Individual Patterns and Temporal Trajectories of Changes in Fear and Pain during Exposure In Vivo: A Multiple Single-Case Experimental Design in Patients with Chronic Pain
Abstract
:1. Introduction
2. Materials and Methods
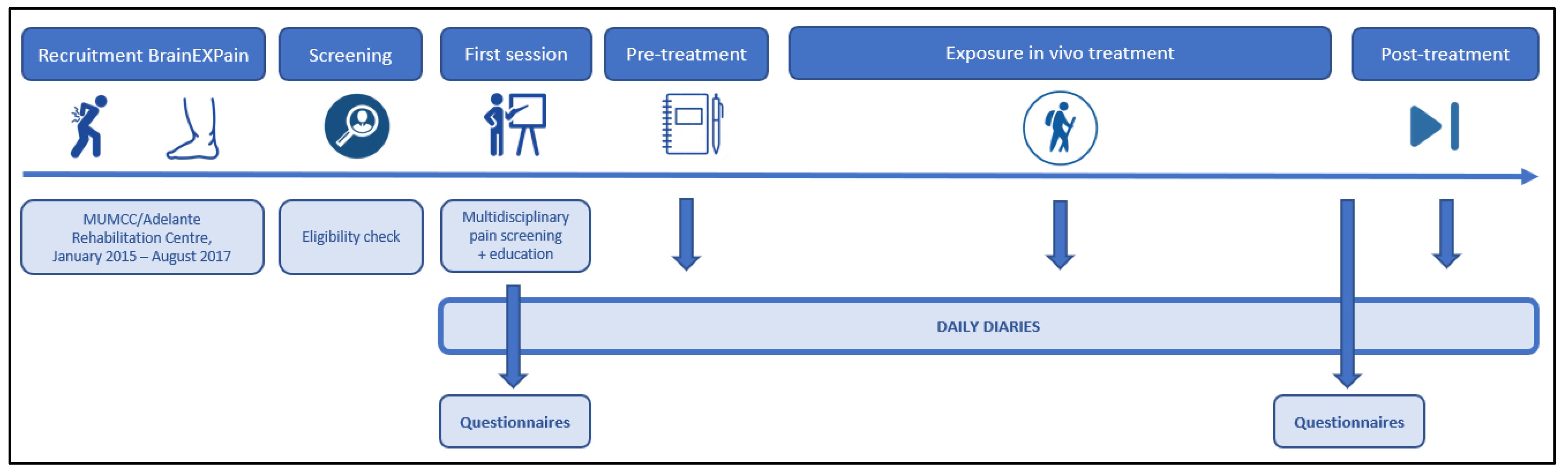
2.1. Study Design
2.2. Procedures
2.3. Participants
2.4. Exposure In Vivo Treatment
2.5. Outcomes
2.5.1. Daily Measures
2.5.2. Non-Daily Questionnaires
2.6. Statistical Analyses
- (1)
- Different phases were created to be used in a sliding window approach. We started comparing baseline data (phase A) with all intervention and post-intervention data (Phase B + C). Afterwards, we systematically added one week to phase A to obtain a timeline for treatment effects (e.g., Phase A + 1w), until phase B consists of less than five measurements.
- (2)
- The time to reach the minimal clinically important difference (MCID) was scrutinized. To unravel the relevance of EXP to patient care, it is useful to not only focus on statistically significant changes, but also on clinically important differences. Even if the statistical result is not significant, the patient might still feel meaningful pain relief or physical improvement due to treatment. A reduction of 30% in pain intensity on a 11-point numeric rating scale has been considered as a MCID in chronic pain populations [46,47]. Therefore, the 30% cut-off value, starting from the baseline average, for pain intensity and for pain-related fear was calculated for each patient. The moment the patient scored lower than this value for at least three consecutive days, was considered as the point of MCID.
- (3)
- Individual visual graphs and descriptive values were explored to divide the patients into clusters based on their response to EXP. Patterns in temporal changes were analysed within these clusters and compared to the results of the sliding window approach, the time to reach the MCID and the differences between baseline and post-intervention questionnaires.
3. Results
3.1. Participant Characteristics
3.2. Treatment Characteristics
3.3. Diary Completion
3.4. Multi-Level Modelling of Daily Diary Outcomes
3.5. Descriptive and One-Level Analyses of Daily Diary Outcomes
3.6. Time to Reach the Minimal Clinically Important Differences (MCID)
3.7. Visual Inspection of Clusters in Single Cases
- Cluster 1: Quick decrease in fear, pain follows
- Cluster 2: Decrease in fear, pain unaffected
- Cluster 3: Late effect in fear
- Cluster 4: No clear effect
3.8. Non-Daily Questionnaires
3.9. Moderating Factors of Treatment Efficacy
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miller, R.M.; Kaiser, R.S. Psychological Characteristics of Chronic Pain: A Review of Current Evidence and Assessment Tools to Enhance Treatment. Curr. Pain Headache Rep. 2018, 22, 22. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef] [Green Version]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.; Karoly, P. Fear-avoidance model of chronic pain: The next generation. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zale, E.L.; Lange, K.L.; Fields, S.A.; Ditre, J.W. The relation between pain-related fear and disability: A meta-analysis. J. Pain 2013, 14, 1019–1030. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Calderon, J.; Flores-Cortes, M.; Morales-Asencio, J.M.; Luque-Suarez, A. Pain-Related Fear, Pain Intensity and Function in Individuals With Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1394–1415. [Google Scholar] [CrossRef] [Green Version]
- Luque-Suarez, A.; Martinez-Calderon, J.; Falla, D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: A systematic review. Br. J. Sports Med. 2019, 53, 554–559. [Google Scholar] [CrossRef] [Green Version]
- Crombez, G.; Vlaeyen, J.W.; Heuts, P.H.; Lysens, R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain 1999, 80, 329–339. [Google Scholar] [CrossRef]
- Wertli, M.M.; Rasmussen-Barr, E.; Weiser, S.; Bachmann, L.M.; Brunner, F. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: A systematic review. Spine J. 2014, 14, 816–836. [Google Scholar] [CrossRef]
- Marshall, P.W.M.; Schabrun, S.; Knox, M.F. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS ONE 2017, 12, e0180788. [Google Scholar] [CrossRef]
- Bean, D.J.; Johnson, M.H.; Heiss-Dunlop, W.; Lee, A.C.; Kydd, R.R. Do psychological factors influence recovery from complex regional pain syndrome type 1? A prospective study. Pain 2015, 156, 2310–2318. [Google Scholar] [CrossRef]
- De Jong, J.R.; Vlaeyen, J.W.; de Gelder, J.M.; Patijn, J. Pain-related fear, perceived harmfulness of activities, and functional limitations in complex regional pain syndrome type I. J. Pain 2011, 12, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Bean, D.J.; Johnson, M.H.; Kydd, R.R. Relationships between psychological factors, pain, and disability in complex regional pain syndrome and low back pain. Clin. J. Pain 2014, 30, 647–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vlaeyen, J.W.; Morley, S.; Linton, S.J.; Boersma, K.; de Jong, J. Pain-Related Fear: Exposure-Based Treatment of Chronic Pain; IASP Press: Malaga, Spain, 2012. [Google Scholar]
- Vlaeyen, J.W.S.; Crombez, G. Behavioral Conceptualization and Treatment of Chronic Pain. Annu. Rev. Clin. Psychol. 2020, 16, 187–212. [Google Scholar] [CrossRef] [PubMed]
- Woods, M.P.; Asmundson, G.J.G. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: A randomized controlled clinical trial. Pain 2008, 136, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Leeuw, M.; Goossens, M.; van Breukelen, G.J.P.; de Jong, J.R.; Heuts, P.; Smeets, R.; Köke, A.J.A.; Vlaeyen, J.W.S. Exposure in vivo versus operant graded activity in chronic low back pain patients: Results of a randomized controlled trial. Pain 2008, 138, 192–207. [Google Scholar] [CrossRef]
- Glombiewski, J.A.; Holzapfel, S.; Riecke, J.; Vlaeyen, J.W.S.; de Jong, J.; Lemmer, G.; Rief, W. Exposure and CBT for chronic back pain: An RCT on differential efficacy and optimal length of treatment. J. Consult. Clin. Psychol. 2018, 86, 533–545. [Google Scholar] [CrossRef]
- De Jong, J.R.; Vlaeyen, J.W.S.; Onghena, P.; Cuypers, C.; den Hollander, M.; Ruijgrok, J. Reduction of pain-related fear in complex regional pain syndrome type I: The application of graded exposure In Vivo. Pain 2005, 116, 264–275. [Google Scholar] [CrossRef]
- Den Hollander, M.; Goossens, M.; de Jong, J.; Ruijgrok, J.; Oosterhof, J.; Onghena, P.; Smeets, R.; Vlaeyen, J.W.S. Expose or protect? A randomized controlled trial of exposure in vivo vs pain-contingent treatment as usual in patients with complex regional pain syndrome type 1. Pain 2016, 157, 2318–2329. [Google Scholar] [CrossRef]
- De Jong, J.R.; Vlaeyen, J.W.S.; van Eijsden, M.; Loo, C.; Onghena, P. Reduction of pain-related fear and increased function and participation in work-related upper extremity pain (WRUEP): Effects of exposure In Vivo. Pain 2012, 153, 2109–2118. [Google Scholar] [CrossRef]
- Dekker, C.; Goossens, M.; Winkens, B.; Remerie, S.; Bastiaenen, C.; Verbunt, J. Functional Disability in Adolescents with Chronic Pain: Comparing an Interdisciplinary Exposure Program to Usual Care. Children 2020, 7, 288. [Google Scholar] [CrossRef]
- Timmers, I.; van de Ven, V.; Vlaeyen, J.W.S.; Smeets, R.J.; Verbunt, J.A.; de Jong, J.R.; Kaas, A.L. Cortico-Limbic Circuitry in Chronic Pain Tracks Pain Intensity Relief Following Exposure In Vivo. Biol. Psychiatry Glob. Open Sci. 2021, 1, 28–36. [Google Scholar] [CrossRef]
- Labrenz, F.; Icenhour, A.; Schlamann, M.; Forsting, M.; Bingel, U.; Elsenbruch, S. From Pavlov to pain: How predictability affects the anticipation and processing of visceral pain in a fear conditioning paradigm. NeuroImage 2016, 130, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Gheldof, E.L.; Crombez, G.; Van den Bussche, E.; Vinck, J.; Van Nieuwenhuyse, A.; Moens, G.; Mairiaux, P.; Vlaeyen, J.W. Pain-related fear predicts disability, but not pain severity: A path analytic approach of the fear-avoidance model. Eur. J. Pain 2010, 14, e871–e879. [Google Scholar] [CrossRef] [Green Version]
- Onghena, P.; Edgington, E.S. Customization of pain treatments: Single-case design and analysis. Clin. J. Pain 2005, 21, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Timmers, I.; de Jong, J.R.; Goossens, M.; Verbunt, J.A.; Smeets, R.J.; Kaas, A.L. Exposure in vivo Induced Changes in Neural Circuitry for Pain-Related Fear: A Longitudinal fMRI Study in Chronic Low Back Pain. Front. Neurosci. 2019, 13, 970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harden, N.R.; Bruehl, S.; Perez, R.S.G.M.; Birklein, F.; Marinus, J.; Maihofner, C.; Lubenow, T.; Buvanendran, A.; Mackey, S.; Graciosa, J.; et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain 2010, 150, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Derogatis, L.R.; Unger, R. Symptom checklist-90-revised. Corsini Encycl. Psychol. 2010, 1–2. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; den Hollander, M.; de Jong, J.; Simons, L. Exposure In Vivo for pain-related fear. In Psychological Approaches to Pain Management, 3rd ed.; Turk, D., Gatchel, R., Eds.; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Trost, Z.; France, C.R.; Thomas, J.S. Examination of the photograph series of daily activities (PHODA) scale in chronic low back pain patients with high and low kinesiophobia. Pain 2009, 141, 276–282. [Google Scholar] [CrossRef]
- Hollander, M.D.; de Jong, J.; Onghena, P.; Vlaeyen, J.W.S. Generalization of exposure in vivo in Complex Regional Pain Syndrome type I. Behav. Res. 2020, 124, 103511. [Google Scholar] [CrossRef]
- Tait, R.C.; Pollard, C.A.; Margolis, R.B.; Duckro, P.N.; Krause, S.J. The Pain Disability Index: Psychometric and validity data. Arch. Phys. Med. Rehabil. 1987, 68, 438–441. [Google Scholar]
- Leeuw, M.; Goossens, M.E.; van Breukelen, G.J.; Boersma, K.; Vlaeyen, J.W. Measuring perceived harmfulness of physical activities in patients with chronic low back pain: The Photograph Series of Daily Activities-short electronic version. J. Pain 2007, 8, 840–849. [Google Scholar] [CrossRef] [PubMed]
- Dubbers, A.T.; Vikström, M.H.; Jong, J.D. The Photograph Series of Daily Activities (PHODA-UE): Cervical Spine and Shoulder, CD-Rom Version 1.2; Zuyd University, Institute for Rehabilitation Research (iRv), Maastricht University: Heerlen/Maastricht, The Netherlands, 2003. [Google Scholar]
- Jelinek, S.; Germes, D.; Leyckes, N.; de Jong, J.R. The Photograph Series of Daily Activities (PHODA-LE): Lower Extremities, CD-Rom Version 1.2; Zuyd University, Institute for Rehabilitation Research (iRv), Maastricht University: Heerlen/Maastricht, The Netherlands, 2003. [Google Scholar]
- Miller, R.; Kori, S.; Todd, D. The tampa scale for kinisophobia. Clin. J. Pain 1991, 7, 51. [Google Scholar] [CrossRef]
- Van Damme, S.; Crombez, G.; Bijttebier, P.; Goubert, L.; Van Houdenhove, B. A confirmatory factor analysis of the Pain Catastrophizing Scale: Invariant factor structure across clinical and non-clinical populations. Pain 2002, 96, 319–324. [Google Scholar] [CrossRef]
- Snaith, R.P. The Hospital Anxiety And Depression Scale. Health Qual. Life Outcomes 2003, 1, 29. [Google Scholar] [CrossRef] [Green Version]
- Melzack, R. The short-form McGill Pain Questionnaire. Pain 1987, 30, 191–197. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Hjermstad, M.J.; Fayers, P.M.; Haugen, D.F.; Caraceni, A.; Hanks, G.W.; Loge, J.H.; Fainsinger, R.; Aass, N.; Kaasa, S. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: A systematic literature review. J. Pain Symptom. Manag. 2011, 41, 1073–1093. [Google Scholar] [CrossRef]
- Declercq, L.; Cools, W.; Beretvas, S.N.; Moeyaert, M.; Ferron, J.M.; Van den Noortgate, W. MultiSCED: A tool for (meta-)analyzing single-case experimental data with multilevel modeling. Behav. Res. Methods 2020, 52, 177–192. [Google Scholar] [CrossRef] [Green Version]
- Moeyaert, M.; Manolov, R.; Rodabaugh, E. Meta-Analysis of Single-Case Research via Multilevel Models: Fundamental Concepts and Methodological Considerations. Behav. Modif. 2020, 44, 265–295. [Google Scholar] [CrossRef]
- De, T.K.; Michiels, B.; Tanious, R.; Onghena, P. Handling missing data in randomization tests for single-case experiments: A simulation study. Behav. Res. Methods 2020, 52, 1355–1370. [Google Scholar] [CrossRef]
- Edgington, E.; Onghena, P. Randomization Tests; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Rowbotham, M.C. What is a “clinically meaningful” reduction in pain? Pain 2001, 94, 131–132. [Google Scholar] [CrossRef]
- Farrar, J.T.; Young, J.P., Jr.; LaMoreaux, L.; Werth, J.L.; Poole, R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.; de Jong, J.; Geilen, M.; Heuts, P.H.; van Breukelen, G. Graded exposure in vivo in the treatment of pain-related fear: A replicated single-case experimental design in four patients with chronic low back pain. Behav. Res. 2001, 39, 151–166. [Google Scholar] [CrossRef]
- Volders, S.; Boddez, Y.; De Peuter, S.; Meulders, A.; Vlaeyen, J.W.S. Avoidance behavior in chronic pain research: A cold case revisited. Behav. Res. 2015, 64, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D.J.; Northoff, G. Common brain activations for painful and non-painful aversive stimuli. BMC Neurosci. 2012, 13, 60. [Google Scholar] [CrossRef] [Green Version]
- Vogt, B.A. Pain and emotion interactions in subregions of the cingulate gyrus. Nat. Rev. Neurosci. 2005, 6, 533–544. [Google Scholar] [CrossRef] [Green Version]
- Elman, I.; Borsook, D. Threat Response System: Parallel Brain Processes in Pain vis-à-vis Fear and Anxiety. Front. Psychiatry 2018, 9, 29. [Google Scholar] [CrossRef] [Green Version]
- Ochsner, K.N.; Ludlow, D.H.; Knierim, K.; Hanelin, J.; Ramachandran, T.; Glover, G.C.; Mackey, S.C. Neural correlates of individual differences in pain-related fear and anxiety. Pain 2006, 120, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Sambuco, N.; Costa, V.D.; Lang, P.J.; Bradley, M.M. Assessing the role of the amygdala in fear of pain: Neural activation under threat of shock. J. Affect. Disord. 2020, 276, 1142–1148. [Google Scholar] [CrossRef]
- Biggs, E.E.; Timmers, I.; Meulders, A.; Vlaeyen, J.W.S.; Goebel, R.; Kaas, A.L. The neural correlates of pain-related fear: A meta-analysis comparing fear conditioning studies using painful and non-painful stimuli. Neurosci. Biobehav. Rev. 2020, 119, 52–65. [Google Scholar] [CrossRef]
- Uddin, L.Q.; Nomi, J.S.; Hébert-Seropian, B.; Ghaziri, J.; Boucher, O. Structure and Function of the Human Insula. J. Clin. Neurophysiol. 2017, 34, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Ong, W.-Y.; Stohler, C.S.; Herr, D.R. Role of the Prefrontal Cortex in Pain Processing. Mol. Neurobiol. 2019, 56, 1137–1166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merskey, H.; Bogduk, N. Part III pain terms, a current list with definitions and notes on usage. In Classification of Chronic Pain, 2nd ed.; IASP Press: Seattle, DC, USA, 1994; pp. 207–214. [Google Scholar]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Gilam, G.; Gross, J.J.; Wager, T.D.; Keefe, F.J.; Mackey, S.C. What Is the Relationship between Pain and Emotion? Bridging Constructs and Communities. Neuron 2020, 107, 17–21. [Google Scholar] [CrossRef]
- Simons, L.E.; Vlaeyen, J.W.S.; Declercq, L.; Smith, A.M.; Beebe, J.; Hogan, M.; Li, E.; Kronman, C.A.; Mahmud, F.; Corey, J.R.; et al. Avoid or engage? Outcomes of graded exposure in youth with chronic pain using a sequential replicated single-case randomized design. Pain 2020, 161, 520–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, L.; Hendrick, P.A. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur. J. Pain 2019, 23, 234–249. [Google Scholar] [CrossRef]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults with Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef]
- Marques, A.A.; Bevilaqua, M.C.d.N.; da Fonseca, A.M.P.; Nardi, A.E.; Thuret, S.; Dias, G.P. Gender Differences in the Neurobiology of Anxiety: Focus on Adult Hippocampal Neurogenesis. Neural Plast. 2016, 2016, 5026713. [Google Scholar] [CrossRef] [Green Version]
- Vlaeyen, J.W.S.; de Jong, J.; Geilen, M.; Heuts, P.H.T.G.; van Breukelen, G. The Treatment of Fear of Movement/(Re)injury in Chronic Low Back Pain: Further Evidence on the Effectiveness of Exposure In Vivo. Clin. J. Pain 2002, 18, 251–261. [Google Scholar] [CrossRef]
- Ells, L.J.; Lang, R.; Shield, J.P.; Wilkinson, J.R.; Lidstone, J.S.; Coulton, S.; Summerbell, C.D. Obesity and disability-a short review. Obes. Rev. 2006, 7, 341–345. [Google Scholar] [CrossRef]
- Wasser, J.G.; Vasilopoulos, T.; Zdziarski, L.A.; Vincent, H.K. Exercise Benefits for Chronic Low Back Pain in Overweight and Obese Individuals. PM R 2017, 9, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Narouze, S.; Souzdalnitski, D. Obesity and chronic pain: Systematic review of prevalence and implications for pain practice. Reg. Anesth. Pain Med. 2015, 40, 91–111. [Google Scholar] [CrossRef] [PubMed]
- Shadish, W.R.; Sullivan, K.J. Characteristics of single-case designs used to assess intervention effects in 2008. Behav. Res. Methods 2011, 43, 971–980. [Google Scholar] [CrossRef] [PubMed] [Green Version]



 pre–post effect (p < 0.05);
pre–post effect (p < 0.05);  change in trend (p < 0.05);
change in trend (p < 0.05);  non-significant change;
non-significant change;  end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
 pre–post effect (p < 0.05);
pre–post effect (p < 0.05);  change in trend (p < 0.05);
change in trend (p < 0.05);  non-significant change;
non-significant change;  end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
 pre-post effect (p < 0.05);
pre-post effect (p < 0.05);  change in trend (p < 0.05);
change in trend (p < 0.05);  non-significant change;
non-significant change;  end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
 pre-post effect (p < 0.05);
pre-post effect (p < 0.05);  change in trend (p < 0.05);
change in trend (p < 0.05);  non-significant change;
non-significant change;  end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.
end of EXP. Note. A light blue box means the trend of scores before that specific week was significantly different than the trend of scores after this point. A white box after a light blue box means that that week no big changes occurred anymore.


| Topic | Question | Scale |
|---|---|---|
| Pain-related fear | “How threatening would it be for you to perform this activity at this moment?” (one question for each of the three tailored activities) | 0 = not at all–100 = very |
| Pain intensity | “How intense is your pain at this moment?” “How intense was your most intense pain during the last 24 h?” “How intense was your least intense pain during the last 24 h?” | 0 = not at all–100 = worst imaginable |
| Case | Population | Age | Sex (% M) | BMI | Duration Complaints (Total = Median) | Average Pain Score | PDI | PHODA |
|---|---|---|---|---|---|---|---|---|
| C01 | CRPS LE | 43 | M | 27.47 | 3–6 m | 6.4 | 34 | 45.00 |
| C02 | CLBP | 55 | F | 26.29 | >5 y | 5 | 28 | 49.43 |
| C03 | CLBP | 41 | F | 25.71 | 2–5 y | 6.8 | 50 | 61.30 |
| C04 | CRPS UE | 28 | M | 24.22 | 1–2 y | 7.6 | 57 | 73.00 |
| C05 | CLBP | 35 | M | 28.40 | 2–5 y | 3.4 | 7 | 18.28 |
| C06 | CLBP | 36 | M | 28.70 | 6–12 m | 7 | 48 | 43.38 |
| C07 | CLBP | 28 | F | 25.00 | 2–5 y | 3.8 | 41 | 40.25 |
| C08 | CLBP | 23 | M | 22.64 | >5 y | 7.6 | 45 | 71.15 |
| C09 | CLBP | 37 | M | 20.28 | 2–5 y | 4 | 19 | 28.20 |
| C10 | CLBP | 53 | M | 26.85 | 2–5 y | 5.8 | 39 | 65.35 |
| C11 | CLBP | 32 | M | 29.39 | 1–2 y | 5.6 | 38 | 35.38 |
| C12 | CLBP | 57 | M | 25.00 | 2–5 y | 4.6 | 49 | 71.28 |
| C13 | CLBP | 52 | M | 30.76 | 1–2 y | 5.2 | 35 | 40.55 |
| C14 | CLBP | 40 | M | 29.39 | >5 y | 3.6 | 19 | 54.00 |
| C15 | CRPS LE | 33 | F | 27.76 | 6–12 m | 6.2 | 42 | 47.95 |
| C16 | CLBP | 44 | M | 27.93 | >5 y | 0 | 57 | 70.40 |
| C17 | CRPS LE | 62 | F | 31.99 | >5 y | 6.4 | 44 | 83.88 |
| C18 | CRPS LE | 27 | F | 24.81 | 2–5 y | 3.6 | 35 | 7.28 |
| C19 | CRPS UE | 34 | F | 44.63 | 3–6 m | 8.4 | 49 | 72.17 |
| C20 | CRPS LE | 29 | F | 37.11 | 1–2 y | 8 | 29 | 25.25 |
| Mean CLBP | 13 | 41 | 77% | 27 | 2–5 y | 5 | 37 | 50 |
| Mean CRPS | 7 | 37 | 29% | 31 | 1–2 y | 7 | 41 | 51 |
| Overall mean | 20 | 39 | 60% | 28 | 2–5 y | 5 | 38 | 50 |
| Case | Duration Baseline | Duration EXP | Duration Post-Intervention | |||
|---|---|---|---|---|---|---|
| Duration (Days) | Measurements | Duration (Days (Weeks)) | Completion (%) | Duration (Days) | Completion (%) | |
| C01 | 23 | 12 | 94 (14) | 100 | 19 | 100 |
| C02 | 9 | 9 | 72 (11) | 90 | 12 | 61 |
| C03 | 34 | 9 | 47 (7) | 64 | 17 | 56 |
| C04 | 33 | 10 | 66 (10) | 41 | 19 | 61 |
| C05 | 7 | 7 | 30 (5) | 67 | 0 | - |
| C06 | 33 | 10 | 29 (5) | 79 | 9 | 89 |
| C07 | 26 | 5 | 59 (9) | 66 | 0 | - |
| C08 | 35 | 6 | 43 (7) | 53 | 0 | - |
| C09 | 27 | 11 | 37 (6) | 97 | 7 | 89 |
| C10 | 34 | 11 | 66 (10) | 55 | 4 | 56 |
| C11 | 47 | 11 | 45 (7) | 56 | 0 | - |
| C12 | 42 | 11 | 51 (8) | 64 | 0 | - |
| C13 | 93 | 10 | 57 (9) | 88 | 7 | 86 |
| C14 | 31 | 5 | 52 (8) | 88 | 0 | - |
| C15 | 9 | 9 | 96 (14) | 81 | 0 | - |
| C16 | 41 | 5 | 57 (9) | 81 | 0 | - |
| C17 | 52 | 3 | 92 (14) | 89 | 12 | 100 |
| C18 | 29 | 9 | 57 (9) | 81 | 0 | - |
| C19 | 113 | 10 | 52 (8) | 51 | 0 | - |
| C20 | 65 | 9 | 57 (9) | 59 | 0 | - |
| Average | 39.15 | 8.60 | 57.95 (8.95) | 72.50 | 5.30 | 77.55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bontinck, J.; den Hollander, M.; Kaas, A.L.; De Jong, J.R.; Timmers, I. Individual Patterns and Temporal Trajectories of Changes in Fear and Pain during Exposure In Vivo: A Multiple Single-Case Experimental Design in Patients with Chronic Pain. J. Clin. Med. 2022, 11, 1360. https://doi.org/10.3390/jcm11051360
Bontinck J, den Hollander M, Kaas AL, De Jong JR, Timmers I. Individual Patterns and Temporal Trajectories of Changes in Fear and Pain during Exposure In Vivo: A Multiple Single-Case Experimental Design in Patients with Chronic Pain. Journal of Clinical Medicine. 2022; 11(5):1360. https://doi.org/10.3390/jcm11051360
Chicago/Turabian StyleBontinck, Jente, Marlies den Hollander, Amanda L. Kaas, Jeroen R. De Jong, and Inge Timmers. 2022. "Individual Patterns and Temporal Trajectories of Changes in Fear and Pain during Exposure In Vivo: A Multiple Single-Case Experimental Design in Patients with Chronic Pain" Journal of Clinical Medicine 11, no. 5: 1360. https://doi.org/10.3390/jcm11051360
APA StyleBontinck, J., den Hollander, M., Kaas, A. L., De Jong, J. R., & Timmers, I. (2022). Individual Patterns and Temporal Trajectories of Changes in Fear and Pain during Exposure In Vivo: A Multiple Single-Case Experimental Design in Patients with Chronic Pain. Journal of Clinical Medicine, 11(5), 1360. https://doi.org/10.3390/jcm11051360






