Influence of Ultrasound Examination on Diagnosis and Treatment of Temporomandibular Disorders
Abstract
:1. Introduction
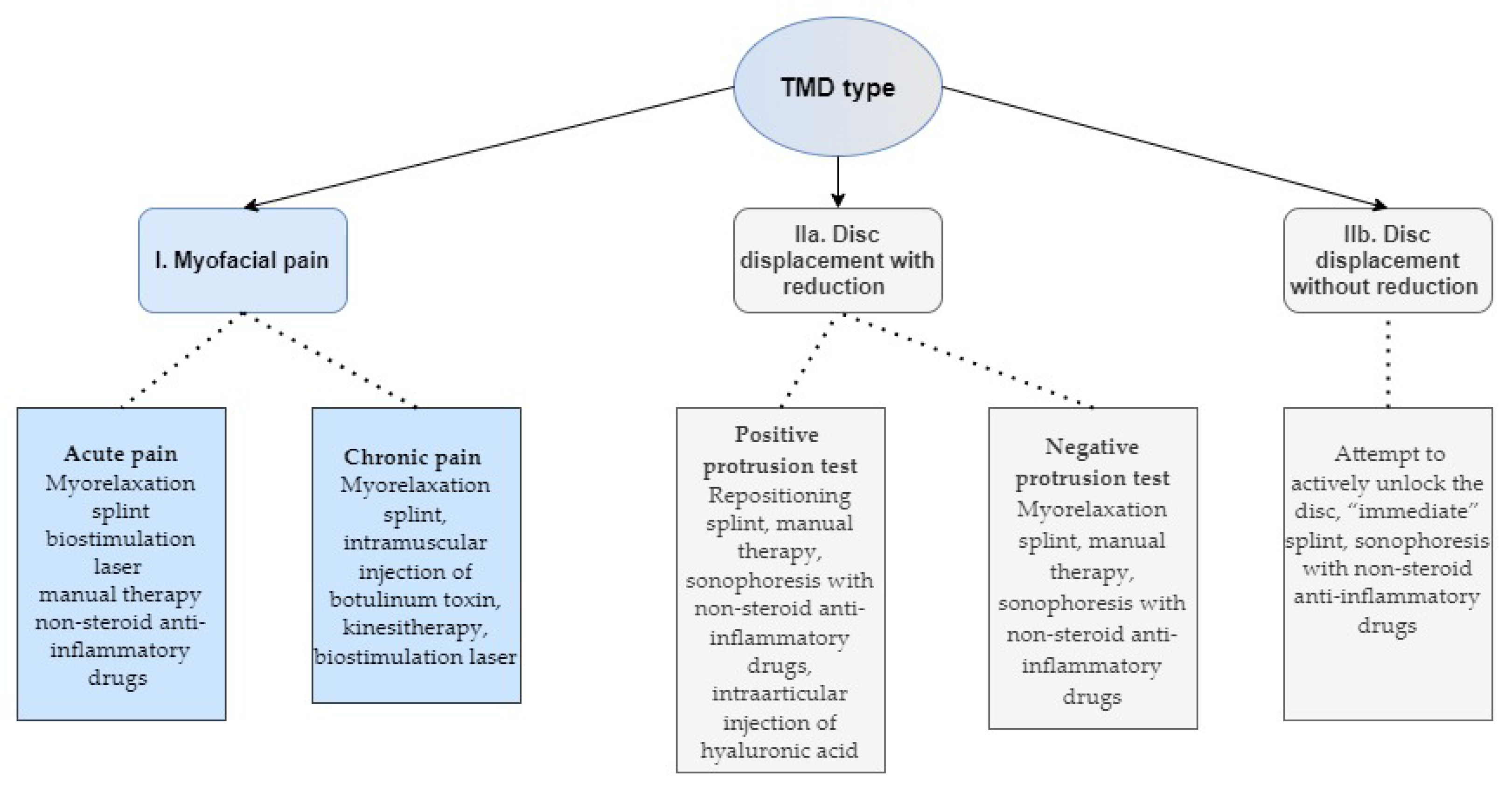
2. Materials and Methods
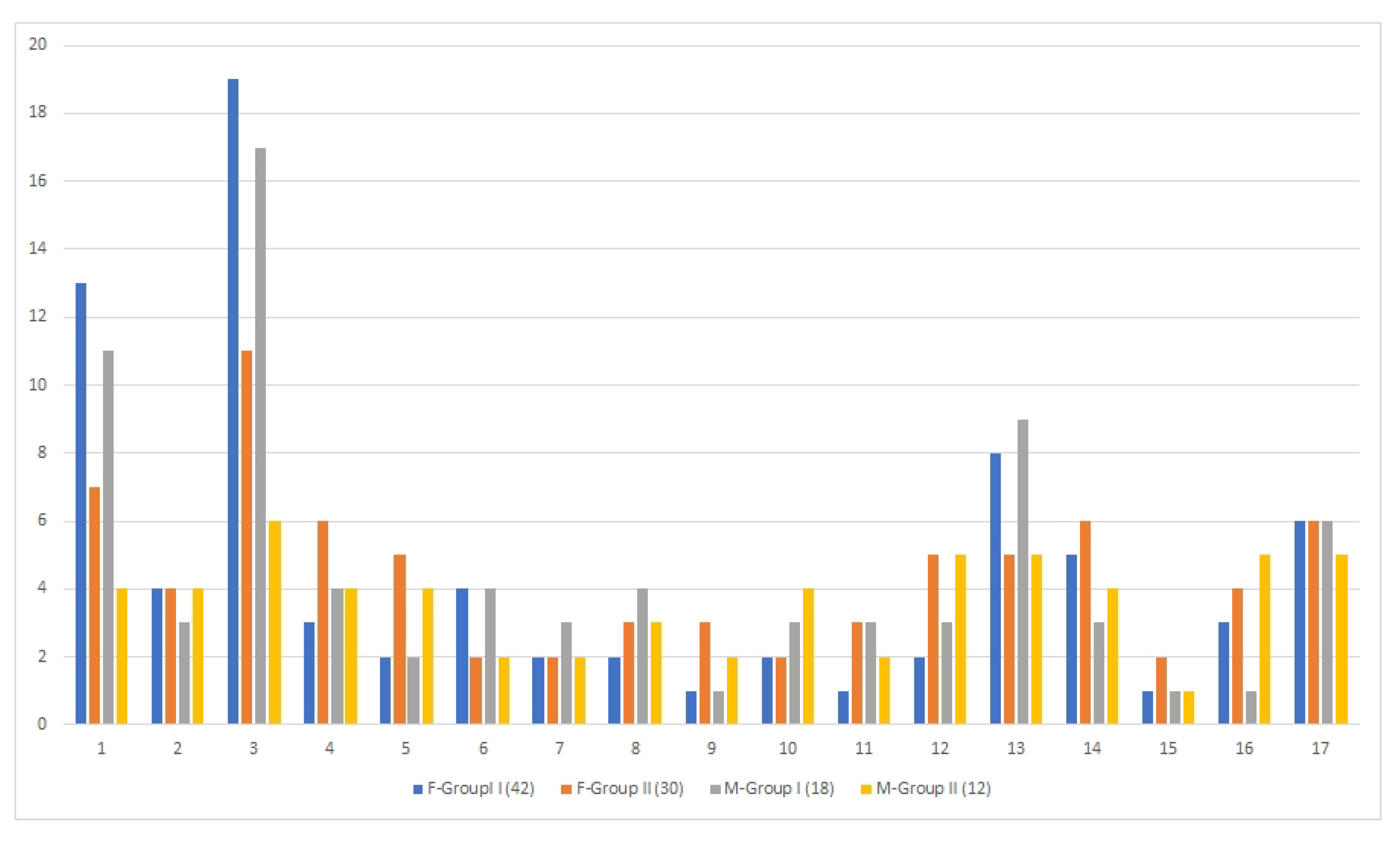
3. Results
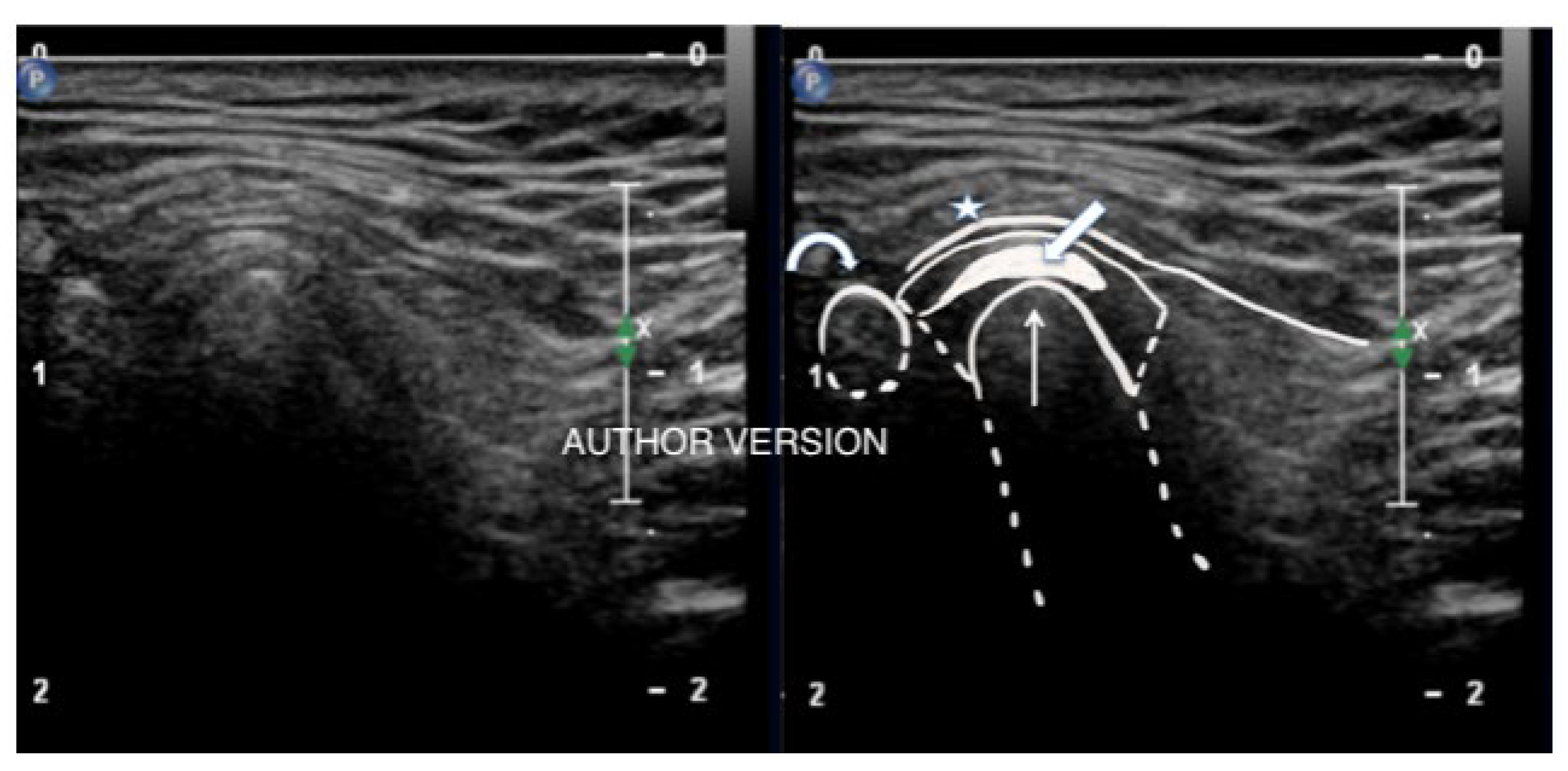
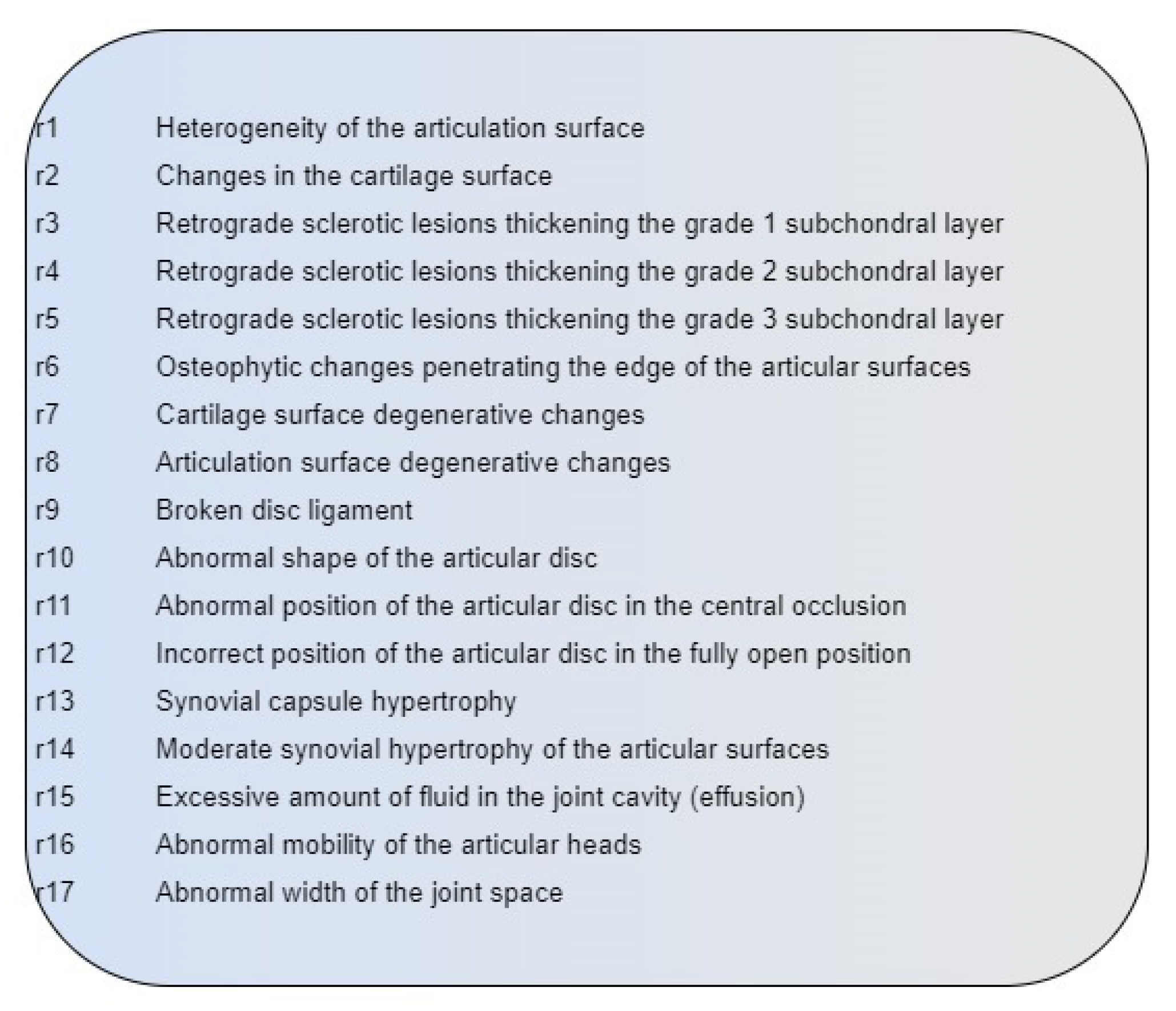
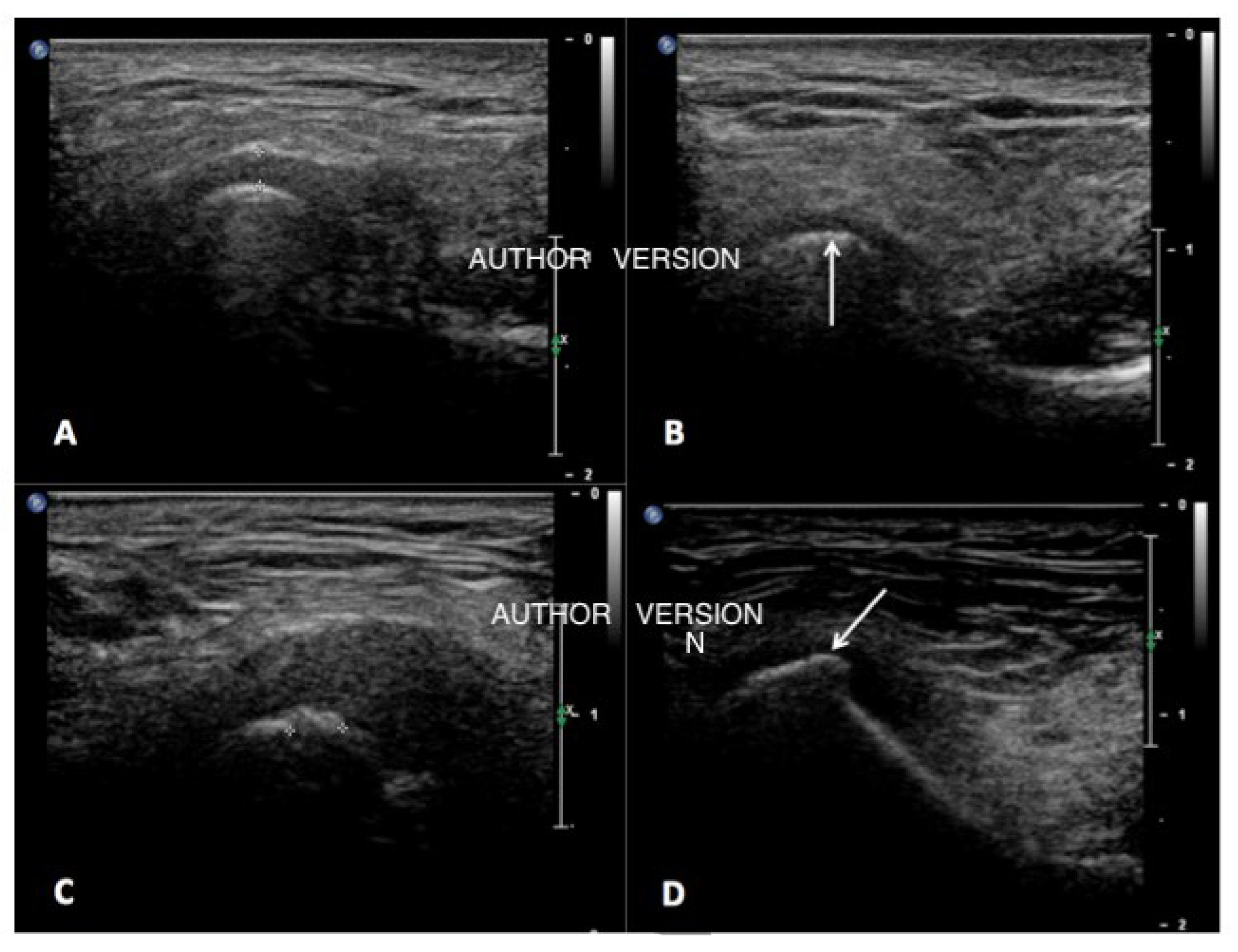
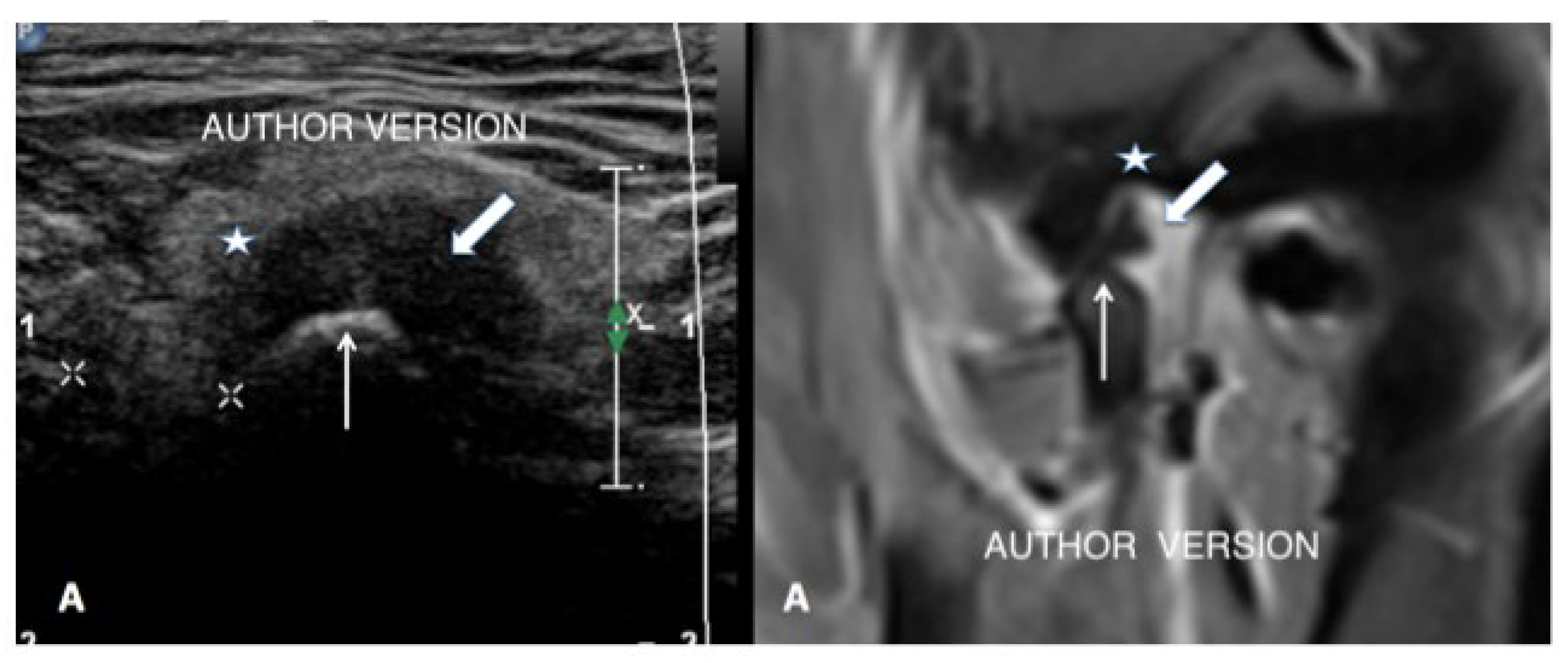
Ultrasound Examinations Results
4. Discussion
5. Conclusions
- Ultrasound results collected in this study showed a higher prevalence of pathomorphological TMJ changes in the myofascial pain group than expected based on clinical examination.
- Further studies based on larger sample size are recommended to compare and verify if ultrasound imaging can be an effective new method supporting diagnoses of temporomandibular disorders.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 2nd ed; Czelej: Lublin, Poland, 2018; pp. 26–45, 173–189. [Google Scholar]
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis and treatment of temporomandibular disorder. Dent. Clin. N. Am. 2013, 57, 465–479. [Google Scholar] [CrossRef]
- Bender, S.D. Orofacial pain and headache: A review and look at the commonalities. Curr. Pain Headache Rep. 2014, 18, 400. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, M.; Otonari-Yamamoto, M.; Sano, T.; Fujikura, M.; Wakoh, M. Diagnosis of retrodiscal tissue in painful temporomandibular joint (TMJ) by fluid-attenuated inversion recovery (FLAIR) signal intensity. CRANIO® 2015, 33, 271–275. [Google Scholar] [CrossRef]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of Temporomandibular disorder. Am. Fam. Phys. 2015, 91, 376–386. [Google Scholar]
- De Freitas, R.F.C.P.; Ferreira, M.Â.F.; Barbosa, G.A.S.; Calderon, P.S. Counselling and self-management therapies for temporomandibular disorders: A systematic review. J. Oral Rehabil. 2013, 40, 864–874. [Google Scholar] [CrossRef]
- Bonjardim, L.; Gavido, M.; Pereira, L.; Castelo, P.; Garcia, R. Signs and symptoms of temporomandibular disorders in adolescensts. Braz. Oral Res. 2005, 19, 93–98. [Google Scholar] [CrossRef]
- Klatkiewicz, T.; Gawriołek, K.; Podudek Radzikowska, M.; Czajka-Jakubowska, A. Ultrasounography in the diagnosis of temporomandibular disorder: A meta-analysis. Med. Sci. Monit. 2018, 24, 812–817. [Google Scholar] [CrossRef] [Green Version]
- Jank, S.; Emshoff, R.; Norer, B.; Missmann, M.; Nicasi, A.; Strobl, H.; Gassner, R.; Rudisch, A.; Bodner, G. Diagnostic quality of dynamic high-resolution ultrasonography of the TMJ: A pilot study. Int. J. Oral Maxillofac. Surg. 2005, 34, 132–137. [Google Scholar] [CrossRef]
- Cakir-Ozkan, N.; Sarikaya, B.; Erkorkmaz, U.; Aktürk, Y. Ultrasonographic evaluation of disc displacement of the temporomandibular joint compared with magnetic resonance imaging. J. Oral Maxillofac. Surg. 2010, 68, 1075–1080. [Google Scholar] [CrossRef]
- Kundu, H.; Basavaraj, P.; Kote, S.; Singla, A.; Singh, S. Assessment of TMJ Disorders Using Ultrasonography as a Diagnostic Tool: A Review. J. Clin. Diagn. Res. 2013, 7, 3116–3120. [Google Scholar] [CrossRef]
- Kurita, H.; Uehara, S.; Yokochi, M.; Nakatsuka, A.; Kobayashi, H.; Kurashina, K. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int. J. Oral Maxillofac. Surg. 2006, 35, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Su, N.; Yang, X.; Yang, X.; Shi, Z.; Li, L. Ultrasonography for the detection of disc displacement of Temporomandibular Joint: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2012, 70, 1300–1309. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Detamore, M.S.; Mercuri, L. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.M.; Packota, G.; Major, P.W.; Flores-Mir, C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: A systematic review. Dentomaxillofac. Radiol. 2008, 37, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Siva Kalyan, U.; Moturi, K.; Padma Rayalu, K. The Role of Ultrasound in Diagnosis of Temporomandibular Joint Disc Displacement: A Case-Control Study. J. Maxillofac. Oral Surg. 2018, 17, 383–388. [Google Scholar] [CrossRef]
- Byahatti, S.M.; Ramamurthy, B.R.; Mubeen, M.; Agnihothri, P.G. Assessment of diagnostic accuracy of high-resolution ultrasonography in determination of temporomandibular joint internal derangement. Indian J. Dent. Res. 2010, 21, 189–194. [Google Scholar] [CrossRef]
- Emshoff, R.; Jank, S.; Rudisch, A.; Bodner, G. Are High- Resolution Ultrasonographic signs of disc displacement valid? J. Oral Maxillofac. Surg. 2002, 60, 623–628. [Google Scholar] [CrossRef]
- Emshoff, R.; Jank, S.; Bertram, S.; Rudisch, A.; Bodner, G. Disk displacement of the temporomandibular joint: Sonography versus MR imaging. AJR Am. J. Roentgenol. 2002, 178, 1557–1562. [Google Scholar] [CrossRef]
- Osiewicz, M.A.; Lobbezoo, F.; Loster, B.W.; Wilkosz, M.; Naeije, M.; Ohrbach, R. Research diagnostic criteria for temporomandibular disorders (RDC/TMD)-the Polish version of a dual axis system for the diagnosis of TMD-RDC/TMD form. J. Stom. 2013, 66, 576–649. [Google Scholar] [CrossRef]
- Pihut, M.; Kazana, P.; Wiśniewska, G. Assessment of the effectiveness of sonophoresis in the treatment of TMD. Prot. Stomatol. 2011, 61, 91–97. [Google Scholar]
- Rai, S.; Ranjan, V.; Misra, D.; Panjwani, S. Management oh myofascial pain by therapeutic ultrasound and transcutaneous electrical nerve stimulation: A comparative study. Eur. J. Dent. 2016, 10, 46–53. [Google Scholar]
- Mello Junior, C.F.; Saito, O.D.; Guimarães Filho, H.A. Sonographic evaluation of temporomandibular joint internal disorder. Radiol. Bras. 2011, 44, 355–359. [Google Scholar] [CrossRef] [Green Version]
- Razek, A.A.; Al Mahdy Al Belasy, F.; Ahmed, W.M.; Haggag, M.A. Assessment of articular disc displacement of temporomandibular joint with ultrasound. J. Ultrasound 2014, 18, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, N.; van Wijk, A.J.; Visscher, C.M.; Lobbezoo, F.; van der Heijden, G.J.M.G. Diagnostic value of ultrasonography for the detection of disc displacements in the temporomandibular joint: A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2599–2614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yılmaz, D.; Kamburoğlu, K. Comparison of the effectiveness of high resolution ultrasound with MRI in patients with temporomandibular joint dısorders. Dentomaxillofac. Radiol. 2019, 48, 20180349. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.T.; Pacheco-Pereira, C.; Flores-Mir, C.; Le, L.H.; Jaremko, J.L.; Major, P.W. Diagnostic ultrasound assessment of temporomandibular joints: A systematic review and meta-analysis. Dentomaxillofac. Radiol. 2019, 48, 20180144. [Google Scholar] [CrossRef]
- Hechler, B.L.; Phero, J.A.; Van Mater, H.; Matthews, N.S. Ultrasound versus magnetic resonance imaging of the temporomandibular joint in juvenile idiopathic arthritis: A systematic review. Int. J. Oral Maxillofac. Surg. 2018, 47, 83–89. [Google Scholar] [CrossRef]
- Manfredini, D.; Guarda-Nardini, L. Ultrasonography of the temporomandibular joint: A literature review. Int. J. Oral Maxillofac. Surg. 2009, 38, 1229–1236. [Google Scholar] [CrossRef]
- Sivri, M.B.; Ozkan, Y.; Pekiner, F.N.; Gocmen, G. Comparison of ultrasound-guided and conventional arthrocentesis of the temporomandibular joint. Br. J. Oral Maxillofac. Surg. 2016, 54, 677–681. [Google Scholar] [CrossRef]
- Friedman, S.N.; Grushka, M.; Beituni, H.K.; Rehman, M.; Bressler, H.B.; Friedman, L. Advanced Ultrasound Screening for Temporomandibular Joint (TMJ) Internal Derangement. Radiol. Res. Pract. 2020, 2020, 1809690. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pihut, M.; Gala, A.; Obuchowicz, R.; Chmura, K. Influence of Ultrasound Examination on Diagnosis and Treatment of Temporomandibular Disorders. J. Clin. Med. 2022, 11, 1202. https://doi.org/10.3390/jcm11051202
Pihut M, Gala A, Obuchowicz R, Chmura K. Influence of Ultrasound Examination on Diagnosis and Treatment of Temporomandibular Disorders. Journal of Clinical Medicine. 2022; 11(5):1202. https://doi.org/10.3390/jcm11051202
Chicago/Turabian StylePihut, Małgorzata, Andrzej Gala, Rafał Obuchowicz, and Karolina Chmura. 2022. "Influence of Ultrasound Examination on Diagnosis and Treatment of Temporomandibular Disorders" Journal of Clinical Medicine 11, no. 5: 1202. https://doi.org/10.3390/jcm11051202
APA StylePihut, M., Gala, A., Obuchowicz, R., & Chmura, K. (2022). Influence of Ultrasound Examination on Diagnosis and Treatment of Temporomandibular Disorders. Journal of Clinical Medicine, 11(5), 1202. https://doi.org/10.3390/jcm11051202








