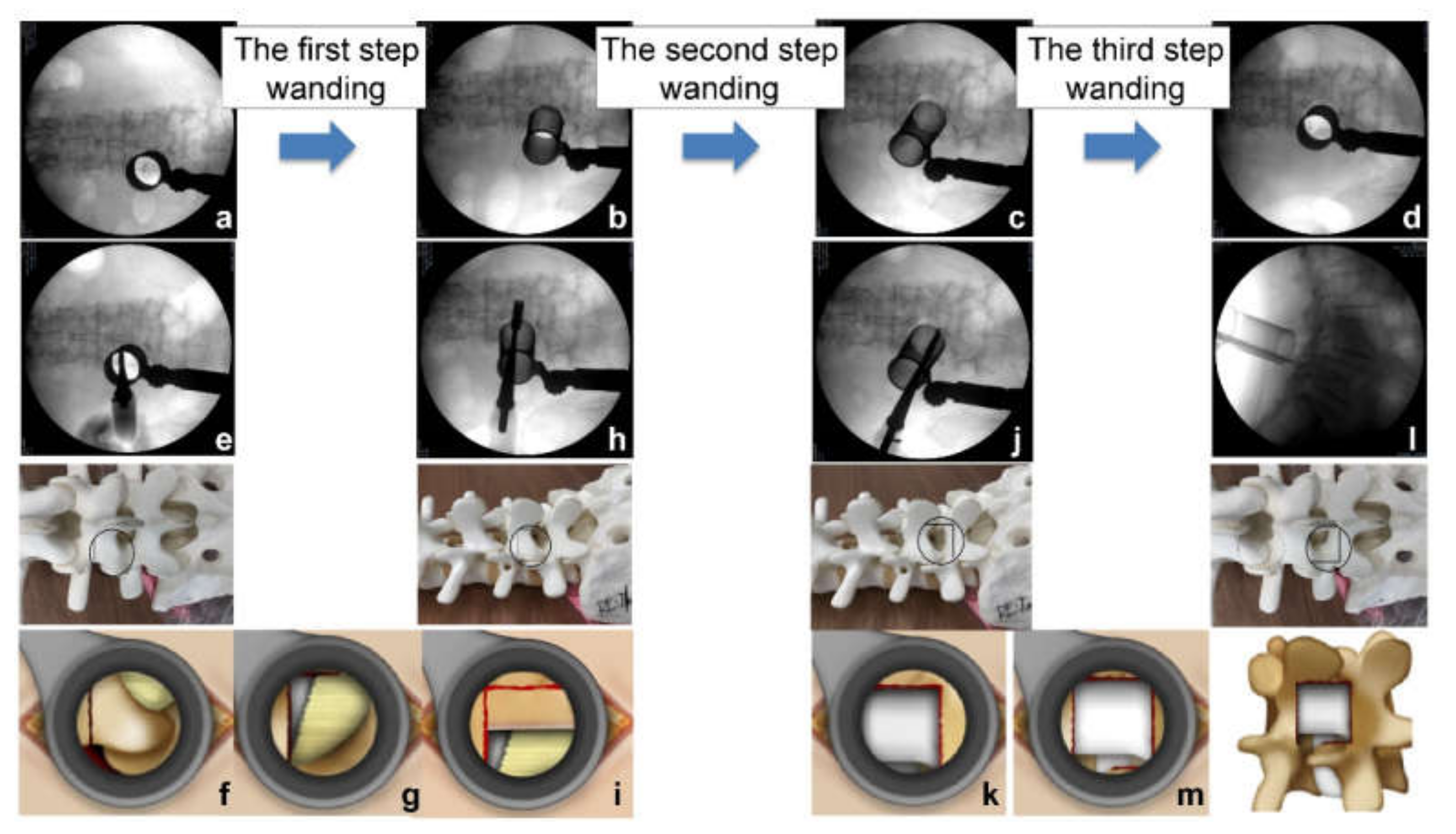
Posterior Oblique Square Decompression with a Three-Step Wanding Technique in Tubular Minimally Invasive Transforaminal Lumbar Interbody Fusion: Technical Report and Mid-Long-Term Clinical Outcomes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
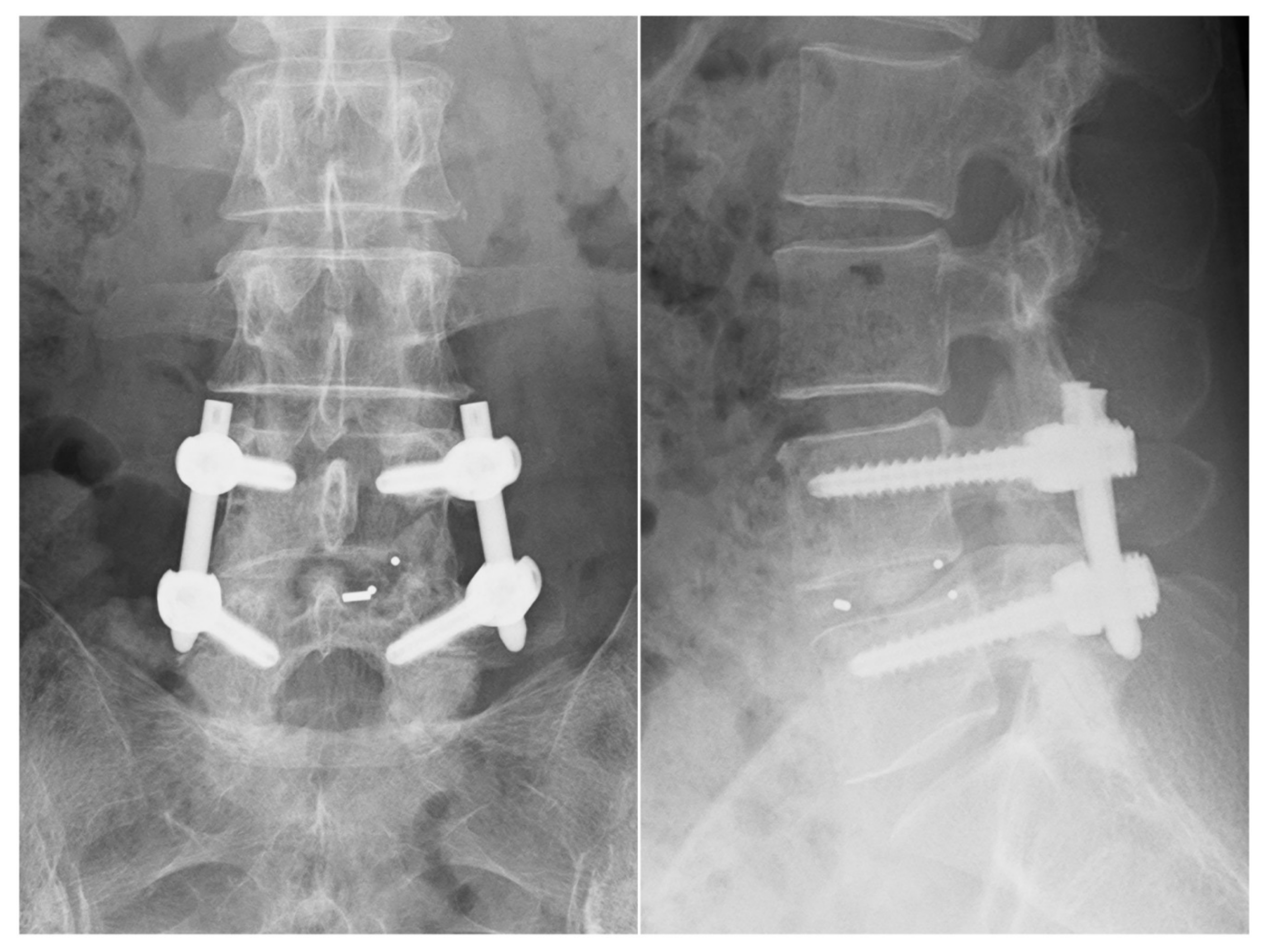
2.2. Surgical Procedures
2.3. Outcome Assessment
2.4. Statistical Analysis
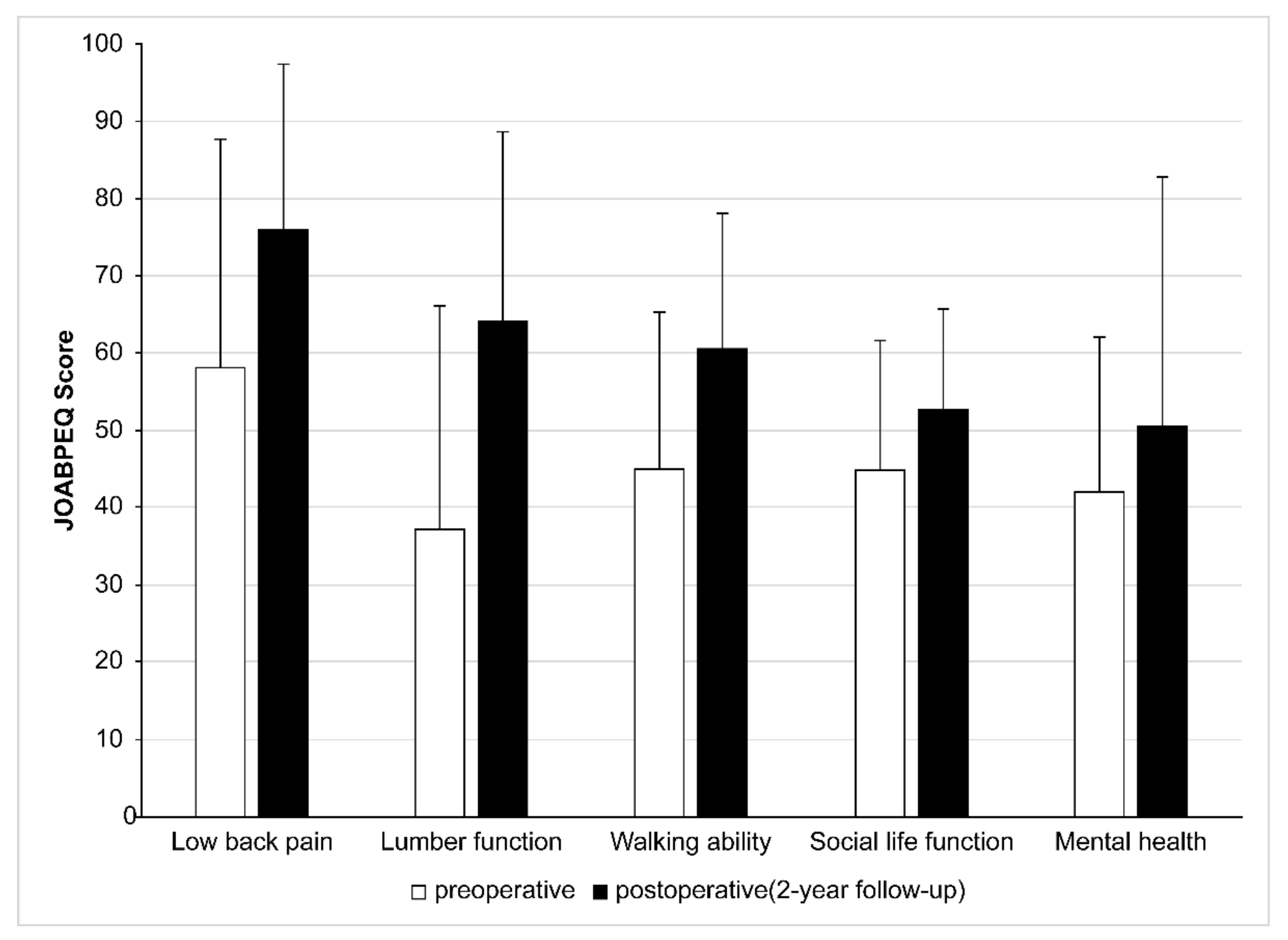
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baba, S. The super-aged society. World Health 1993, 46, 9–11. [Google Scholar]
- Cloward, R.B. The treatment of ruptured lumbar intervertebral discs; criteria for spinal fusion. Am. J. Surg. 1953, 86, 145–151. [Google Scholar] [CrossRef]
- Harms, J.; Rolinger, H. Die operative Behandlung der Spondylolisthese durch dorsale Aufrichtung und ventrale Verblockung. Z. Orthop. Ihre. Grenzgeb. 1982, 120, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.T.; Holly, L.T.; Schwender, J.D. Minimally invasive lumbar fusion. Spine 2003, 28, S26–S35. [Google Scholar] [CrossRef]
- Park, Y.; Ha, J.W. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 2007, 32, 537–543. [Google Scholar] [CrossRef]
- Peng, C.W.; Yue, W.M.; Poh, S.Y.; Yeo, W.; Tan, S.B. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine 2009, 34, 1385–1389. [Google Scholar] [CrossRef]
- Fan, S.; Zhao, X.; Zhao, F.; Fang, X. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine 2010, 35, 1615–1620. [Google Scholar]
- Lee, K.H.; Yue, W.M.; Yeo, W.; Soeharno, H.; Tan, S.B. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur. Spine J. 2012, 21, 2265–2270. [Google Scholar] [CrossRef]
- Fan, G.; Zhang, H.; Guan, X.; Gu, G.; Wu, W.; Hu, A.; Gu, X.; He, S. Patient-reported and radiographic outcomes of minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis with or without reduction: A comparative study. J. Clin. Neurosci. 2016, 33, 111–118. [Google Scholar] [CrossRef]
- Schwender, J.D.; Holly, L.T.; Rouben, D.P.; Foley, K.T. Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. Clin. Spine Surg. 2005, 18, S1–S6. [Google Scholar] [CrossRef] [Green Version]
- Channg, K.L.; Jeong, Y.P.; Ho, Y.Z. Minimally invasive transforaminal lumbar interbody fusion using a single interbody cage and a tubular retraction system: Technical tips, and perioperative, radiological and clinical outcomes. J. Korean Neurosurg. Soc. 2010, 48, 219–224. [Google Scholar]
- Wada, A.; Takahashi, H.; Yokoyama, Y. Minimally invasive transforaminal lumbar interbody fusion using a tubular retractor and percutaneous pedicle screw for patients with degenerative spondylolisthesis. J. Spine Res. 2011, 2, 1382–1390. [Google Scholar]
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 2015, 1, 2–18. [Google Scholar] [PubMed]
- Kevin, P.; Prashanth, J.; Andrew, C.; Mobbs, R.J. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: Systematic review and meta-analysis. Eur. Spine J. 2015, 24, 1017–1030. [Google Scholar]
- Park, Y.; Lee, S.B.; Seok, S.O.; Lee, S.B.; Seok, S.O.; Jo, B.W.; Ha, J.W. Perioperative surgical complications and learning curve associated with minimally invasive transforaminal lumbar interbody fusion: A single-institute experience. Clin. Orthop. Surg. 2015, 7, 91–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lener, S.; Wipplinger, C.; Hernandez, R.N.; Hussain, I.; Kimaz, S.; Navarro-Ramirez, R.; Schmidt, F.A.; Kim, E.; Hartl, L. Defining the MIS-TLIF: A systematic review of techniques and technologies used by surgeons worldwide. Glob. Spine J. 2020, 10, 151–167. [Google Scholar] [CrossRef]
- Hasegawa, K.; Kitahara, K.; Simoda, H.; Hara, T. Facet joint opening in lumbar degenerative diseases indicating segmental instability. J. Neurosurg. Spine 2010, 12, 687–693. [Google Scholar] [CrossRef] [Green Version]
- Hasegawa, K.; Kitahara, K.; Simoda, H.; Ishii, K.; Ono, M.; Homma, T.; Watanabe, K. Lumbar degenerative spondylolisthesis is not always unstable: Clinicobiomechanical evidence. Spine 2014, 39, 2127–2135. [Google Scholar] [CrossRef] [Green Version]
- Bridwell, K.H.; Lenke, L.G.; McEnery, K.W.; Baldus, C.; Blanke, K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 1995, 20, 1410–1418. [Google Scholar] [CrossRef]
- Kim, J.E.; Choi, D.J. Biportal endoscopic transforaminal lumbar interbody fusion with arthroscopy. Clin. Orthop. Surg. 2018, 10, 248–252. [Google Scholar] [CrossRef]
- Lv, Y.; Chen, M.; Wang, S.L.; Qin, R.J.; Ma, C.; Ding, Q.R.; Qin, H.N.; Wang, X.F.; Ren, Y.X. Endo-TLIF versus MIS-TLIF in 1-segment lumbar spondylolisthesis: A prospective randomized pilot study. Clin. Neurol. Neurosurg. 2022, 212, 107082. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Wang, L.; Yuan, S.; Tian, Y.; Zhao, Y.; Liu, X. Percutaneous endoscopic robot-assisted transforaminal lumbar interbody fusion (PE RA-TLIF) for lumbar spondylolisthesis: A technical note and two years clinical results. Pain Phys. 2022, 25, E73–E86. [Google Scholar]
- Ozgur, B.M.; Aryan, H.E.; Pimenta, L.; Taylor, W.R. Extreme lateral interbody fusion (XLIF): A novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006, 6, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Guigui, P.; Ferrero, E. Surgical treatment of degenerative spondylolisthesis. Orthop. Traumatol. Surg. Res. 2017, 103, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Fujibayashi, S.; Kawakami, N.; Asazuma, T.; Ito, M.; Mizutani, J.; Nagashima, H.; Nakamura, M.; Sairyo, K.; Takemasa, R.; Iwasaki, M. Complications associated with lateral interbody fusion: Nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine 2017, 42, 1478–1484. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.S.; Walker, C.T.; Godzik, J.; Turner, J.D.; Smith, W.; Uribe, J.S. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: A literature review. Ann. Transl. Med. 2018, 6, 104. [Google Scholar] [CrossRef]
- Allain, J.; Dufour, T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop. Traumatol. Surg. Res. 2020, 106, 149–157. [Google Scholar] [CrossRef]
- Leonova, O.N.; Cherepanov, E.A.; Krutko, A.V. MIS-TLIF versus O-TLIF for single-level degenerative stenosis: Study protocol for randomised controlled trial. BML Open 2021, 5, e041134. [Google Scholar] [CrossRef]
- Kotani, Y.; Koike, Y.; Ikeura, A.; Tokunaga, H.; Saito, T. Clinical and radiologic comparison of anterior-posterior single-position lateral surgery versus MIS-TLIF for degenerative lumbar spondylolisthesis. J. Orthop. Sci. 2021, 26, 992–998. [Google Scholar] [CrossRef]
- Hung, S.F.; Liao, J.C.; Tsai, T.T.; Li, Y.D.; Chiu, P.Y.; Hsieh, M.K.; Kao, F.C. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci. Rep. 2021, 17, 12783. [Google Scholar] [CrossRef]
- Sembrano, J.N.; Tohmeh, A.; Isaacs, R.; SOLAS Degenerative Study Group. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part I: Clinical findings. Spine 2016, 41, S123–S132. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, R.E.; Sembrano, J.N.; Tohmeh, A.G.; SOLAS Degenerative Study Group. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part II: Radiographic findings. Spine 2016, 41, S133–S134. [Google Scholar] [CrossRef]
- Kim, C.H.; Easley, K.; Lee, J.S.; Hong, J.Y.; Virk, M.; Hsieh, P.C.; Yoon, S.T. Comparison of minimally invasive versus open transforaminal interbody lumbar fusion. Glob. Spine J. 2020, 10, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Guiot, B.H.; Khoo, L.T.; Fessler, R.G. A minimally invasive technique for decompression of the lumbar spine. Spine 2002, 27, 432–438. [Google Scholar] [CrossRef]
- Holly, L.T.; Schwender, J.D.; Rouben, D.P.; Foley, K.T. Minimally invasive transforaminal lumbar interbody fusion: Indications, technique, and complications. Neurosurg. Focus 2006, 15, E6. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Tabaraee, E.; Singh, K. Minimally invasive transforaminal lumbar interbody fusion. J. Spinal Disord. Tech. 2015, 28, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Nandyala, S.V.; Fineberg, S.J.; Pelton, M.; Singh, K. Minimally invasive transforaminal lumbar interbody fusion: One surgeon’s learning curve. Spine J. 2014, 14, 1460–1465. [Google Scholar] [CrossRef]
- Poletti, C.E. Central lumbar stenosis caused by ligamentum flavum: Unilateral laminotomy for bilateral ligamentectomy: Preliminary report of two case. Neurosurgery 1995, 37, 343–347. [Google Scholar] [CrossRef]
- Spetzger, U.; Bertalanffy, H.; Reinges, M.H.T.; Gilsback, J.M. Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis part II: Clinical experiences. Acta Neurochir. 1997, 139, 397–403. [Google Scholar] [CrossRef]
- Khoo, L.T.; Fessler, R.G. Microendoscopic decompressive laminotomy for the treatment of lumbar stenosis. Neurosurgery 2002, 51, S146–S154. [Google Scholar] [CrossRef]
- Palmer, S.; Turner, R.; Palmer, R. Bilateral decompressive surgery in lumbar spinal stenosis associated with spondylolisthesis: Unilateral approach and use of a microscope and tubular retractor system. FOC 2002, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Inanami, H.; Saiki, F.; Oshima, Y. Microendoscope-assisted posterior lumbar interbody fusion, a technical note. J. Spine Surg. 2018, 4, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Matsui, H.; Tsuji, H. Back muscle injury after posterior lumbar surgery. A histological and enzymatic analysis. Spine 1996, 21, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Y.; Chong, F.; Zhou, Y.; Huang, B. Clinical outcomes of minimally invasive transforaminal lumbar interbody fusion via a novel tubular retractor. J. Int. Med. Res. 2020, 48, 300060520920090. [Google Scholar] [CrossRef]
- Silva, P.S.; Pereira, P.; Monteiro, P. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg. Focus 2013, 35, E7. [Google Scholar] [CrossRef] [Green Version]
- Parker, S.L.; Adogwa, O.; Witham, T.F.; Aaronson, O.S.; Cheng, J.; McGirt, M.J. Post-operative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): Literature review and cost analysis. Minim. Invasive Neurosurg. 2011, 54, 33–37. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare Ministerial Notification No. 65. Available online: https://hodanren.doc-net.or.jp/iryoukankei/20kaitei/horei/2_3_200305_hi1_1_0609.pdf (accessed on 8 December 2021).
- Harrop, J.S.; Hilibrand, A.; Mihalovich, K.E.; Dettori, J.R.; Chapman, J. Cost-effectiveness of surgical treatment for degenerative spondylolisthesis and spinal stenosis. Spine 2014, 39, S75–S85. [Google Scholar] [CrossRef]
- Tosteson, A.N.; Lurie, J.D.; Tosteson, T.D.; Skinner, J.S.; Herkowitz, H.; Albert, T.; Boden, S.D.; Bridwell, K.; Longley, M.; Andersson, G.B.; et al. Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: Cost-effectiveness after 2 years. Ann. Intern. Med. 2008, 16, 845–853. [Google Scholar] [CrossRef]
- Kim, C.H.; Chung, C.K.; Choi, Y.; Lee, J.; Yang, S.H.; Lee, C.H.; Park, S.B.; Kim, K.T.; Rhee, J.M.; Park, M.S. Direct medical costs after surgical or nonsurgical treatment for degenerative lumbar spinal disease: A nationwide matched cohort study with a 10-year follow-up. PLoS ONE 2021, 1, e0260460. [Google Scholar] [CrossRef]
- Parker, S.L.; Mendenhall, S.K.; Shau, D.N.; Zuckerman, S.L.; Godil, S.S.; Cheng, J.S.; McGirt, M.J. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: Comparative effectiveness and cost-utility analysis. World Neurosurg. 2014, 82, 230–238. [Google Scholar] [CrossRef]
| Characteristics | POSDe | OS | p-Value |
|---|---|---|---|
| No. of cases | 50 | 27 | |
| Age (year), means ± SD (range) | 69.2 ± 9.6 (46–89) | 67.9 ± 6.6 (49–78) | 0.361 |
| Sex (male:female) | 19:31 | 4:23 | 0.0397 # |
| No. of levels treated | 1.000 | ||
| L3/4 | 5 | 3 | |
| L4/5 | 40 | 11 | |
| L5/S1 | 5 | 3 |
| Characteristics | POSDe | OS | p-Value |
|---|---|---|---|
| VAS for back pain | |||
| Preop. | 64.3 | 78.3 | <0.0001 * |
| Postop. (2 years) | 12.1 | 12.8 | <0.0001 * |
| JOA score | |||
| Preop. | 12.1 | 12.8 | 0.423 |
| Postop. (2 years) | 26.0 | 24.6 | 0.0514 |
| Operation time (min) | 103.1 | 172.1 | <0.0001 * |
| Blood loss (mL) | 74.2 | 135.3 | <0.0001 * |
| Complications | POSDe N (%) | OS N (%) | p-Value |
|---|---|---|---|
| Deep wound infection | 0 (0) | 0 (0) | 1.000 |
| Pseudoarthrosis | 4 (8) | 2 (7.4) | 1.000 |
| Dural injury | 2 (4) | 0 (0) | 0.55 |
| Cage retropulsion | 3 (6) | 2 (7.4) | 1.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomita, T.; Kamei, K.; Yamauchi, R.; Nakagawa, T.; Omi, H.; Nitobe, Y.; Asari, T.; Kumagai, G.; Wada, K.; Ito, J.; et al. Posterior Oblique Square Decompression with a Three-Step Wanding Technique in Tubular Minimally Invasive Transforaminal Lumbar Interbody Fusion: Technical Report and Mid-Long-Term Clinical Outcomes. J. Clin. Med. 2022, 11, 1651. https://doi.org/10.3390/jcm11061651
Tomita T, Kamei K, Yamauchi R, Nakagawa T, Omi H, Nitobe Y, Asari T, Kumagai G, Wada K, Ito J, et al. Posterior Oblique Square Decompression with a Three-Step Wanding Technique in Tubular Minimally Invasive Transforaminal Lumbar Interbody Fusion: Technical Report and Mid-Long-Term Clinical Outcomes. Journal of Clinical Medicine. 2022; 11(6):1651. https://doi.org/10.3390/jcm11061651
Chicago/Turabian StyleTomita, Takashi, Keita Kamei, Ryota Yamauchi, Takahiro Nakagawa, Hirotsugu Omi, Yoshiro Nitobe, Toru Asari, Gentaro Kumagai, Kanichiro Wada, Junji Ito, and et al. 2022. "Posterior Oblique Square Decompression with a Three-Step Wanding Technique in Tubular Minimally Invasive Transforaminal Lumbar Interbody Fusion: Technical Report and Mid-Long-Term Clinical Outcomes" Journal of Clinical Medicine 11, no. 6: 1651. https://doi.org/10.3390/jcm11061651
APA StyleTomita, T., Kamei, K., Yamauchi, R., Nakagawa, T., Omi, H., Nitobe, Y., Asari, T., Kumagai, G., Wada, K., Ito, J., & Ishibashi, Y. (2022). Posterior Oblique Square Decompression with a Three-Step Wanding Technique in Tubular Minimally Invasive Transforaminal Lumbar Interbody Fusion: Technical Report and Mid-Long-Term Clinical Outcomes. Journal of Clinical Medicine, 11(6), 1651. https://doi.org/10.3390/jcm11061651






