Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender
Abstract
1. Introduction
2. Methods
2.1. Materials
2.2. Definitions
2.3. Statistical Analysis
3. Results
3.1. General Characteristics at Baseline
3.2. Coronary Angiography and Procedural Indices
3.3. Procedure-Related Complications
3.4. Pharmacotherapy during the Procedure
3.5. Risk Factors for Procedural Death
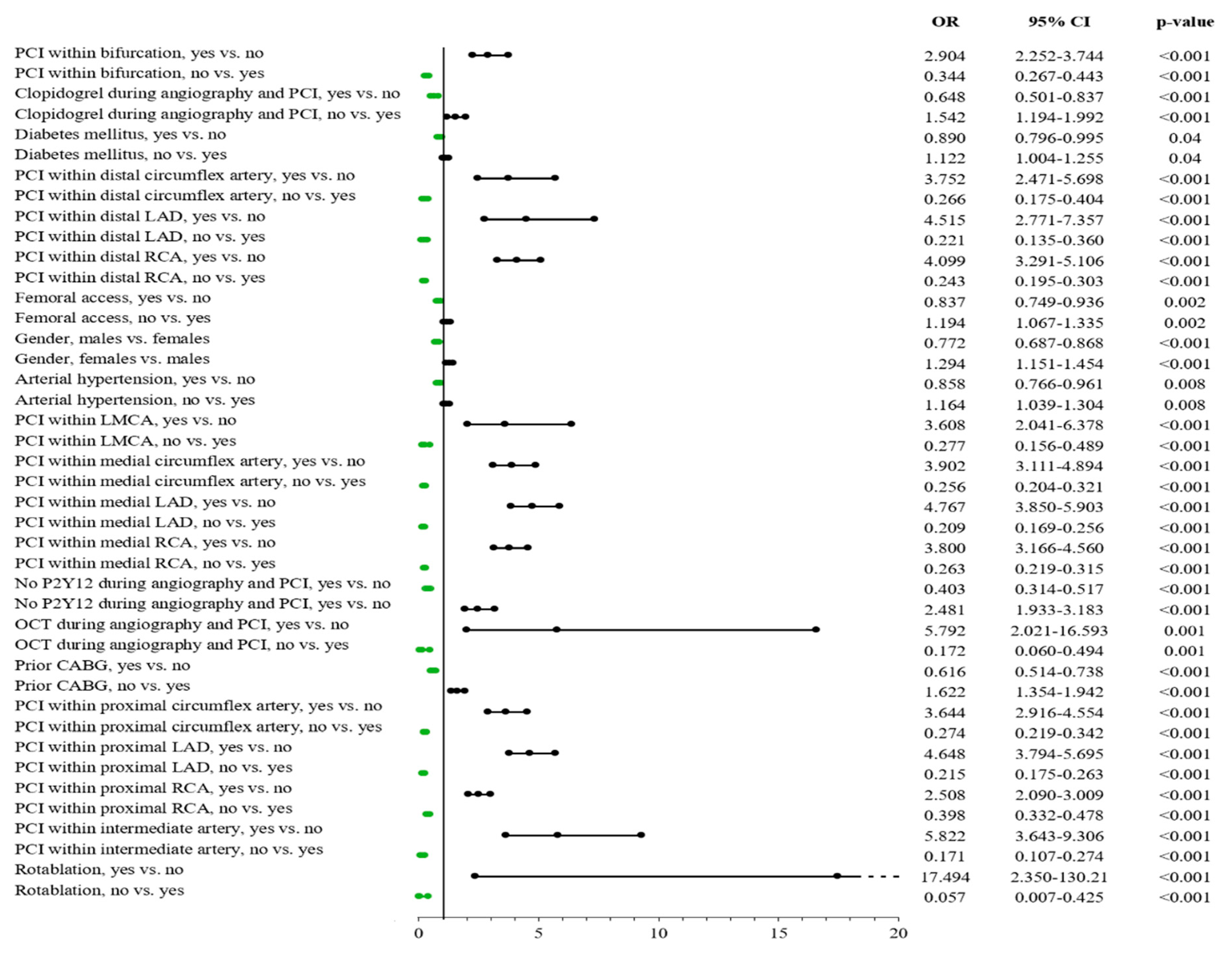
3.6. Risk Factors for Overall Periprocedural Complications
3.7. Predictors of Procedural Success
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Protty, M.; Sharp, A.S.P.; Gallagher, S.; Farooq, V.; Spratt, J.C.; Ludman, P.; Anderson, R.; McEntegart, M.M.; Hanratty, C.; Walsh, S.; et al. Defining Percutaneous Coronary Intervention Complexity and Risk: An Analysis of the United Kingdom BCIS Database 2006–2016. JACC Cardiovasc. Interv. 2022, 15, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Sabatowski, K.; Malinowski, K.P.; Siudak, Z.; Reczuch, K.; Dobrzycki, S.; Lesiak, M.; Hawranek, M.; Gil, R.J.; Witkowski, A.; Wojakowski, W.; et al. Sex-related differences and rotational atherectomy: Analysis of 5177 percu-taneous coronary interventions based on a large national registry from 2014 to 2020. Kardiol Pol. 2021, 79, 1320–1327. [Google Scholar] [CrossRef] [PubMed]
- Januszek, R.; Pawlik, A.; Staszczak, B.; Jędrychowska, M.; Bartuś, J.; Legutko, J.; Dudek, D.; Surdacki, A.; Bartuś, S. Age and gender differences in clinical outcomes of patients with heavy-calcified coronary artery lesions treated percutaneously with rotational atherectomy. Adv. Clin. Exp. Med. 2020, 29, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Pawlik, A.; Januszek, R.; Ruzsa, Z.; Óriás, V.; Kleczyński, P.; Wojtasik-Bakalarz, J.; Arif, S.; Nyerges, A.; Chyrchel, M.; Stanek, A.; et al. Gender differences and long-term clinical outcomes in patients with chronic total oc-clusions of infrainguinal lower limb arteries treated from retrograde access with peripheral vascular interventions. Adv. Med. Sci. 2020, 65, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Jędrychowska, M.; Januszek, R.; Plens, K.; Surdacki, A.; Bartuś, S.; Dudek, D. Impact of sex on the follow-up course and predictors of clinical outcomes in patients hospitalised due to myocardial infarction with non-obstructive coronary arteries: A single-centre experience. Kardiol. Pol. 2019, 77, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Wilson, W.; Smith, W.; McEntegart, M.; Oldroyd, K.; Sidik, N.; Bagnall, A.; Egred, M.; Irving, J.; Strange, J.; et al. Comparison of Characteristics and Complications in Men Versus Women Undergo-ing Chronic Total Occlusion Percutaneous Intervention. Am. J. Cardiol. 2017, 119, 535–541. [Google Scholar] [CrossRef]
- Cheney, A.; Kearney, K.E.; Lombardi, W. Sex-Based Differences in Chronic Total Occlusion Management. Curr. Atheroscler. Rep. 2018, 20, 60. [Google Scholar] [CrossRef]
- Wolff, R.; Fefer, P.; Knudtson, M.L.; Cheema, A.N.; Diane Galbraith, P.; Sparkes, J.D.; Wright, G.A.; Wijeysundera, H.C.; Strauss, B.H. Gender differences in the prevalence and treatment of coronary chronic total occlusions. Catheter. Cardiovasc. Interv. 2016, 87, 1063–1071. [Google Scholar] [CrossRef]
- Akodad, M.; Spaziano, M.; Garcia-Alonso, C.J.; Louvard, Y.; Sanguineti, F.; Garot, P.; Hovasse, T.; Unterseeh, T.; Unterseeh, B.; Lefèvre, T.; et al. Is sex associated with adverse outcomes after percutaneous coronary inter-vention for CTO? Int. J. Cardiol. 2019, 288, 29–33. [Google Scholar] [CrossRef]
- Flores-Umanzor, E.J.; Cepas-Guillén, P.L.; Caldentey, G.; Pérez-Fuentes, P.; Arévalos, V.; Ivey-Miranda, J.; Regueiro, A.; Freixa, X.; Brugaletta, S.; Farrero, M.; et al. Sex-based differences in chronic total occlusion management and long-term clinical outcomes. Int. J. Cardiol. 2020, 319, 46–51. [Google Scholar] [CrossRef]
- Pershad, A.; Gulati, M.; Karmpaliotis, D.; Moses, J.; Nicholson, W.J.; Nugent, K.; Tang, Y.; Sapontis, J.; Lombardi, W.; Grantham, J.A.; et al. A sex stratified outcome analysis from the OPEN-CTO registry. Catheter. Cardiovasc. Interv. 2019, 93, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Guelker, J.E.; Bansemir, L.; Ott, R.; Kuhr, K.; Koektuerk, B.; Turan, R.G.; Klues, H.G.; Bufe, A. Gender-based acute outcome in percutaneous coronary intervention of chronic total coronary occlusion. Neth. Hear. J. 2017, 25, 304–311. [Google Scholar] [CrossRef][Green Version]
- Karatasakis, A.; Iwnetu, R.; Danek, B.; Karmpaliotis, D.; Alaswad, K.; A Jaffer, F.; Yeh, R.W.; E Kandzari, D.; Lembo, N.J.; Patel, M.; et al. The Impact of Age and Sex on In-Hospital Outcomes of Chronic Total Occlusion Percutaneous Coronary Intervention. J. Invasive Cardiol. 2017, 59, 116–122. [Google Scholar]
- Toma, A.; Stähli, B.E.; Gick, M.; Ferenc, M.; Mashayekhi, K.; Buettner, H.J.; Neumann, F.-J.; Gebhard, C. Temporal changes in outcomes of women and men undergoing percutaneous coronary intervention for chronic total occlusion: 2005–2013. Clin. Res. Cardiol. 2018, 107, 449–459. [Google Scholar] [CrossRef]
- Daly, C.; Clemens, F.; Lopez Sendon, J.L.; Tavazzi, L.; Boersma, E.; Danchin, N.; Delahaye, F.; Gitt, A.; Julian, D.; Mulcahy, D.; et al. Euro Heart Survey Investigators. Gender Differences in the Management and Clinical Outcome of Stable Angina. Circulation 2006, 113, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Steg, P.G.; Greenlaw, N.; Tardif, J.C.; Tendera, M.; Ford, I.; Kääb, S.; Abergel, H.; Fox, K.M.; Ferrari, R. CLARIFY Registry Investigators. Women and men with stable coronary artery disease have similar clinical outcomes: Insights from the international prospective CLARIFY registry. Eur. Heart J. 2012, 33, 2831–2840. [Google Scholar] [CrossRef] [PubMed]
- Fefer, P.; Knudtson, M.L.; Cheema, A.N.; Galbraith, P.D.; Osherov, A.B.; Yalonetsky, S.; Gannot, S.; Samuel, M.; Weisbrod, M.; Bierstone, D.; et al. Current perspectives on coronary chronic total occlusion—The Canadian multi-center CTO registry. J. Am. Coll. Cardiol. 2012, 59, 991–997. [Google Scholar] [CrossRef]
- Brilakis, E.S.; Banerjee, S.; Karmpaliotis, D.; Lombardi, W.L.; Tsai, T.T.; Shunk, K.A.; Kennedy, K.F.; Spertus, J.A.; Holmes, D.R.; Grantham, J.A. Procedural outcomes of chronic total occlusion percutaneous coronary inter-vention. J. Am. Coll. Cardiol. Intv. 2015, 8, 245–253. [Google Scholar]
- Anderson, H.V.; Shaw, R.E.; Brindis, R.G.; Hewitt, K.; Krone, R.J.; Block, P.C.; McKay, C.R.; Weintraub, W.S. A contemporary overview of percutaneous coronary interventions. The Ameri-can College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). J. Am. Coll. Cardiol. 2002, 39, 1096–1103. [Google Scholar] [CrossRef]
- Januszek, R.; Bryniarski, L.; Siudak, Z.; Malinowski, K.P.; Bryniarski, K.L.; Surdacki, A.; Dziewierz, A.; Mika, P.; Wańha, W.; Wojakowski, W.; et al. Five-year report from the Polish national registry on percutaneous coronary interventions with a focus on coronary artery perforations within chronic total occlusions. Postepy Kardiol Interwencyjnej 2020, 16, 399–409. [Google Scholar] [CrossRef]
- Safley, D.M.; Koshy, S.; Grantham, J.A.; Bybee, K.A.; House, J.A.; Kennedy, K.F.; Rutherford, B.D. Changes in myocardial ischemic burden following percutaneous coronary inter-vention of chronic total occlusions. Catheter. Cardiovasc. Interv. 2011, 78, 337–343. [Google Scholar] [PubMed]
- Rossello, X.; Pujadas, S.; Serra, A.; Bajo, E.; Carreras, F.; Barros, A.; Cinca, J.; -Lladó, G.P.; Vaquerizo, B. Assessment of Inducible Myocardial Ischemia, Quality of Life, and Functional Status After Successful Percutaneous Revascularization in Patients with Chronic Total Coronary Occlusion. Am. J. Cardiol. 2015, 117, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Safley, D.M.; Grantham, J.A.; Hatch, J.; Ms, P.G.J.; Spertus, J.A. Quality of life benefits of percutaneous coronary intervention for chronic occlusions. Catheter. Cardiovasc. Interv. 2013, 84, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Azzalini, L.; Torregrossa, G.; Puskas, J.D.; Brilakis, E.S.; Lombardi, W.L.; Karmpaliotis, D.; Nakamura, S.; Colombo, A.; Carlino, M. Percutaneous revascularization of chronic total occlusions: Rationale, indications, techniques, and the cardiac surgeon’s point of view. Int. J. Cardiol. 2017, 231, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Farooq, V.; Serruys, P.W.; Garcia-Garcia, H.M.; Zhang, Y.; Bourantas, C.V.; Holmes, D.R.; Mack, M.; Feldman, T.; Morice, M.-C.; Ståhle, E.; et al. The negative impact of incomplete angiographic revascularization on clini-cal outcomes and its association with total occlusions: The SYNTAX (Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J. Am. Coll. Cardiol. 2013, 61, 282–294. [Google Scholar] [CrossRef]
- Azzalini, L.; Candilio, L.; Ojeda, S.; Dens, J.; La Manna, A.; Benincasa, S.; Bellini, B.; Hidalgo, F.; Chavarría, J.; Maeremans, J.; et al. Impact of Incomplete Revascularization on Long-Term Outcomes Following Chronic Total Occlusion Percutaneous Coronary Intervention. Am. J. Cardiol. 2018, 121, 1138–1148. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Christakopoulos, G.E.; Christopoulos, G.; Carlino, M.; Jeroudi, O.M.; Roesle, M.; Rangan, B.V.; Abdullah, S.; Grodin, J.; Kumbhani, D.J.; Vo, M.; et al. Meta-analysis of clinical outcomes of patients who underwent per-cutaneous coronary interventions for chronic total occlusions. Am. J. Cardiol. 2015, 115, 1367–1375. [Google Scholar] [CrossRef]
- Joyal, D.; Afilalo, J.; Rinfret, S. Effectiveness of recanalization of chronic total occlusions: A systematic review and meta-analysis. Am. Heart J. 2010, 160, 179–187. [Google Scholar] [CrossRef]
- Lee, P.H.; Lee, S.-W.; Park, H.-S.; Kang, S.H.; Bae, B.J.; Chang, M.; Roh, J.-H.; Yoon, S.-H.; Ahn, J.-M.; Park, D.-W.; et al. Successful Recanalization of Native Coronary Chronic Total Occlusion Is Not Associated with Improved Long-Term Survival. JACC: Cardiovasc. Interv. 2016, 9, 530–538. [Google Scholar] [CrossRef]
- Schnyder, G.; Sawhney, N.; Whisenant, B.; Tsimikas, S.; Turi, Z.G. Common femoral artery anatomy is influenced by demographics and comor-bidity: Implications for cardiac and peripheral invasive studies. Catheter. Cardiovasc. Interv. 2001, 53, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.R.; Sianos, G.; Werner, G.S.; Escaned, J.; Tomasello, S.D.; Boukhris, M.; Castaing, M.; Büttner, J.H.; Bufe, A.; Kalnins, A.; et al. Retrograde recanalization of chronic total occlusions in Europe: Procedural, in-hospital, and long-term outcomes from the multicenter ERCTO registry. J. Am. Coll. Cardiol. 2015, 65, 2388–2400. [Google Scholar] [CrossRef] [PubMed]
- Claessen, B.E.; Chieffo, A.; Dangas, G.D.; Godino, C.; Lee, S.-W.; Obunai, K.; Carlino, M.; Chantziara, V.; Apostolidou, I.; Henriques, J.P.S.; et al. Gender differences in long-term clinical outcomes after percutaneous coronary intervention of chronic total occlusions. J. Invasive Cardiol. 2012, 24, 484–488. [Google Scholar] [PubMed]



| Clinical Variables | Overall (%) N = 14,903 (100) | Men (%) N = 11,177 (75) | Women (%) N = 3726 (25) | p-Value |
|---|---|---|---|---|
| Age, years | 65.6 ± 9.8 | 64.6 ± 9.7 | 68.7 ± 9.2 | <0.001 |
| 66 (59 ÷ 72) | 65 (58 ÷ 71) | 68 (63 ÷ 75) | ||
| Weight, kg | 83.4 ± 15.8 | 86.2 ± 15.1 | 75 ± 15 | <0.001 |
| 82 (74 ÷ 92) | 85 (77.5 ÷ 95) | 75 (65 ÷ 83) | ||
| Arterial hypertension | 11,045 (73.9) | 8153 (72.9) | 2871 (77) | <0.001 |
| Diabetes mellitus | 3873 (25.9) | 2662 (23.8) | 1203 (32.3) | <0.001 |
| Prior stroke | 448 (3) | 326 (2.9) | 121 (3.2) | 0.3 |
| Prior MI | 7455 (49.9) | 5718 (51.2) | 1720 (46.2) | <0.001 |
| Prior PCI | 8409 (56.3) | 6435 (57.6) | 1956 (52.5) | <0.001 |
| Prior CABG | 1213 (8.1) | 974 (8.7) | 238 (6.4) | <0.001 |
| Smoking | 2654 (17.8) | 2169 (19.4) | 478 (12.8) | <0.001 |
| Psoriasis | 54 (0.36) | 42 (0.38) | 12 (0.32) | 0.63 |
| Kidney disease | 900 (6) | 631 (5.6) | 267 (7.2) | <0.001 |
| COPD | 354 (2.4) | 277 (2.5) | 75 (2) | 0.1 |
| Variable | Overall (%) N = 14,903 (100) | Men (%) N = 11,177 (75) | Women (%) N = 3726 (25) | p-Value |
|---|---|---|---|---|
| Vascular access | ||||
| Femoral | 2093 (24.5) | 1527 (24.2) | 563 (25.5) | 0.003 |
| Radial | 6383 (74.6) | 4752 (75.1) | 1613 (73.1) | |
| Other | 78 (0.9) | 46 (0.7) | 32 (1.4) | |
| Location of culprit lesion | ||||
| RCA | 6231 (41.7) | 4617 (41.3) | 1600 (42.9) | 0.08 |
| LMCA | 209 (1.4) | 146 (1.3) | 63 (1.7) | 0.08 |
| LAD | 4034 (27) | 2958 (26.5) | 1068 (28.7) | 0.009 |
| Cx | 2600 (17.4) | 1981 (17.7) | 610 (16.4) | 0.06 |
| Others | 1868 (12.5) | 1475 (13.2) | 385 (11.5) | <0.001 |
| Coronary angiography | ||||
| - SVD | 12,878 (86.2) | 9631 (86.2) | 3213 (86.2) | 0.09 |
| - MVD − LMCA | 903 (6) | 690 (6.2) | 211 (5.7) | |
| - MVD + LMCA | 151 (1) | 100 (0.9) | 51 (1.4) | |
| - Separate LMCA | 58 (0.39) | 46 (0.4) | 12 (0.3) | |
| - Others | 952 (6.4) | 710 (6.3) | 239 (6.4) | |
| TIMI grade after PCI | ||||
| - 0 | 4253 (28.5) | 3307 (29.7) | 940 (25.3) | <0.001 |
| - I | 373 (2.5) | 276 (2.5) | 96 (2.6) | |
| - II | 404 (2.7) | 300 (2.7) | 104 (2.8) | |
| - III | 9869 (66.2) | 7261 (65.2) | 2576 (69.3) | |
| Rotablation | 146 (0.98) | 115 (1.03) | 31 (0.83) | 0.29 |
| Bifurcation | 1134 (7.6) | 861 (7.7) | 267 (7.2) | 0.28 |
| FFR | 150 (1.7) | 110 (1.7) | 40 (1.8) | 0.82 |
| IVUS | 66 (0.8) | 46 (0.7) | 19 (0.9) | 0.53 |
| OCT | 15 (0.2) | 9 (0.1) | 6 (0.3) | 0.23 |
| Type of PCI | ||||
| Drug-eluting stent | 9006 (60.3) | 6631 (59.3) | 2352 (63.1) | <0.001 |
| Bare-metal stent | 200 (1.3) | 137 (1.2) | 63 (1.7) | 0.03 |
| BRS | 97 (0.6) | 75 (0.7) | 22 (0.6) | 0.6 |
| Implanted stent | 9265 (62) | 6818 (61) | 2424 (65.1) | <0.001 |
| Number of implanted stents | <0.001 | |||
| 0 | 5677 (38) | 4359 (39) | 1302 (34.9) | |
| 1 | 6950 (46.5) | 5096 (45.6) | 1837 (49.3) | |
| 2 | 1756 (11.7) | 1314 (11.8) | 437 (11.7) | |
| 3 | 498 (3.3) | 359 (3.2) | 139 (3.7) | |
| 4 | 56 (0.4) | 44 (0.4) | 11 (0.3) | |
| 5 | 4 (0.03) | 4 (0.04) | 0 (0) | |
| 6 | 1 (0.01) | 1 (0.01) | 0 (0) | |
| Number of implanted stents ≥2 | 2315 (15.5) | 1722 (15.4) | 587 (15.7) | 0.6 |
| Stent type | <0.001 | |||
| BMS alone | 176 (1.2) | 122 (1.1) | 54 (1.4) | |
| BVS alone | 82 (0.55) | 64 (0.57) | 18 (0.48) | |
| BVS + BMS | 1 (0.01) | 1 (0.01) | 0 (0) | |
| DES | 8969 (60) | 6607 (59.1) | 2339 (62.8) | |
| DES + BMS | 23 (0.15) | 14 (0.13) | 9 (0.24) | |
| DES + BVS | 14 (0.09) | 10 (0.09) | 14 (0.09) | |
| No stent used | 5677 (38) | 4359 (39) | 1302 (34.9) | |
| DEB | 208 (1.7) | 142 (1.5) | 65 (2.1) | 0.03 |
| Contrast dose, | 205.3 ± 102 | 209.4 ± 103.2 | 193.1 ± 97.6 | <0.001 |
| mL | 190 (140; 250) | 200 (150; 250) | 175 (130; 240) | |
| Radiation exposure, Gy | 1.53 ± 1.29 | 1.62 ± 1.33 | 1.24 ± 1.12 | <0.001 |
| 1.16 | 1.26 | 0.9 | ||
| (0.65; 2.01) | (0.71; 2.14) | (0.5;1.62) | ||
| Type of Complication | Overall (%) N = 14,903 (100) | Men (%) N = 11,177 (75) | Women (%) N = 3726 (25) | p-Value |
|---|---|---|---|---|
| All complications | 138 (2.67) | 82 (2.31) | 56 (3.45) | 0.02 |
| Death | 17 (0.3) | 6 (0.2) | 11 (0.7) | 0.006 |
| MI | 22 (0.4) | 13 (0.4) | 9 (0.6) | 0.36 |
| No-reflow | 36 (0.7) | 25 (0.7) | 11 (0.7) | 1.00 |
| Puncture-site bleeding | 11 (0.2) | 5 (0.1) | 6 (0.3) | 0.11 |
| Cardiac arrest | 27 (0.5) | 13 (0.4) | 14 (0.9) | 0.04 |
| Allergic reaction | 3 (0.1) | 1 (0.0) | 2 (0.1) | 0.23 |
| CAP | 45 (0.9) | 28 (0.8) | 17 (1.1) | 0.34 |
| Stroke | 0 (0) | 0 (0) | 0 (0) | - |
| CAD | 3 (0.2) | 3 (0.2) | 0 (0) | 0.56 |
| Type of Complication | Overall (%) n = 14,903 (100) | Men (%) n = 11,177 (75) | Women (%) n = 3726 (25) | p-Value |
|---|---|---|---|---|
| Acetyl-salicylic acid | 4563 (43.4) | 3349 (42.9) | 1193 (44.5) | 0.16 |
| Clopidogrel | 5078 (48.5) | 3697 (47.6) | 1361 (50.8) | 0.004 |
| Prasugrel | 48 (0.6) | 38 (0.6) | 10 (0.4) | 0.42 |
| Ticagrelor | 622 (7.1) | 468 (7.2) | 152 (6.8) | 0.47 |
| No P2Y12 during procedure | 4910 (46.1) | 3715 (46.9) | 1190 (43.9) | 0.006 |
| Unfractionated heparin | 12,931 (93.3) | 9697 (93.5) | 3198 (92.8) | 0.18 |
| LMWH | 696 (7.7) | 511 (7.7) | 185 (7.9) | 0.68 |
| GP IIb/IIIa | 203 (1.4) | 158 (1.4) | 45 (1.2) | 0.34 |
| Bivalirudin | 13 (0.1) | 9 (0.1) | 4 (0.2) | 0.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siudak, Z.; Bryniarski, L.; Malinowski, K.P.; Wańha, W.; Wojakowski, W.; Surowiec, S.; Balan, R.; Januszek, S.; Pawlik, A.; Siwiec, N.; et al. Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender. J. Clin. Med. 2022, 11, 1419. https://doi.org/10.3390/jcm11051419
Siudak Z, Bryniarski L, Malinowski KP, Wańha W, Wojakowski W, Surowiec S, Balan R, Januszek S, Pawlik A, Siwiec N, et al. Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender. Journal of Clinical Medicine. 2022; 11(5):1419. https://doi.org/10.3390/jcm11051419
Chicago/Turabian StyleSiudak, Zbigniew, Leszek Bryniarski, Krzysztof Piotr Malinowski, Wojciech Wańha, Wojciech Wojakowski, Sławomir Surowiec, Robert Balan, Sławomir Januszek, Artur Pawlik, Natalia Siwiec, and et al. 2022. "Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender" Journal of Clinical Medicine 11, no. 5: 1419. https://doi.org/10.3390/jcm11051419
APA StyleSiudak, Z., Bryniarski, L., Malinowski, K. P., Wańha, W., Wojakowski, W., Surowiec, S., Balan, R., Januszek, S., Pawlik, A., Siwiec, N., Bryniarski, K., Surdacki, A., Legutko, J., Bartuś, K., Bartuś, S., & Januszek, R. (2022). Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender. Journal of Clinical Medicine, 11(5), 1419. https://doi.org/10.3390/jcm11051419








