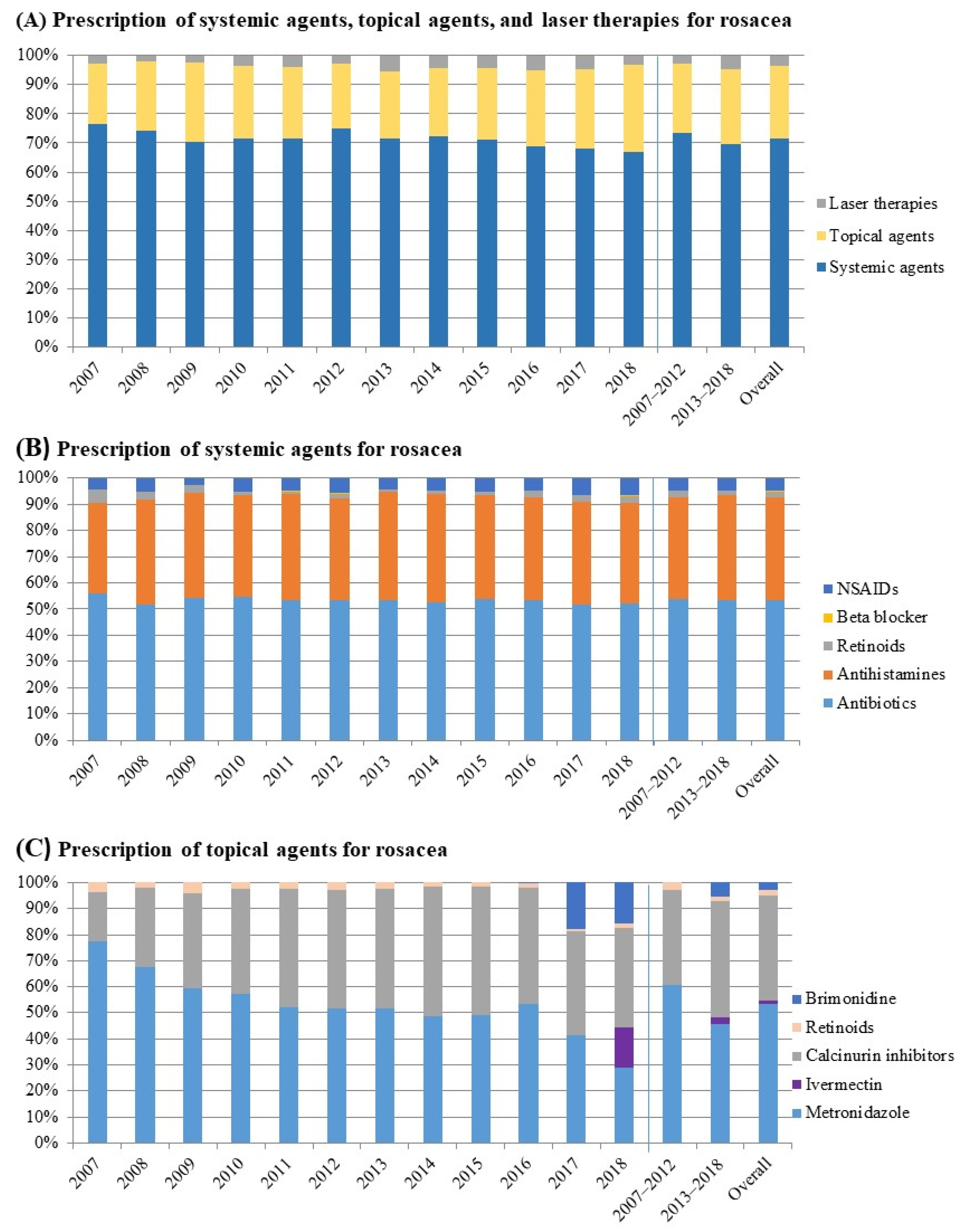
3.2. Factors That Affect Dermatologists’ Prescriptions for Rosacea
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Gallo, R.L.; Granstein, R.D.; Kang, S.; Mannis, M.; Steinhoff, M.; Tan, J.; Thiboutot, D. Standard classification and pathophysiology of rosacea: The 2017 update by the National Rosacea Society Expert Committee. J. Am. Acad. Dermatol. 2018, 78, 148–155. [Google Scholar] [CrossRef]
- Gether, L.; Overgaard, L.K.; Egeberg, A.; Thyssen, J.P. Incidence and prevalence of rosacea: A systematic review and meta-analysis. Br. J. Dermatol. 2018, 179, 282–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexis, A.F.; Callender, V.D.; Baldwin, H.E.; Desai, S.R.; Rendon, M.I.; Taylor, S.C. Global epidemiology and clinical spectrum of rosacea, highlighting skin of color: Review and clinical practice experience. J. Am. Acad. Dermatol. 2019, 80, 1722–1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dlova, N.C.; Mosam, A. Rosacea in black South Africans with skin phototypes V and VI. Clin. Exp. Dermatol. 2017, 42, 670–673. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Lee, Y.J.; Lee, M.H.; Won, C.H.; Chang, S.E.; Choi, J.H.; Lee, M.W. Prognosis of 234 rosacea patients according to clinical subtype: The significance of central facial erythema in the prognosis of rosacea. J. Dermatol. 2016, 43, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Cheong, K.W.; Yew, Y.W.; Lai, Y.C.; Chan, R. Clinical characteristics and management of patients with rosacea in a tertiary dermatology center in Singapore from 2009 to 2013. Int. J. Dermatol. 2018, 57, 541–546. [Google Scholar] [CrossRef]
- Schaller, M.; Almeida, L.; Bewley, A.; Cribier, B.; Del Rosso, J.; Dlova, N.; Gallo, R.; Granstein, R.; Kautz, G.; Mannis, M.; et al. Recommendations for rosacea diagnosis, classification and management: Update from the global ROS acea CO nsensus 2019 panel. Br. J. Dermatol. 2020, 182, 1269–1276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Rosso, J.Q.; Tanghetti, E.; Webster, G.; Gold, L.S.; Thiboutot, D.; Gallo, R.L. Update on the Management of Rosacea from the American Acne & Rosacea Society (AARS). J. Clin. Aesthetic Dermatol. 2019, 12, 17. [Google Scholar]
- Rosamilla, L. Rosacea treatment schema: An update. Cutis 2017, 100, 11–13. [Google Scholar]
- Spoendlin, J.; Voegel, J.J.; Jick, S.; Meier, C.R. A study on the epidemiology of rosacea in the U.K. Br. J. Dermatol. 2012, 167, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Berg, M. Rosacea: Current state of epidemiology. J. Am. Acad. Dermatol. 2013, 69, S27–S35. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Schöfer, H.; Araviiskaia, E.; Audibert, F.; Kerrouche, N.; Berg, M.; group, R.s. Prevalence of rosacea in the general population of Germany and Russia–The RISE study. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 428–434. [Google Scholar] [CrossRef]
- Augustin, M.; Herberger, K.; Hintzen, S.; Heigel, H.; Franzke, N.; Schäfer, I. Prevalence of skin lesions and need for treatment in a cohort of 90,880 workers. Br. J. Dermatol. 2011, 165, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Hancox, J.G.; Sheridan, S.C.; Feldman, S.R.; Fleischer, A.B., Jr. Seasonal variation of dermatologic disease in the USA: A study of office visits from 1990 to 1998. Int. J. Dermatol. 2004, 43, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Weissenbacher, S.; Merkl, J.; Hildebrandt, B.; Wollenberg, A.; Braeutigam, M.; Ring, J.; Hofmann, H. Pimecrolimus cream 1% for papulopustular rosacea: A randomized vehicle-controlled double-blind trial. Br. J. Dermatol. 2007, 156, 728–732. [Google Scholar] [CrossRef] [PubMed]
- Koca, R.; Altinyazar, H.C.; Ankarali, H.; Muhtar, Ş.; Tekin, N.S.; Çinar, S. A comparison of metronidazole 1% cream and pimecrolimus 1% cream in the treatment of patients with papulopustular rosacea: A randomized open-label clinical trial. Clin. Exp. Dermatol. 2010, 35, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Schaller, M.; Almeida, L.; Bewley, A.; Cribier, B.; Dlova, N.; Kautz, G.; Mannis, M.; Oon, H.; Rajagopalan, M.; Steinhoff, M. Rosacea treatment update: Recommendations from the global ROS acea CO nsensus (ROSCO) panel. Br. J. Dermatol. 2017, 176, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Asai, Y.; Tan, J.; Baibergenova, A.; Barankin, B.; Cochrane, C.L.; Humphrey, S.; Lynde, C.W.; Marcoux, D.; Poulin, Y.; Rivers, J.K.; et al. Canadian Clinical Practice Guidelines for Rosacea. J. Cutan. Med. Surg. 2016, 20, 432–445. [Google Scholar] [CrossRef] [PubMed]
- Del Rosso, J.Q.; Thiboutot, D.; Gallo, R.; Webster, G.; Tanghetti, E.; Eichenfield, L.F.; Stein-Gold, L.; Berson, D.; Zaenglein, A. Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 5: A guide on the management of rosacea. Cutis 2014, 93, 134–138. [Google Scholar] [PubMed]
- Hampton, P.; Berth-Jones, J.; Duarte Williamson, C.E.; Hay, R.; Leslie, T.A.; Porter, I.; Rauz, S.; Seukeran, D.; Winn, R.; Hashme, M.; et al. British Association of Dermatologists guidelines for the management of people with rosacea 2021*. Br. J. Dermatol. 2021, 185, 725–735. [Google Scholar] [CrossRef] [PubMed]
- Del Rosso, J.Q. Systemic therapy for rosacea: Focus on oral antibiotic therapy and safety. Cutis 2000, 66, 7–13. [Google Scholar] [PubMed]
- Deng, Z.; Xu, S.; Peng, Q.; Sha, K.; Xiao, W.; Liu, T.; Zhang, Y.; Wang, B.; Xie, H.; Chen, M. Aspirin alleviates skin inflammation and angiogenesis in rosacea. Int. Immunopharmacol. 2021, 95, 107558. [Google Scholar] [CrossRef] [PubMed]
- Bogetti, P.; Boltri, M.; Spagnoli, G.; Dolcet, M. Surgical Treatment of Rhinophyma: A Comparison of Techniques. Aesthetic Plast. Surg. 2002, 26, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Nam, J.H.; Yun, Y.; Kim, H.S.; Kim, H.N.; Jung, H.J.; Chang, Y.; Ryu, S.; Shin, H.; Kim, H.L.; Kim, W.S. Rosacea and its association with enteral microbiota in Korean females. Exp. Dermatol. 2018, 27, 37–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.-J.; Lee, W.-H.; Ho, H.J.; Tseng, C.-H.; Wu, C.-Y. An altered fecal microbial profiling in rosacea patients compared to matched controls. J. Formos. Med Assoc. 2021, 120, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Manzhalii, E.; Hornuss, D.; Stremmel, W. Intestinal-borne dermatoses significantly improved by oral application of Escherichia coli Nissle 1917. World J. Gastroenterol. 2016, 22, 5415–5421. [Google Scholar] [CrossRef]
- Fortuna, M.C.; Garelli, V.; Pranteda, G.; Romaniello, F.; Cardone, M.; Carlesimo, M.; Rossi, A. A case of Scalp Rosacea treated with low dose doxycycline and probiotic therapy and literature review on therapeutic options. Dermatol. Ther. 2016, 29, 249–251. [Google Scholar] [CrossRef]

| Variables | Rosacea Visits, n (%) |
|---|---|
| Age, year | |
| ≤20 | 1117 (1.97) |
| 21–30 | 3584 (6.33) |
| 31–40 | 6946 (12.26) |
| 41–50 | 16,301 (28.77) |
| 51–60 | 17,614 (31.09) |
| 61–70 | 7250 (12.80) |
| 71–80 | 3476 (6.14) |
| >80 | 363 (0.64) |
| Sex | |
| Female | 39,697 (70.07) |
| Male | 16,954 (29.93) |
| Setting | |
| Metropolitan | 25,000 (44.12) |
| Urban | 31,651 (55.88) |
| Variables | Sex (Case/Reference: Female/Male) | Age (years) (Case/Reference: ≥50/<50) | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Topical agents | ||||||
| Metronidazole | 0.86 | 0.82–0.91 | <0.001 * | 1.13 | 1.25–1.38 | <0.001 * |
| Ivermectin | 1.14 | 1.02–1.31 | 0.02 * | 1.10 | 0.98–1.24 | 0.09 |
| CNIs | 0.96 | 0.91–1.01 | 0.15 | 1.17 | 1.11–1.23 | <0.001 * |
| Retinoid | 0.81 | 0.64–1.03 | 0.09 | 0.60 | 0.47–0.77 | <0.001 * |
| Brimonidine | 1.39 | 1.22–1.58 | <0.001 * | 1.22 | 1.08–1.37 | 0.001 * |
| Systemic agents | ||||||
| Antibiotics | 1.22 | 1.21–1.27 | <0.001 * | 0.84 | 0.81–0.88 | <0.001 * |
| Antihistamine | 1.23 | 1.18–1.28 | <0.001 * | 1.08 | 1.04–1.12 | <0.001 * |
| Retinoids | 0.48 | 0.42–0.56 | <0.001 * | 0.40 | 0.34–0.47 | <0.001 * |
| Beta blockers | 2.57 | 1.81–3.65 | <0.001 * | 1.05 | 0.80–1.37 | 0.80 |
| NSAIDs | 1.39 | 1.27–1.51 | <0.001 * | 1.13 | 1.04–1.22 | 0.001 * |
| Skin care products and laser therapy | ||||||
| Moisturizer | 1.61 | 1.51–1.72 | <0.001 * | 0.95 | 0.89–1.00 | 0.07 |
| Sunscreen | 2.20 | 1.79–2.70 | <0.001 * | 0.96 | 0.82–1.14 | 0.71 |
| Cleanser | 1.46 | 1.27–1.68 | <0.001 * | 0.60 | 0.53–0.69 | <0.001 * |
| Laser | 1.00 | 0.92–1.08 | 0.99 | 0.71 | 0.66–0.77 | <0.001 * |
| Adjunctives | ||||||
| γ-linoleic acid | 1.11 | 0.94–1.30 | 0.19 | 0.78 | 0.67–0.91 | 0.002 * |
| Probiotics | 1.31 | 1.22–1.41 | <0.001 * | 0.96 | 0.90–1.03 | 0.34 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woo, Y.R.; Ju, H.J.; Bae, J.M.; Cho, M.; Cho, S.H.; Kim, H.S. Patient Visits and Prescribing Patterns Associated with Rosacea in Korea: A Real-World Retrospective Study Based on Electronic Medical Records. J. Clin. Med. 2022, 11, 1671. https://doi.org/10.3390/jcm11061671
Woo YR, Ju HJ, Bae JM, Cho M, Cho SH, Kim HS. Patient Visits and Prescribing Patterns Associated with Rosacea in Korea: A Real-World Retrospective Study Based on Electronic Medical Records. Journal of Clinical Medicine. 2022; 11(6):1671. https://doi.org/10.3390/jcm11061671
Chicago/Turabian StyleWoo, Yu Ri, Hyun Jeong Ju, Jung Min Bae, Minah Cho, Sang Hyun Cho, and Hei Sung Kim. 2022. "Patient Visits and Prescribing Patterns Associated with Rosacea in Korea: A Real-World Retrospective Study Based on Electronic Medical Records" Journal of Clinical Medicine 11, no. 6: 1671. https://doi.org/10.3390/jcm11061671
APA StyleWoo, Y. R., Ju, H. J., Bae, J. M., Cho, M., Cho, S. H., & Kim, H. S. (2022). Patient Visits and Prescribing Patterns Associated with Rosacea in Korea: A Real-World Retrospective Study Based on Electronic Medical Records. Journal of Clinical Medicine, 11(6), 1671. https://doi.org/10.3390/jcm11061671







