Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Enrollment
2.2. Ethics
2.3. Study Design
2.4. Treatment
2.5. Protocol Phases and Parent Training Procedures
2.6. Training Experience
2.7. Outcome Measurements
2.7.1. Parenting Stress Index/Short Form (PSI-SF)
2.7.2. Home Situation Questionnaire (HSQ-ASD)
2.8. Statistical Analysis
3. Results
3.1. Fidelity
3.2. Inter-Rater Agreement
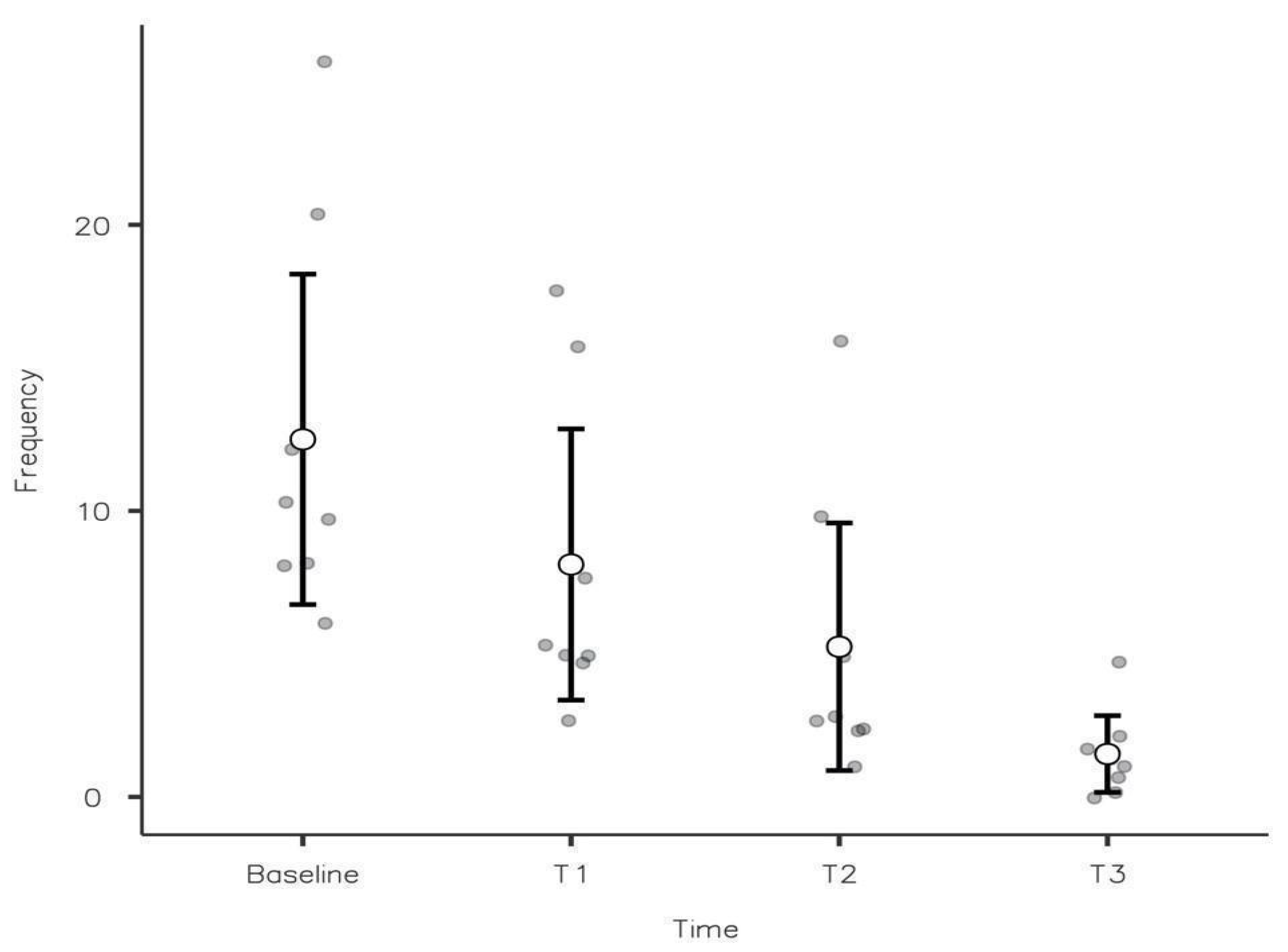
3.3. Behavioural Results
3.4. Parental Wellbeing
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eshraghi, A.A.; Li, C.; Alessandri, M.; Messinger, D.S.; Eshraghi, R.S.; Mittal, R.; Armstrong, F.D. COVID-19: Overcoming the challenges faced by individuals with autism and their families. Lancet Psychiatry 2020, 7, 481–483. [Google Scholar] [CrossRef]
- Kogan, M.D.; Strickland, B.B.; Blumberg, S.J.; Singh, G.K.; Perrin, J.M.; van Dyck, P.C. A National Profile of the Health Care Experiences and Family Impact of Autism Spectrum Disorder Among Children in the United States, 2005–2006. Pediatrics 2008, 122, e1149–e1158. [Google Scholar] [CrossRef] [PubMed]
- Colizzi, M.; Sironi, E.; Antonini, F.; Ciceri, M.L.; Bovo, C.; Zoccante, L. Psychosocial and Behavioral Impact of COVID-19 in Autism Spectrum Disorder: An Online Parent Survey. Brain Sci. 2020, 10, 341. [Google Scholar] [CrossRef] [PubMed]
- Narzisi, A. Handle the autism spectrum condition dur- ing coronavirus (COVID-19) stay at home period: Ten tips for helping parents and caregivers of young children. Brain Sci. 2020, 10, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amaral, D.G.; de Vries, P.J. COVID-19 and autism research: Perspectives from around the globe. Autism Res. 2020, 13, 844–869. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Rosen, R.; Shaw, S.E.; Byng, R.; Faulkner, S.; Finlay, T.; Grundy, E.; Husain, L.; Hughes, G.; Leone, C.; et al. Planning and Evaluating Remote Consultation Services: A New Conceptual Framework Incorporating Complexity and Practical Ethics. Front. Digit. Health 2021, 3, 726095. [Google Scholar] [CrossRef]
- Jordan, C.; Leslie, K.; Roder-DeWan, H.H.; Adeyi, O.S.; Barker, P.; Daelmans, B.; Doubova, S.V.; English, M.; Elorrio, E.G.; Guanais, F.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar]
- Hyman, S.L.; Levy, S.E.; Myers, S.M. Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, Evaluation, and Management of Children with Autism Spectrum Disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef] [Green Version]
- Pakyurek, M.; Yellowlees, P.; Hilty, D. The child and adolescent telepsychiatry consultation: Can it be a more effective clinical process for certain patients than conventional practice? Telemed J. E Health 2010, 16, 289–292. [Google Scholar] [CrossRef]
- Boisvert, M.; Lang, R.; Andrianopoulos, M.; Boscardin, M.L. Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Dev. Neurorehabilit. 2010, 13, 423–432. [Google Scholar] [CrossRef]
- Lindgren, S.; Wacker, D.P.; Suess, A.; Schieltz, K.; Pelzel, K.; Kopelman, T.; Lee, J.; Romani, P.; Waldron, D. Telehealth and Autism: Treating Challenging Behavior at Lower Cost. Pediatrics 2015, 137, 167–175. [Google Scholar] [CrossRef] [Green Version]
- Ingersoll, B.; Gergans, S. The effect of a parent-implemented imitation intervention on spontaneous imitation skills in young children with autism. Res. Dev. Disabil. 2007, 28, 163–175. [Google Scholar] [CrossRef]
- Vismara, L.A.; McCormick, C.; Young, G.S.; Nadhan, A.; Monlux, K. Preliminary findings of a telehealth approach to parent training in autism. J. Autism Dev. Disord. 2013, 43, 2953–2969. [Google Scholar] [CrossRef]
- Dittman, C.K.; Farruggia, S.P.; Palmer, M.L.; Sanders, M.R.; Keown, L.J. Predicting success in an online parenting intervention: The role of child, parent, and family factors. J. Fam. Psychol. 2014, 28, 236–243. [Google Scholar] [CrossRef]
- Miltenberger, R.G. Behavior skills training procedures. In Behavior Modification Principles and Procedures; Miltenberger, R.G., Ed.; Thompson Wadsworth: Belmont, CA, USA, 2004; pp. 237–249. [Google Scholar]
- Koegel, R.L.; Glahn, T.J.; Nieminen, G.S. Generalization of parent-training results1. J. Appl. Behav. Anal. 1978, 11, 95–109. [Google Scholar] [CrossRef] [Green Version]
- Robertson, R.E.; Wehby, J.H.; King, S.M. Increased parent reinforcement of spontaneous requests in children with autism spectrum disorder: Effects on problem behavior. Res. Dev. Disabil. 2013, 34, 1069–1082. [Google Scholar] [CrossRef]
- Stokes, J.V.; Luiselli, J.K. In-home parent training of functional analysis skills. Int. J. Behav. Consult. Ther. 2008, 4, 259–263. [Google Scholar] [CrossRef] [Green Version]
- Haskett, M.E.; Ahern, L.S.; Ward, C.S.; Allaire, J.C. Factor Structure and Validity of the Parenting Stress Index-Short Form. J. Clin. Child Adolesc. Psychol. 2006, 35, 302–312. [Google Scholar] [CrossRef]
- Chowdhury, M.; Aman, M.G.; Lecavalier, L.; Smith, T.; Johnson, C.; Swiezy, N.; McCracken, J.T.; King, B.; McDougle, C.J.; Bearss, K.; et al. Factor structure and psychometric properties of the revised Home Situations Questionnaire for autism spectrum disorder: The Home Situations Questionnaire-Autism Spectrum Disorder. Autism 2015, 20, 528–537. [Google Scholar] [CrossRef] [Green Version]
- Cooper, J.O.; Heron, T.E.; Heward, W.L. Applied Behavior Analysis; Merrill: New York, NY, USA, 2007. [Google Scholar]
- Schieltz, K.M.; Wacker, D.P. Functional assessment and function-based treatment delivered via telehealth: A brief summary. J. Appl. Behav. Anal. 2020, 53, 1242–1258. [Google Scholar] [CrossRef]
- McStay, R.L.; Trembath, D.; Dissanayake, C. Stress and Family Quality of Life in Parents of Children with Autism Spectrum Disorder: Parent Gender and the Double ABCX Model. J. Autism Dev. Disord. 2014, 44, 3101–3118. [Google Scholar] [CrossRef]
- Heitzman-Powell, L.S.; Buzhardt, J.; Rusinko, L.C.; Miller, T.M. Formative Evaluation of an ABA Outreach Training Program for Parents of Children with Autism in Remote Areas. Focus Autism Other Dev. Disabil. 2014, 29, 23–38. [Google Scholar] [CrossRef]
- Friesen, K.A.; Weiss, J.A.; Howe, S.J.; Kerns, C.M.; McMorris, C.A. Mental Health and Resilient Coping in Caregivers of Autistic Individuals during the COVID-19 Pandemic: Findings from the Families Facing COVID Study. J. Autism Dev. Disord. 2021, 1–11. [Google Scholar] [CrossRef]
- Powell, D.; Dunlap, G.; Fox, L. Prevention and Intervention for the Challenging Behaviors of Toddlers and Preschoolers. Infants Young-Child. 2006, 19, 25–35. [Google Scholar] [CrossRef] [Green Version]
- Brookman-Frazee, L.; Stahmer, A.; Baker-Ericzén, M.J.; Tsai, K. Parenting Interventions for Children with Autism Spectrum and Disruptive Behavior Disorders: Opportunities for Cross-Fertilization. Clin. Child Fam. Psychol. Rev. 2006, 9, 181–200. [Google Scholar] [CrossRef] [Green Version]
- Patterson, S.Y.; Smith, V.; Mirenda, P. A systematic review of training programs for parents of children with autism spectrum disorders: Single subject contributions. Autism 2012, 16, 498–522. [Google Scholar] [CrossRef]
- Tonge, B.; Brereton, A.; Kiomall, M.; Mackinnon, A.; King, N.; Rinehart, N. Effects on Parental Mental Health of an Education and Skills Training Program for Parents of Young Children With Autism: A Randomized Controlled Trial. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 561–569. [Google Scholar] [CrossRef]
- Hassan, M.; Simpson, A.; Danaher, K.; Haesen, J.; Makela, T.; Thomson, K. An Evaluation of Behavioral Skills Training for Teaching Caregivers How to Support Social Skill Development in Their Child with Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 1957–1970. [Google Scholar] [CrossRef]
- Unholz-Bowden, E.; McComas, J.J.; McMaster, K.L.; Girtler, S.; Kolb, R.L.; Shipchandler, A. Caregiver Training Via Telehealth on Behavioral Procedures: A Systematic Review. J. Behav. Educ. 2020, 29, 246–281. [Google Scholar] [CrossRef]
- Boutain, A.R.; Sheldon, J.B.; Sherman, J.A. Evaluation of a telehealth parent training program in teaching self-care skills to children with autism. J. Appl. Behav. Anal. 2020, 53, 1259–1275. [Google Scholar] [CrossRef]
- Gerow, S.; Radhakrishnan, S.; Akers, J.S.; McGinnis, K.; Swensson, R. Telehealth parent coaching to improve daily living skills for children with ASD. J. Appl. Behav. Anal. 2021, 54, 566–581. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.; Craig, E.A.; Dounavi, K. Telehealth as a Model for Providing Behaviour Analytic Interventions to Individuals with Autism Spectrum Disorder: A Systematic Review. J. Autism Dev. Disord. 2019, 49, 582–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Phases | Therapist’s Tasks | Parent’s Tasks |
|---|---|---|
| Phase 1 | Protocol explanation, Data collection | Behaviours frequency checklist |
| Phase 2 | First baseline, selection of target behaviour, instruction for video recording | Selection of target behaviour, starts video recording |
| Phase 3 | Insert examples in the ABC worksheet from gathered observations. Gives Instruction on ABC worksheet and functional analysis | ABC worksheet recording |
| Phase 4 | Analysis of the type of problem behavior, instruction on functional analysis trough ABC worksheet and videos | Receives instruction, starts the protocol and gather the objective baseline (T0) |
| Phase 5 | Gather T0. Start BST parent training program, teaches procedures for behavioural change | Receive BST |
| Phase 6 | Debrief and fidelity | Receive feedback |
| Phase 7 | Data analysis; external review of fidelity | - |
| Phase 8 | Debrief | Gives feedback |
| Protocol (days) | Treatment (days) | Week | Phase | Meetings | Data Gathering |
|---|---|---|---|---|---|
| - | - | - | 0 | 0 | Psychological Assessment T0 |
| 0 | - | 1 | 1 | 1 | |
| 7 | - | 2 | 2 | 2 | |
| 14 | - | 3 | 3 | 3 | |
| 21 | - | 4 | 4 | 4 | |
| 22 | 0 | - | - | - | Behavioral T0 |
| 28 | 6 | 5 | 5 | 5 | |
| 35 | 13 | 6 | 5–6 | 6 | |
| 42 | 20 | 7 | 5–6 | 7 | Behavioral T1 |
| 49 | 27 | 8 | 5–6 | 8 | |
| 56 | 34 | 9 | 5–6 | 9 | |
| 62 | 40 | - | - | - | Behavioral T2 |
| 63 | 41 | 10 | 5–6 | 10 | |
| 70 | 48 | 11 | 5–6 | 11 | |
| 77 | 55 | 12 | 5–6 | 12 | |
| 82 | 60 | - | - | - | Behavioral T3 |
| 83–90 | - | 13 | 7 | - | |
| 91 | - | 13 | 8 | 13 | Psychological Assessment T1 |
| Measure | Completed | Dropped |
|---|---|---|
| Number of children/parents | 8/16 | 6/12 |
| Gender (M/F) | 6/2 | 6/0 |
| Age (months) | 72.0 ± 30.4 68 (40–138) | 57 ± 14.1 51 (48–84) |
| Total DQ Griffiths | 67.0 ± 19.3 67.5 (45.5–95.5) | 63.9 ± 14.2 69.4 (39.0–75.0) |
| Age of Mother (years) | 41.0 ± 5.8 39 (33–52) | 37.7 ± 2.3 38 (35–40) |
| Age of Father (years) | 48.4 ± 5.0 49 (41–57) | 43.0 ± 4.8 49 (41–57) |
| Education of Mother (years) | 16.1 ± 2.6 18 (13–18) | 13.8 ± 2.0 13 (13–18) |
| Education of Father (years) | 16.8 ± 2.3 18 (8–21) | 14.7 ± 2.6 18 (8–21) |
| Working Mother/Father (ratio) | 0.50/1.00 | 0.83/1.00 |
| Number of siblings | 0.25 ± 0.46 0 (0–1) | 1.33 ± 1.37 1 (0–3) |
| Problem Behavior | Behavioral Function | Context | |
|---|---|---|---|
| ASD S1 | Difficulties in accepting Stop Signal (“no”) | Access to the tangible | At home when routine activities in the presence of both parents are changed or interrupted |
| ASD S2 | Repetitive requests | Access to the tangible | At home during routine activities in the presence of both parents |
| ASD S3 | Unshared laughter | Seeking attention | At home when the child carries out independent activities requested by the parents |
| ASD S4 | Shouting when faced with a task proposed by the mother | Task avoidance/escape | At home when following the mother’s request to perform tasks |
| ASD S5 | Climbing on furniture, shouting, taking dangerous objects | Attention-seeking | At home in the presence of both parents engaged in other activities |
| ASD S6 | Echolalia | Automatic reinforcement | At home when engaged in independent play activities |
| ASD S7 | Throwing objects | Automatic reinforcement | At home while carrying out independent activities, with the mother engaged in other activities |
| ASD S8 | Expressing denial and rejection as a for of idiosyncratic behavior | Task avoidance | At home when following requests by both parents |
| Behavioral Procedure | Explanation | |
|---|---|---|
| ASD S1 | Extinction | Parents physically remove themselves from the child when the target behaviour occurs (consequence intervention). |
| ASD S2 | Desensitization | Gradual reduction of the number of requests the child can make and to which the parents can respond (antecedent intervention) according to the established criterion. |
| ASD S3 | Differential reinforcement/Extinction | Extinction: Parents ignore the child when he/she emits the target behavior (consequence intervention) DRO (Differential Reinforcement of Other Behavior): parents were instructed to provide a reinforcement, agreed during the session, whenever the child did not exhibit the problem behavior in a given period of time. |
| ASD S4 | High-p/fading of the prompt | Rapid presentation of a high-probability prompt followed by a low-probability prompt (antecedent intervention). Fading of the prompt: gradual reduction of the help provided by the parents on the task with low probability of the issue (intervention on the antecedent) |
| ASD S5 | Differential reinforcement/Extinction | Extinction: Parents ignore the child when they display the target behavior (consequence intervention) DRO: parents were instructed to provide reinforcement, agreed during the session, whenever the child did not exhibit the problem behavior in a given period of time. |
| ASD S6 | Expanding interests/Direction of Attention | Associating disliked objects/activities with liked, albeit restricted, objects/activities (antecedent intervention) |
| ASD S7 | Expanding interests | Presenting functional auditory stimuli through songs or videos |
| ASD S8 | Token economy | Child had the opportunity to earn tokens during the day (tangible tokens). After reaching an agreed number of tokens, they had the opportunity to exchange them for a reward they liked. The token economy was built on a billboard on which the child could attach points, thus favoring the visual channel for collecting points, and did not use a response cost. |
| Main Behavioral Symptoms | Frequency * T0 | Frequency T1 (20 days) | Frequency T2 (40 days) | Frequency T3 (60 days) | |
|---|---|---|---|---|---|
| ASD S1 | Difficulties in accepting Stop Signal (“no”) | 6 | 5 | 2 | 0 |
| ASD S2 | Repetitive requests | 20 | 16 | 10 | 5 |
| ASD S3 | unshared’ laughter | 10 | 5 | 5 | 1 |
| ASD S4 | Shouting when faced with a task proposed by the mother | 10 | 5 | 2 | 1 |
| ASD S5 | Climbing on furniture, shouting, and taking dangerous objects | 12 | 8 | 3 | 2 |
| ASD S6 | Echolalia | 26 | 18 | 16 | 2 |
| ASD S7 | Throwing objects | 8 | 3 | 1 | 1 |
| ASD S8 | Expressing denial and rejection as a for of idiosyncratic behavior | 8 | 5 | 3 | 0 |
| Before Treatment | After Treatment | W/p-Level | Paired t-Test/p-Level | |
|---|---|---|---|---|
| PSI-SF Scale | ||||
| Total Value | 105.7 ± 7.3 105 (90–114) | 95.4 ± 8.1 98 (84–107) | 105/0.001 | 6.2/<0.001 |
| PD | 35.6 ± 7.9 36 (21–47) | 29.3 ± 8.1 30 (16–43) | 67/0.03 | 2.7/0.02 |
| P-CDI | 36.2 ± 8.7 33 (26–52) | 29 ± 5.4 29.5 (19–38) | 73.5/0.008 | 3.6/0.003 |
| DC | 32.9 ± 12.4 30 (19–53) | 36.9 ± 7.1 37 (21–50) | n.s | n.s |
| HSQ-ASD Scale | ||||
| Total Value | 4.8 ± 1.8 4.6 (1.9–7.4) | 3.5 ± 1.6 3 (1–7) | 66/0.003 | 6.3/<0.001 |
| Inflexibility | 5.3 ± 1.6 5.4 (2–8.2) | 3.4 ± 1.2 3.3 (2–5) | 78/0.002 | 4.3/0.001 |
| Avoidance | 4.8 ± 2.1 4.4 (1.8–7.8) | 3.2 ± 2 2.8 (1–6) | 91/0.001 | 7.9/<0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marino, F.; Chilà, P.; Failla, C.; Minutoli, R.; Vetrano, N.; Luraschi, C.; Carrozza, C.; Leonardi, E.; Busà, M.; Genovese, S.; et al. Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program. J. Clin. Med. 2022, 11, 1194. https://doi.org/10.3390/jcm11051194
Marino F, Chilà P, Failla C, Minutoli R, Vetrano N, Luraschi C, Carrozza C, Leonardi E, Busà M, Genovese S, et al. Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program. Journal of Clinical Medicine. 2022; 11(5):1194. https://doi.org/10.3390/jcm11051194
Chicago/Turabian StyleMarino, Flavia, Paola Chilà, Chiara Failla, Roberta Minutoli, Noemi Vetrano, Claudia Luraschi, Cristina Carrozza, Elisa Leonardi, Mario Busà, Sara Genovese, and et al. 2022. "Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program" Journal of Clinical Medicine 11, no. 5: 1194. https://doi.org/10.3390/jcm11051194
APA StyleMarino, F., Chilà, P., Failla, C., Minutoli, R., Vetrano, N., Luraschi, C., Carrozza, C., Leonardi, E., Busà, M., Genovese, S., Musotto, R., Puglisi, A., Arnao, A. A., Cardella, G., Famà, F. I., Cusimano, G., Vagni, D., Martines, P., Mendolia, G., ... Pioggia, G. (2022). Psychological Interventions for Children with Autism during the COVID-19 Pandemic through a Remote Behavioral Skills Training Program. Journal of Clinical Medicine, 11(5), 1194. https://doi.org/10.3390/jcm11051194









