Current Concepts in the Etiology and Pathogenesis of Pectus Excavatum in Humans—A Systematic Review
Abstract
1. Introduction
2. The Historic Perspective
3. The Histologic Perspective
4. The Genetic Perspective
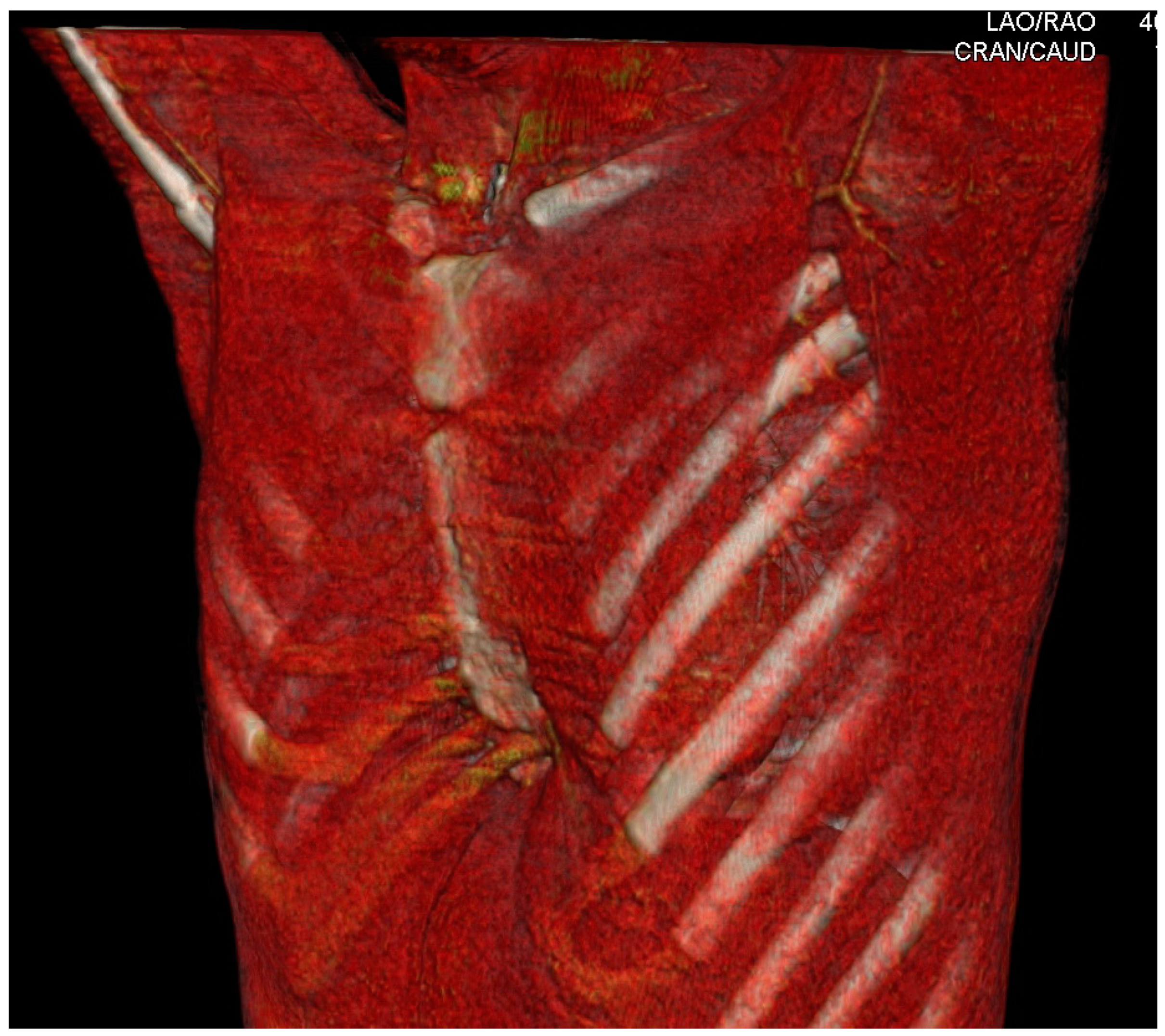
5. The Anatomopathological and Biomechanical Perspectives
6. Experimental Studies and Animal Models of Pectus Excavatum
7. Overview of the Current Concepts Regarding the Etiopathogenesis of Pectus Excavatum
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kelly, R.E., Jr. Pectus excavatum: Historical background, clinical picture, preoperative evaluation and criteria for operation. Semin. Pediatr. Surg. 2008, 17, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Brochhausen, C.; Turial, S.; Müller, F.K.P.; Schmitt, V.H.; Coerdt, W.; Wihlm, J.M.; Schier, F.; Kirkpatrick, C.J. Pectus excavatum: History, hypotheses and treatment options. Interact. Cardiovasc. Thorac. Surg. 2012, 14, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Shamberger, R.C.; Welch, K.J. Surgical repair of pectus excavatum. J. Pediatr. Surg. 1988, 23, 615–622. [Google Scholar] [CrossRef]
- Nuss, D.; Obermeyer, R.J.; Kelly, R.E., Jr. Pectus excavatum from a pediatric surgeon’s perspective. Ann. Cardiothorac. Surg. 2016, 5, 493–500. [Google Scholar] [CrossRef]
- Nicodin, A.; Boi, A.E.S.; Popoiu, M.C.; Cozma, G.; Nicodin, G.; Badeti, R.; Trailescu, M.; Adam, O.; David, V.L. Preliminary results after Nuss procedure. Chirurgia 2010, 105, 203–210. [Google Scholar]
- Kulik, I.O.; Plyakin, V.A.; Sarukhanyan, O.O.; Ignat’Eva, N.Y.; Poludov, S.A. Etiology and pathogenesis of pectus excavatum in children. Traumatol. Orthop. Russ. 2013, 19, 136–141. [Google Scholar] [CrossRef]
- Toth, G.A.; Bud, A.B.L. Funnel chest (pectus excavatum) in 10–16th century fossil material. J. Paleontol. 2001, 13, 63–66. [Google Scholar]
- Bauhinus, J. Observatio. In Ioannis Schenckii a Grafenberg; Johannes Observatorium Medicarum, Rararum, Novar-um, Admirabilium, et Montrosarum, Liber Secundus; De partibus Vitalibus, Thorace Contentis: Frankfurt, Germany, 1609; p. 322. [Google Scholar]
- Eggel, C. Eine seltene Mißbildung des Thorax. Virchows. Arch. Path Anat. 1870, 49, 230. [Google Scholar] [CrossRef]
- Langer, H.; Zuckerkandel, E. Untersuchungen über den mißbildeten Brustkorb des. Herrn. JW Wien. Med. Zeit 1880, 49, 515. [Google Scholar]
- Flesch, M. Ueber eine seltene Missbildung des Thorax. Virchow. Arch. Path Anat. 1873, 57, 289–294. [Google Scholar] [CrossRef][Green Version]
- Hagmann. Selten vorkommende Abnormität des Brustkastens. J. B Kinderheilkd. 1888, 15, 455. [Google Scholar]
- Meyer, L. Zur chirurgischen Behandlung der angeborenen Trichterbrust. Berl. Klin. Wschr. 1911, 48, 1563–1566. [Google Scholar]
- Muller, C. Zur Entwicklung des Menschlichen Brustkorbs, Morphol Jahrb; W Engelman: Leipzig, Germany, 1906; Volume 35, pp. 591–596. [Google Scholar]
- Ochsner, A.; Debakey, M.E. Chonechondrosternon: Report of a case and review of the Iiterature. J. Tboracic. Surg. 1938, 8, 469–511. [Google Scholar] [CrossRef]
- Kelley, S.W. Surgical Diseases of Children: A Modern Treatise on Pediatric Surgery. Ann. Surg. 1910, 51, 438. [Google Scholar]
- Brown, A.L.; Cook, O. Funnel chest (pectus excavatum) in infancy and adult life. Calif. Med. 1951, 74, 174–178. [Google Scholar]
- Maneke, M. Untersuchungen zur Pathogenese der Brustkorbverformungen1. DMW Dtsch. Med. Wochenschr. 1959, 84, 504–509. [Google Scholar] [CrossRef]
- Curschmann, H. Über erbliche Arachnodaktylie. Nervenarzt 1936, 9, 624. [Google Scholar]
- Saxena, A.K. History of Surgical Repairs of Chest Wall Deformities in Saxena AK editor. In Chest Wall Deformities; Springer: Berlin/Heidelberg, Germany, 2017; pp. 3–18. [Google Scholar]
- Brown, A.L. Pectus Excavatum. J. Thorac. Surg. 1939, 9, 164. [Google Scholar] [CrossRef]
- Brown, A. Lincoln: Pectus Excavatum (Funnel Chest). Anatomic Basis: Surgical Treatment of the Incipient Stage in In-fancy; and Correction of the Deformity in the Fully Developed Stage. J. Thorac. Surg. 1940, 9, 164–184. [Google Scholar] [CrossRef]
- Brodkin, H.A. Congenital chondrosternal depression (funnel chest) Its treatment by phrenosternolysis and chondroster-noplasty. Dis. Chest. 1951, 19, 288–306. [Google Scholar] [CrossRef]
- Brodkin, H.A. Congenital Anterior Chest Wall Deformities of Diaphragmatic Origin. Dis. Chest 1953, 24, 259–277. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.L.; George, R.E.; Hewlett, T.H.; Bowers, W.F. Pectus excavatum: Surgical experiences in thirty-four cases. Am. J. Surg. 1959, 98, 664–676. [Google Scholar] [CrossRef]
- Ravitch, M.M. The Operative Treatment of Pectus Excavatum. Ann. Surg. 1949, 129, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Lester, C.W. Funnel chest: Its cause, effects, and treatment. J. Pediatr. 1950, 37, 224–230. [Google Scholar] [CrossRef]
- Koop, C.E. The Management of Pectus Excavatum. Surg. Clin. N. Am. 1956, 36, 1627–1637. [Google Scholar] [CrossRef]
- Sweet, R.H. Pectus Excavatum: Report of Two Cases Successfully Operated Upon. Ann. Surg. 1944, 119, 922–934. [Google Scholar]
- Lindskog, G.E.; Felton, W.L. Considerations in the Surgical Treatment of Pectus Excavatum. Ann. Surg. 1955, 142, 654–661. [Google Scholar] [CrossRef]
- Mahoney, E.B.; Emerson, G.L. Surgical treatment of the congenital funnel-chest deformity. AMA Arch. Surg. 1953, 67, 317–329. [Google Scholar] [CrossRef]
- Mullard, K. Observations on the aetiology of pectus excavatum and other chest deformities, and a method of recording them. Br. J. Surg. 1967, 54, 115–120. [Google Scholar] [CrossRef]
- Sauerbruch, F. Die Chirurgie Der Brustorgane; Julius Springer: Berlin, Germany, 1920; Volume 1, p. 437. [Google Scholar]
- Nuss, D.; Kelly, R.E., Jr.; Croitoru, D.P.; Katz, M.E. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J. Pediatr. Surg. 1998, 33, 545–552. [Google Scholar] [CrossRef]
- Allen, R.G.; Douglas, M. Cosmetic improvement of thoracic wall defects using a rapid setting silastic mold: A special technique. J. Pediatr. Surg. 1979, 14, 745–749. [Google Scholar] [CrossRef]
- Rehbein, F.; Wernicke, H.H. The operative treatment of the funnel chest. Arch. Dis. Child. 1957, 32, 5–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Welch, K.J. Satisfactory surgical correction of pectus excavatum deformity in childhood; a limited opportunity. J. Thorac. Surg. 1958, 36, 697–713. [Google Scholar] [CrossRef]
- Haller, J.A., Jr.; Kramer, S.S.; Lietman, S.A. Use of CT scans in selection of patients for pectus excavatum surgery: A preliminary report. J. Pediatr Surg. 1987, 22, 904–906. [Google Scholar] [CrossRef]
- Fonkalsrud, E.W. 912 Open Pectus Excavatum Repairs: Changing Trends, Lessons Learned: One Surgeon’s Experience. World J. Surg. 2008, 33, 180–190. [Google Scholar] [CrossRef]
- Saxena, A.K.; Willital, G.H. Valuable lessons from two decades of pectus repair with the Willital-Hegemann procedure. J. Thorac. Cardiovasc. Surg. 2007, 134, 871–876. [Google Scholar] [CrossRef][Green Version]
- Wada, J. Surgical correction of the funnel chest “sternoturnover”. West. J. Surg. Obstet. Gynecol. 1961, 69, 358–361. [Google Scholar]
- Isakov, J.F.; Geraskin, V.I.; Rudakov, S.S.; Vasiljev, G.S.; Gerberg, A.N.; Burinov, G.M.; Muho, S.B.; Kondrashin, N.I.; Besjadovskaja, G.L. A new method of surgical treatment of funnel chest with help of permanent magnets. Chir. Pediatr. 1980, 21, 361–362. [Google Scholar]
- Harrison, M.R.; Estefan-Ventura, D.; Fechter, R.; Moran, A.M., Jr.; Christensen, D. Magnetic mini-mover procedure for pectus excavatum: I. Development, design, and simulations for feasibility and safety. J. Pediatr. Surg. 2007, 42, 81–85, discussion 85–86. [Google Scholar] [CrossRef]
- Jamshidi, R.; Harrison, M. Magnet-mediated thoracic remodeling: A new approach to the sunken chest. Expert Rev. Med. Devices 2007, 4, 283–286. [Google Scholar] [CrossRef][Green Version]
- Graves, C.E.; Hirose, S.; Raff, G.W.; Iqbal, C.W.; Imamura-Ching, J.; Christensen, D.; Fechter, R.; Kwiat, D.; Harrison, M.R. Magnetic Mini-Mover Procedure for pectus excavatum IV: FDA sponsored multicenter trial. J. Pediatr. Surg. 2017, 52, 913–919. [Google Scholar] [CrossRef] [PubMed]
- Weber, P.G.; Hümmer, H.P. Die “neue” Erlanger Trichterbrustkorrektur—Minimalisierung eines bewährten Verfahrens [The “new” Erlangen technique of funnel chest correction—minimalization of a well working procedure]. Zentralbl. Chir. 2006, 131, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Schulz-Drost, S.; Luber, A.M.; Simon, K.; Schulz-Drost, M.; Syed, J.; Carbon, R.T.; Besendörfer, M. Elastic stable chest repair and its hybrid variants in 86 patients with pectus excavatum. J. Thorac. Dis. 2018, 10, 5736–5746. [Google Scholar] [CrossRef]
- Giem, R.N.; Paulsen, G.A.; Dykes, J. Pectus deformities. Calif. Med. 1961, 94, 306–309. [Google Scholar] [PubMed]
- Lester, C.W. The etiology and pathogenesis of funnel chest, pigeon breast, and related deformities of the anterior chest wall. J. Thorac. Surg. 1957, 34, 1–10. [Google Scholar] [CrossRef]
- Cormack, D.H. Essential Histology, 2nd ed.; Lippincott Williams &Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Geisbe, H.; Buddecke, E.; Flach, A.; Müller, G.; Stein, U. Biochemical, morphological and physical as well as animal ex-perimental studies on the pathogenesis of funnel chest. Langenbecks Arch. Chir. 1967, 319, 536–541. [Google Scholar] [CrossRef]
- Müller, G.; Flach, A.; Geisbe, H. Morphological studies on resected rib cartilage in funnel chest. Frankf. Z. Fur Pathol. 1967, 76, 164–178. [Google Scholar]
- Geisbe, H.; Mildenberger, H.; Flach, A.; Fendel, H. The aetiology and pathogenesis of funnel chest. Prog. Pediatr. Surg. 1971, 3, 13–26. [Google Scholar]
- Tischer, W.; Leutert, G. Morphologische Veränderungen der Rippenknorpel bei Trichterbrust (Morphologic changes of rib cartilages in funnel chest). Beitr. Orthop. Traumatol. 1968, 15, 65–66. [Google Scholar]
- Rupprecht, H.; Hümmer, H.P.; Stöss, H.; Waldherr, T. Pathogenesis of chest wall abnormalities—electron microscopy studies and trace element analysis of rib cartilage. Zeitschrift Kinderchirurgie 1987, 42, 228–229. [Google Scholar]
- Kuritsyn, V.M.; Shabanov, A.M.; Shekhonin, B.V.; Rukosuev, V.S.; Rudakov, S.S. Pathohistology of costal cartilage and immunomorphologic characteristics of collagen in funnel chest. Arkhiv. Patol. 1987, 49, 20–26. [Google Scholar]
- Rupprecht, H.; Freiberger, N. Light microscopic studies of the cartilage in funnel chest. A new view of the pathogenesis. Z. Exp. Chir. Transpl. Kunstl. Organe 1989, 22, 314–318. [Google Scholar]
- Sokolov, B.P.; Sher, B.M.; Kozlov, E.A.; Tsvetkova, T.A.; Rudakov, S.S.; Del’vig, A.A.; Kalinin, V.N. Changes in the structure of type I collagen and cross-links between type I and type III collagen chains in a patient with funnel chest. Vopr. Med. Khim. 1989, 35, 91–102. [Google Scholar]
- Sokolov, B.P.; She, R.B.M.; Kozlov, E.A.; Tsvetkova, T.A.; Rudakov, S.S.; Del’vig, A.A.; Kalinin, V.N. Structural charac-teristics of collagens from the skin and rib cartilage of patients with Ehlers-Danlos syndrome type II. Vopr. Med. Khim. 1990, 36, 90–93. [Google Scholar] [PubMed]
- Tsvetkova, T.A.; Kozlov, E.A.; Rudakov, S.S.; Del’vig, A.A. Extractability of collagen from the rib cartilage and skin in funnel chest in children. Vopr. Med. Khim. 1988, 34, 71–74. [Google Scholar]
- Tsvetkova, T.A.; Gorokhova, T.A.; Del’vig, A.A. The effect of ascorbic acid on the collagen synthesis in skin fibroblasts of children with funnel chest. Vopr. Med. Khim. 1990, 36, 53–55. [Google Scholar] [PubMed]
- Prozorovskaya, N.N.; Kozlov, E.A.; Voronov, A.V.; Verovskii, V.A.; Delvig, A.A. Characterization of Costal Cartilage Collagen in Funnel Chest. Biomed. Sci. 1991, 2, 576–580. [Google Scholar] [PubMed]
- Borisova, N.V.; Pokrovskaya, A.Y.; Zakharova, E.Y.; Krasnopol’skaya, K.D. Analysis of collagen hydroxypyridinium crosslinks in samples of tissues and urine of patients with inherited connective tissue disorders. Connect. Tissue Res. 1994, 30, 177–190. [Google Scholar] [CrossRef]
- Borisova, N.V.; Pokrovskaya, A.Y.; Zakharova, E.Y.; Krasnopol’skaya, K.D.; Poliudov, S.A. Analysis of hydroxypyri-dine cross-links of collagen from human rib cartilage. Biull. Eksp. Biol. Med. 1993, 115, 516–518. [Google Scholar] [CrossRef]
- Feng, J.; Hu, T.; Liu, W.; Zhang, S.; Tang, Y.; Chen, R.; Jiang, X.; Wei, F. The biomechanical, morphologic, and histochem-ical properties of the costal cartilages in children with pectus excavatum. J. Pediatr. Surg. 2001, 36, 1770–1776. [Google Scholar] [CrossRef]
- Serafin, J.; Swiatkowski, J.; Majkusiak, R.; Nowakowski, P. 40-year experience in surgical treatment of congenital chest deformationsethio–pathogenesis, operative techniques and clinical results. Acta Chir. Orthop. Traumatol. Cech. 2003, 70, 207–213. [Google Scholar] [PubMed]
- Fokin, A.A.; Steuerwald, N.M.; Ahrens, W.A.; Allen, K.E. Anatomical, histologic, and genetic characteristics of congeni-tal chest wall deformities. Semin. Thorac. Cardiovasc. Surg. 2009, 21, 44–57. [Google Scholar] [CrossRef]
- David, V.L.; Izvernariu, D.A.; Popoiu, C.M.; Puiu, M.; Boia, E.S. Morphologic, morphometrical and histochemical pro-prieties of the costal cartilage in children with pectus excavatum. Rom. J. Morphol. Embryol. 2011, 52, 625–629. [Google Scholar]
- Tocchioni, F.; Ghionzoli, M.; Calosi, L.; Guasti, D.; Romagnoli, P.; Messineo, A. Rib Cartilage Characterization in Patients Affected by Pectus Excavatum. Anat. Rec. Adv. Integr. Anat. Evol. Biol. 2013, 296, 1813–1820. [Google Scholar] [CrossRef] [PubMed]
- Kurkov, A.V.; Paukov, V.; Fayzullin, A.L.; Shekhter, A.B. Costal cartilage changes in children with pectus excavatum and pectus carinatum. Arkhiv. Patol. 2018, 80, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Kurkov, A.; Guller, A.; Fayzullin, A.; Fayzullina, N.; Plyakin, V.; Kotova, S.; Timashev, P.; Frolova, A.; Kurtak, N.; Pau-kov, V.; et al. Amianthoid transformation of costal cartilage matrix in children with pectus excavatum and pec-tus carinatum. PLoS ONE 2021, 16, e0245159. [Google Scholar] [CrossRef] [PubMed]
- Bardakhch’ian, E.; Chepurnoĭ, G.; Shamik, V. Ultrastructural changes of child rib cartilage in different deformations of chest cells. Arkhiv. Patologii 2001, 64, 40–45. [Google Scholar]
- Hall, A.C.; Horwitz, E.R.; Wilkins, R.J. The cellular physiology of articular cartilage. Exp. Physiol. 1996, 81, 535–545. [Google Scholar] [CrossRef]
- Coulson, W. Deformities of the chest. Lond. Med. Gaz. 1820, 4, 69–73. [Google Scholar]
- Sainsbury, H. Congenital Funnel Chest. Lancet 1947, 250, 615. [Google Scholar] [CrossRef]
- Eggel, W. Eine seltene Missbildung des Thorax. Virchow’s Archiv. 1870, 49, 230–236. [Google Scholar] [CrossRef]
- Williams, C.T. Congenital malformation of the thorax: Great depression of the sternum. Trans. Path Soc. 1872, 24, 50. [Google Scholar]
- Grunenthal, A. Ueber Trichterbrust; Inaug. Diss.: Berlin, Germany, 1888. [Google Scholar]
- Herbst, E. Zur Kasuistik der Trichterbrust. Deutsch. Arch. Klin. Med. 1887, 41, 308. [Google Scholar]
- Creswick, H.A.; Stacey, M.W.; Kelly, R.E., Jr.; Gustin, T.; Nuss, D.; Harvey, H.; Goretsky, M.J.; Vasser, E.; Welch, J.C.; Mitchell, K.; et al. Family study of the inheritance of pectus excavatum. J. Pediatr. Surg. 2006, 41, 1699–1703. [Google Scholar] [CrossRef]
- Goretsky, M.J.; Kelly, R.E., Jr.; Croitoru, D.; Nuss, D. Chest wall anomalies: Pectus excavatum and pectus carinatum. Adolesc. Med. Clin. 2004, 15, 455–471. [Google Scholar] [CrossRef]
- Horth, L.; Stacey, M.W.; Proud, V.K.; Segna, K.; Rutherford, C.; Nuss, D.; Kelly, R.E. Advancing our understanding of the inheritance and transmission of pectus excavatum. J. Pediatr. Genet. 2012, 1, 161–173. [Google Scholar]
- Kotzot, D.; Schwabegger, A.H. Etiology of chest wall deformities—A genetic review for the treating physician. J. Pediatr. Surg. 2009, 44, 2004–2011. [Google Scholar] [CrossRef]
- Dietz, H. Marfan Syndrome; GeneReviews® [Internet]; Adam, M.P., Ardinger, H.H., Pagon, R.A., Eds.; University of Washington: Seattle, WA, USA, 1993–2022. [Google Scholar]
- Loeys, B.L.; Dietz, H.C.; Braverman, A.C.; Callewaert, B.L.; de Backer, J.; Devereux, R.B.; Hilhorst-Hofstee, Y.; Jondeau, G.; Faivre, L.; Milewicz, D.M.; et al. The revised Ghent nosology for the Marfan syndrome. J. Med. Genet. 2010, 47, 476–485. [Google Scholar] [CrossRef]
- Antia, A.U. Familial skeletal cardiovascular syndrome (Holt-Oram) in a polygamous African family. Heart 1970, 32, 241–244. [Google Scholar] [CrossRef][Green Version]
- Allanson, J.E.; Roberts, A.E. Noonan Syndrome; Adam, M.P., Ardinger, H.H., Pagon, R.A., Eds.; University of Washington: Washington, DC, USA, 1993–2020. [Google Scholar]
- Miklovic, T.; Sieg, V.C. Ehlers Danlos Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Romanini, M.V.; Calevo, M.G.; Puliti, A.; Vaccari, C.; Valle, M.; Senes, F.; Torre, M. Poland syndrome: A proposed classification system and perspectives on diagnosis and treatment. Semin. Pediatr. Surg. 2018, 27, 189–199. [Google Scholar] [CrossRef]
- Bavinck, J.N.; Weaver, D.D. Subclavian artery supply disruption sequence: Hypothesis of a vascular etiology for Poland, Klippel-Feil, and Möbius anomalies. Am. J. Med. Genet. 1986, 23, 903–918. [Google Scholar] [CrossRef]
- Armon, K.; Bale, P. Identifying heritable connective tissue disorders in childhood. Practitioner 2012, 256, 19–24. [Google Scholar]
- Gurnett, C.A.; Alaee, F.; Bowcock, A.; Kruse, L.; Lenke, L.G.; Bridwell, K.H.; Kuklo, T.; Luhmann, S.J.; Dobbs, M.B. Genetic linkage localizes an adolescent idiopathic scoliosis and pectus excavatum gene to chromosome 18 q. Spine 2009, 34, E94–E100. [Google Scholar] [CrossRef]
- Karner, C.M.; Long, F.; Solnica-Krezel, L.; Monk, K.R.; Gray, R.S. Gpr126/Adgrg6 deletion in cartilage models idiopathic scoliosis and pectus excavatum in mice. Hum. Mol. Genet. 2015, 24, 4365–4373. [Google Scholar] [CrossRef]
- Hamann, J.; Aust, G.; Araç, D.; Engel, F.; Formstone, C.; Fredriksson, R.; Hall, R.; Harty, B.L.; Kirchhoff, C.; Knapp, B.; et al. International Union of Basic and Clinical Pharmacology. XCIV. Adhesion G Protein–Coupled Receptors. Pharmacol. Rev. 2015, 67, 338–367. [Google Scholar] [CrossRef]
- Paavola, K.J.; Sidik, H.; Zuchero, J.B.; Eckart, M.; Talbot, W.S. Type IV collagen is an activating ligand for the adhesion G protein–coupled receptor GPR126. Sci. Signal. 2014, 7, ra76. [Google Scholar] [CrossRef]
- Gudbjartsson, D.F.; Walters, G.B.; Thorleifsson, G.; Stefansson, H.; Halldorsson, B.V.; Zusmanovich, P.; Sulem, P.; Thorlacius, S.; Gylfason, A.; Steinberg, S.; et al. Many sequence variants affecting diversity of adult human height. Nat. Genet. 2008, 40, 609–615. [Google Scholar] [CrossRef]
- Seko, A.; Hara-Kuge, S.; Yamashita, K. Molecular cloning and characterization of a novel human galactose 3-O-sulfotransferase that transfers sulfate to gal beta 1—>3galNAc residue in O-glycans. J. Biol. Chem. 2001, 276, 25697–25704. [Google Scholar] [CrossRef]
- Wu, S.; Sun, X.; Zhu, W.; Huang, Y.; Mou, L.; Liu, M.; Li, X.; Li, F.; Li, X.; Zhang, Y.; et al. Evidence for GAL3ST4 mutation as the potential cause of pectus excavatum. Cell Res. 2012, 22, 1712–1715. [Google Scholar] [CrossRef]
- Heinegård, D.; Oldberg, Å. Structure and biology of cartilage and bone matrix noncollagenous macromolecules. FASEB J. 1989, 3, 2042–2051. [Google Scholar] [CrossRef]
- Tong, X.; Li, G.; Feng, Y. TINAG mutation as a genetic cause of pectus excavatum. Med. Hypotheses 2020, 137, 109557. [Google Scholar] [CrossRef]
- TINAG. Tubulointerstitial Nephritis Antigen. Available online: https://www.ncbi.nlm.nih.gov/gene?Db=gene&Cmd=ShowDetailView&TermToSearch=27283 (accessed on 12 December 2021).
- Jakowlev, K.; Livshits, G.; Kalichman, L.; Ben-Asher, E.; Malkin, I.; Lancet, D.; Kobyliansky, E. Search for hand osteoar-thritis susceptibility locus on chromosome 6p12.3-p12.1. Hum. Biol. 2007, 79, 1–14. [Google Scholar] [CrossRef]
- Shamberger, R.C. Congenital chest wall deformities. Curr. Probl. Surg. 1996, 33, 469–542. [Google Scholar] [CrossRef]
- Pilegaard, H.K. Growth and pectus excavatum: Is there a relation? Eur. J. Cardiothorac. Surg. 2016, 50, 1110. [Google Scholar] [CrossRef]
- Schamberger, R.C.; Welch, K.J. Chest Wall Deformities in Ashcraft KW, 2nd ed.; Holder, T.M., Ed.; Saunders Compmany: Philadelphia, PA, USA, 1986; pp. 146–150. [Google Scholar]
- Schamberger, R.C. Congenital Chest Wall Deformities, 6th ed.; Grosfeld, J.L., O’Neil, J.A., Jr., Fonkalsrud, E.W., Corab, A.G., Eds.; Mosby: Philadelphia, PA, USA, 2006; pp. 894–930. [Google Scholar]
- Peltomäki, T.; Häkkinen, L. Growth of the ribs at the costochondral junction in the rat. J. Anat. 1992, 181, 259–264. [Google Scholar]
- Nakaoka, T.; Uemura, S.; Yano, T.; Nakagawa, Y.; Tanimoto, T.; Suehiro, S. Does overgrowth of costal cartilage cause pectus excavatum? A study on the lengths of ribs and costal cartilages in asymmetric patients. J. Pediatr. Surg. 2009, 44, 1333–1336. [Google Scholar] [CrossRef]
- Nakaoka, T.; Uemura, S.; Yoshida, T.; Tanimoto, T.; Miyake, H. Overgrowth of costal cartilage is not the etiology of pec-tus excavatum. J. Pediatr. Surg. 2010, 45, 2015–2018. [Google Scholar] [CrossRef]
- David, V.L.; Cerbu, S.; Haragus, H.; Popoiu, M.C.; Stanciulescu, C.M.; Cozma, G.; Burlac, O.; Boia, E.S. Costal Cartilages Do Not Overgrow in Patients with Pectus Excavatum. Med. Princ. Pract. 2016, 25, 533–538. [Google Scholar] [CrossRef]
- Karakılıç, A.; Karaçam, V.; Ersöz, H.; Ağababaoğlu, I.; Ulugün, F.I.; Şanlı, A. Determination of severity of deformity with rib length to costal cartilage length ratio in thorax deformities. Turk. J. Thorac. Cardiovasc. Surg. 2018, 26, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Eisinger, R.S.; Harris, T.; Rajderkar, D.A.; Islam, S. Against the Overgrowth Hypothesis: Shorter Costal Cartilage Lengths in Pectus Excavatum. J. Surg. Res. 2019, 235, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Kim, T.H.; Haam, S.; Lee, S. Rib overgrowth may be a contributing factor for pectus excavatum: Evaluation of prepubertal patients younger than 10years old. J. Pediatr. Surg. 2015, 50, 1945–1948. [Google Scholar] [CrossRef]
- Kondo, S.; Takagi, D.; Osaga, S.; Okuda, K.; Nakanishi, R. The costochondral length in patients with pectus excavatum is longer than that of the normal thorax. Pediatr. Surg. Int. 2020, 36, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Haje, S.A.; Harcke, H.T.; Bowen, J.R. Growth disturbance of the sternum and pectus deformities: Imaging studies and clinical correlation. Pediatr Radiol. 1999, 29, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Zavala-Garcia, A.; Teekappanavar, N.; Lee, C.; Idowu, O.; Kim, S. Measurement of sternal curvature angle on patients with pectus excavatum. Pediatr Surg Int. 2017, 33, 65–67. [Google Scholar] [CrossRef]
- Haje, D.P.; Teixeira, K.O.; Silva, M.; Volpon, J.B.; Mendlovitz, P.S.; Dolabela, P. Analysis of sternal curvature patterns in patients with pectus and control. Acta Ortop Bras. 2021, 29, 258–262. [Google Scholar] [CrossRef]
- Wang, R.; Yang, W.; Cai, L.; Yang, J.; Xiang, X.; Zhang, C.; Jiang, Q.; Yang, Y.; Chen, Z. Establishment of a rabbit model of pectus excavatum. Int. J. Clin. Exp. Med. 2017, 10, 6429–6436. [Google Scholar]
- David, V.-L.; Ciornei, B.; Horhat, F.-G.; Amaricai, E.; Horhat, I.-D.; Hoinoiu, T.; Boia, E.-S. Rat Animal Model of Pectus Excavatum. Life 2020, 10, 96. [Google Scholar] [CrossRef]
- David, V.L.; Stanciulescu, M.C.; Horhat, F.G.; Sharma, A.; Kundnani, N.R.; Ciornei, B.; Stroescu, R.F.; Popoiu, M.C.; Boia, E. S: Costal cartilage overgrowth does not induce pectus-like deformation in the chest wall of a rat model. Exp. Ther. Med. 2022, 23, 146. [Google Scholar] [CrossRef]
| Author | Surgical Procedure | Etiological Hypothesis | Fate |
|---|---|---|---|
| Meyer 1911 [13] | First successful repair of PE Unilateral costal cartilage resection | Costochondral origin |
|
| Brown 1940 [22] | Section of the sternal diaphragmatic insertion | Diaphragmatic traction |
|
| Ravitch 1949 [26] | Open correction Bilateral costal cartilage resection Sternal osteotomy Multiple improvements | Substernal ligament |
|
| |||
| |||
| |||
| |||
| |||
| Wada 1961 [41] | Sternal turnover Complete sternal detachment | Cartilage Overgrowth |
|
| |||
| Allen et al. 1979 [35] | Silicon implant The defect is filled with a silicon implant | - |
|
| |||
| Nuss et al. 1998 [34] | Minimal invasive (MIRPE) Thoracoscopic approach No cartilage resection | Cartilage Overgrowth |
|
| Isakov et al. 1980 [42] Harrison et al. 2007 [43,44] | Minimover—magnetic implant Substernal placement of a magnet Second magnet on external corset Correction by magnetic attraction | Cartilage Overgrowth |
|
| Weber et al. 2006 [46,47] | Elastic correction Minimal cartilage resection Insertion of elastic thoracic bar | Cartilage Overgrowth | Limited experience |
| Method | Findings | Literature Report | |
|---|---|---|---|
| 1 | LM | Regressive-cataplastic transformations | Geisbe et al. 1967 [51,52,53] |
| BCH | Increased activity of catabolic enzymes of mucopolysaccharides | ||
| 2 | LM | Asbestiform degeneration and transformation zones | Tischer et al. 1968 [54] |
| 3 | BCH | Low Zn levels | Rupprecht et al. 1987 [55] |
| Increased Mg and Ca | |||
| EM | Presence of vascular channels | ||
| Areas of normal chondrocytes alternating with areas of degenerative chondrocytes with long-spacing collagen | |||
| 4 | LM | Large acellular zones, map-like areas, unmasked chondrin fibers, and “marrow” cavities. | Kuritsyn et al. 1987 [56] |
| Signs of early aging | |||
| 5 | LM | Chondrocytes increases within the single chondrons | Rupprecht et al. 1989 [57] |
| 6 | BCH | Mutation in the N-terminal region of alpha 1 chain of collagen I | Sokolov et al. 1989 [58] |
| Decreased stability of collagen II | |||
| 7 | BCH | Deteriorations in the structure of collagen I, resulting in a lower stability of collagen II | Sokolov et al. 1990 [59] |
| Similar findings in a patient with Ehlers-Danlos syndrome and PE | |||
| 8 | BCH | Increased content of collagen | Tsvetkova et al. 1988 [60] |
| Decreased content of immobilized water | |||
| Premature aging of the cartilages | |||
| 9 | BCH | Synthesis of collagen was lower in skin fibroblasts of patients with PE | Tsvetkova et al. 1990 [61] |
| PE is a connective tissue disease | |||
| 10 | BCH | High levels of pyridinoline | Prozorovskaya et al. 1991 [62] |
| Modified soluble/insoluble collagen ratio | |||
| Increased percentage of endogenous collagenolysis compared to controls | |||
| 11 | CHG | Normal hydroxylysylpyridinoline and lysylpyridinoline crosslinks in PE patients (abnormal in Ehlers–Danlos and Marfan) | Borisova et al. 1993 [63,64] |
| 12 | LM | Unremarkable cellularity | Feng et al. 2001 [65] |
| Unequal and patchy staining | |||
| BCH | Decreased biomechanical stability of the cartilage | ||
| Diminished strength at tension, compression, and flexure | |||
| EM | Collagen fibrils distributed unequally and arranged irregularly in deep zones of the cartilage | ||
| 13 | LM | Disturbances in endochondral ossification and a growth of costal cartilage | Serafin et al. 2013 [66] |
| 14 | LM | Greater cellularity, more variable cellular distribution, larger vessel clusters, and more frequent myxoid matrix degeneration and focal necrosis | Fokin et al. 2009 [67] |
| 15 | LM | Unremarkable chondrocytes | David et al. 2011 [68] |
| Unremarkable collagen fibers | |||
| PE cartilages have a lower content of strongly sulfated mucopolysaccharides, indicating an immature pattern | |||
| 16 | LM | Great morphologic and morphometric variability of the cartilage | Tocchioni et al. 2013 [69] |
| LM | PE cartilage are almost exclusively alcianophilic | ||
| ICH | No differences between control and PE | ||
| EM | No specific findings for PE | ||
| 17 | LM | Decreased number of cartilage lacunae in PE | Kurkov et al. 2018 [70] |
| Decreased number of cartilage channels | |||
| 18 | LM | Amianthoid transformation present in both PE and normal cartilages | Kurkov et al. 2021 [71] |
| Amianthoid fibers are thicker collagen II fibers | |||
| ICH | Type II collagen present, I and III absent, no differences between PE, PC, and normal | ||
| EM | Thicker matrix fibers in PE samples | ||
| Higher incidence of amianthoid transformation areas in PE and PC |
| Agreed Upon | The disease may be present at birth, but it has an uneven progression through life. |
| Rapid progression of the deformity occurs during the prepubertal growth spurt, while the deformation becomes stable in adulthood, suggesting a direct linkage between skeletal growth and PE. | |
| Familial aggregation of PE. | |
| Most PE is non-syndromic. | |
| PE is frequently associated with several genetic syndromes that involve defects of the hyaline cartilage. | |
| The structure and the physical proprieties of the costal cartilages in patients with PE are severely disturbed. | |
| The diaphragm muscle, excessive traction, or fibrous bands are not involved in the etiopathogenesis of PE. | |
| There is no relation between the metabolism of vitamin D and PE, meaning that rickets are not responsible for PE deformation. | |
| Controversial | The results of the histologic studies are disparate and sometimes in contradiction with each other, with respect to the different eras and different methods of investigation. |
| Structural weakness in the costal cartilages causes the collapse of the anterior chest wall, meaning that such weakness is an etiologic factor of PE. | |
| Overgrowing lower costal cartilages grow excessively and push the sternum backwards, meaning that such overgrowth is the etiologic factor of PE. | |
| The mechanisms of inheritance include autosomal recessive (most likely), autosomal dominant, and X-linked. | |
| The genetic defect leading to the PE deformation is related to Chromosomal 5, 15, 17, or 18. | |
| The shape and length of the costal cartilages are different among PE versus normal subjects. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
David, V.L. Current Concepts in the Etiology and Pathogenesis of Pectus Excavatum in Humans—A Systematic Review. J. Clin. Med. 2022, 11, 1241. https://doi.org/10.3390/jcm11051241
David VL. Current Concepts in the Etiology and Pathogenesis of Pectus Excavatum in Humans—A Systematic Review. Journal of Clinical Medicine. 2022; 11(5):1241. https://doi.org/10.3390/jcm11051241
Chicago/Turabian StyleDavid, Vlad Laurentiu. 2022. "Current Concepts in the Etiology and Pathogenesis of Pectus Excavatum in Humans—A Systematic Review" Journal of Clinical Medicine 11, no. 5: 1241. https://doi.org/10.3390/jcm11051241
APA StyleDavid, V. L. (2022). Current Concepts in the Etiology and Pathogenesis of Pectus Excavatum in Humans—A Systematic Review. Journal of Clinical Medicine, 11(5), 1241. https://doi.org/10.3390/jcm11051241






