Non-Small-Cell Lung Cancer Patients with Coexistence of High PD-L1 Expression and RET Fusion—Which Path Should We Follow? Case Reports and Literature Review
Abstract
:1. Introduction
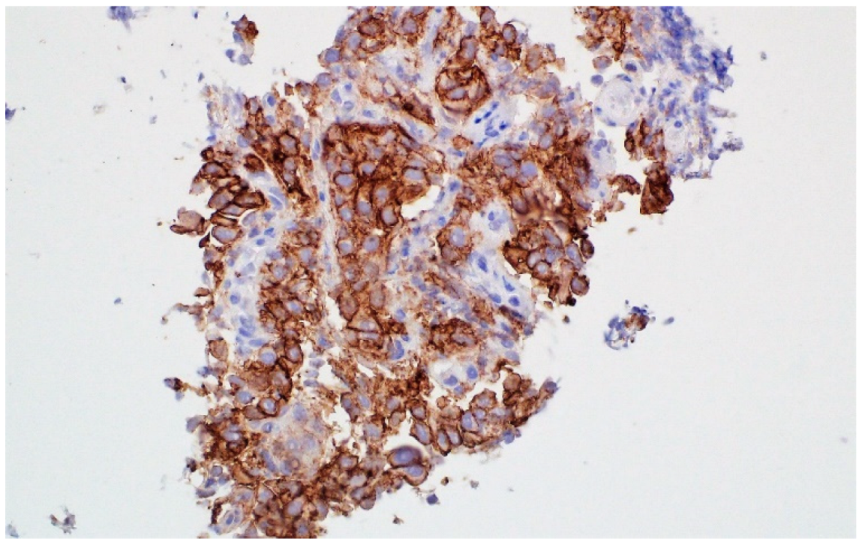
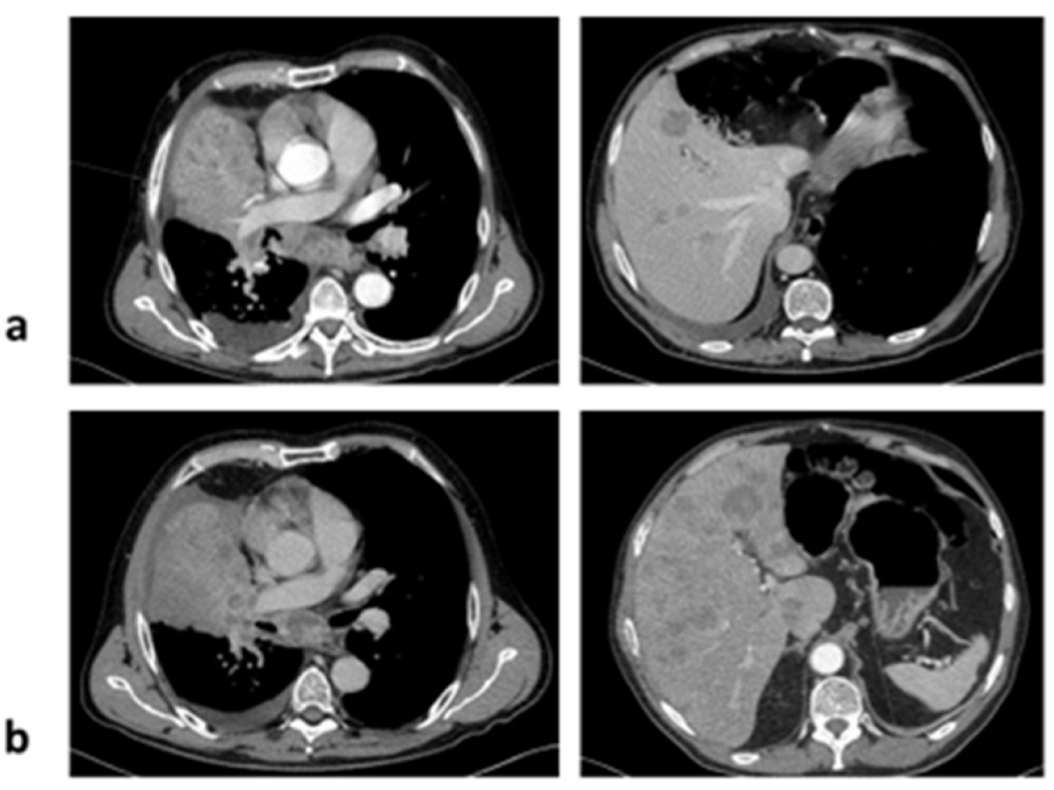
2. Case 1
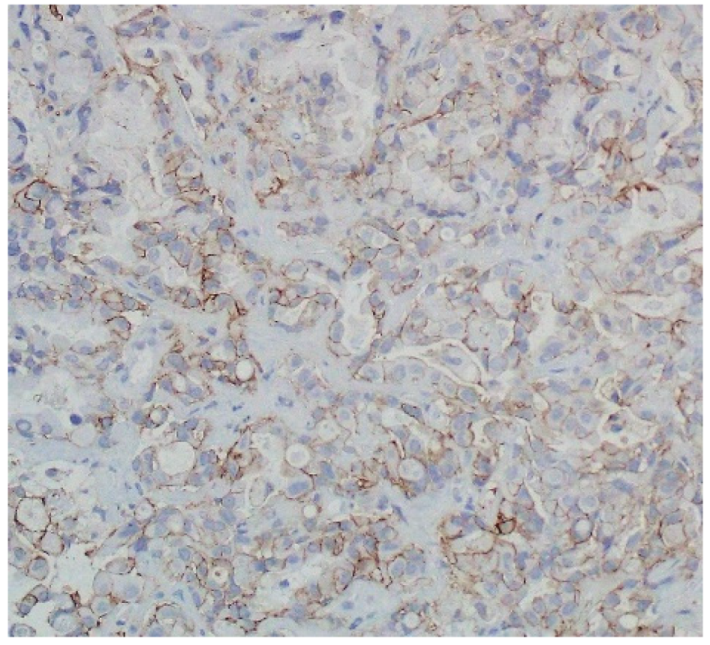
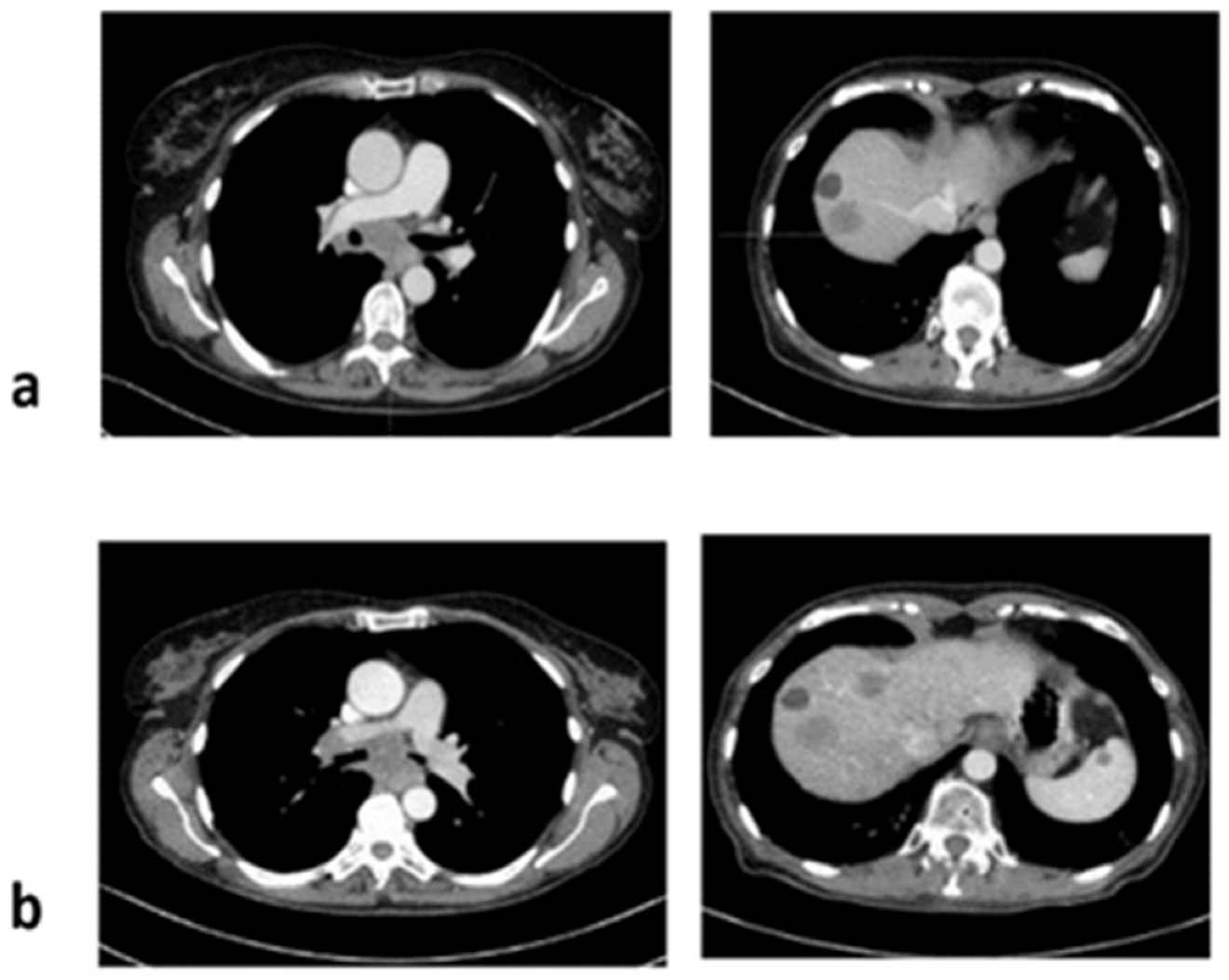
3. Case 2
4. Discussion
4.1. The Value of Immunotherapy in Patients with RET Fusion
4.2. Effectiveness of Immunotherapy in Patients with Other Rare Molecular Alterations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1–Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Five-Year Outcomes With Pembrolizumab Versus Chemotherapy for Metastatic Non–Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score ≥ 50. J. Clin. Oncol. 2021, 39, 2339–2349. [Google Scholar] [CrossRef] [PubMed]
- Rittmeyer, A.; Barlesi, F.; Waterkamp, D.; Park, K.; Ciardiello, F.; von Pawel, J.; Gadgeel, S.M.; Hida, T.; Kowalski, D.M.; Dols, M.C.; et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): A phase 3, open-label, multicentre randomised controlled trial. Lancet 2017, 389, 255–265. [Google Scholar] [CrossRef]
- Calles, A.; Riess, J.W.; Brahmer, J.R. Checkpoint Blockade in Lung Cancer With Driver Mutation: Choose the Road Wisely. Am. Soc. Clin. Oncol. Educ. Book 2020, 40, 372–384. [Google Scholar] [CrossRef]
- Dudnik, E.; Bshara, E.; Grubstein, A.; Fridel, L.; Shochat, T.; Roisman, L.C.; Ilouze, M.; Rozenblum, A.B.; Geva, S.; Zer, A.; et al. Rare targetable drivers (RTDs) in non-small cell lung cancer (NSCLC): Outcomes with immune check-point inhibitors (ICPi). Lung Cancer 2018, 124, 117–124. [Google Scholar] [CrossRef]
- Gautschi, O.; Milia, J.; Filleron, T.; Wolf, J.; Carbone, D.P.; Owen, D.H.; Camidge, R.; Narayanan, V.; Doebele, R.C.; Besse, B.; et al. Targeting RET in Patients With RET-Rearranged Lung Cancers: Results From the Global, Multicenter RET Registry. J. Clin. Oncol. 2017, 35, 1403–1410. [Google Scholar] [CrossRef] [Green Version]
- Hess, L.M.; Han, Y.; Zhu, Y.E.; Bhandari, N.R.; Sireci, A. Characteristics and outcomes of patients with RET-fusion positive non-small lung cancer in real-world practice in the United States. BMC Cancer 2021, 21, 28. [Google Scholar] [CrossRef]
- Drilon, A.; Bergagnini, I.; Delasos, L.; Sabari, J.; Woo, K.M.; Plodkowski, A.; Wang, L.; Hellmann, M.D.; Joubert, P.; Sima, C.S.; et al. Clinical outcomes with pemetrexed-based systemic therapies in RET-rearranged lung cancers. Ann. Oncol. 2016, 27, 1286–1291. [Google Scholar] [CrossRef] [Green Version]
- Shen, T.; Pu, X.; Wang, L.; Yu, Z.; Li, J.; Zhang, Y.; Liang, X.; Chen, H.; Xu, C.; Song, Z.; et al. Association Between RET Fusions and Efficacy of Pemetrexed-based Chemotherapy for Patients With Advanced NSCLC in China: A Multicenter Retrospective Study. Clin. Lung Cancer 2020, 21, e349–e354. [Google Scholar] [CrossRef]
- Hida, T.; Velcheti, V.; Reckamp, K.L.; Nokihara, H.; Sachdev, P.; Kubota, T.; Nakada, T.; Dutcus, C.E.; Ren, M.; Tamura, T. A phase 2 study of lenvatinib in patients with RET Fusion-positive lung adenocarcinoma. Lung Cancer 2019, 138, 124–130. [Google Scholar] [CrossRef] [Green Version]
- Drilon, A.; Rekhtman, N.; Arcila, M.; Wang, L.; Ni, A.; Albano, M.; van Voorthuysen, M.; Somwar, R.; Smith, R.S.; Montecalvo, J.; et al. Cabozantinib in patients with advanced RET -rearranged non-small-cell lung cancer: An open-label, single-centre, phase 2, single-arm trial. Lancet Oncol. 2016, 17, 1653–1660. [Google Scholar] [CrossRef] [Green Version]
- Yoh, K.; Seto, T.; Satouchi, M.; Nishio, M.; Yamamoto, N.; Murakami, H.; Nogami, N.; Nosaki, K.; Kohno, T.; Tsuta, K.; et al. Vantedanib in patients with previously treated RET-rearranged advanced non-small-cell lung cancer (LURET): An open-label, multicentre phase 2 trial. Lung Cancer 2021, 155, 40–45. [Google Scholar] [CrossRef]
- Gainor, J.F.; Curigliano, G.; Kim, D.-W.; Lee, D.H.; Besse, B.; Baik, C.S.; Doebele, R.C.; Cassier, P.A.; Lopes, G.; Tan, D.S.W.; et al. Pralsetinib for RET fusion-positive non-small-cell lung cancer (ARROW): A multi-cohort, open-label, phase 1/2 study. Lancet Oncol. 2021, 22, 959–969. [Google Scholar] [CrossRef]
- Drilon, A.; Oxnard, G.R.; Tan, D.S.; Loong, H.H.; Johnson, M.; Gainor, J.; McCoach, C.E.; Gautschi, O.; Besse, B.; Cho, B.C.; et al. Efficacy of Selpercatinib in RET Fusion-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Offin, M.; Guo, R.; Wu, S.L.; Sabari, J.; Land, J.D.; Ni, A.; Montecalvo, J.; Halpenny, D.F.; Buie, L.W.; Pak, T.; et al. Immunophenotype and Response to Immunotherapy of RET-Rearranged Lung Cancers. JCO Precis. Oncol. 2019, 3, PO.18.00386. [Google Scholar] [CrossRef] [PubMed]
- Dantoing, E.; Piton, N.; Salaün, M.; Thiberville, L.; Guisier, F. Anti-PD1/PD-L1 Immunotherapy for Non-Small Cell Lung Cancer with Actionable Oncogenic Driver Mutations. Int. J. Mol. Sci. 2021, 22, 6288. [Google Scholar] [CrossRef] [PubMed]
- Greillier, L.; Tomasini, P.; Barlesi, F. The clinical utility of tumor mutational burden in non-small cell lung cancer. Transl. Lung Cancer Res. 2018, 7, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, A.J.; Rizvi, H.; Bandlamudi, C.; Sauter, J.L.; Travis, W.D.; Rekhtman, N.; Plodkowski, A.J.; Perez-Johnston, R.; Sawan, P.; Beras, A.; et al. Clinical and molecular correlates of PD-L1 expression in patients with lung adenocarcinomas. Ann. Oncol. 2020, 31, 599–608. [Google Scholar] [CrossRef]
- Guisier, F.; Dubos-Arvis, C.; Viñas, F.; Doubre, H.; Ricordel, C.; Ropert, S.; Janicot, H.; Bernardi, M.; Fournel, P.; Lamy, R.; et al. Efficacy and safety of anti-PD-1 immunotherapy in patients with advanced non-small cell lung cancer with BRAF, HER2 or MET mutation or RET-translocation: GFPC 01-2018. J. Thorac. Oncol. 2020, 15, 628–636. [Google Scholar] [CrossRef]
- Hegde, A.; Huang, L.; Liu, S.; Hess, K.; Cabanillas, M.; Hu, M.; Busaidy, N.; Sherman, S.; Simon, G.; Blumenschein, G.; et al. Abstract 4997: Responsiveness to immune checkpoint inhibitors in RET dependent cancers. Cancer Res. 2019, 79, 4997. [Google Scholar]
- Lee, J.; Ku, B.M.; Shim, J.H.; La Choi, Y.; Sun, J.-M.; Lee, S.-H.; Ahn, J.S.; Park, K.; Ahn, M.-J. Characteristics and outcomes of RET-rearranged Korean non-small cell lung cancer patients in real-world practice. Jpn. J. Clin. Oncol. 2020, 50, 594–601. [Google Scholar] [CrossRef]
- Bhandari, N.R.; Hess, L.M.; Han, Y.; Zhu, Y.E.; Sireci, A.N. Efficacy of immune checkpoint inhibitor therapy in patients with RET fusion-positive non-small-cell lung cancer. Immunotherapy 2021, 13, 893–904. [Google Scholar] [CrossRef]
- Rodriguez, E.; Dawar, R.; Gawri, K.; Thammineni, V.; Torres, T.; Fanfan, D.; Saul, E.; Ikpeazu, C.; Lopes, G. Chemotherapy and immunotherapy outcomes of RET-rearranged lung cancers: A Case Series. J. Thorac. Oncol. 2021, 16, S685–S686. [Google Scholar] [CrossRef]
- Baglivo, S.; Ludovini, V.; Moretti, R.; Bellezza, G.; Sidoni, A.; Roila, F.; Metro, G. RET Rearrangement as a Predictor of Unresponsiveness to Immunotherapy in Non-Small Cell Lung Cancer: Report of Two Cases with Review of the Literature. Oncol. Ther. 2020, 8, 333–339. [Google Scholar] [CrossRef]
- Riudavets, M.; Caramella, C.; Pradere, P.; Naltet, C.; Le Pechoux, C.; Adam, J.; Mabille, L.; Rouleau, E.; Besse, B.; Planchard, D. Complete, unpredictable, multi-site response including brain and liver metastases in a patient with RET-rearranged non-small-cell Lung cancer treated with single-agent immunotherapy: A case report. Clin. Lung Cancer 2020, 22, e215–e219. [Google Scholar] [CrossRef]
- Mazieres, J.; Drilon, A.; Lusque, A.B.; Mhanna, L.; Cortot, A.; Mezquita, L.; Thai, A.A.; Mascaux, C.; Couraud, S.; Veillon, R.; et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: Results from the IMMUNOTARGET registry. Ann. Oncol. 2019, 30, 1321–1328. [Google Scholar] [CrossRef]
- Baby, S.; Khalil, F.; Tanvetyanon, T. Frontline pembrolizumab for the treatment of RET-rearranged non-small cell lung cancer: A case report. Cancer Treat. Res. Commun. 2021, 28, 100423. [Google Scholar] [CrossRef]
- Bodor, J.N.; Boumber, Y.; Borghaei, H. Biomarkers for immune checkpoint inhibition in non-small cell lung cancer (NSCLC). Cancer 2020, 126, 260–270. [Google Scholar] [CrossRef]
- Sabari, J.; Leonardi, G.; Shu, C.; Umeton, R.; Montecalvo, J.; Ni, A.; Chen, R.; Dienstag, J.; Mrad, C.; Bergagnini, I.; et al. PD-L1 expression, tumor mutational burden, and response to immunotherapy in patients with MET exon 14 altered lung cancers. Ann. Oncol. 2018, 29, 2085–2091. [Google Scholar] [CrossRef]
- Lai, W.C.V.; Feldman, D.L.; Buonocore, D.J.; Brzostowski, E.B.; Rizvi, H.; Plodkowski, A.J.; Ni, A.; Sabari, J.K.; Offin, M.D.; Kris, M.G.; et al. PD-L1 expression, tumor mutation burden and response to immune checkpoint blockade in patients with HER2-mutant lung cancers. J. Clin. Oncol. 2018, 36, 9060. [Google Scholar] [CrossRef]
- Negrao, M.V.; Skoulidis, F.; Montesion, M.; Schulze, K.; Bara, I.; Shen, V.; Xu, H.; Hu, S.; Sui, D.; Elamin, Y.Y.; et al. Oncogene-specific differences in tumor mutational burden, PD-L1 expression, and outcomes from immunotherapy in non-small cell lung cancer. J. Immunother. Cancer 2021, 9, e002891. [Google Scholar] [CrossRef]
- Eguren-Santamaria, I.; Sanmamed, M.F.; Gil-Bazo, I. Are Immune Checkpoint Inhibitors Effective Against Uncommon Oncogene-Driven NSCLC Subtypes? J. Thorac. Oncol. 2020, 15, 489–492. [Google Scholar] [CrossRef]
- McCoach, C.E.; Rolfo, C.; Drilon, A.; Lacouture, M.; Besse, B.; Goto, K.; Zhu, V.W.; Tan, D.S.; Farajian, S.; Potter, L.A.; et al. Hypersensitivity Reactions to Selpercatinib Treatment with or Without Prior Immune Checkpoint Inhibitor Therapy in Patients with Non-Small-Cell Lung Cancer in LIBRETTO-001. J. Thorac. Oncol. 2022, 17, S1556-0864(22)00094-6. [Google Scholar] [CrossRef]
| Author | Number of Patients | Number of Patients with PD-L1 > 50% | Response | Efficacy |
|---|---|---|---|---|
| Rodriguez 2021 [23] | 6 | 3 | 6 * | mPFS 9 months |
| Baglivo 2020 [24] | 2 | 2 | PD in both patients | PD after 1 cycle of pembrolizumab in both patients |
| Riudavets 2020 [25] | 1 | 1 | CR | Treatment discontinuation due to toxicity |
| Offin 2019 [22] | 16 | 1 | Assessed in 13 patients: PD-8 (62%), SD-3 (23%), non-CR/non-PD—2 (15%) | mPFS 3.4 months (95% CI 2.1–5.6) Patient with PD-L1 > 50%: PD after 1.3 month (nivolumab plus ipilimumab) |
| Mazieres 2019 [26] | 16 | NA | PR-1, SD-3 (25%) PD-12 (75%) | mPFS 2.1 months (95% CI 1.3–4.7) mOS 21.3 months (95% CI 3.8–28) |
| Dudnik 2018 [5] | 13 | 1 | Assessed in 4 patients- ORR 0/4 | mPFS 3.0 months (95% CI 1.9–3.1) mOS 14.9 months (95% CI 7.2–19.7) |
| Guisier 2019 [18] | 9 | 2 | PR-3, SD-2, PD-3, NA-1 | mPFS 7.6 months (95% CI 2.3-NR) mOS NR, 12 months OS 88.9% pts |
| Lee 2020 [21] | 13 | NA | ORR-0% DCR-25–50% | mPFS 2.1 months (95% CI: 1.6–2.6) mOS 12.4 (95% CI: 2.9–21.8) |
| Bhandari 2021 [22] | 69 | NA | ** ORR-33% DCR 66% | mPFS 4,2 months (95% CI: 1.4–8.4) mOS 19.1 months (95% CI: 6.9–NR) |
| Baby 2021 [27] | 1 | 1 | CR | tumour response lasting for 29 months and ongoing |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knetki-Wróblewska, M.; Wojas-Krawczyk, K.; Kowalski, D.M.; Krzakowski, M. Non-Small-Cell Lung Cancer Patients with Coexistence of High PD-L1 Expression and RET Fusion—Which Path Should We Follow? Case Reports and Literature Review. J. Clin. Med. 2022, 11, 1630. https://doi.org/10.3390/jcm11061630
Knetki-Wróblewska M, Wojas-Krawczyk K, Kowalski DM, Krzakowski M. Non-Small-Cell Lung Cancer Patients with Coexistence of High PD-L1 Expression and RET Fusion—Which Path Should We Follow? Case Reports and Literature Review. Journal of Clinical Medicine. 2022; 11(6):1630. https://doi.org/10.3390/jcm11061630
Chicago/Turabian StyleKnetki-Wróblewska, Magdalena, Kamila Wojas-Krawczyk, Dariusz M. Kowalski, and Maciej Krzakowski. 2022. "Non-Small-Cell Lung Cancer Patients with Coexistence of High PD-L1 Expression and RET Fusion—Which Path Should We Follow? Case Reports and Literature Review" Journal of Clinical Medicine 11, no. 6: 1630. https://doi.org/10.3390/jcm11061630
APA StyleKnetki-Wróblewska, M., Wojas-Krawczyk, K., Kowalski, D. M., & Krzakowski, M. (2022). Non-Small-Cell Lung Cancer Patients with Coexistence of High PD-L1 Expression and RET Fusion—Which Path Should We Follow? Case Reports and Literature Review. Journal of Clinical Medicine, 11(6), 1630. https://doi.org/10.3390/jcm11061630






