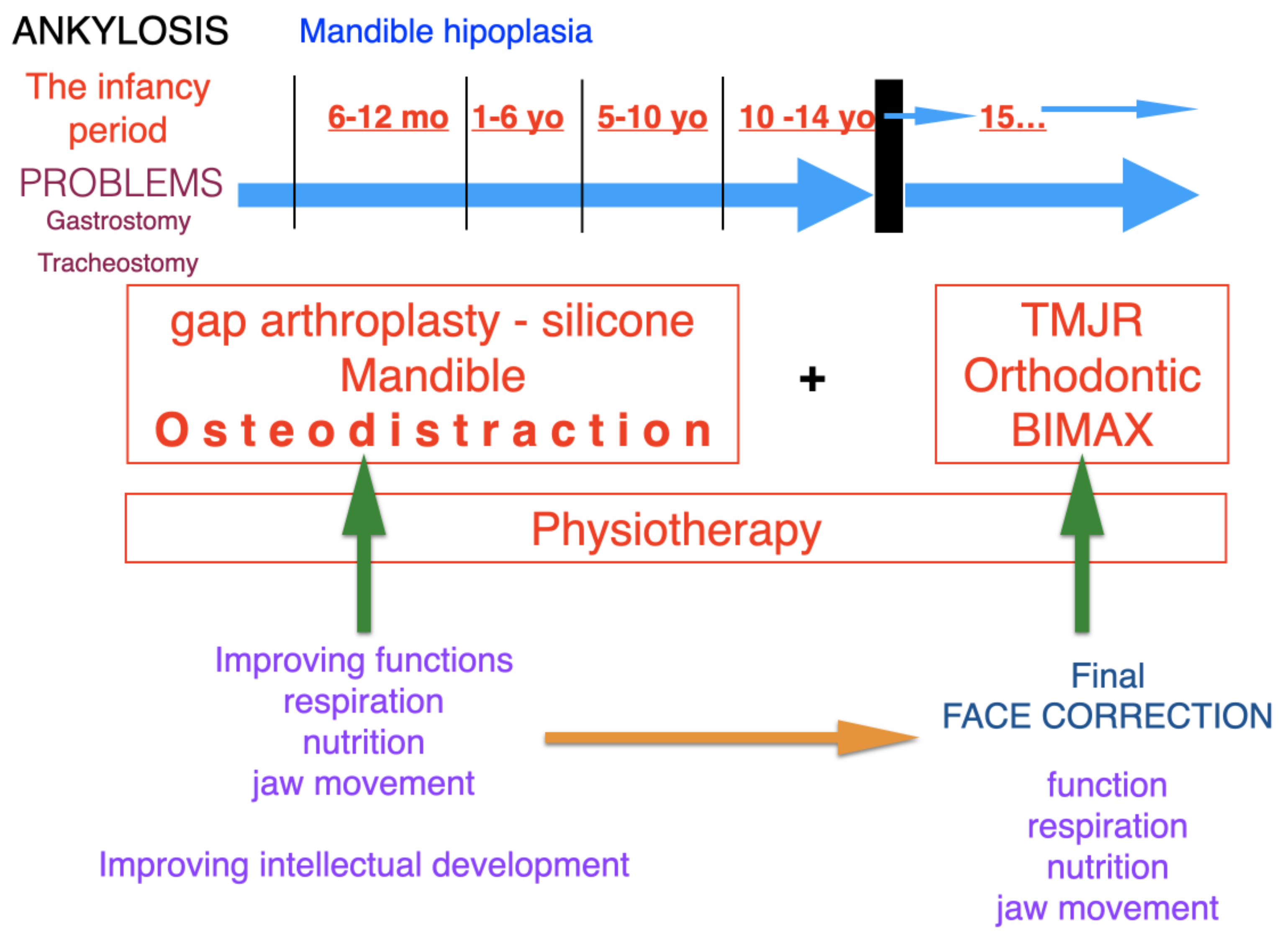
Protocol for Multi-Stage Treatment of Temporomandibular Joint Ankylosis in Children and Adolescents
Abstract
:1. Introduction
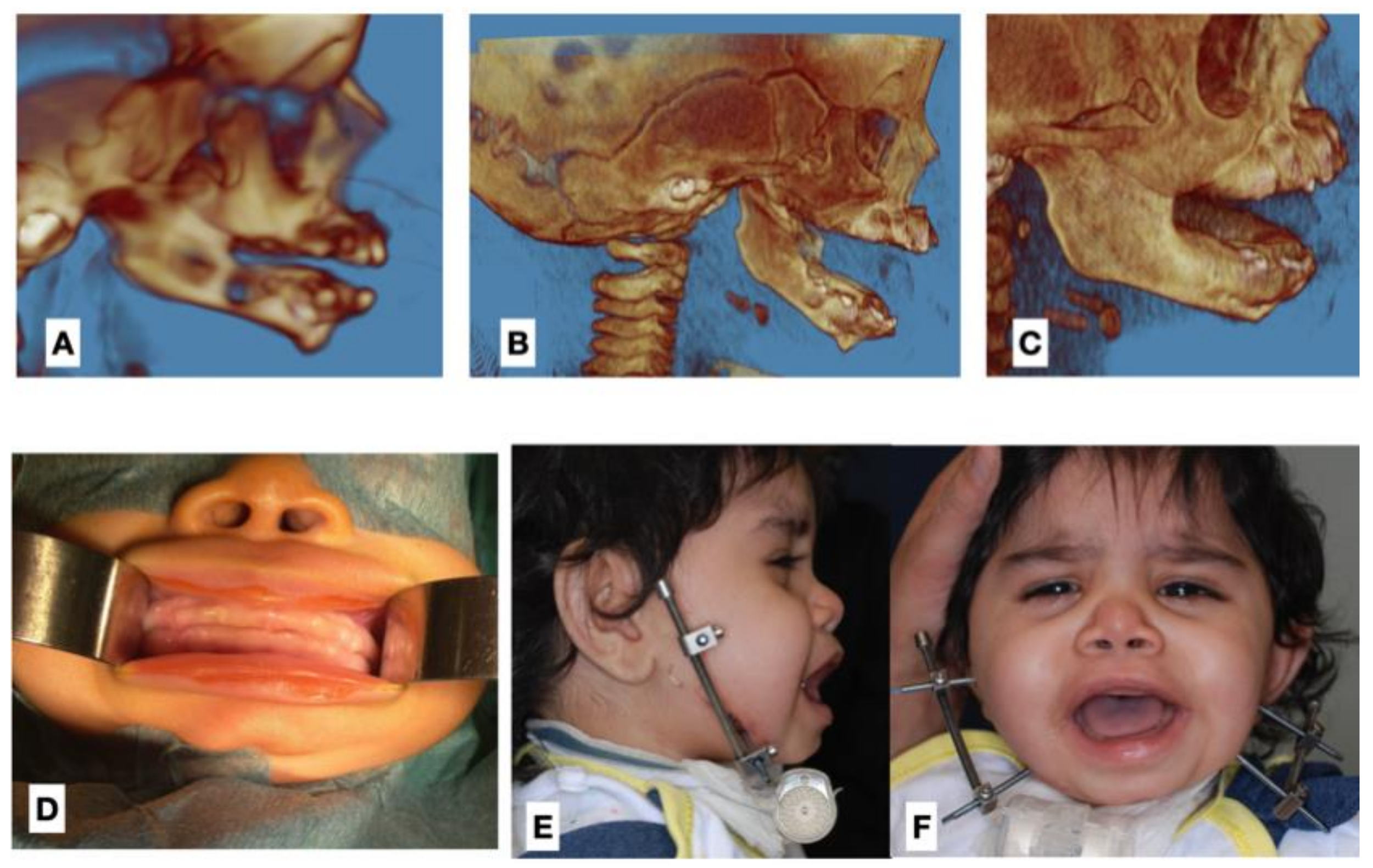
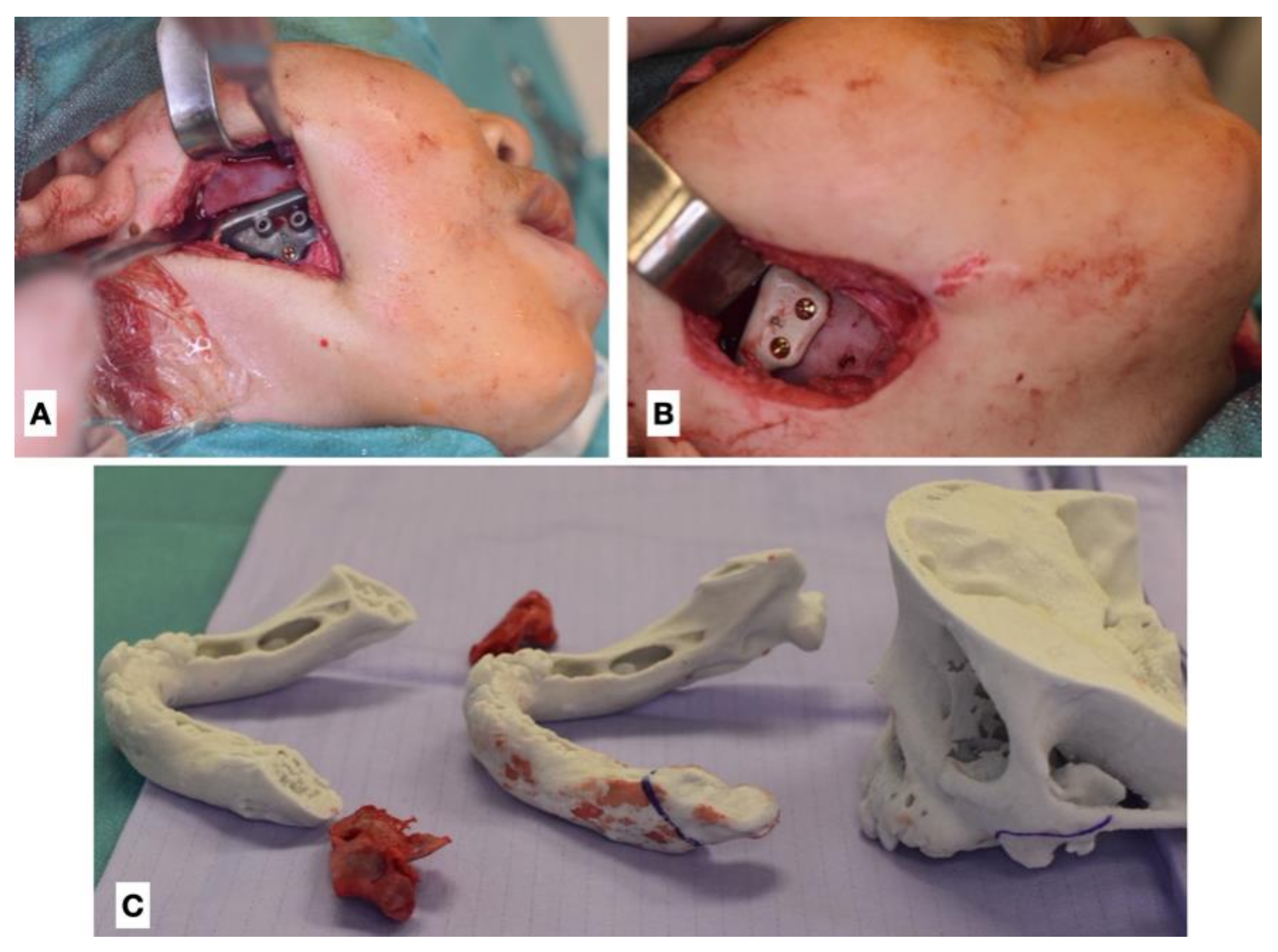
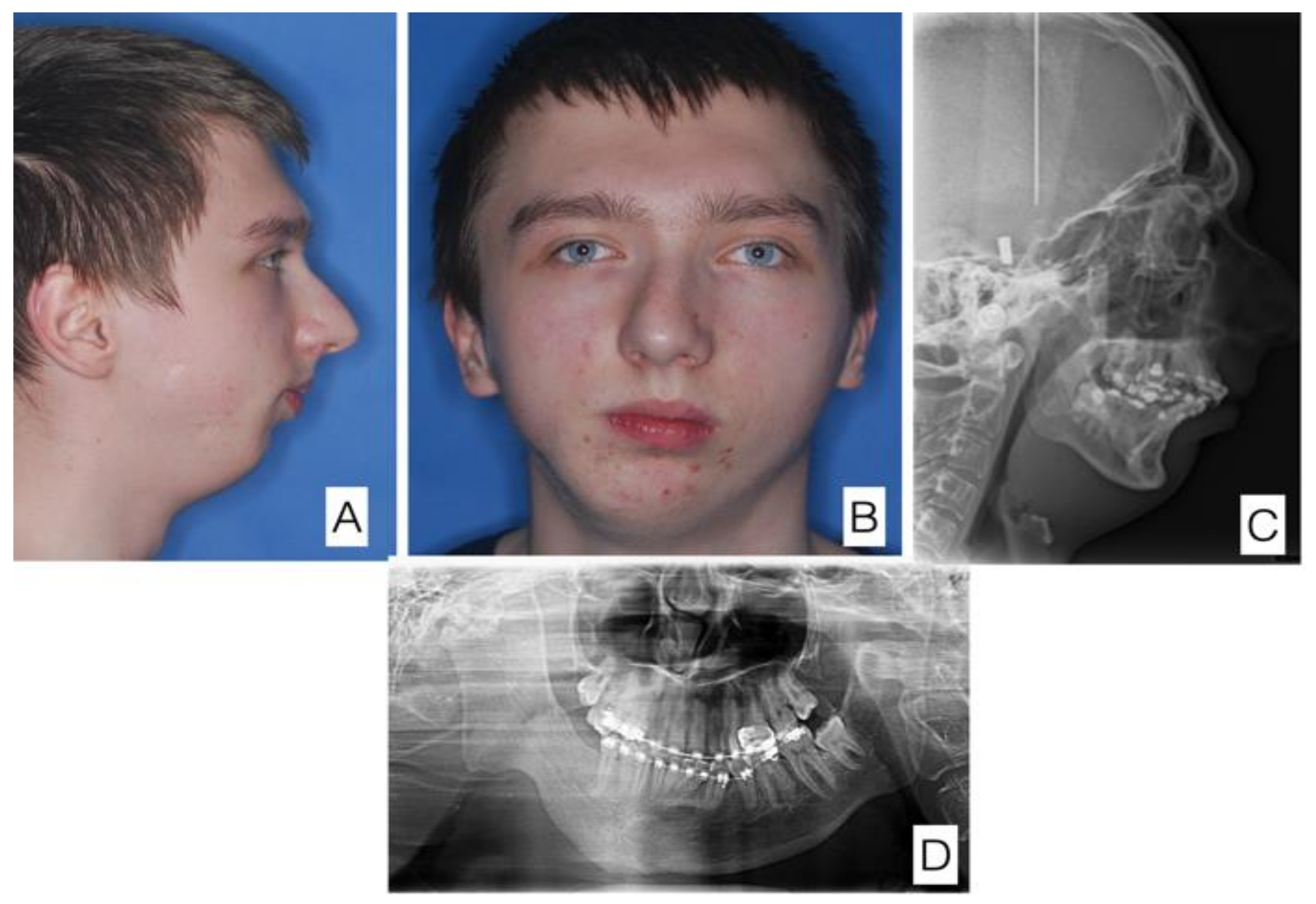
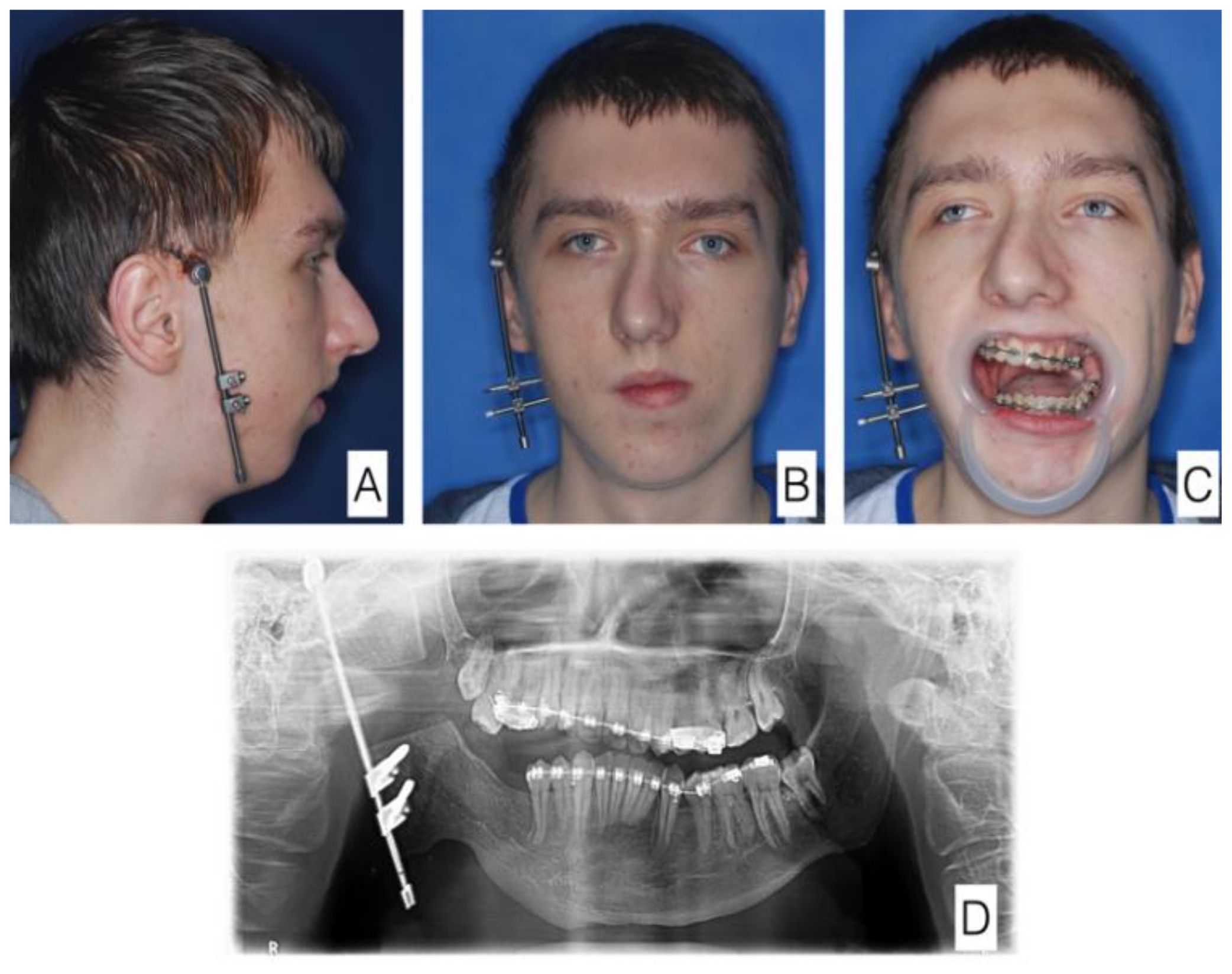
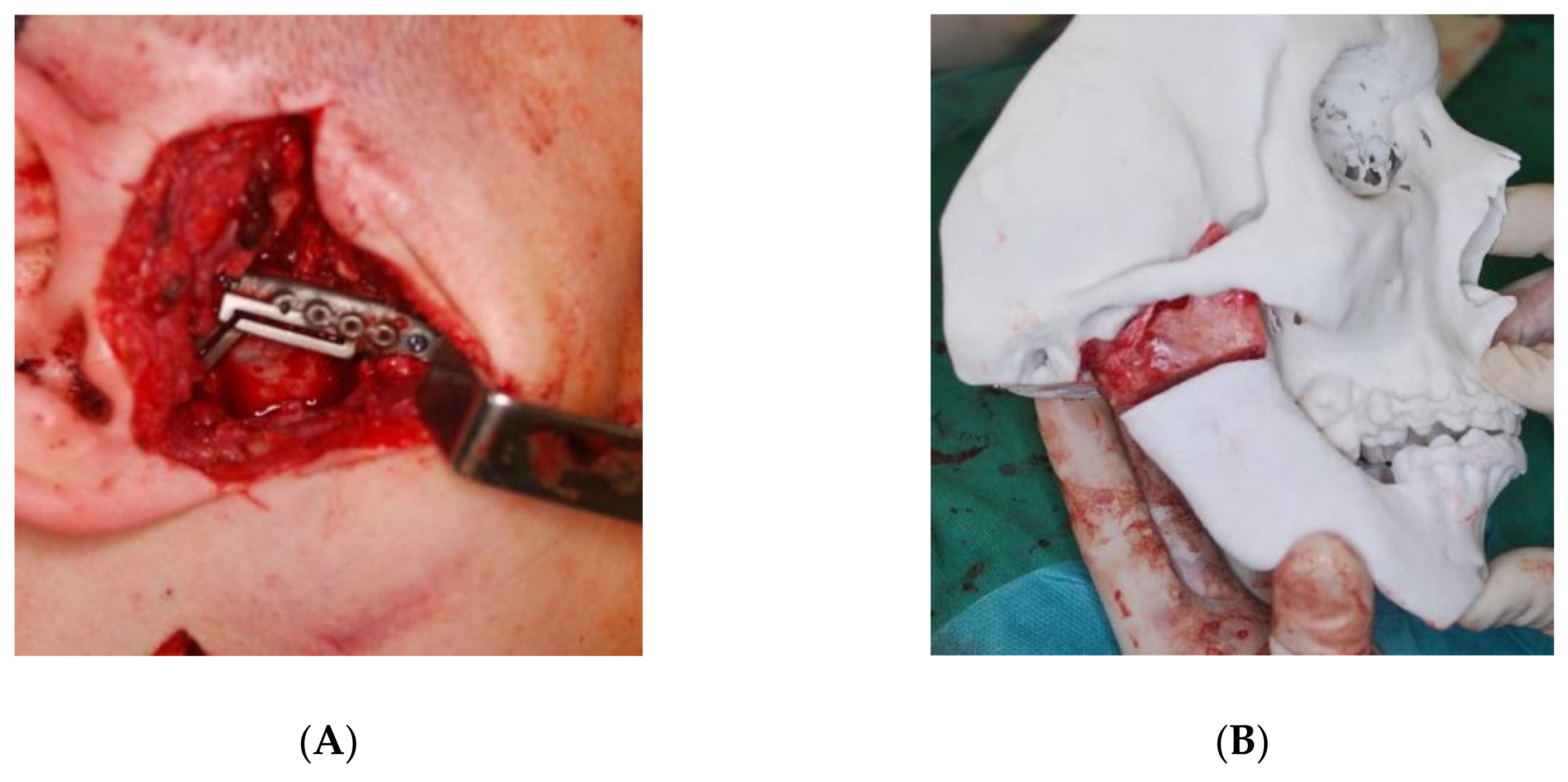
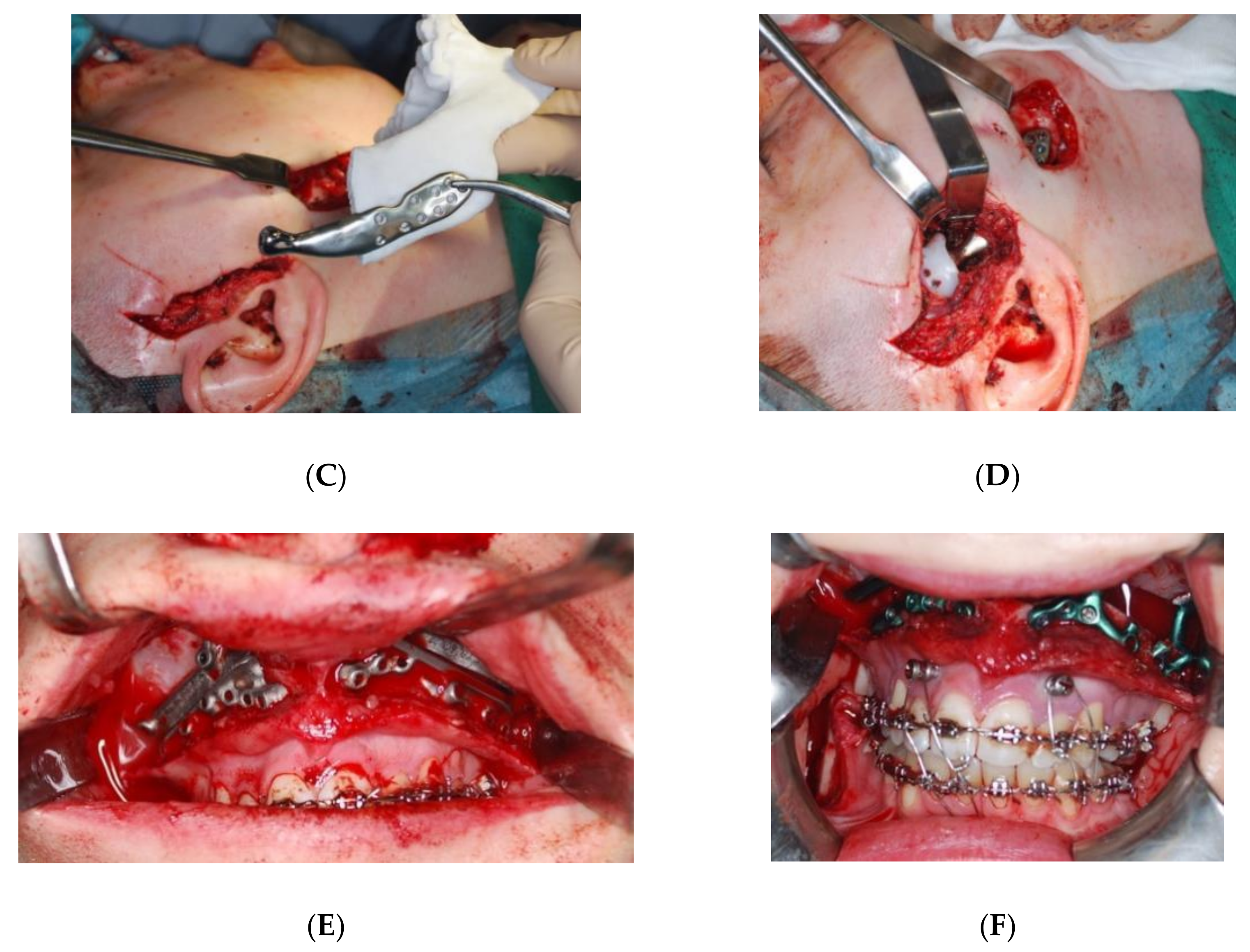
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kaban, L.B.; Bouchard, C.; Troulis, M.J. A Protocol for Management of Temporomandibular Joint Ankylosis in Children. J. Oral Maxillofac. Surg. 2009, 67, 1966–1978. [Google Scholar] [CrossRef]
- Kulesa-Mrowiecka, M.; Piech, J.; Dowgierd, K.; Myśliwiec, A. Physical therapy of temporomandibular disorder in a child with arthrogryposis multiplex congenita: A case report and literature review. CRANIO 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rikhotso, R.E.; Nkonyane, M.; Rikhotso, R.E.; Nkonyane, M. Zygomatico-Coronoid Ankylosis: A Case Report. Open J. Stomatol. 2017, 7, 475–480. [Google Scholar] [CrossRef] [Green Version]
- Dhupar, V.; Akkara, F.; Khandelwal, P.; Louis, A. Zygomatico-coronoid Ankylosis as Sequel of Inadequate Treatment. Ann. Maxillofac. Surg. 2018, 8, 158. [Google Scholar] [CrossRef] [PubMed]
- Dowgierd, K.; Lipowicz, A.; Kulesa-mrowiecka, M.; Linek, P.; Myśliwiec, A. Efficacy of immediate physiotherapy after surgical release of zygomatico-coronoid ankylosis in a young child : A case report. Physiother. Theory Pract. 2021, 00, 1–7. [Google Scholar] [CrossRef]
- Ohno, K.; Michi, K.; Ueno, T. Mandibular growth following ankylosis operation in childhood. Int. J. Oral Surg. 1981, 10 (Suppl. 1), 324–328. Available online: https://europepmc.org/article/med/6807903 (accessed on 22 November 2021).
- Cheong, R.C.T.; Kassam, K.; Eccles, S.; Hensher, R. Congenital Temporomandibular Joint Ankylosis: Case Report and Literature Review. Case Rep. Otolaryngol. 2016, 2016, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Clauser, L.C.; Consorti, G.; Elia, G.; Tieghi, R.; Galiè, M. Management of temporomandibular joint reankylosis in syndromic patients corrected with joint prostheses: Surgical and rehabilitation protocols. Craniomaxillofac. Trauma Reconstr. 2014, 7, 71–77. [Google Scholar] [CrossRef] [Green Version]
- Björk, A.; Skieller, V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur. J. Orthod. 1983, 5, 1–46. [Google Scholar] [CrossRef] [PubMed]
- Vibhute, P.J.; Bhola, N.; Borle, R.M. TMJ Ankylosis: Multidisciplinary Approach of Treatment for Dentofacial Enhancement-A Case Report. Case Rep. Dent. 2011, 2011, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.W.; Choi, J.Y.; Baek, S.H. Longitudinal management of recurrent temporomandibular joint ankylosis from infancy to adulthood in perspective of surgical and orthodontic treatment. Korean J. Orthod. 2019, 49, 413. [Google Scholar] [CrossRef]
- Dowgierd, K.; Pokrowiecki, R.; Borowiec, M.; Kozakiewicz, M.; Smyczek, D.; Krakowczyk, Ł. A Protocol for the Use of a Combined Microvascular Free Flap with Custom-Made 3D-Printed Total Temporomandibular Joint (TMJ) Prosthesis for Mandible Reconstruction in Children. Appl. Sci. 2021, 11, 2176. [Google Scholar] [CrossRef]
- Dowgierd, K.; Krakowczyk, Ł. The use of microsurgical reconstruction in treatment of craniofacial defects in paediatric patients. Int. J. Oral Maxillofac. Surg. 2019, 48, 136–137. [Google Scholar] [CrossRef]
- Bender, M.E.; Lipin, R.B.; Goudy, S.L. Development of the Pediatric Temporomandibular Joint. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 1–9. [Google Scholar] [CrossRef]
- Lipowicz, A.; Wolański, W.; Kawlewska, E.; Zwolska, P.; Kulesa-Mrowiecka, M.; Dowgierd, K.; Linek, P.; Myśliwiec, A. Evaluation of Mandibular Growth and Symmetry in Child with Congenital Zygomatic-Coronoid Ankylosis. Symmetry 2021, 13, 1634. [Google Scholar] [CrossRef]
- Resnick, C.M. Temporomandibular Joint Reconstruction in the Growing Child. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Felstead, A.M.; Revington, P.J. Surgical management of temporomandibular joint ankylosis in ankylosing spondylitis. Int. J. Rheumatol. 2011, 2011, 854167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arakeri, G.; Kusanale, A.; Zaki, G.A.; Brennan, P.A. Pathogenesis of post-traumatic ankylosis of the temporomandibular joint: A critical review. Br. J. Oral Maxillofac. Surg. 2012, 50, 8–12. [Google Scholar] [CrossRef]
- Mercuri, L.G.; Swift, J.Q. Considerations for the Use of Alloplastic Temporomandibular Joint Replacement in the Growing Patient. J. Oral Maxillofac. Surg. 2009, 67, 1979–1990. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III; Schneiderman, E.D.; Carlson, D.S. Growth of the mandible after replacement of the mandibular condyle: An experimental investigation in Macaca mulatta. J. Oral Maxillofac. Surg. 2002, 60, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Guyot, L.; Richard, O.; Layoun, W.; Cheynet, F.; Bellot-Samson, V.; Chossegros, C.; Blanc, J.L.; Gola, R. Long-term radiological findings following reconstruction of the condyle with fibular free flaps. J. Craniomaxillofac. Surg. 2004, 32, 98–102. [Google Scholar] [CrossRef]
- Sultana, J.; Haque Chowdhury, E.; Sultana Juyena, N.; Abul Bashar, M. Clinical evaluation of growth potentiality of autogenous costochondral graft in Temporomandibular joint on New Zealand white rabbit—An experimental study. J. Dent. Health Oral Disord. Ther. 2021, 12, 8–18. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; El-Sharkawy, T.M.; Mounair, R.M.; El-Ghareeb, T.I. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int. J. Oral Maxillofac. Surg. 2015, 44, 470–482. [Google Scholar] [CrossRef] [PubMed]
- Malis, D.D.; Xia, J.J.; Gateno, J.; Donovan, D.T.; Teichgraeber, J.F. New Protocol for 1-Stage Treatment of Temporomandibular Joint Ankylosis Using Surgical Navigation. J. Oral Maxillofac. Surg. 2007, 65, 1843–1848. [Google Scholar] [CrossRef] [PubMed]

| Patient | Age (Years) | Sex | Side | Aetiology | Age of Diagnosis (Years) |
|---|---|---|---|---|---|
| 1 | 2 | F | B | Congenital | 0 |
| 2 | 7 | F | R | Trauma | 4 |
| 3 | 9 | M | L | Trauma | 4 |
| 4 | 11 | F | B | Congenital | 0 |
| 5 | 11 | M | B | Congenital | 10 |
| 6 | 13 | M | L | Trauma | 10 |
| 7 | 13 | M | R | Trauma | 12 |
| 8 | 14 | M | R | Trauma | 7 |
| 9 | 14 | M | R | Trauma | 5 |
| 10 | 14 | M | R | Trauma | 7 |
| 11 | 14 | F | L | Trauma | 7 |
| 12 | 14 | F | L | Trauma | 7 |
| 13 | 15 | F | B | Infection | 12 |
| 14 | 15 | F | R | Infection | 6 |
| 15 | 15 | M | L | Infection | 5 |
| 16 | 15 | F | R | Congenital | 0 |
| 17 | 15 | M | B | Congenital | 0 |
| 18 | 15 | F | B | Trauma | 12 |
| 19 | 15 | F | L | Trauma | 6 |
| 20 | 15 | F | L | Trauma | 12 |
| 21 | 15 | M | L | Trauma | 13 |
| 22 | 16 | M | R | Infection | 12 |
| 23 | 16 | F | R | Infection | 5 |
| 24 | 16 | F | L | Infection | 9 |
| 25 | 16 | F | R | Trauma | 10 |
| 26 | 16 | F | R | Trauma | 9 |
| 27 | 16 | F | L | Trauma | 14 |
| 28 | 16 | M | B | Iatrogenic | 10 |
| 29 | 16 | M | L | Infection | 9 |
| 30 | 17 | F | L | Congenital | 0 |
| 31 | 18 | F | L | Infection | 4 |
| 32 | 18 | M | L | Infection | 10 |
| 33 | 18 | M | L | Infection | 13 |
| Patient | Tracheostomy | 1 Stage of the Treatment | 2 Stage of the Treatment | 3 Stage of the Treatment | 4 Stage of the Treatment | Orthodontic Treatment | Final Surgery | TMJP |
|---|---|---|---|---|---|---|---|---|
| 1 | RAS + silicone block placement | none | none | none | N/A | I Stage | N/A | |
| 2 | no | RAS + silicone block placement | Ramus TDO | none | none | After RAS | II Stage | N/A |
| 3 | no | RAS | Ramus TDO | none | none | N/A | II Stage | N/A |
| 4 | no | RAS | Ramus TDO | none | none | N/A | II Stage | N/A |
| 5 | no | RAS | Ramus TDO | none | none | After RAS | Orthognatic surgery | Custom |
| 6 | no | none | none | none | none | Before final surgery | Orthognatic surgery + RAS | stock |
| 7 | no | RAS | Ramus TDO | none | none | After RAS | Orthognatic surgery | |
| 8 | no | RAS + TMJP | none | none | none | N/A | I Stage | Custom |
| 9 | yes | Ramus and body BDO | RAS | Mandible body osseodistraction | osteotomia LF I | N/A | uwolnienie ankylozy | Custom |
| 10 | no | RAS | Ramus TDO | Bimaxillary transverse osseodistraction | none | After RAS | Orthognatic surgery | N/A |
| 11 | no | none | none | none | none | Before final surgery | Orthognatic surgery | Custom |
| 12 | no | RAS + silicone block placement | Ramus TDO | none | none | After RAS | II Stage | N/A |
| 13 | no | Ramus and body BDO | none | none | none | After RAS | Orthognatic surgery | Custom |
| 14 | no | Ramus and body BDO | none | none | none | N/A | Orthognatic surgery | Custom |
| 15 | no | RAS | RAS | none | none | N/A | Orthognatic surgery | Custom |
| 16 | yes | RAS | RAS | Ramus TDO | none | N/A | II Stage | N/A |
| 17 | no | Coronoidectiomy | none | none | none | N/A | I Stage | N/A |
| 18 | no | RAS | Ramus TDO | none | none | N/A | II Stage | N/A |
| 19 | no | RAS | none | none | none | After RAS | Orthognatic surgery | Custom |
| 20 | no | RAS | none | none | none | After RAS | Orthognatic surgery | |
| 21 | no | none | none | none | none | After RAS | Orthognatic surgery + RAS | Custom |
| 22 | no | RAS | Ramus TDO | none | none | N/A | II Stage | |
| 23 | yes | RAS | none | none | none | N/A | Mandible reconstruction with microvascular graft | Custom |
| 24 | no | none | none | none | none | N/A | Orthognatic surgery + RAS | Stock |
| 25 | yes | RAS + silicone block placement | none | none | none | Before final surgery | Orthognatic surgery | Custom |
| 26 | RAS + silicone block placement | none | none | none | Before final surgery | Orthognatic surgery | Custom | |
| 27 | no | RAS | Ramus and body BDO | none | none | After RAS | Orthognatic surgery | Custom |
| 28 | no | RAS | none | none | none | After RAS | Orthognatic surgery | Custom |
| 29 | no | Ramus and body BDO | RAS + TMJP | none | none | N/A | II Stage | N/A |
| 30 | no | RAS | Thrid molars removal | none | none | Before final surgery | Mandible osteotomy | Stock |
| 31 | no | none | none | none | none | N/A | Orthognatic surgery + RAS | Stock |
| 32 | no | none | none | none | none | Before final surgery | Orthognatic surgery + RAS | Custom |
| 33 | no | Ramus and body BDO | RAS | none | none | After RAS | Orthognatic surgery | Stock |
| Patient | MIO Pre-Op | MIO Post-Op |
|---|---|---|
| 1 | 0.5 | |
| 2 | 0.5 | 3.5 |
| 3 | 2 | 3.5 |
| 4 | 0 | 2 |
| 5 | 1 | 3.5 |
| 6 | 1.5 | 3.5 |
| 7 | 1 | 4.5 |
| 8 | 1 | 4 |
| 9 | 2 | 4 |
| 10 | 1 | 4 |
| 11 | 2 | 4 |
| 12 | 2 | 4 |
| 13 | 2 | 4 |
| 14 | 1.5 | 4 |
| 15 | 0.5 | 3.5 |
| 16 | 0.5 | 3.5 |
| 17 | 0 | 3 |
| 18 | 0 | 3.5 |
| 19 | 2 | 4.5 |
| 20 | 2 | 4 |
| 21 | 1 | 4 |
| 22 | 1 | 4 |
| 23 | 0.5 | 4 |
| 24 | 0.5 | 4 |
| 25 | 1.5 | 3.5 |
| 26 | 1 | 4 |
| 27 | 2 | 4 |
| 28 | 1 | 3.5 |
| 29 | 1.5 | 3.5 |
| 30 | 3 | 4 |
| 31 | 0.5 | 3.5 |
| 32 | 1 | 4 |
| 33 | 2 | 4 |
| Age | Gender | Side | Complication |
|---|---|---|---|
| 18 | M | L | Ectopic bone formation on the TMJP |
| 15 | F | B | Relapse |
| 15 | F | B | Relapse |
| 16 | F | L | Relapse |
| 18 | F | L | Infection |
| 11 | F | B | Infection |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dowgierd, K.; Pokrowiecki, R.; Kulesa Mrowiecka, M.; Dowgierd, M.; Woś, J.; Szymor, P.; Kozakiewicz, M.; Lipowicz, A.; Roman, M.; Myśliwiec, A. Protocol for Multi-Stage Treatment of Temporomandibular Joint Ankylosis in Children and Adolescents. J. Clin. Med. 2022, 11, 428. https://doi.org/10.3390/jcm11020428
Dowgierd K, Pokrowiecki R, Kulesa Mrowiecka M, Dowgierd M, Woś J, Szymor P, Kozakiewicz M, Lipowicz A, Roman M, Myśliwiec A. Protocol for Multi-Stage Treatment of Temporomandibular Joint Ankylosis in Children and Adolescents. Journal of Clinical Medicine. 2022; 11(2):428. https://doi.org/10.3390/jcm11020428
Chicago/Turabian StyleDowgierd, Krzysztof, Rafał Pokrowiecki, Małgorzata Kulesa Mrowiecka, Martyna Dowgierd, Jan Woś, Piotr Szymor, Marcin Kozakiewicz, Anna Lipowicz, Małgorzata Roman, and Andrzej Myśliwiec. 2022. "Protocol for Multi-Stage Treatment of Temporomandibular Joint Ankylosis in Children and Adolescents" Journal of Clinical Medicine 11, no. 2: 428. https://doi.org/10.3390/jcm11020428
APA StyleDowgierd, K., Pokrowiecki, R., Kulesa Mrowiecka, M., Dowgierd, M., Woś, J., Szymor, P., Kozakiewicz, M., Lipowicz, A., Roman, M., & Myśliwiec, A. (2022). Protocol for Multi-Stage Treatment of Temporomandibular Joint Ankylosis in Children and Adolescents. Journal of Clinical Medicine, 11(2), 428. https://doi.org/10.3390/jcm11020428









