Characteristics of the Maxillofacial Morphology in Patients with Idiopathic Mandibular Condylar Resorption
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Cephalometric Analysis
2.3. Statistical Analysis
3. Results
3.1. Clinical Findings on Malocclusion
3.2. TMJ Findings
3.3. Evaluation of Skeletal Pattern
3.4. Evaluation of Denture Pattern
3.5. Evaluation of Soft Tissue
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnett, G.W.; Milam, S.B.; Gottesman, L. Progressive mandibular retrusion—idiopathic condylar resorption. Part I. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 8–15. [Google Scholar] [CrossRef]
- Arnett, G.W.; Milam, S.B.; Gottesman, L. Progressive mandibular retrusion—idiopathic condylar resorption. Part II. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 117–127. [Google Scholar] [CrossRef]
- Rabey, G.P. Bilateral mandibular condylysis—A morphanalytic diagnosis. Br. J. Oral Surg. 1977, 15, 121–134. [Google Scholar] [CrossRef]
- Brennan, M.T.; Patronas, N.J.; Brahim, J.S. Bilateral condylar resorption in dermatomyositis: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1999, 87, 446–451. [Google Scholar] [CrossRef]
- Osial, T.A.; Avakian, A.; Sassouni, V.; Agarwal, A.; Medsger, T.A., Jr.; Rodnan, G.P. Resorption of the mandibular condyles and coronoid processes in progressive systemic sclerosis (scleroderma). Arthritis Rheum. 1981, 24, 729–733. [Google Scholar] [CrossRef]
- Iizuka, T.; Lindqvist, C.; Hallikainen, D.; Mikkonen, P.; Paukku, P. Severe bone resorption and osteoarthrosis after miniplate fixation of high condylar fractures: A clinical and radiologic study of thirteen patients. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 400–407. [Google Scholar] [CrossRef]
- Burke, P.H. A Case of Acquired Unilateral Mandibular Condylar Hypoplasia. Proc. R. Soc. Med. 1961, 54, 507–510. [Google Scholar] [CrossRef] [Green Version]
- Abramowicz, S.; Kim, S.; Prahalad, S.; Chouinard, A.-F.; Kaban, L. Juvenile arthritis: Current concepts in terminology, etiopathogenesis, diagnosis, and management. Int. J. Oral Maxillofac. Surg. 2016, 45, 801–812. [Google Scholar] [CrossRef]
- Wolford, L.M. Idiopathic Condylar Resorption of the Temporomandibular Joint in Teenage Girls (Cheerleaders Syndrome). Bayl. Univ. Med. Cent. Proc. 2001, 14, 246–252. [Google Scholar] [CrossRef]
- Alsabban, L.; Amarista, F.J.; Mercuri, L.G.; Perez, D. Idiopathic Condylar Resorption: A Survey and Review of the Literature. J. Oral Maxillofac. Surg. 2018, 76, 2316.e1. [Google Scholar] [CrossRef] [PubMed]
- Posnick, J.C.; Fantuzzo, J.J. Idiopathic Condylar Resorption: Current Clinical Perspectives. J. Oral Maxillofac. Surg. 2007, 65, 1617–1623. [Google Scholar] [CrossRef] [PubMed]
- Wolford, L.M.; Cardenas, L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 667–677. [Google Scholar] [CrossRef]
- Papadaki, M.E.; Tayebaty, F.; Kaban, L.B.; Troulis, M.J. Condylar resorption. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Schendel, S.A.; Tulasne, J.-F.; Linck, D.W. Idiopathic condylar resorption and micrognathia: The case for distraction osteogenesis. J. Oral Maxillofac. Surg. 2007, 65, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Troulis, M.J.; Tayebaty, F.T.; Papadaki, M.; Williams, W.B.; Leonard, B.; Kaban, L.B. Condylectomy and Costochondral Graft Reconstruction for Treatment of Active Idiopathic Condylar Resorption. J. Oral Maxillofac. Surg. 2008, 66, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Mehra, P.; Nadershah, M.; Chigurupati, R. Is alloplastic temporomandibular joint reconstruction a viable option in the surgical management of adult patients with idiopathic condylar resorption? J. Oral Maxillofac. Surg. 2016, 74, 2044–2054. [Google Scholar] [CrossRef]
- Chung, C.J.; Choi, Y.-J.; Kim, I.-S.; Huh, J.-K.; Kim, H.-G.; Kim, K.-H. Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 404–417. [Google Scholar] [CrossRef]
- Coleta, K.E.; Wolford, L.M.; Gonçalves, J.R.; Pinto, A.D.S.; Pinto, L.P.; Cassano, D.S. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts® total joint prostheses: Part I—Skeletal and dental stability. Int. J. Oral Maxillofac. Surg. 2009, 38, 126–138. [Google Scholar] [CrossRef]
- Gunson, M.J.; Arnett, G.W.; Formby, B.; Falzone, C.; Mathur, R.; Alexander, C. Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: A case for low serum 17beta-estradiol as a major factor in progressive condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 772–779. [Google Scholar] [CrossRef]
- Catherine, Z.; Breton, P.; Bouletreau, P. Condylar resorption after orthognathic surgery: A systematic review. Rev. Stomatol. Chir. Maxillo-Faciale Chir. Orale 2016, 117, 3–10. [Google Scholar] [CrossRef]
- Phillips, R.M.; Bell, W.H. Atrophy of mandibular condyles after sagittal ramus split osteotomy: Report of case. J. Oral Surg. (Am. Dent. Assoc. 1965) 1978, 36, 45–49. [Google Scholar]
- Tanimoto, K.; Awada, T.; Onishi, A.; Hirose, N. A survey of idiopathic mandibular condylar resorption in the department of Orthodontics Hiroshima University Hospital. J. CHU-SHI. Orthod. Soc. 2021, 33, 5–9. [Google Scholar]
- Sassouni, V.; Sotereanos, G.C. Diagnosis and Treatment of Dent-Facial Abnormalities; Charles C Thomas Publisher: Springfield, MO, USA, 1974; pp. 57–83. [Google Scholar]
- Akl, H.E.; Abouelezz, A.M.; El Sharaby, F.A.; El-Beialy, A.R.; El-Ghafour, M.A. Force magnitude as a variable in maxillary buccal segment intrusion in adult patients with skeletal open bite. Angle Orthod. 2020, 90, 507–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sansare, K.; Raghav, M.; Mallya, S.M.; Karjodkar, F. Management-related outcomes and radiographic findings of idiopathic condylar resorption: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 209–216. [Google Scholar] [CrossRef]
- Solow, B. The dentoalveolar compensatory mechanism: Background and clinical implications. Br. J. Orthod. 1980, 7, 145–161. [Google Scholar] [CrossRef]
- Kucera, J.; Marek, I.; Tycova, H.; Baccetti, T. Molar height and dentoalveolar compensation in adult subjects with skeletal open bite. Angle Orthod. 2011, 81, 564–569. [Google Scholar] [CrossRef]
- Kuitert, R.; Beckmann, S.; van Loenen, M.; Tuinzing, B.; Zentner, A. Dentoalveolar compensation in subjects with vertical skeletal dysplasia. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 649–657. [Google Scholar] [CrossRef]
- Abubaker, A.O.; Raslan, W.F.; Sotereanos, G.C. Estrogen and progesterone receptors in temporomandibular joint discs of symptomatic and asymptomatic persons: A preliminary study. J. Oral Maxillofac. Surg. 1993, 51, 1096–1100. [Google Scholar] [CrossRef]

| Measurement | Definition |
|---|---|
| Skeletal pattern: linear | |
| S-N | Distance between S and N |
| N-A | Distance between N and A |
| A-B | Distance between A and B |
| Go-Me | Distance between Go and Me |
| Ar-Lr | Distance between Ar and Lr |
| Skeletal pattern: angular | |
| Facial angle | Angle between FH plane and N-Pog line |
| Angel of convexity | Angle between NA line and A-Pog line |
| SN to MP | Angle between SN plane and MP |
| FMA | Angle between FH plane and MP |
| Gonial angle | Angle between Ramus plane and MP |
| SNP | Angle between SN plane and N-Pog |
| SNA | Angle between SN plane and NA line |
| SNB | Angle between SN plane and NB line |
| ANB | Difference between SNA and SNB |
| Denture pattern: linear | |
| Overjet | Distance between the incisal edges of the upper and lower central incisors measured at the level of OP |
| Overbite | Distance between the incisal edges of the upper and lower central incisors, measured perpendicular to OP |
| U1 to Ar-A | Ar-A line to U1 |
| L1 to Lr-B | Lr-B line to L1 |
| U6 to Ar-A | Ar-A line to U6 |
| L6 to Lr-B | Lr-B line to L6 |
| Denture pattern: angular | |
| SN to OP | Angle between SN plane and OP |
| PP to OP | Angle between PP and OP |
| U1 to SN | Angle between long axis of U1 and SN plane |
| U1 to FH | Angle between long axis of U1 and FH plane |
| U1 to PP | Angle between long axis of U1 and PP |
| U1 to OP | Angle between long axis of U1 and OP |
| L1 to FH (FMIA) | Angle between long axis of L1 and FH plane |
| L1 to OP | Angle between long axis of L1 and OP |
| L1 to MP (IMPA) | Angle between long axis of L1 and MP |
| Interincisal angle | Angle between long axis of U1 and L1 |
| Soft tissue: linear | |
| E-line to ULP | Retruded or protruded upper lip relative to E-line |
| E-line to LLP | Retruded or protruded lower lip relative to E-line |
| Soft tissue: angular | |
| Z-angle | Angle formed by the intersection of FH plane and a line connecting soft tissue pogonion and the most protrusive lip point |
| Landmark | Abbreviation | Definition |
|---|---|---|
| Lateral cephalometric analysis | ||
| Sella | S | Mid-point of sella turcica |
| Nasion | N | Most anterior point of frontonasal suture |
| Porion | Po | Most superior point of the external auditory meatus |
| Orbitale | Or | Most inferior point on the lower border of the bony orbit |
| Ariculare | Ar | Intersecting point of the inferior cranial base with mandibular posterior border |
| Posterior nasal spine | PNS | Most posterior point of hard palate |
| Anterior nasal spine | ANS | Anterior point of maxilla |
| A-point | A | Deepest anterior point on maxilla anterior concavity |
| B-point | B | Deepest anterior point on mandibular symphysis |
| Pogonion | Most anterior point on mandibular symphysis | |
| Lr | Lr | A contact point of ramus plane to mandibular ramus |
| Gonion | Go | Intersection of the lines tangent to the posterior margin of the ascending ramus and the MP |
| Menton | Me | Most inferior point on mandibular symphysis |
| Upper incisor | U1 | Edge of the upper central incisor |
| Lower incisor | L1 | Edge of the lower central incisor |
| Upper first molar | U6 | Mesio-distal mid-point of the upper first molar outline |
| Lower first molar | L6 | Mesio-distal mid-point of the lower first molar outline |
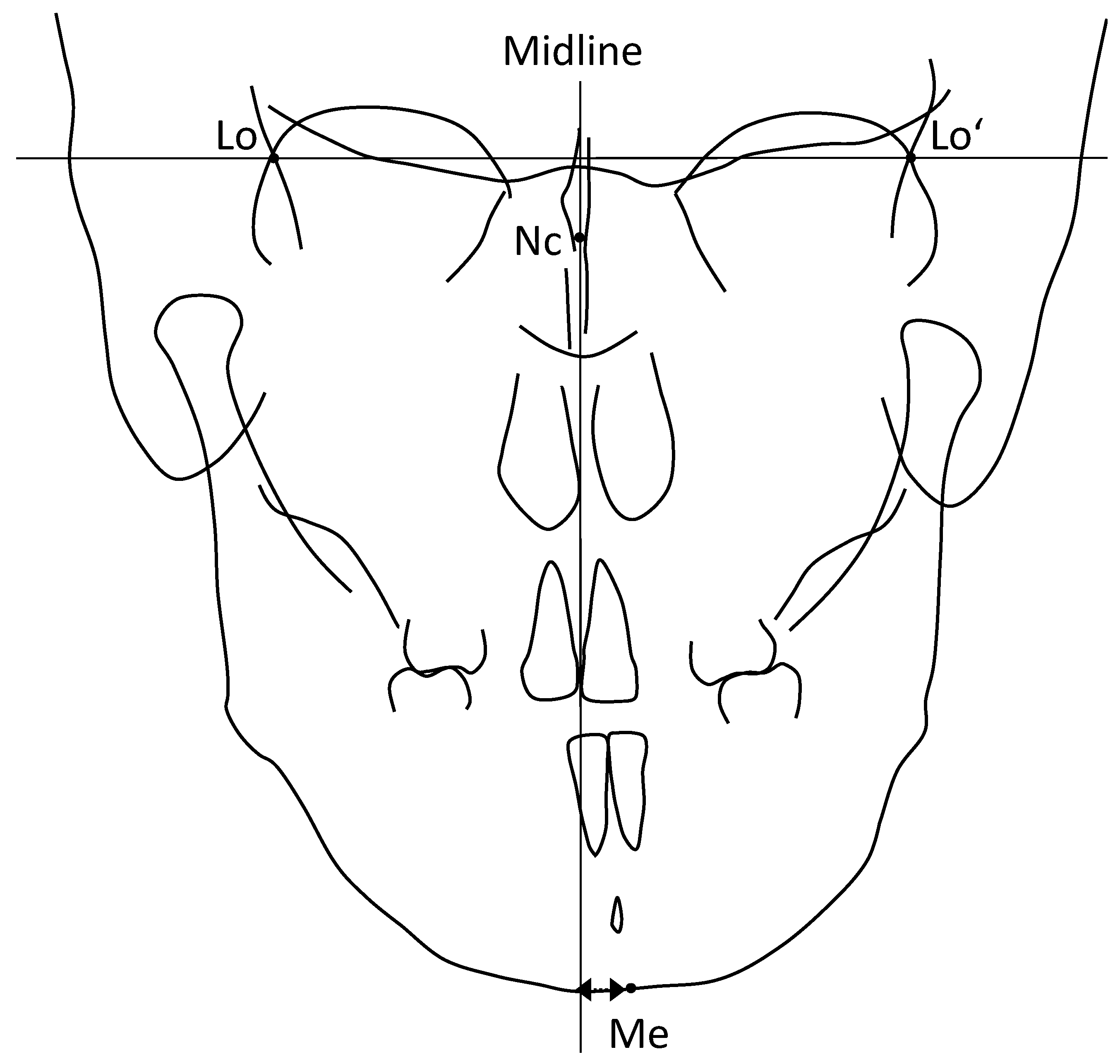
| Frontal cephalometric analysis | ||
| Latero-orbitale | Lo | Intersecting point between the external orbital contour laterally and the oblique line |
| Crista galli | Nc | The most narrowed part of the neck of crista galli |
| Menton | Me | The point on the inferior border of bony chin right below the genial tubercle |
| Subject | Age | Sex | Overjet (mm) | Overbite (mm) | Molar Relationship | TMJ Symptoms | Disk Displacement | Condylar Deformity | Mandibular Deviation | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R | L | R | L | R | L | R | L | ||||||
| 1 | 23Y6M | F | 5.4 | −1.2 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 2 | 31Y5M | F | 8.9 | −4.4 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 3 | 23Y3M | F | 11.7 | −5.2 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | L |
| 4 | 26Y7M | F | 16.5 | 0.6 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 5 | 29Y8M | F | 6.1 | −6.6 | II | II | N | N | ADDWOR | ADDWR | Y | Y | N |
| 6 | 20Y3M | F | 4.1 | 1.7 | II | II | N | N | ADDWOR | ADDWR | Y | Y | R |
| 7 | 34Y2M | F | 3.3 | 1.3 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | R |
| 8 | 21Y8M | F | 7.2 | 0.8 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 9 | 28Y6M | F | 6.6 | −1.6 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | L |
| 10 | 26Y6M | F | 5.2 | −2.5 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 11 | 27Y9M | F | 3.8 | 2.2 | II | II | N | Creptus | N | ADDWOR | N | Y | L |
| 12 | 16Y6M | F | 9 | 4.8 | II | II | Click, pain | Click, pain | ADDWOR | ADDWOR | Y | Y | L |
| 13 | 28Y2M | F | 4.5 | 0.4 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 14 | 20Y6M | F | 10.8 | 0.8 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | R |
| 15 | 33Y11M | F | 9.9 | −2.1 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | R |
| 16 | 17Y11M | F | 12.5 | 3.8 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| 17 | 20Y5M | F | 6.5 | −1.2 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | R |
| 18 | 29Y0M | F | 8.5 | −0.5 | II | II | N | N | ADDWOR | ADDWOR | Y | Y | N |
| Measurement | Control | ICR | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Linear | ||||
| S-N | 67.9 | 2.6 | 69.9 | 2.8 |
| N-A | 62.6 | 3.6 | 62.8 | 3.0 |
| A-B | 42.2 | 3.7 | 46.0 * | 4.9 |
| Go-Me | 74.6 | 3.8 | 69.5 * | 4.8 |
| Ar-Lr | 41.1 | 4.8 | 30.7 * | 4.8 |
| Angular | ||||
| Facial angle (FH to N-Pog) | 85.0 | 4.1 | 80.1 * | 5.3 |
| Angel of convexity (N-A-Pog) | 5.3 | 5.3 | 19.6 * | 8.5 |
| SN to MP | 33.2 | 4.5 | 51.5 * | 7.1 |
| FMA (MP to FH) | 28.8 | 6.0 | 41.6 * | 6.8 |
| Gonial angle | 119.3 | 5.8 | 127.7 * | 7.4 |
| SN to Ramus plane | 93.9 | 4.3 | 103.8 * | 9.6 |
| SNP | 80.6 | 2.9 | 70.2 * | 4.7 |
| SNA | 83.1 | 2.5 | 80.1 * | 3.8 |
| SNB | 80.2 | 2.6 | 71.3 * | 4.2 |
| ANB | 2.9 | 2.2 | 8.9 * | 3.2 |
| Measurement | Control | ICR | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Linear | ||||
| Overjet | 3.5 | 0.8 | 7.8 * | 3.5 |
| Overbite | 2.0 | 1.1 | −0.5 * | 3 |
| U1 to Ar-A | 23.0 | 2.1 | 23.7 | 3.7 |
| L1 to Lr-B | 20.5 | 2.6 | 22.6 | 3.3 |
| U6 to Ar-A | 24.4 | 2.1 | 24.2 | 3.1 |
| L6 to Lr-B | 16.1 | 2.3 | 16.0 | 2.3 |
| Angular | ||||
| SN to OP | 17.6 | 3.3 | 25.1 * | 5.1 |
| PP to OP | 7.7 | 2.5 | 14.1 * | 4.1 |
| U1 to SN | 103.5 | 11.1 | 105.7 | 5.8 |
| U1 to FH | 110.0 | 7.0 | 113.4 | 11.2 |
| U1 to PP | 115.6 | 5.0 | 114.4 | 10.8 |
| U1 to OP | 56.7 | 4.6 | 51.4 | 8.4 |
| L1 to FH (FMIA) | 56.6 | 6.9 | 43.6 * | 10.5 |
| L1 to OP | 69.9 | 6.7 | 58.7 * | 8.6 |
| L1 to MP (IMPA) | 94.5 | 7.7 | 94.8 | 8.9 |
| Interincisal angle | 126.6 | 10.3 | 110.1 * | 13.8 |
| Measurement | Control | ICR | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Linear | ||||
| E-line to ULP | −1.7 | 2.3 | 4.5 * | 4.7 |
| E-line to LLP | −0.3 | 2.5 | 5.3 * | 4.8 |
| Angular | ||||
| Z-angle | 71.7 | 7.8 | 54.0 * | 14.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanimoto, K.; Awada, T.; Onishi, A.; Kubo, N.; Asakawa, Y.; Kunimatsu, R.; Hirose, N. Characteristics of the Maxillofacial Morphology in Patients with Idiopathic Mandibular Condylar Resorption. J. Clin. Med. 2022, 11, 952. https://doi.org/10.3390/jcm11040952
Tanimoto K, Awada T, Onishi A, Kubo N, Asakawa Y, Kunimatsu R, Hirose N. Characteristics of the Maxillofacial Morphology in Patients with Idiopathic Mandibular Condylar Resorption. Journal of Clinical Medicine. 2022; 11(4):952. https://doi.org/10.3390/jcm11040952
Chicago/Turabian StyleTanimoto, Kotaro, Tetsuya Awada, Azusa Onishi, Naoki Kubo, Yuki Asakawa, Ryo Kunimatsu, and Naoto Hirose. 2022. "Characteristics of the Maxillofacial Morphology in Patients with Idiopathic Mandibular Condylar Resorption" Journal of Clinical Medicine 11, no. 4: 952. https://doi.org/10.3390/jcm11040952
APA StyleTanimoto, K., Awada, T., Onishi, A., Kubo, N., Asakawa, Y., Kunimatsu, R., & Hirose, N. (2022). Characteristics of the Maxillofacial Morphology in Patients with Idiopathic Mandibular Condylar Resorption. Journal of Clinical Medicine, 11(4), 952. https://doi.org/10.3390/jcm11040952






