Regular School Sport versus Dedicated Physical Activities for Body Posture—A Prospective Controlled Study Assessing the Sagittal Plane in 7–10-Year-Old Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Intervention
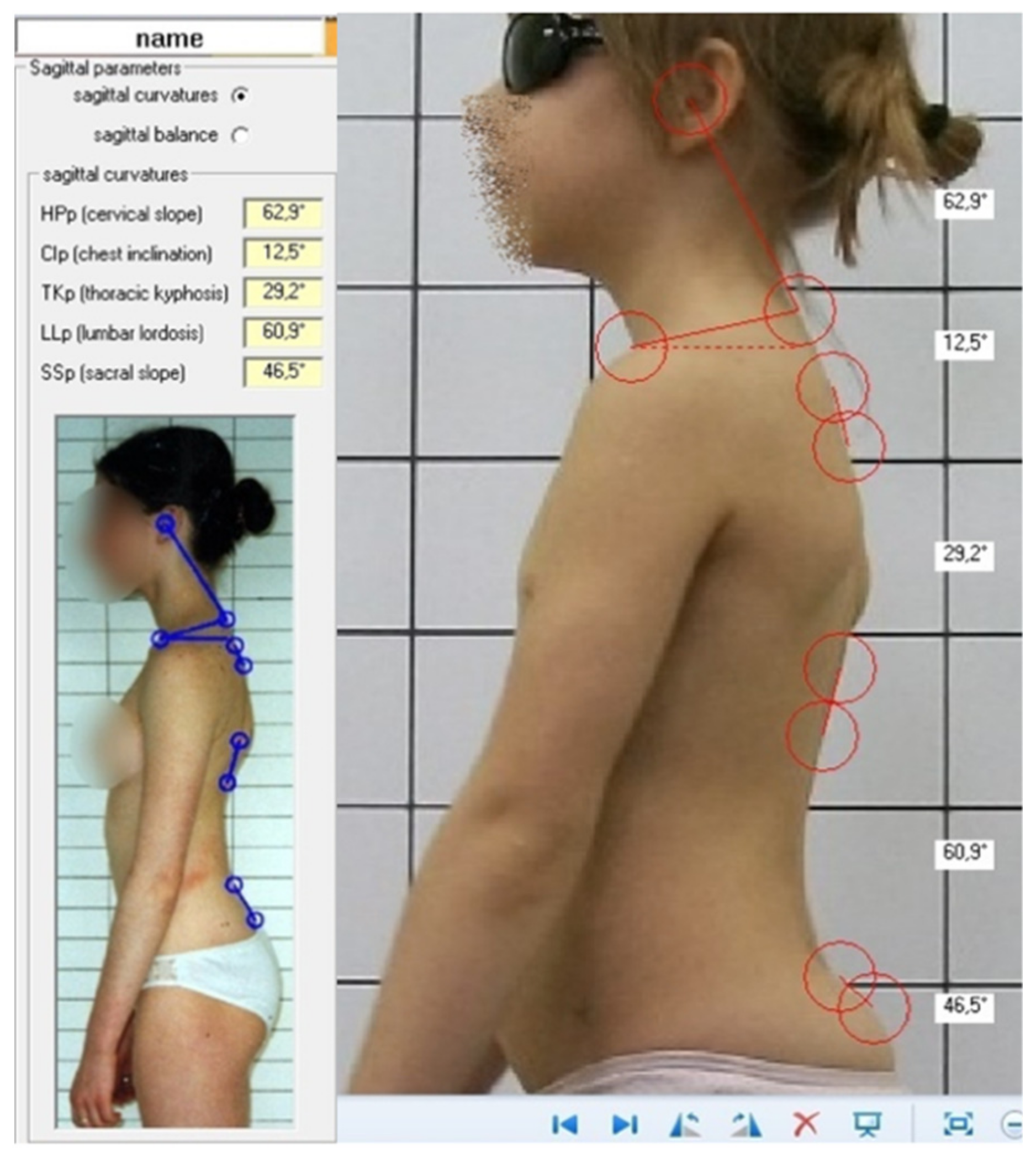
2.3. Assessment
2.4. Intra- and Inter-Rater Reliability
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Body Posture Evaluation Technique
4.2. Sample Selection
4.3. Impact of Physical Activities on the Body Posture
4.4. Impact of Corrective Activities on Body Posture in the Literature
4.5. Impact of Physical Activities on the General Health of the Child
4.6. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Parameter | ICC | 95% C.I. | SEM [°] | SD [°] |
|---|---|---|---|---|
| Sacral slope | 0.940 | 0.892–0.969 | 0.910 | 6.5 |
| Lumbar lordosis | 0.975 | 0.954–0.987 | 0.888 | 9.82 |
| Thoracic kyphosis | 0.920 | 0.856–0.959 | 0.913 | 7.10 |
| Chest inclination | 0.916 | 0.842–0.958 | 0.913 | 5.76 |
| Head protraction | 0.885 | 0.802–0.939 | 0.949 | 4.59 |
References
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’ sitting posture real? Measurement of spinal curves in four sitting postures. Man Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Angelakopoulos, G.; Savelsbergh, G.J.; Bennett, S.; Davids, K.; Haralambos, T.; George, G. Systematic review regarding posture development from infancy to adulthood. Hell. J. Phys. Educ. Sport Sci. 2008, 68, 35–43. [Google Scholar]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Dewitte, V.; De Pauw, R.; De Meulemeester, K.; Peersman, W.; Danneels, L.; Bouche, K.; Roets, A.; Cagnie, B. Clinical classification criteria for nonspecific low back pain: A Delphi-survey of clinical experts. Musculoskelet. Sci. Pract. 2018, 34, 66–76. [Google Scholar] [CrossRef]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-dimensional digital photography for child body posture evaluation: Standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord. 2017, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Hemming, K.; Eldridge, S.; Forbes, G.; Weijer, C.; Taljaard, M. How to design efficient cluster randomized trials. BMJ 2017, 358, 3064. [Google Scholar] [CrossRef]
- Cerny, P.; Stolinski, L.; Drnkova, J.; Czaprowski, D.; Kosteas, A.; Marik, I. Skeletal deformities measurements of X-ray images and photos on the computer. Locomot. Syst. J. 2016, 23, 32–36. [Google Scholar]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Stoliński, Ł.; Czaprowski, D.; Kozinoga, M.; Kotwicki, T. Clinical measurement of sagittal trunk curvatures: Photographic angles versus Rippstein plurimeter angles in healthy school children. Scoliosis 2014, 9, 15. [Google Scholar] [CrossRef]
- Stolinski, L.; Kotwicki, T.; Czaprowski, D.; Chowanska, J.; Suzuki, N. Analysis of the Anterior Trunk Symmetry Index (ATSI). Preliminary report. Stud. Health Technol. Inf. 2012, 176, 242–246. [Google Scholar] [CrossRef][Green Version]
- Young, S. Research for medical photographers: Photographic measurement. J. Audiov. Media Med. 2002, 25, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Dunk, N.M.; Lalonde, J.; Callaghan, J.P. Implications for the use of postural analysis as a clinical diagnostic tool: Reliability of quantifying upright standing spinal postures from photographic images. J. Manip. Physiol. 2005, 28, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Van Niekerk, S.M.; Louw, Q.; Vaughan, C.; Grimmer-Somers, K.; Schreve, K. Photographic measurement of upper-body sitting posture of high school students: A reliability and validity study. BMC Musculoskelet. Disord. 2008, 9, 113–123. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, M.P.; Grimmer, K. Reliability of upright posture measurements in primary school children. BMC Musculoskelet. Disord 2005, 6, 35. [Google Scholar] [CrossRef]
- Stoliński, Ł. Ocena Postawy Ciała z Wykorzystaniem Fotografii Cyfrowej: Opracowanie Metody Wraz z Normami Dla Wieku 8–11 lat. Ph.D. Thesis, Poznan University of Medical Sciences, Poznan, Poland, 2015. (In Polish). [Google Scholar]
- Canales, J.Z.; Cordás, T.A.; Fiquer, J.T.; Cavalcante, A.F.; Moreno, R.A. Posture and body image in individuals with major depressive disorder: A controlled study. Rev. Bras. Psiquiatr. 2010, 32, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Theory and Practical Applications; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2001. [Google Scholar]
- Kułaga, Z.; Różdżyńska-Świątkowska, A.; Grajda, A.; Gurzkowska, B.; Wojtyło, M.; Góźdź, M.; Świąder-Leśniak, A.; Litwin, M. Siatki centylowe dla oceny wzrastania i stanu odżywienia polskich dzieci i młodzieży od urodzenia do 18 roku życia. Stand. Med. Pediatr. 2015, 12, 119–135. (In Polish) [Google Scholar]
- Neinstein, L.S.; Kaufman, F.R. Chapter 1: Normal Physical Growth and Development. In Adolescent Health Care: A Practical Guide, 4th ed.; Neinstein, L.S., Ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2002. [Google Scholar]
- Dutkiewicz, R. Skuteczność Zajęć Korekcyjno-Wyrównawczych w Zniekształceniach Statycznych Ciała u Dzieci w Wieku Szkolnym; Wydawnictwo Uniwersytetu Humanistyczno-Przyrodniczego Jana Kochanowskiego: Kielce, Poland, 2010. (In Polish) [Google Scholar]
- Cosma, G.; Ilinca, I.; Rusu, L.; Nanu, C.; Burileanu, A. Physical exercise and its role in a correct postural alignment. Phys. Educ. Sport Kinetotherapy J. 2015, 11, 39. [Google Scholar]
- Torlaković, A.; Muftić, M.; Avdić, D.; Kebata, R. Effects of the combined swimming, corrective and aqua gymnastics programme on body posture of preschool age children. J. Health Sci. 2013, 3, 103–108. [Google Scholar]
- US Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report. 2008. Available online: https://health.gov/sites/default/files/2019-10/CommitteeReport_7.pdf (accessed on 11 November 2021).
- Sundberg, M.; Gärdsell, P.; Johnell, O.; Karlsson, M.K.; Ornstein, E.; Sandstedt, B.; Sernbo, I. Physical Activity Increases Bone Size in Prepubertal Boys and Bone Mass in Prepubertal Girls: A Combined Cross-Sectional and 3-Year Longitudinal Study. Calcif. Tissue Int. 2002, 71, 406–415. [Google Scholar] [CrossRef]
- Welten, D.C.; Kemper, H.C.; Post, G.B.; Van Mechelen, W.; Twisk, J.; Lips, P.; Teule, G.J. Weight-bearing activity during youth is a more important factor for peak bone mass than calcium intake. J. Bone Min. Res. 1994, 9, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Bielemann, R.M.; Martinez-Mesa, J.; Gigante, D.P. Physical activity during life course and bone mass: A systematic review of methods and findings from cohort studies with young adults. BMC Musculoskelet. Disord. 2013, 14, 77. [Google Scholar] [CrossRef] [PubMed]
| Parameter | ICC | 95% C.I. | SEM [°] | SD [°] |
|---|---|---|---|---|
| Sacral slope | 0.975 | 0.884–0.986 | 1.007 | 6.4 |
| Lumbar lordosis | 0.981 | 0.968–0.989 | 1.225 | 8.88 |
| Thoracic kyphosis | 0.987 | 0.977–0.992 | 1.170 | 10.14 |
| Chest inclination | 0.981 | 0.968–0.989 | 0.901 | 6.55 |
| Head protraction | 0.995 | 0.991–0.997 | 0.447 | 6.32 |
| Posture | Control N = 167 | Intervention N = 233 | p | |
|---|---|---|---|---|
| Parameter | ||||
| Sacral slope [°] | 29.58 ± 7.23 | 28.63 ± 7.6 | 0.210 | |
| Lumbar lordosis [°] | 46.94 ± 8.96 | 46.08 ± 9.78 | 0.366 | |
| Thoracic kyphosis [°] | 41.63 ± 9.55 | 42.23 ± 9.11 | 0.523 | |
| Chest inclination [°] | 15.9 ± 7 | 16.1 ± 5.64 | 0.757 | |
| Head protraction [°] | 31.65 ± 5.16 | 31.96 ± 6.44 | 0.611 | |
| Posture | H0 | H1 | p | |
|---|---|---|---|---|
| Parameter | ||||
| Sacral slope [°] | 29.58 ± 7.23 | 29.75 ± 6.79 | 0.758 | |
| Lumbar lordosis [°] | 46.94 ± 8.96 | 47.50 ± 9.19 | 0.38 | |
| Thoracic kyphosis [°] | 41.63 ± 9.55 | 42.38 ± 9.39 | 0.328 | |
| Chest inclination [°] | 15.9 ± 7 | 16.86 ± 6.32 | 0.081 | |
| Head protraction [°] | 31.65 ± 5.16 | 32.45 ± 6.08 | 0.106 | |
| Posture | H0 | H1 | p | |
|---|---|---|---|---|
| Parameter | ||||
| Sacral slope [°] | 28.63 ± 7.6 | 27.23 ± 6.68 | 0.001 | |
| Lumbar lordosis [°] | 46.08 ± 9.78 | 44.49 ± 9.34 | 0.062 | |
| Thoracic kyphosis [°] | 42.23 ± 9.11 | 42.79 ± 9.98 | 0.404 | |
| Chest inclination [°] | 16.1 ± 5.64 | 16.37 ± 5.95 | 0.547 | |
| Head protraction [°] | 31.96 ± 6.44 | 32.80 ± 6.07 | 0.058 | |
| Posture | Control N = 167 | Intervention N = 233 | p | |
|---|---|---|---|---|
| Parameter | ||||
| Sacral slope [°] | 29.747 ± 6.79 | 27.23 ± 6.68 | 0.0002 | |
| Lumbar lordosis [°] | 47.50 ± 9.19 | 44.92 ± 9.34 | 0.0064 | |
| Thoracic kyphosis [°] | 42.38 ± 9.38 | 42.79 ± 9.98 | 0.674 | |
| Chest inclination [°] | 16.86 ± 6.32 | 16.37 ± 5.95 | 0.427 | |
| Head protraction [°] | 32.45 ± 6.08 | 32.80 ± 6.07 | 0.57 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozinoga, M.; Stoliński, Ł.; Korbel, K.; Politarczyk, K.; Janusz, P.; Kotwicki, T. Regular School Sport versus Dedicated Physical Activities for Body Posture—A Prospective Controlled Study Assessing the Sagittal Plane in 7–10-Year-Old Children. J. Clin. Med. 2022, 11, 1255. https://doi.org/10.3390/jcm11051255
Kozinoga M, Stoliński Ł, Korbel K, Politarczyk K, Janusz P, Kotwicki T. Regular School Sport versus Dedicated Physical Activities for Body Posture—A Prospective Controlled Study Assessing the Sagittal Plane in 7–10-Year-Old Children. Journal of Clinical Medicine. 2022; 11(5):1255. https://doi.org/10.3390/jcm11051255
Chicago/Turabian StyleKozinoga, Mateusz, Łukasz Stoliński, Krzysztof Korbel, Katarzyna Politarczyk, Piotr Janusz, and Tomasz Kotwicki. 2022. "Regular School Sport versus Dedicated Physical Activities for Body Posture—A Prospective Controlled Study Assessing the Sagittal Plane in 7–10-Year-Old Children" Journal of Clinical Medicine 11, no. 5: 1255. https://doi.org/10.3390/jcm11051255
APA StyleKozinoga, M., Stoliński, Ł., Korbel, K., Politarczyk, K., Janusz, P., & Kotwicki, T. (2022). Regular School Sport versus Dedicated Physical Activities for Body Posture—A Prospective Controlled Study Assessing the Sagittal Plane in 7–10-Year-Old Children. Journal of Clinical Medicine, 11(5), 1255. https://doi.org/10.3390/jcm11051255






