A Better Cardiopulmonary Fitness Is Associated with Improved Concentration Level and Health-Related Quality of Life in Primary School Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Anthropometrics
2.3. Physical Fitness Assessment
2.4. Concentration
2.5. Health-Related Quality of Life
2.6. Data Analysis
3. Results
3.1. Analysis of Descriptive Statistics and Sex Differences
3.2. Analysis of Descriptive Statistics and Weight Class Differences
3.3. Analysis of Descriptive Statistics and Differences between Age Groups in Boys and Girls
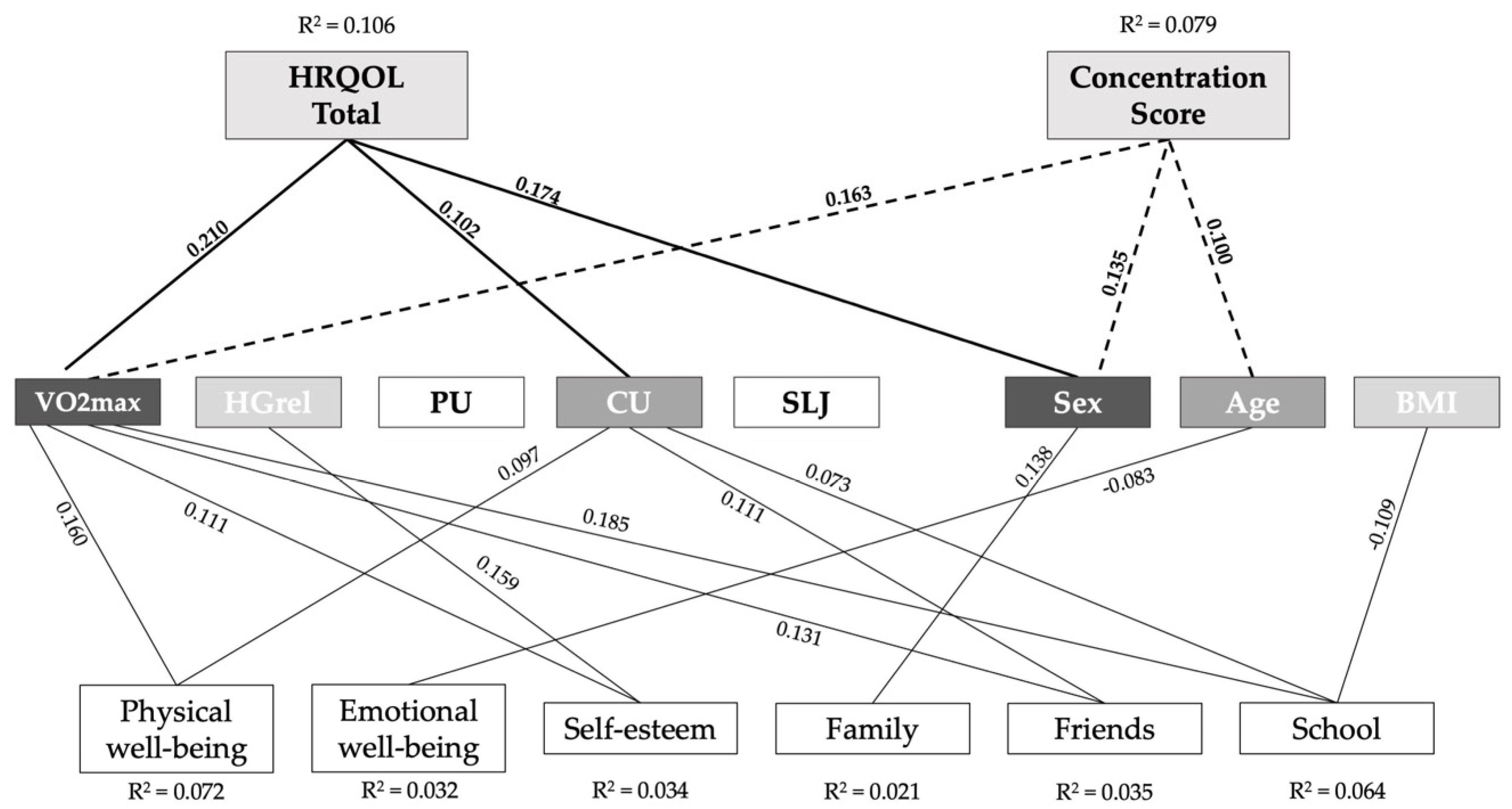
3.4. Association between Physical Fitness, Concentration, and HRQOL in a Subcohort of 9- to 10- Year-Old Children
4. Discussion
- Boys scored significantly better in estimatedVO2max, HG, SLJ, and PU throughout nearly all age groups;
- Girls showed better concentration scores in the d2-R total score and a better overall HRQOL than boys, independent of age;
- Estimated VO2max is the strongest predictor for higher concentration levels and a better overall HRQOL.
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Council, N.R. Children’s Health, the Nation’s Wealth: Assessing and Improving Child Health; National Academic Press: Washington, DC, USA, 2004. [Google Scholar]
- Lona, G.; Hauser, C.; Köchli, S.; Infanger, D.; Endes, K.; Faude, O.; Hanssen, H. Changes in physical activity behavior and development of cardiovascular risk in children. Scand. J. Med. Sci. Sports 2021, 31, 1313–1323. [Google Scholar] [CrossRef] [PubMed]
- Velde, G.T.; Plasqui, G.; Willeboordse, M.; Winkens, B.; Vreugdenhil, A. Associations between physical activity, sedentary time and cardiovascular risk factors among Dutch children. PLoS ONE 2021, 16, e0256448. [Google Scholar] [CrossRef]
- Barker, A.R.; Gracia-Marco, L.; Ruiz, J.R.; Castillo, M.J.; Aparicio-Ugarriza, R.; González-Gross, M.; Kafatos, A.; Androutsos, O.; Polito, A.; Molnar, D.; et al. Physical activity, sedentary time, TV viewing, physical fitness and cardiovascular disease risk in adolescents: The HELENA study. Int. J. Cardiol. 2018, 254, 303–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, B.; Kobel, S.; Wartha, O.; Kettner, S.; Dreyhaupt, J.; Steinacker, J.M. High sedentary time in children is not only due to screen media use: A cross-sectional study. BMC Pediatr. 2019, 19, 154. [Google Scholar] [CrossRef] [PubMed]
- Kobel, S.; Wartha, O.; Dreyhaupt, J.; Kettner, S.; Steinacker, J.M. Cross-sectional associations of objectively assessed sleep duration with physical activity, BMI and television viewing in German primary school children. BMC Pediatr. 2019, 19, 54. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Mouratidou, T.; Börnhorst, C.; Peplies, J.; De Henauw, S.; Marild, S.; Molnár, D.; Siani, A.; Tornaritis, M.; Veidebaum, T.; et al. Food consumption and cardiovascular risk factors in European children: The IDEFICS study. Pediatr. Obes. 2012, 8, 225–236. [Google Scholar] [CrossRef]
- Steene-Johannessen, J.; Hansen, B.H.; Dalene, K.E.; Kolle, E.; Northstone, K.; Møller, N.C.; Grøntved, A.; Wedderkopp, N.; Kriemler, S.; Page, A.S.; et al. Variations in accelerometry measured physical activity and sedentary time across Europe—Harmonized analyses of 47,497 children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 38. [Google Scholar] [CrossRef] [Green Version]
- Guthold, R.; Cowan, M.J.; Autenrieth, C.S.; Kann, L.; Riley, L.M. Physical Activity and Sedentary Behavior Among Schoolchildren: A 34-Country Comparison. J. Pediatr. 2010, 157, 43–49.e1. [Google Scholar] [CrossRef]
- Finger, J.D.; Varnaccia, G.; Borrmann, A.; Lange, C.; Mensink, G. Physical activity among children and adolescents in Germany. Results of the cross-sectional KiGGS Wave 2 study and trends. J. Health Monit. 2018, 3, 23–30. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Poethko-Müller, C.; Kuntz, B.; Lampert, T.; Neuhauser, H. The general health of children and adolescents in Germany. Results of the cross-sectional KiGGS Wave 2 study and trends. J. Health Monit. 2018, 3, 8–14. [Google Scholar] [CrossRef]
- Messiah, S.E.; Arheart, K.L.; Natale, R.; Hlaing, W.M.; Lipshultz, S.E.; Miller, T.L. BMI, Waist Circumference, and Selected Cardiovascular Disease Risk Factors Among Preschool-Age Children. Obesity 2012, 20, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Wyszyńska, J.; Ring-Dimitriou, S.; Thivel, D.; Weghuber, D.; Hadjipanayis, A.; Grossman, Z.; Ross-Russell, R.; Dereń, K.; Mazur, A. Physical Activity in the Prevention of Childhood Obesity: The Position of the European Childhood Obesity Group and the European Academy of Pediatrics. Front. Pediatr. 2020, 8, 662. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-Muñoz, M.; Adsuar, J.; Pérez-Gómez, J.; Muñoz-Bermejo, L.; Garcia-Gordillo, M.; Carlos-Vivas, J. Influence of Body Composition on Physical Fitness in Adolescents. Medicina 2020, 56, 328. [Google Scholar] [CrossRef]
- Chomitz, V.R.; Slining, M.M.; McGowan, R.J.; Mitchell, S.E.; Dawson, G.F.; Hacker, K.A. Is There a Relationship Between Physical Fitness and Academic Achievement? Positive Results From Public School Children in the Northeastern United States. J. Sch. Health 2009, 79, 30–37. [Google Scholar] [CrossRef]
- Gomes, T.N.; Dos Santos, F.K.; Katzmarzyk, P.T.; Maia, J. Active and strong: Physical activity, muscular strength, and metabolic risk in children. Am. J. Hum. Biol. 2016, 29, e22904. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F.; Muñoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-García, P.; Henriksson, H.; Mena-Molina, A.; Martínez-Vizcaíno, V.; et al. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 1383–1410. [Google Scholar] [CrossRef]
- Remmel, L.; Tamme, R.; Tillmann, V.; Mäestu, E.; Purge, P.; Mengel, E.; Riso, E.-M.; Jürimäe, J. Pubertal Physical Activity and Cardiorespiratory Fitness in Relation to Late Adolescent Body Fatness in Boys: A 6-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2021, 18, 4881. [Google Scholar] [CrossRef]
- Hurtig-Wennlöf, A.; Ruiz, J.; Harro, M.; Sjöström, M. Cardiorespiratory fitness relates more strongly than physical activity to cardiovascular disease risk factors in healthy children and adolescents: The European Youth Heart Study. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 575–581. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9–17 years: Results from 2 779 165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2018, 52, 1445–1456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meredith, M.D.; Welk, G. Fitnessgram and Activitygram Test Administration Manual-Updated, 4th ed.; Human Kinetics: Champaign, IL, USA, 2010. [Google Scholar]
- Woll, A.; Kurth, B.-M.; Opper, E.; Worth, A.; Bös, K. The ‘Motorik-Modul’ (MoMo): Physical fitness and physical activity in German children and adolescents. Eur. J. Pediatr. 2011, 170, 1129–1142. [Google Scholar] [CrossRef]
- Kidokoro, T.; Edamoto, K. Improvements in Physical Fitness are Associated with Favorable Changes in Blood Lipid Concentrations in Children. J. Sports Sci. Med. 2021, 20, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Lewitt, M.S.; Baker, J.S. Relationship between abdominal adiposity, cardiovascular fitness, and biomarkers of cardiovascular risk in British adolescents. J. Sport Health Sci. 2019, 9, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Du, T.; Fernandez, C.; Barshop, R.; Guralnik, J.; Bazzano, L.A. Cardiovascular risk factors from childhood and midlife physical function: The Bogalusa Heart Study. Exp. Gerontol. 2020, 136, 110947. [Google Scholar] [CrossRef] [PubMed]
- Caamaño-Navarrete, F.; Latorre-Román, P.; Párraga-Montilla, J.; Jerez-Mayorga, D.; Delgado-Floody, P. Selective Attention and Concentration Are Related to Lifestyle in Chilean Schoolchildren. Children 2021, 8, 856. [Google Scholar] [CrossRef]
- Páez-Maldonado, J.A.; Reigal, R.E.; Morillo-Baro, J.P.; Carrasco-Beltrán, H.; Hernández-Mendo, A.; Morales-Sánchez, V. Physical Fitness, Selective Attention and Academic Performance in a Pre-Adolescent Sample. Int. J. Environ. Res. Public Health 2020, 17, 6216. [Google Scholar] [CrossRef]
- McPherson, A.; Mackay, L.; Kunkel, J.; Duncan, S. Physical activity, cognition and academic performance: An analysis of mediating and confounding relationships in primary school children. BMC Public Health 2018, 18, 936. [Google Scholar] [CrossRef] [Green Version]
- Hakala, J.O.; Rovio, S.P.; Pahkala, K.; Nevalainen, J.; Juonala, M.; Hutri-Kähönen, N.; Heinonen, O.J.; Hirvensalo, M.; Telama, R.; Viikari, J.S.A.; et al. Physical Activity from Childhood to Adulthood and Cognitive Performance in Midlife. Med. Sci. Sports Exerc. 2019, 51, 882–890. [Google Scholar] [CrossRef]
- Evaristo, S.; Moreira, C.; Lopes, L.; Oliveira, A.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Santos, R.; Mota, J. Muscular fitness and cardiorespiratory fitness are associated with health-related quality of life: Results from labmed physical activity study. J. Exerc. Sci. Fit. 2019, 17, 55–61. [Google Scholar] [CrossRef]
- Andersen, J.R.; Natvig, G.K.; Aadland, E.; Moe, V.F.; Kolotkin, R.; Anderssen, S.A.; Resaland, G.K. Associations between health-related quality of life, cardiorespiratory fitness, muscle strength, physical activity and waist circumference in 10-year-old children: The ASK study. Qual. Life Res. 2017, 26, 3421–3428. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Heal. Qual. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Tebar, A.; Ruiz-Hermosa, A.; Martínez-Vizcaíno, V.; Cobo-Cuenca, A.I.; Bermejo-Cantarero, A.; Cavero-Redondo, I.; López, M.S. Associations between health-related quality of life and physical fitness in 4–7-year-old Spanish children: The MOVIKIDS study. Qual. Life Res. 2019, 28, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.J.; Steinbeck, K. The role of puberty in students’ academic motivation and achievement. Learn. Individ. Differ. 2017, 53, 37–46. [Google Scholar] [CrossRef]
- Robins, R.W.; Trzesniewski, K.H. Self-Esteem Development Across the Lifespan. Curr. Dir. Psychol. Sci. 2005, 14, 158–162. [Google Scholar] [CrossRef] [Green Version]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; Von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Ergeb. Physiol. 2001, 149, 807–818. [Google Scholar] [CrossRef] [Green Version]
- Morrow, J.R., Jr.; Martin, S.B.; Jackson, A.W. Reliability and validity of the FITNESSGRAM: Quality of teacher-collected health-related fitness surveillance data. Res. Q. Exerc. Sport 2010, 81, S24–S30. [Google Scholar] [CrossRef]
- Utesch, T.; Strauß, B.; Tietjens, M.; Büsch, D.; Ghanbari, M.-C.; Seidel, I.; Information, R. Die Überprüfung der Konstruktvalidität des Deutschen Motorik-Tests 6-18 für 9- bis 10-Jährige. Z. Sportpsychol. 2015, 22, 77–90. [Google Scholar] [CrossRef]
- Santos, J.d.R.F.; Ruiz, J.R.; Gonzalez-Montesinos, J.L.; Castro-Piñero, J. Reliability and Validity of Field-Based Tests to Assess Upper-Body Muscular Strength in Children Aged 6-12 Years. Pediatr. Exerc. Sci. 2016, 28, 331–340. [Google Scholar] [CrossRef]
- MacDermid, J.; Solomon, G.; Valdes, K. Clinical Assessment Recommendations; American Society of Hand Therapists: Mt. Laurel, NJ, USA, 2015. [Google Scholar]
- Mahar, M.T.; Guerieri, A.M.; Hanna, M.S.; Kemble, C.D. Estimation of Aerobic Fitness from 20-m Multistage Shuttle Run Test Performance. Am. J. Prev. Med. 2011, 41, S117–S123. [Google Scholar] [CrossRef]
- Mahar, M.T.; Welk, G.J.; Rowe, D.A. Estimation of aerobic fitness from PACER performance with and without body mass index. Meas. Phys. Educ. Exerc. Sci. 2017, 22, 239–249. [Google Scholar] [CrossRef] [Green Version]
- Brickenkamp, R.; Schmidt-Atzert, L.; Liepmann, D. Test. d2—Revision: Aufmerksamkeits- und Konzentrationstest; Hogrefe: Goettingen, Germany, 2010. [Google Scholar]
- Reigal, R.E.; Barrero, S.; Martín, I.; Sánchez, V.O.M.; De Mier, R.J.-R.; Hernández-Mendo, A. Relationships Between Reaction Time, Selective Attention, Physical Activity, and Physical Fitness in Children. Front. Psychol. 2019, 10, 2278. [Google Scholar] [CrossRef] [PubMed]
- Santner, A.; Kopp, M.; Federolf, P. Partly randomised, controlled study in children aged 6–10 years to investigate motor and cognitive effects of a 9-week coordination training intervention with concurrent mental tasks. BMJ Open 2018, 8, e021026. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Ellert, U.; Erhart, M. Gesundheitsbezogene Lebensqualität von Kindern und Jugendlichen in Deutschland. Bundesgesundheitsblatt Gesundh. Gesundh. 2007, 50, 810–818. [Google Scholar] [CrossRef]
- Fühner, T.; Granacher, U.; Golle, K.; Kliegl, R. Age and sex effects in physical fitness components of 108,295 third graders including 515 primary schools and 9 cohorts. Sci. Rep. 2021, 11, 17566. [Google Scholar] [CrossRef]
- Agostinis-Sobrinho, C.; Ruiz, J.R.; Moreira, C.; Lopes, L.; Ramírez-Vélez, R.; García-Hermoso, A.; Mota, J.; Santos, R. Changes in muscular fitness and its association with blood pressure in adolescents. Eur. J. Pediatr. 2018, 177, 1101–1109. [Google Scholar] [CrossRef]
- Artero, E.G.; Ruiz, J.R.; Ortega, F.B.; España-Romero, V.; Vicente-Rodríguez, G.; Molnar, D.; Gottrand, F.; González-Gross, M.; Breidenassel, C.; Moreno, L.A.; et al. Muscular and cardiorespiratory fitness are independently associated with metabolic risk in adolescents: The HELENA study. Pediatr. Diabetes 2011, 12, 704–712. [Google Scholar] [CrossRef]
- Dumuid, D.; Olds, T.; Martín-Fernández, J.A.; Lewis, L.K.; Cassidy, L.; Maher, C. Academic Performance and Lifestyle Behaviors in Australian School Children: A Cluster Analysis. Health Educ. Behav. 2017, 44, 918–927. [Google Scholar] [CrossRef]
- Bolados, C.C.; Ferrari, G.; Suárez-Reyes, M.; Dourado, D.Q.S.; Diaz-Peña, H.; Pizarro, T. Muscular Strength of Upper and Lower Limbs and Self-Esteem in Chilean SchoolChildren: Independent Associations with Body Composition Indicators. Int. J. Environ. Res. Public Health 2021, 18, 361. [Google Scholar] [CrossRef]
- Eddolls, W.T.B.; McNarry, M.A.; Lester, L.; Winn, C.O.N.; Stratton, G.; Mackintosh, K.A. The association between physical activity, fitness and body mass index on mental well-being and quality of life in adolescents. Qual. Life Res. 2018, 27, 2313–2320. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.J.; Belanger, K.; Poitras, V.; Janssen, I.; Tomkinson, G.R.; Tremblay, M.S. Systematic review of the relationship between 20 m shuttle run performance and health indicators among children and youth. J. Sci. Med. Sport 2018, 21, 383–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Noncommunicable Diseases: Progress Monitor 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Baumgartner, L.; Postler, T.; Graf, C.; Ferrari, N.; Haller, B.; Oberhoffer-Fritz, R.; Schulz, T. Can School-Based Physical Activity Projects Such as Skipping Hearts Have a Long-Term Impact on Health and Health Behavior? Front. Public Health 2020, 8, 352. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Luan, J.; Sherar, L.B.; Esliger, D.W.; Griew, P.; Cooper, A. Moderate to Vigorous Physical Activity and Sedentary Time and Cardiometabolic Risk Factors in Children and Adolescents. JAMA 2012, 307, 704–712. [Google Scholar] [CrossRef] [Green Version]
| Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | 7 | 8 | 9 | 10 | ||||||||
| n | M [CI 95%] | n | M [CI 95%] | n | M [CI 95%] | n | M [CI 95%] | n | M [CI 95%] | p | ||
| Anthropometrics | ||||||||||||
| BMI (kg/m2) | Total | 552 | 15.93 [15.76, 16.10] 8,9,10 | 1491 | 16.16 [16.05, 16.28] 8,9,10 | 1596 | 16.73 [16.60, 16.85] 6,7,9,10 | 1731 | 17.23 [17.10, 17.36] 6,7,8,10 | 1143 | 17.99 [17.80, 18.18] 6,7,8,9 | <0.001 * |
| Girls | 291 | 15.82 [15.57, 16.06] 8,9,10 | 761 | 16.02 [15.87, 16.17] 8,9,10 | 830 | 16.67 [16.50, 16.85] 6,7,9,10 | 857 | 17.13 [16.95, 17.32] 6,7,8,10 | 538 | 17.76 [17.48, 18.03] 6,7,8,9 | <0.001 * | |
| Boys | 261 | 16.06 [15.83, 16.29] 8,9,10 | 730 | 16.32 [16.15, 16.48] 8,9,10 | 766 | 16.78 [16.61, 16.96] 6,7,9,10 | 874 | 17.33 [17.15, 17.51] 6,7,8,10 | 605 | 18.19 [17.93, 18.45] 6,7,8,9 | <0.001 * | |
| zBMI | Total | 552 | 0.033 [−0.046, 0.113] | 1491 | −0.001 [−0.052, 0.050] | 1596 | 0.031 [−0.019, 0.081] | 1731 | 0.030 [−0.018, 0.078] | 1143 | 0.106 [0.043, 0.169] | 0.117 |
| Girls | 291 | −0.024 [−0.133, 0.085] | 761 | −0.068 [−0.137, 0.002] | 830 | −0.003 [−0.073, 0.066] | 857 | −0.021 [−0.091, 0.050] | 538 | 0.008 [−0.085, 0.100] | 0.690 | |
| Boys | 261 | 0.097 [−0.020, 0.213] | 730 | 0.069 [−0.005, 0.143] | 766 | 0.068 [−0.004, 0.140] | 874 | 0.080 [0.014, 0.145] | 605 | 0.194 [0.107, 0.280] | 0.145 | |
| Physical Fitness | ||||||||||||
| VO2max (ml/kg/min−1) | Total | 469 | 44.57 [44.28, 44.86] 8,9,10 | 1312 | 45.00 [44.77, 45.23] 8,9 | 1409 | 45.77 [45.49, 46.04] 6,7 | 1549 | 46.08 [45.80, 46.37] 6,7,10 | 1026 | 45.47 [45.09, 45.86] 6,9 | <0.001 * |
| Girls | 248 | 44.15 [43.81, 44.48] | 670 | 44.30 [44.05, 44.55] | 747 | 44.77 [44.45, 45.08] | 782 | 44.82 [44.50, 45.15] | 476 | 44.37 [43.92, 44.82] | 0.129 | |
| Boys | 221 | 45.05 [44.57, 45.52] 8,9,10 | 642 | 45.72 [45.34, 46.10] 8,9 | 662 | 46.90 [46.45, 47.35] 6,7 | 767 | 47.37 [46.91, 47.82] 6,7,10 | 550 | 46.43 [45.83, 47.02] 6,9 | <0.001 * | |
| Pacer (laps) | Total | 469 | 18.57 [17.76, 19.38] 7,8,9,10 | 1312 | 22.10 [21.45, 22.75] 6,8,9,10 | 1409 | 27.46 [26.68, 28.24] 6,7,9,10 | 1549 | 31.47 [30.66, 32.28] 6,7,8 | 1026 | 32.57 [31.48, 33.66] 6,7,8 | <0.001 * |
| Girls | 248 | 17.35 [16.39, 18.30] 8,9,10 | 670 | 20.15 [19.43, 20.87] 8,9,10 | 747 | 24.61 [23.71, 25.50] 6,7,9,10 | 782 | 27.88 [26.96, 28.81] 6,7,8 | 476 | 29.43 [28.15, 30.70] 6,7,8 | <0.001 * | |
| Boys | 221 | 19.95 [18.62, 21.28] 7,8,9,10 | 642 | 24.14 [23.05, 25.22] 6,8,9,10 | 662 | 30.68 [29.40, 31.96] 6,7,9,10 | 767 | 35.12 [33.83, 36.41] 6,7,8 | 550 | 35.29 [33.61, 36.97] 6,7,8 | <0.001 * | |
| HGrel | Total | 446 | 0.416 [0.405, 0.428] 7,8,9,10 | 1215 | 0.452 [0.446, 0.459] 6,8,9,10 | 1342 | 0.481 [0.475, 0.487] 6,7,9,10 | 1421 | 0.499 [0.493, 0.504] 6,7,8 | 934 | 0.500 [0.493, 0.507] 6,7,8 | <0.001 * |
| Girls | 231 | 0.390 [0.374, 0.406] 7,8,9,10 | 617 | 0.434 [0.425, 0.443] 6,8,9,10 | 696 | 0.458 [0.450, 0.467] 6,7,9,10 | 698 | 0.477 [0.469, 0.485] 6,7,8 | 444 | 0.482 [0.472, 0.492] 6,7,8 | <0.001 * | |
| Boys | 215 | 0.445 [0.429, 0.461] 7,8,9,10 | 598 | 0.471 [0.461, 0.480] 6,8,9,10 | 646 | 0.506 [0.497, 0.515] 6,7 | 723 | 0.519 [0.511, 0.528] 6,7 | 490 | 0.516 [0.506, 0.526] 6,7 | <0.001 * | |
| PU (number) | Total | 549 | 6.82 [6.17, 7.47] 7,8,9,10 | 1481 | 8.85 [8.39, 9.31] 6,8,9,10 | 1570 | 10.95 [10.46, 11.43] 6,7,9 | 1710 | 12.01 [11.51, 12.52] 6,7,8 | 111 | 11.97 [11.36, 12.59] 6,7 | <0.001 * |
| Girls | 291 | 5.53 [4.76, 6.30] 7,8,9,10 | 751 | 7.57 [7.00, 8.14] 6,9,10 | 813 | 8.59 [8.03, 9.15] 6,10 | 845 | 9.75 [9.16, 10.35] 6,7 | 523 | 10.14 [9.35, 10.92] 6,7,8 | <0.001 * | |
| Boys | 258 | 8.28 [7.23, 9.33] 8,9,10 | 730 | 10.17 [9.46, 10.88] 8,,9,10 | 757 | 13.47 [12.71, 14.24] 6,7 | 865 | 14.23 [13.44, 15.01] 6,7 | 588 | 13.60 [12.69, 14.52] 6,7 | <0.001 * | |
| CU (number) | Total | 550 | 10.92 [9.88, 11.97] 7,8,9,10 | 1489 | 16.69 [15.86, 17.53] 6,8,9,10 | 1582 | 27.89 [26.64, 29.14] 6,7,9,10 | 1725 | 36.01 [34.63, 37.39] 6,7,8,10 | 1132 | 39.55 [37.77, 41.34] 6,7,8,9 | <0.001 * |
| Girls | 290 | 11.00 [9.72, 12.28] 7,8,9,10 | 757 | 18.07 [16.85, 19.29] 6,8,9,10 | 822 | 27.94 [26.22, 29.65] 6,7,9,10 | 851 | 36.95 [34.94, 38.95] 6,7,8 | 535 | 39.83 [37.29, 42.38] 6,7,8 | <0.001 * | |
| Boys | 260 | 10.84 [9.14, 12.53] 8,9,10 | 732 | 15.27 [14.15, 16.39] 8,9,10 | 760 | 27.85 [26.01, 29.68] 6,7,9,10 | 874 | 35.10 [33.20, 36.99] 6,7,8,10 | 597 | 39.30 [36.80, 41.81] 6,7,8,9 | <0.001 * | |
| SLJ (cm) | Total | 550 | 107.2 [105.7, 108.7] 7,8,9,10 | 1491 | 115.1 [114.1, 116.0] 6,8,9,10 | 1585 | 124.1 [123.1, 125.1] 6,7,9,10 | 1728 | 132.8 [131.8, 133.8] 6,7,8,10 | 1136 | 137.1 [135.8, 138.4] 6,7,8,9 | <0.001 * |
| Girls | 290 | 103.8 [102.0, 105.7] 7,8,9,10 | 758 | 111.6 [110.3, 112.9] 6,8,9,10 | 824 | 120.1 [118.8, 121.4] 6,7,9,10 | 857 | 129.2 [127.9, 130.6] 6,7,8,10 | 532 | 133.9 [132.1, 135.6] 6,7,8,9 | <0.001 * | |
| Boys | 260 | 111.0 [108.6, 113.3] 7,8,9,10 | 733 | 118.6 [117.3, 120.0] 6,8,9,10 | 761 | 128.5 [127.0, 130.0] 6,7,9,10 | 871 | 136.3 [134.9, 137.8] 6,7,8,10 | 604 | 140.0 [138.1, 141.8] 6,7,8,9 | <0.001 * | |
| Concentration | ||||||||||||
| d2-R (score) | Total | 123 | 72.50 [69.54, 75.45] 8,9,10 | 414 | 79.67 [77.52, 81.81] 7,9,10 | 508 | 94.19 [92.38, 96.00] 7,8 | 342 | 98.23 [95.56, 100.89] 7,8 | <0.001 * | ||
| Girls | 67 | 73.90 [69.60, 78.19] 9,10 | 218 | 80.13 [77.02, 83.24] 9,10 | 257 | 96.99 [94.47, 99.51] 7,8 | 162 | 100.75 [96.76, 104.73] 7,8 | <0.001 * | |||
| Boys | 56 | 70.82 [66.74, 74.90] 9,10 | 196 | 79.15 [76.19, 82.11] 9,10 | 251 | 91.32 [88.75, 93.90] 7,8 | 180 | 95.96 [92.37, 99.54] 7,8 | <0.001 * | |||
| HRQOL | ||||||||||||
| HRQOL Total (score) | Total | 326 | 76.73 [75.63, 77.83] | 672 | 75.78 [74.98, 76.58] | 0.179 | ||||||
| Girls | 176 | 77.06 [75.68, 78.44] | 339 | 77.08 [75.97, 78.19] | 0.987 | |||||||
| Boys | 150 | 76.34 [74.55, 78.12] | 333 | 74.46 [73.31, 75.61] | 0.066 | |||||||
| Physical well-being (score) | Total | 326 | 79.52 [77.87, 81.18] | 672 | 79.00 [77.82, 80.17] | 0.612 | ||||||
| Girls | 176 | 79.73 [77.59, 81.88] | 339 | 78.60 [76.92, 80.28] | 0.429 | |||||||
| Boys | 150 | 79.28 [76.70, 81.86] | 333 | 79.40 [77.74, 81.06] | 0.937 | |||||||
| Emotional well-being (score) | Total | 326 | 83.94 [82.66, 85.22] 10 | 672 | 82.17 [81.11, 83.22] 9 | 0.036 * | ||||||
| Girls | 176 | 83.53 [81.89, 85.18] | 339 | 83.14 [81.71, 84.58] | 0.751 | |||||||
| Boys | 150 | 84.42 [82.40, 86.44] 10 | 333 | 81.17 [79.62, 82.73] 9 | 0.013 * | |||||||
| Self-esteem (score) | Total | 326 | 61.73 [59.48, 63.99] | 672 | 61.61 [60.07, 63.15] | 0.929 | ||||||
| Girls | 176 | 61.49 [58.74, 64.25] | 339 | 62.86 [60.75, 64.97] | 0.474 | |||||||
| Boys | 150 | 62.01 [58.28, 65.75] | 333 | 60.34 [58.09, 62.60] | 0.406 | |||||||
| Family (score) | Total | 326 | 84.33 [82.63, 86.03] | 672 | 84.09 [82.88, 85.29] | 0.819 | ||||||
| Girls | 176 | 86.62 [84.83, 88.41] | 339 | 86.20 [84.68, 87.71] | 0.769 | |||||||
| Boys | 150 | 81.64 [78.64, 84.64] | 333 | 81.94 [80.09, 83.79] | 0.846 | |||||||
| Friends (score) | Total | 326 | 76.83 [75.02, 78.65] | 672 | 77.24 [75.95, 78.52] | 0.722 | ||||||
| Girls | 176 | 76.66 [74.22, 79.09] | 339 | 78.88 [77.11, 80.64] | 0.155 | |||||||
| Boys | 150 | 77.04 [74.30, 79.78] | 333 | 75.57 [73.71, 77.43] | 0.373 | |||||||
| School (score) | Total | 326 | 73.84 [71.99, 75.70] 10 | 672 | 70.50 [69.09, 71.90] 9 | 0.005 * | ||||||
| Girls | 176 | 74.11 [71.61, 76.61] | 339 | 72.62 [70.65, 74.58] | 0.372 | |||||||
| Boys | 150 | 73.53 [70.73, 76.33] 10 | 333 | 68.34 [66.33, 70.34] 9 | 0.003 * | |||||||
| Coefficients | b [95% CIb] a | Seb a | β | t | p |
|---|---|---|---|---|---|
| Dependent variable: Total HRQOL (n = 802) | |||||
| Sex | 3.661 [2.259, 5.102] | 0.76 | 0.17 | 4904 | <0.001 * |
| BMI | −0.005 [−0.282, 0.295] | 0.14 | −0.00 | −0.033 | 0.973 |
| VO2max | 0.340 [0.191, 0.488] | 0.07 | 0.21 | 4691 | <0.001 * |
| HGrel | 4.265 [−3.477, 11.98] | 4.12 | 0.04 | 1073 | 0.284 |
| PU | 0.073 [−0.008, 0.150] | 0.04 | 0.07 | 1710 | 0.088 |
| CU | 0.033 [0.012, 0.055] | 0.01 | 0.10 | 2828 | 0.005 * |
| SLJ | 0.003 [−0.041, 0.050] | 0.02 | 0.01 | 0.154 | 0.878 |
| Dependent variable: Concentration (n = 752) | |||||
| Age | 4.522 [1.127, 7.653] | 1.76 | 0.10 | 2.779 | 0.006 * |
| Sex | 7.909 [4.752, 11.36] | 1.74 | 0.18 | 4.743 | <0.001 * |
| BMI | 0.112 [−0.520, 0.744] | 0.32 | 0.01 | 0.348 | 0.728 |
| VO2max | 0.594 [0.260, 0.927] | 0.16 | 0.16 | 3.494 | <0.001 * |
| PU | 0.127 [−0.066, 0.321] | 0.09 | 0.06 | 1.290 | 0.198 |
| CU | 0.013 [−0.038, 0.064] | 0.02 | 0.02 | 0.507 | 0.612 |
| SLJ | 0.087 [−0.006, 0.179] | 0.04 | 0.08 | 1.841 | 0.066 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Köble, K.; Postler, T.; Oberhoffer-Fritz, R.; Schulz, T. A Better Cardiopulmonary Fitness Is Associated with Improved Concentration Level and Health-Related Quality of Life in Primary School Children. J. Clin. Med. 2022, 11, 1326. https://doi.org/10.3390/jcm11051326
Köble K, Postler T, Oberhoffer-Fritz R, Schulz T. A Better Cardiopulmonary Fitness Is Associated with Improved Concentration Level and Health-Related Quality of Life in Primary School Children. Journal of Clinical Medicine. 2022; 11(5):1326. https://doi.org/10.3390/jcm11051326
Chicago/Turabian StyleKöble, Katharina, Tanja Postler, Renate Oberhoffer-Fritz, and Thorsten Schulz. 2022. "A Better Cardiopulmonary Fitness Is Associated with Improved Concentration Level and Health-Related Quality of Life in Primary School Children" Journal of Clinical Medicine 11, no. 5: 1326. https://doi.org/10.3390/jcm11051326
APA StyleKöble, K., Postler, T., Oberhoffer-Fritz, R., & Schulz, T. (2022). A Better Cardiopulmonary Fitness Is Associated with Improved Concentration Level and Health-Related Quality of Life in Primary School Children. Journal of Clinical Medicine, 11(5), 1326. https://doi.org/10.3390/jcm11051326






