Usefulness of 68-Gallium PET in Type I Gastric Neuroendocrine Neoplasia: A Case Series
Abstract
1. Background
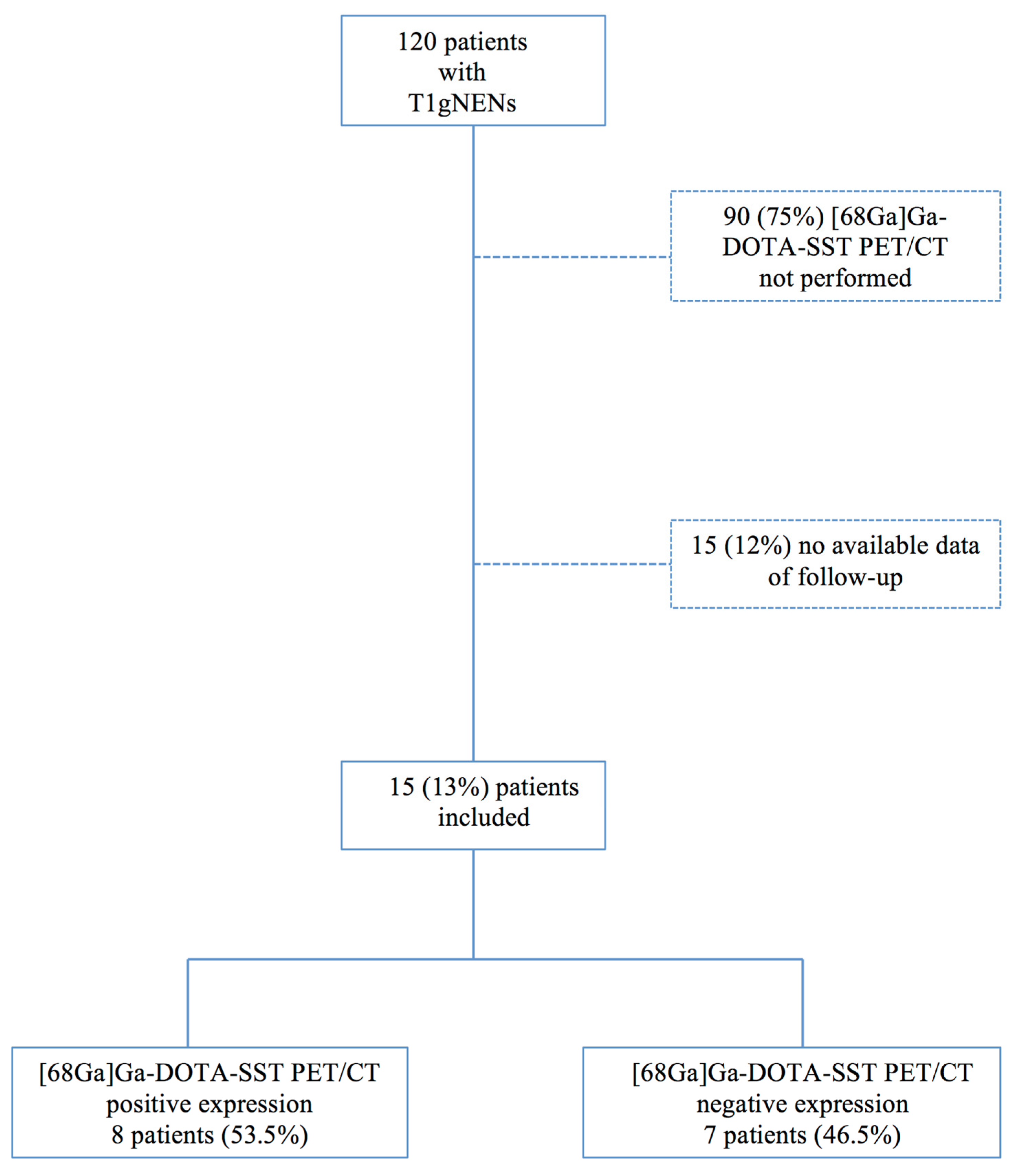
2. Patients and Method
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delle Fave, G.; Sundin, A.; Taal, B.; Ferolla, P.; Ramage, J.K.; Ferone, D.; Ito, T.; Weber, W.; Zheng-Pei, Z.; De Herder, W.W.; et al. ENETS Consensus Guidelines Update for Gastroduodenal Neuroendocrine Neoplasms. Neuroendocrinology 2016, 103, 119. [Google Scholar] [CrossRef] [PubMed]
- Grozinsky-Glasberg, S.; Thomas, D.; Strosberg, J.R.; Pape, U.F.; Felder, S.; Tsolakis, A.V.; Alexandraki, K.I.; Fraenkel, M.; Saiegh, L.; Reissman, P.; et al. Metastatic type 1 gastric carcinoid: A real threat or just a myth? World J. Gastroenterol. 2013, 19, 8687–8695. [Google Scholar] [CrossRef] [PubMed]
- Panzuto, F.; Campana, D.; Massironi, S.; Faggiano, A.; Rinzivillo, M.; Lamberti, G.; Sciola, V.; Lahner, E.; Manuzzi, L.; Colao, A.; et al. Tumour type and size are prognostic factors in gastric neuroendocrine neoplasia: A multicentre retrospective study. Dig. Liver Dis. 2019, 51, 1456–1460. [Google Scholar] [CrossRef] [PubMed]
- Vanoli, A.; La Rosa, S.; Miceli, E.; Klersy, C.; Maragliano, R.; Capuano, F.; Persichella, A.; Martino, M.; Inzani, F.; Luinetti, O.; et al. Prognostic Evaluations Tailored to Specific Gastric Neuroendocrine Neoplasms: Analysis Of 200 Cases with Extended Follow-Up. Neuroendocrinology 2018, 107, 114. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Tsolakis, A.V.; Grozinsky-Glasberg, S.; Fraenkel, M.; Alexandraki, K.; Sougioultzis, S.; Gross, D.J.; Kaltsas, G. Long-term follow-up of a large series of patients with type 1 gastric carcinoid tumors: Data from a multicenter study. Eur. J. Endocrinol. 2013, 168, 185–193. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vannella, L.; Sbrozzi-Vanni, A.; Lahner, E.; Bordi, C.; Pilozzi, E.; Corleto, V.D.; Osborn, J.F.; Fave, G.D.; Annibale, B. Development of type I gastric carcinoid in patients with chronic atrophic gastritis. Aliment. Pharmacol. Ther. 2011, 33, 1361–1369. [Google Scholar] [CrossRef] [PubMed]
- Ngamruengphong, S.; Ferri, L.; Aihara, H.; Draganov, P.V.; Yang, D.J.; Perbtani, Y.B.; Jue, T.L.; Munroe, C.A.; Boparai, E.S.; Mehta, N.A.; et al. Efficacy of Endoscopic Submucosal Dissection for Superficial Gastric Neoplasia in a Large Cohort in North America. Clin. Gastroenterol. Hepatol. 2020, 19, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Panzuto, F.; Magi, L.; Esposito, G.; Rinzivillo, M.; Annibale, B. Comparison of Endoscopic Techniques in the Management of Type I Gastric Neuroendocrine Neoplasia: A Systematic Review. Gastroenterol. Res. Pract. 2021, 2021, 6679397. [Google Scholar] [CrossRef] [PubMed]
- Esposito, G.; Cazzato, M.; Rinzivillo, M.; Pilozzi, E.; Lahner, E.; Annibale, B.; Panzuto, F. Management of type-I gastric neuroendocrine neoplasms: A 10-years prospective single centre study. Dig. Liver Dis. 2021; in press. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.R.; Coppola, D.; Klimstra, D.S.; Phan, A.T.; Kulke, M.H.; Wiseman, G.A.; Kvols, L.K.; North American Neuroendocrine Tumor Society (NANETS). The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas 2010, 39, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.H.; Goldner, W.S.; Benson, A.B.; Bergsland, E.; Blaszkowsky, L.S.; Brock, P.; Chan, J.; Das, S.; Dickson, P.V.; Fanta, P.; et al. Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 839–868. [Google Scholar] [CrossRef] [PubMed]
- WHO Classification of Tumours Editorial Board (Ed.) Gastric neuroendocrine neoplasms. Digestive system tumours. In WHO Classification of Tumours, 5th ed.; IARC Press: Lyon, France, 2019; Volume 1, pp. 104–109. [Google Scholar]
- Carideo, L.; Prosperi, D.; Panzuto, F.; Magi, L.; Pratesi, M.S.; Rinzivillo, M.; Annibale, B.; Signore, A. Role of Combined [68Ga]Ga-DOTA-SST Analogues and [18F]FDG PET/CT in the Management of GEP-NENs: A Systematic Review. J. Clin. Med. 2019, 8, 1032. [Google Scholar] [CrossRef]
- Lahner, E.; Esposito, G.; Pilozzi, E.; Galli, G.; Corleto, V.D.; Di Giulio, E.; Annibale, B. Gastric cancer in patients with type I gastric carcinoids. Gastric Cancer 2015, 18, 564–570. [Google Scholar] [CrossRef]
- Lahner, E.; Zagari, R.M.; Zullo, A.; Di Sabatino, A.; Meggio, A.; Cesaro, P.; Lenti, M.V.; Annibale, B.; Corazza, G.R. Chronic atrophic gastritis: Natural history, diagnosis and therapeutic management. A position paper by the Italian Society of Hospital Gastroenterologists and Digestive Endoscopists [AIGO], the Italian Society of Digestive Endoscopy [SIED], the Italian Society of Gastroenterology [SIGE], and the Italian Society of Internal Medicine [SIMI]. Dig. Liver Dis. 2019, 51, 1621–1632. [Google Scholar] [PubMed]
- La Rosa, S.; Inzani, F.; Vanoli, A.; Klersy, C.; Dainese, L.; Rindi, G.; Capella, C.; Bordi, C.; Solcia, E. Histologic characterization and improved prognostic evaluation of 209 gastric neuroendocrine neoplasms. Hum. Pathol. 2011, 42, 1373–1384. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, S.; Vanoli, A. Gastric neuroendocrine neoplasms and related precursors lesions. J. Clin. Pathol. 2014, 67, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Panzuto, F.; Merola, E.; Pavel, M.E.; Rinke, A.; Kump, P.; Partelli, S.; Rinzivillo, M.; Rodriguez-Laval, V.; Pape, U.F.; Lipp, R.; et al. Stage IV Gastro-Entero-Pancreatic Neuroendocrine Neoplasms: A Risk Score to Predict Clinical Outcome. Oncologist 2017, 22, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Pape, U.-F.; Berndt, U.; Müller-Nordhorn, J.; Böhmig, M.; Roll, S.; Koch, M.; Willich, S.N.; Wiedenmann, B. Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocr. Relat. Cancer 2008, 15, 1083–1097. [Google Scholar] [CrossRef] [PubMed]
- Brighi, N.; La Rosa, S.; Rossi, G.; Grillo, F.; Pusceddu, S.; Rinzivillo, M.; Spada, F.; Tafuto, S.; Massironi, S.; Faggiano, A.; et al. Morphological Factors Related to Nodal Metastases in neuroendocrine Tumors of the Appendix: A Multicentric Retrospective Study. Ann. Surg. 2020, 271, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Merola, E.; Pavel, M.E.; Panzuto, F.; Capurso, G.; Cicchese, N.; Rinke, A.; Gress, T.M.; Iannicelli, E.; Prosperi, D.; Pizzichini, P.; et al. Functional Imaging in the Follow-Up of Enteropancreatic Neuroendocrine Tumors: Clinical Usefulness and Indications. J. Clin. Endocrinol. Metab. 2017, 102, 1486–1494. [Google Scholar] [CrossRef] [PubMed]


| n | |
|---|---|
| Gender | 8 Female (53%) 7 Male (47%) |
| Median Age (years) | 51 (IQR 49–68) |
| Ki-67 Proliferative Index | 6 % (1–9%) |
| Grading * G1 G2 | 9 (60%) 6 (40%) |
| Tumor size (mm) | 13 (IQR 5–55) |
| Multiple tumor at diagnosis | 2 (13.3%) |
| Dimension of Primitive Tumour | Ki-67 Proliferative Index | [68Ga]Ga-DOTA-SST PET/CT Positive Expression on Primitive Tumour | [68Ga]Ga-DOTA-SST PET/CT Positive Expression on Locoregional Metastasis | [68Ga]Ga-DOTA-SST PET/CT Positive Expression on Distant Metastasis | Endoscopical Resection | Positive Margins after Endoscopical Resection | Surgical Resection | Somatostatin Analogue Therapy | |
|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 8 mm | 1% | Yes | No | No | Yes | Yes | No | No |
| Patient 2 | 9 mm | 2% | Yes | No | No | Yes | Yes | No | No |
| Patient 3 | 12 mm | <1% | Yes | No | No | Yes | No | No | No |
| Patient 4 | 12 mm | 2% | Yes | No | No | Yes | No | No | No |
| Patient 5 | 20 mm | 2% | Yes | No | No | Yes | No | No | No |
| Patient 6 | 50 mm | 4% | No | No | Yes | No | - | No | Yes |
| Patient 7 | 20 mm | 3% | No | Yes | No | No | Yes | Yes | No |
| Patient 8 | 20 mm | 2% | No | Yes | No | No | Yes | Yes | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rinzivillo, M.; Panzuto, F.; Esposito, G.; Lahner, E.; Signore, A.; Annibale, B. Usefulness of 68-Gallium PET in Type I Gastric Neuroendocrine Neoplasia: A Case Series. J. Clin. Med. 2022, 11, 1641. https://doi.org/10.3390/jcm11061641
Rinzivillo M, Panzuto F, Esposito G, Lahner E, Signore A, Annibale B. Usefulness of 68-Gallium PET in Type I Gastric Neuroendocrine Neoplasia: A Case Series. Journal of Clinical Medicine. 2022; 11(6):1641. https://doi.org/10.3390/jcm11061641
Chicago/Turabian StyleRinzivillo, Maria, Francesco Panzuto, Gianluca Esposito, Edith Lahner, Alberto Signore, and Bruno Annibale. 2022. "Usefulness of 68-Gallium PET in Type I Gastric Neuroendocrine Neoplasia: A Case Series" Journal of Clinical Medicine 11, no. 6: 1641. https://doi.org/10.3390/jcm11061641
APA StyleRinzivillo, M., Panzuto, F., Esposito, G., Lahner, E., Signore, A., & Annibale, B. (2022). Usefulness of 68-Gallium PET in Type I Gastric Neuroendocrine Neoplasia: A Case Series. Journal of Clinical Medicine, 11(6), 1641. https://doi.org/10.3390/jcm11061641








